Copyright
©The Author(s) 2024.
World J Gastrointest Pathophysiol. Apr 22, 2024; 15(1): 92864
Published online Apr 22, 2024. doi: 10.4291/wjgp.v15.i1.92864
Published online Apr 22, 2024. doi: 10.4291/wjgp.v15.i1.92864
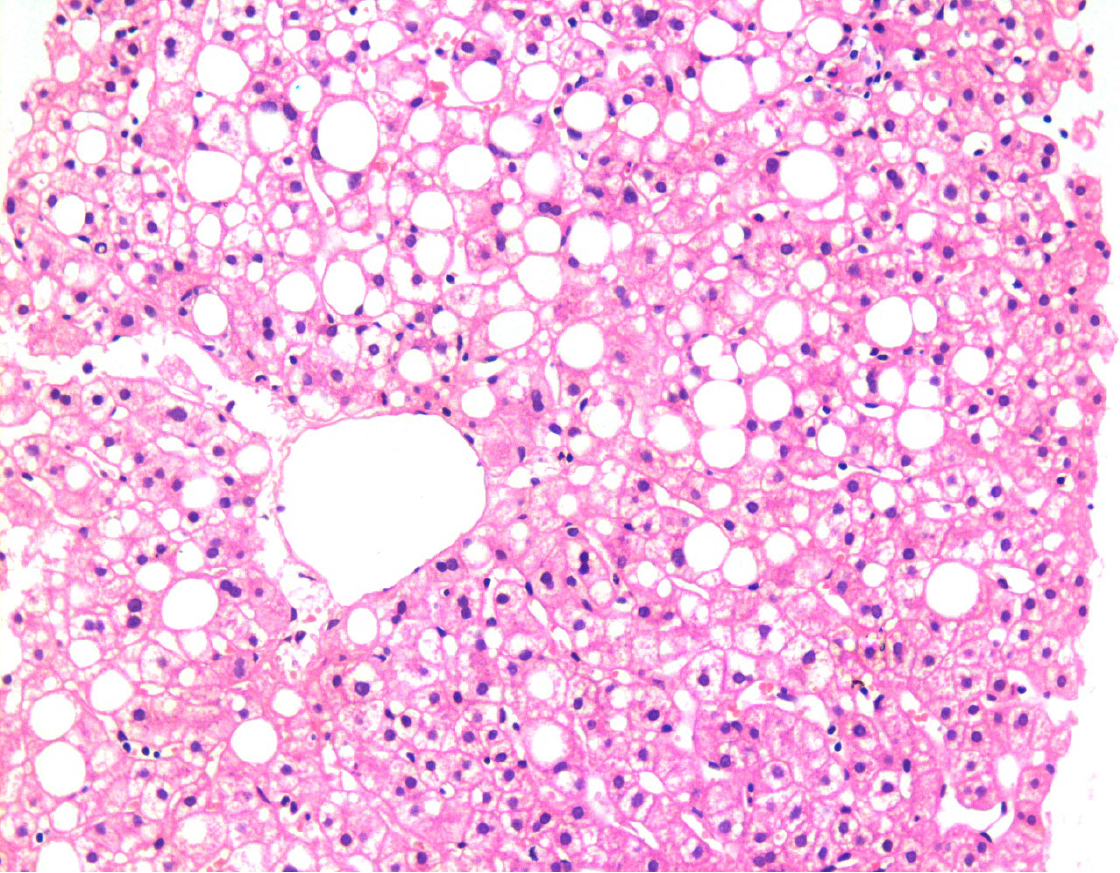
Figure 1 Liver biopsy showing fatty changes.
There is a predominant macro-vesicular fatty change in the centrilobular area. There is no significant hepatocellular damage, inflammation, or fibrosis. This represents one end of the spectrum of fatty diseases of the liver (HE, × 200).
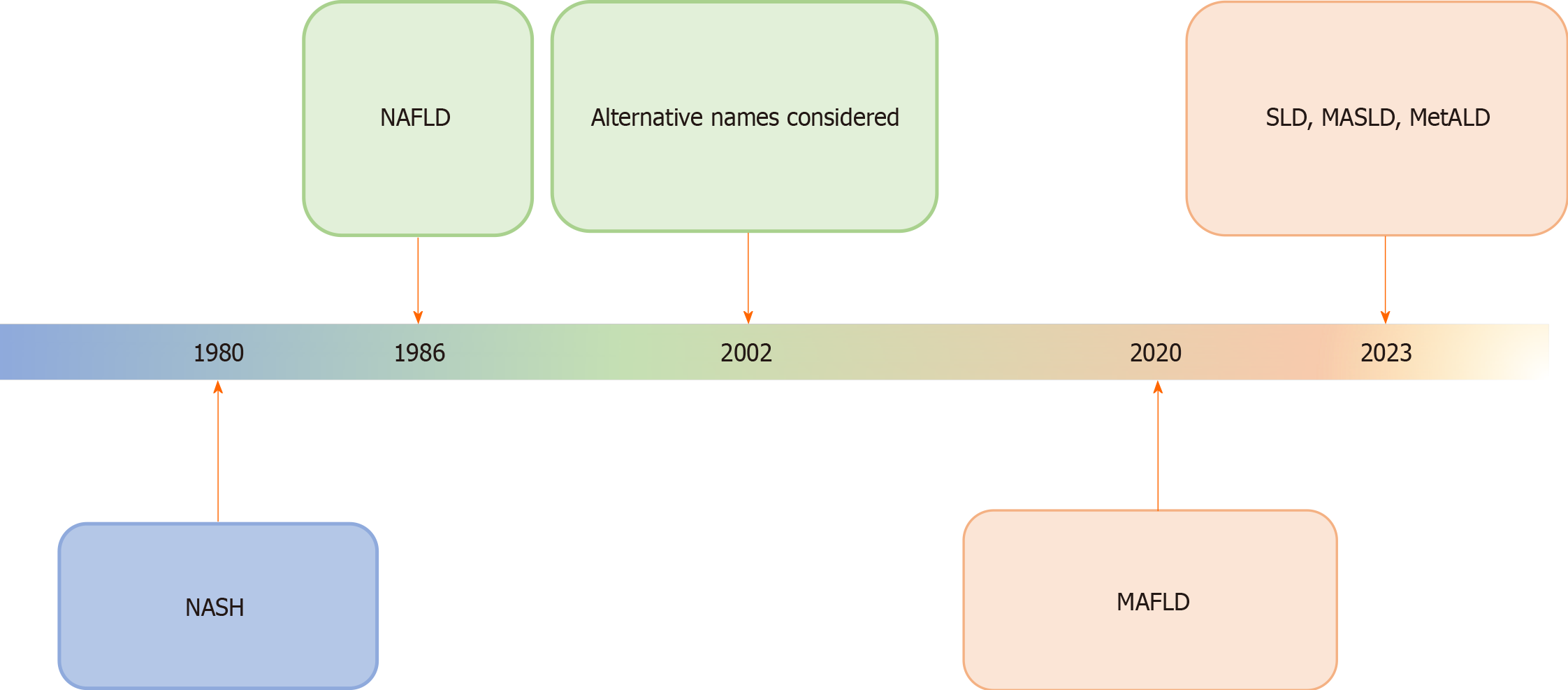
Figure 2 Schematic diagram showing the history of evolution of nomenclature changes of fatty liver diseases, particularly, non-alcoholic fatty liver disease.
The most recent name suggested is the overarching term of steatotic liver disease. The rationalization of classification approaches is highlighted by changes in color. NASH: Non-alcoholic steatohepatitis; MAFLD: Metabolic dysfunction-associated fatty liver disease; MASLD: Metabolic dysfunction-associated SLD; MetALD: MASLD, and moderate alcohol intake; NAFLLD: Non-alcoholic fatty liver disease; SLD: Steatotic liver disease.
Figure 3 Liver biopsy showing morphological changes of non-alcoholic steatohepatitis, now named metabolic dysfunction-associated steatohepatitis.
There is the macro-vesicular fatty change associated with ballooned hepatocytes (green arrow), inflammation, and fibrosis. A few Mallory bodies are seen in the ballooned hepatocytes (blue arrow). This represents the progressive form of fatty disease of the liver that may progress to cirrhosis if left untreated (HE, × 200).
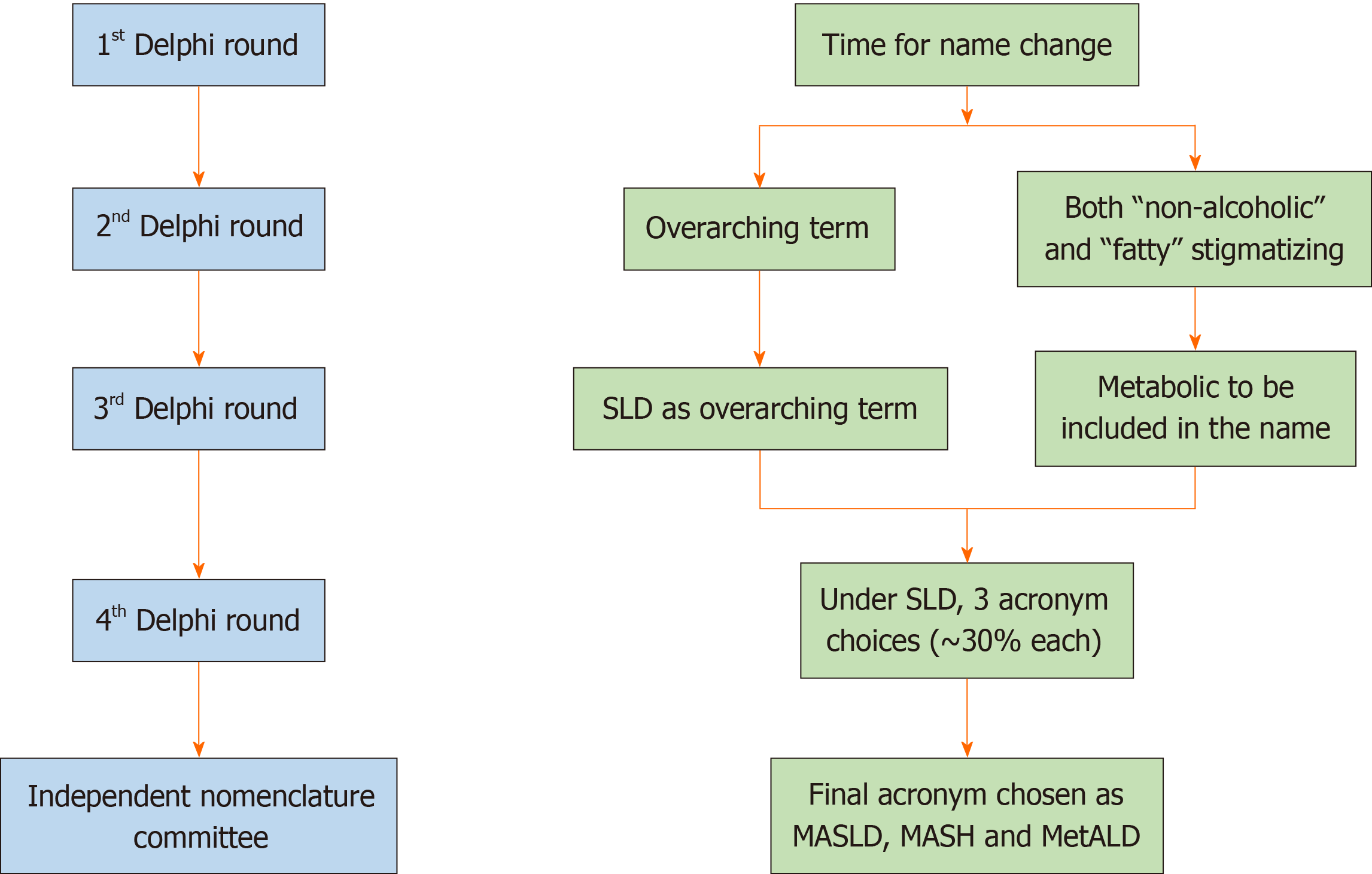
Figure 4 Overview of the main methodology used to change the name of fatty liver disease.
The conclusions reached at each round of the Delphi method are shown on the right. Changes were also made in the diagnostic criteria (not shown here). An independent subcommittee comprising expert hepatologists, endocrinologists, pediatricians, and patients chose between the top three acronyms emerging from the fourth Delphi round. SLD: Steatotic liver disease; MASLD: Metabolic dysfunction-associated SLD; MASH: Metabolic dysfunction-associated steatohepatitis; MetALD: MASLD, and moderate alcohol intake.
Figure 5 Steatotic Liver Disease and its sub-categorization.
This figure shows the schema for steatotic liver disease (SLD) and its sub-categorization. SLD, diagnosed by imaging studies or histology, has many potential causes. Metabolic dysfunction-associated SLD, defined as hepatic steatosis together with one cardiometabolic risk factor and no other apparent cause, ALD, and an overlap of the two (MetALD), comprise the most common causes of SLD. Other specific causes of SLD need to be considered separately, as they exhibit distinct pathogenesis. Multiple etiologies of steatosis can coexist in one case. Those with no identifiable cause are currently placed under the cryptogenic SLD category. However, these may be reclassified in the future in response to an increase in our understanding of disease pathophysiology. SLD: Steatotic liver disease.
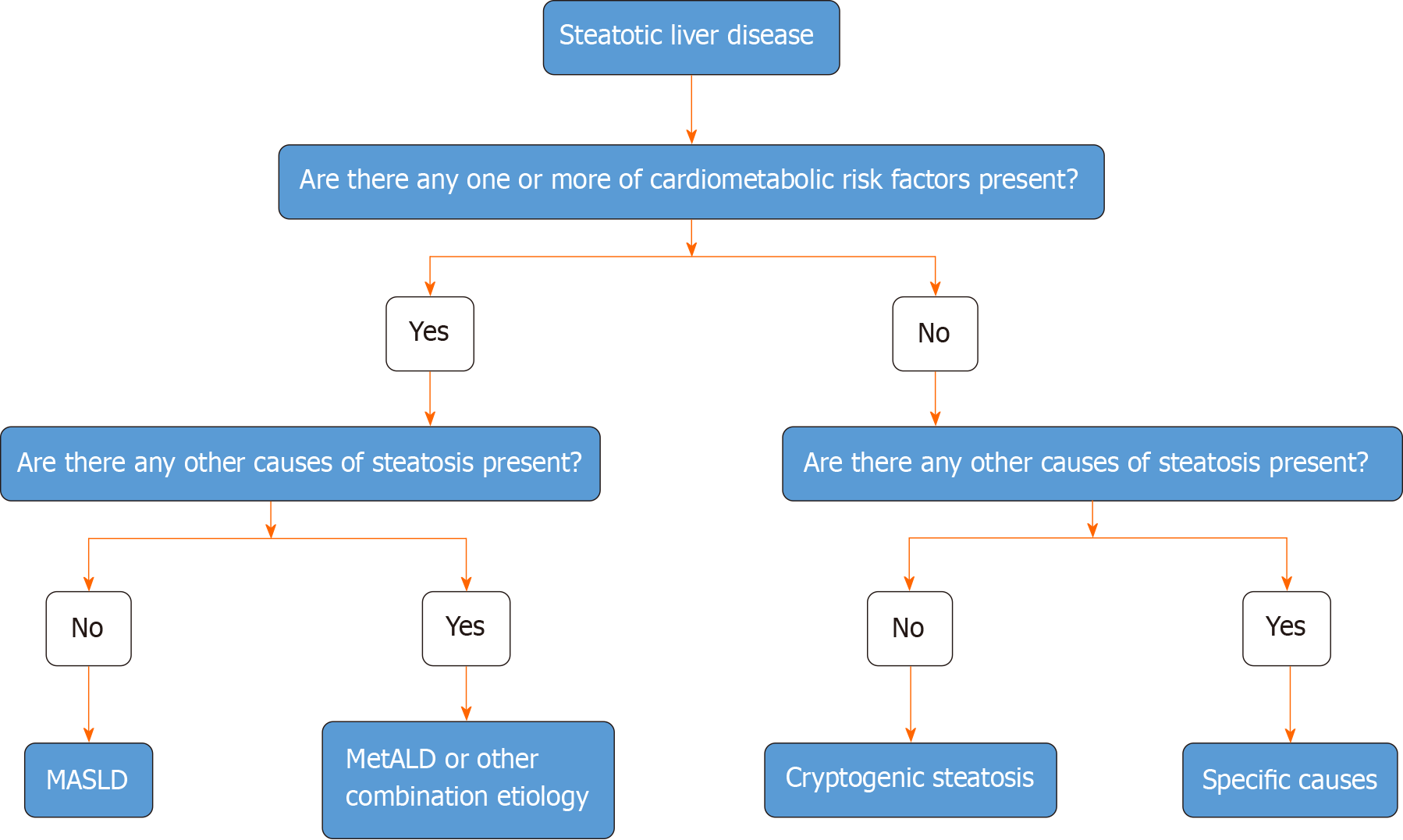
Figure 6 Algorithmic approach to the categorization of steatotic liver disease.
In the presence of hepatic steatosis either on imaging or liver biopsy, the presence of any of a cardiometabolic risk factor (CMRF) will lead to a diagnosis of metabolic dysfunction-associated steatotic liver disease (SLD) in the absence of other causes of hepatic steatosis. If additional causes of steatosis are identified, then this will qualify for a combination etiology. In the case of alcohol, this is labeled MetALD. In the absence of overt CMRF, other causes must be excluded and if none is identified, this is labeled cryptogenic SLD. MASLD: Metabolic dysfunction-associated SLD; MetALD: MASLD, and moderate alcohol intake.
- Citation: Mubarak M. Changes in the terminology and diagnostic criteria of non-alcoholic fatty liver disease: Implications and opportunities. World J Gastrointest Pathophysiol 2024; 15(1): 92864
- URL: https://www.wjgnet.com/2150-5330/full/v15/i1/92864.htm
- DOI: https://dx.doi.org/10.4291/wjgp.v15.i1.92864