Published online May 28, 2017. doi: 10.4329/wjr.v9.i5.223
Peer-review started: October 14, 2016
First decision: November 11, 2016
Revised: February 22, 2017
Accepted: March 16, 2017
Article in press: March 17, 2017
Published online: May 28, 2017
Processing time: 224 Days and 4.6 Hours
To assess the correlation of lateral recess stenosis (LRS) of lumbar segments L4/5 and L5/S1 and the Oswestry Disability Index (ODI).
Nine hundred and twenty-seven patients with history of low back pain were included in this uncontrolled study. On magnetic resonance images (MRI) the lateral recesses (LR) at lumbar levels L4/5 and L5/S1 were evaluated and each nerve root was classified into a 4-point grading scale (Grade 0-3) as normal, not deviated, deviated or compressed. Patient symptoms and disability were assessed using ODI. The Spearman’s rank correlation coefficient was used for statistical analysis (P < 0.05).
Approximately half of the LR revealed stenosis (grade 1-3; 52% at level L4/5 and 42% at level L5/S1) with 2.2% and 1.9% respectively reveal a nerve root compression. The ODI score ranged from 0%-91.11% with an arithmetic mean of 34.06% ± 16.89%. We observed a very weak statistically significant positive correlation between ODI and LRS at lumbar levels L4/5 and L5/S1, each bilaterally (L4/5 left: rho < 0.105, P < 0.01; L4/5 right: rho < 0.111, P < 0.01; L5/S1 left: rho 0.128, P < 0.01; L5/S1 right: rho < 0.157, P < 0.001).
Although MRI is the standard imaging tool for diagnosing lumbar spinal stenosis, this study showed only a weak correlation of LRS on MRI and clinical findings. This can be attributed to a number of reasons outlined in this study, underlining that imaging findings alone are not sufficient to establish a reliable diagnosis for patients with LRS.
Core tip: In the presented study lateral recesses of nearly 1000 patients with low back pain were evaluated on magnetic resonance imaging (MRI) and correlated with patient symptoms. Though MRI is the method of choice for diagnosing lumbar spinal stenosis, we revealed only a very weak correlation of lateral recess stenosis (LRS) and patient symptoms. This can be attributed to numerous reasons outlined in this study, underlining that imaging findings alone are not sufficient for an adequate diagnostic approach of patients with LRS.
- Citation: Splettstößer A, Khan MF, Zimmermann B, Vogl TJ, Ackermann H, Middendorp M, Maataoui A. Correlation of lumbar lateral recess stenosis in magnetic resonance imaging and clinical symptoms. World J Radiol 2017; 9(5): 223-229
- URL: https://www.wjgnet.com/1949-8470/full/v9/i5/223.htm
- DOI: https://dx.doi.org/10.4329/wjr.v9.i5.223
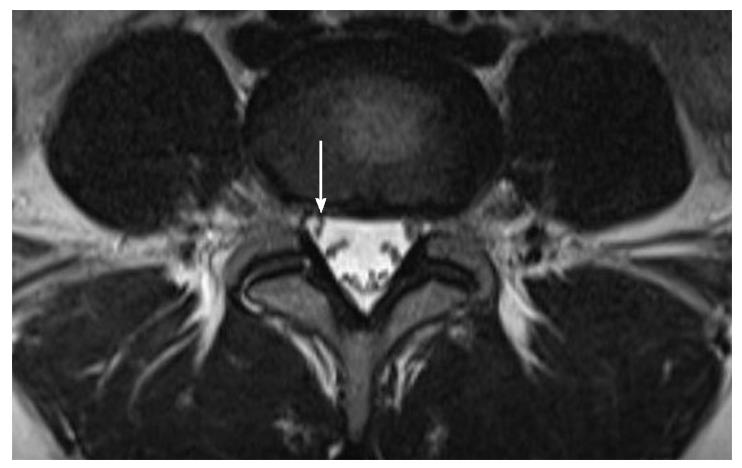
After arthritis and rheumatism[1] low back pain (LBP) is the second most cause of disability in United States adults, and thus is a major social and economic issue[2]. With the aging population the prevalence is even drastically rising[3]. Lumbar spinal stenosis (LSS) is one main cause of LBP. As a distinct syndrome LSS was already described by Verbiest et al[4] in 1954. Most studies about LSS focus on the central LSS. Failure to recognize or adequately treat lateral recess stenosis (LRS) is considered to be the main reason for failed back surgery on the lumbar spine[5]. On account of this we focused on the LRS in the presented study. Regarding imaging analyses LSS is defined by the reduced size of the spinal canal. Based on the anatomical regions, LSS is generally subdivided in central spinal stenosis, LRS and foraminal stenosis. The LRS affects the lateral region of the lumbar spinal canal that is bordered laterally by the pedicle, posteriorly by the superior articular facet, and anteriorly by the vertebral body, endplate margin, and disc margin[6] (Figure 1). LRS is most commonly caused by degenerative changes of the spine such as facet joint osteoarthritis, ligamentum flavum hypertrophy, intervertebral disc degeneration and endplate spur. Congenital abnormalities, bone diseases, tumors or trauma are rare causes of LRS[7]. According to Bartynski et al[8] two pathways for the development of degenerative LRS exist. On the one hand the congenital or acquired trefoil canal in which the nerve root remains in its position in the LR and the narrowing of the LR developes in an anteroposterior fashion. Regarding the acquired trefoil canal first of all facet joint osteoarthritis causes the trefoil-shape, subsequent following endplate and disc degeneration result in LRS. The second pathway is called acute angular pinch. The narrowing occurs simultaneously from all directions due to endplate, disc and facet joint degeneration. The nerve root is either deviated medially or compressed in the LR. Magnetic resonance imaging (MRI) is considered the standard imaging technique for evaluation of LSS[9-11] due to the best soft tissue contrast[7]. Although LSS as a distinct syndrome has already been described more than 60 years ago, the radiological classification systems remain inconsistent[12,13]. In 2014 the “Consensus conference of core radiological parameters to describe lumbar stenosis” with 15 internationally renowned experts focused on this problem[12]. Concerning the LRS they recommend the classification system of Bartynski et al[8] which focuses on the compression and the localization of the nerve root in the LR. In short Bartynski et al[8] divided the LRS in 4 grades: Normal (grade 0), small without root compression (grade 1), small with root compression (grade 2) and severe root compression (grade 3). LSS is usually diagnosed by clinical findings in correlation with imaging results. However in the daily routine we frequently experience a mismatch between LBP and MRI results. The aim of our study was to verify this mismatch regarding LBP and LRS. To the best of our knowledge there are no previous studies investigating the correlation of LBP and MRI findings of LRS in such a large group of patients.
The study was approved by the ethical committee. In total the study involved lumbar MR images of 927 patients (410 men and 517 women). The mean age of the patients included was 47.7 years (ranging from 13 to 92 years). All patients included in the study had suffered from LBP without any history of spinal surgery. Criteria for exclusion of patients were confirmed disc herniation, spinal stenosis, scoliosis and vertebral fractures. The MR images were gathered over a time of one year with suspected disc herniation and facet joint degeneration being the main reasons for MRI.
MRI of the lumbar spine was conducted with a 1.5 Tesla MRI system (Magnetom® Avanto, Siemens AG, Erlangen, Germany) and a dedicated receive only spine coil. For imaging analysis axial T2-weighted images were obtained using fast spin-echo sequences. The sequence parameters were: TR 3550; TE 90; matrix 448; field of view 210 mm; slice thickness 4 mm; interslice gap 10%, number of excitations.
All MR images were assessed in consensus by two blinded authors (Adel Maataoui, M Fawad Khan). Both authors are board certified radiologists with longstanding experience in imaging of the musculoskeletal system. Degeneration of lumbar spine concerns mostly segments L4/5 and L5/S1, for which reason the LR of these segments were graded on axial T2-weighted fast spin-echo images. All in all, an overall number of 3708 lateral recesses were rated.
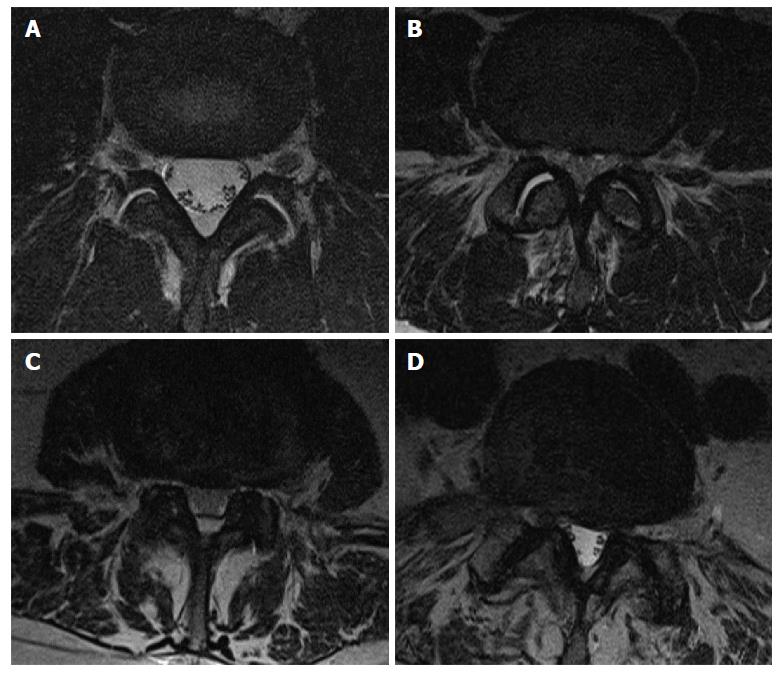
Our grading system of LRS was based on Bartynski’s classification. We defined grade 0 as a normal LR in which the nerve root is bathed in cerebrospinal fluid. There is no contact to the adjacent structures. Grade 1 represents a narrowing of the LR without root deviation. Grade 2 additionally reveals a root deviation. Grade 3 describes a compression of the nerve root (Table 1, Figure 2).
| Grade | Nerve root in the lateral recess |
| 0 | Normal |
| 1 | No deviation |
| 2 | Deviation |
| 3 | Compression |
By means of the Oswestry Disability Index (ODI) functional status was assessed. The ODI is one of the principle outcome measure questionnaires for LBP - it measures pain and disability, which are core items in patients with LBP[14]. We used the german version of the ODI developed by Mannion et al[15]. This standardized, self-administered questionnaire contains ten sections: One section about pain intensity and nine sections about limitations of various activities of daily life, namely personal care (washing, dressing, etc.), lifting, walking, sitting, standing, sleeping, sex life, social life and travelling[16]. The question about sex life was excluded on grounds of ethical aspects. Each section is scored on a scale of 0-5 points with 0 representing no disability and 5 the greatest disability. Section 2 “personal care” for example contains the following statements and scores: I can look after myself normally without causing extra pain (0); I can look after myself normally but it is very painful (1); It is painful to look after myself and I am slow and careful (2); I need some help but manage most of my personal care (3); I need help every day in most aspects of self care (4); and I do not get dressed, wash with difficulty and stay in bed (5)[16].
Finally the index is calculated by dividing the summed score by the total possible score (which has to be reduced by 5 for every question not answered). The result is then multiplied by 100 and expressed as a percentage. The result is interpreted as follows: Score of 0%-20%, minimal disability; 20%-40%, moderate disability; 40%-60%, severe disability; 60%-80%, crippled; 80%-100%, patients are bedbound.
Data were analysed with the use of the BIAS software package (Epsilon publisher, Frankfurt a.M., Germany). In order to evaluate the correlation of LRS and ODI Spearman’s coefficient of rank correlation was determined. P value < 0.05 were considered statistically significant.
Three thousand seven hundred and eight LR of 927 patients were assessed at lumbar level L4/5 and L5/S1. Table 2 presents the number of LR according to the relative grade of stenosis. The image evaluation revealed 430/461 grade 0 stenosis (48.1%), 357/349 grade 1 stenosis (38.1%), 113/103 grade 2 stenosis (11.7%) and 27/14 grade 3 stenosis (2.2%) for the left/right side of lumbar level L4/5 and 528/548 grade 0 stenosis (58%), 303/316 grade 1 stenosis (33.4%), 75/49 grade 2 stenosis (6.7%) and 21/14 grade 3 stenosis (1.9%) for the left/right side of lumbar level L5/S1, respectively.
| Lumbar level | Grades | |||
| 0 | 1 | 2 | 3 | |
| L4/5 left | 430 | 357 | 113 | 27 |
| L4/5 right | 461 | 349 | 103 | 14 |
| L5/S1 left | 528 | 303 | 75 | 21 |
| L5/S1 right | 548 | 316 | 49 | 14 |
According to ODI scores patient symptoms and disability ranged from a minimal score of 0% to a maximal score of 91.11%. The mean value amounted to 34.06% ± 16.89%. Most patients (48.39%) showed a moderate functional disability (21%-40%). Regarding sex no statistical difference between the ODI scores could be revealed: Men 32.47% ± 16.55% and women 35.58% ± 16.55%.
The mean ODI scores for LRS grade 0, 1, 2, 3 of lumbar level L4/5 on the right side were 31.53% ± 15.46%, 31.53% ± 17.60%, 33.01% ± 17.17% and 33.03% ± 16.89%. There was no statistical difference between the ODI score and the grade of LRS on lumbar level L4/5 on the right.
The mean ODI scores for LRS grade 0, 1, 2, 3 of lumbar level L4/5 on the left side were 30.75% ± 17.85%, 30.74% ± 17.03%, 32.39% ± 16.97% and 33.25% ± 16.90%. There was no statistical difference between the ODI score and the grade of LRS on lumbar level L4/5 on the left.
The mean ODI scores for LRS grade 0, 1, 2, 3 of lumbar level L5/S1 on the right side were 32.03% ± 16.58%, 32.03% ± 16.60%, 33.24% ± 16.41% and 33.88% ± 16.76%. There was no statistical difference between the ODI score and the grade of LRS on lumbar level L5/S1 on the right.
The mean ODI scores for LRS grade 0, 1, 2, 3 of lumbar level L5/S1 on the left side were 32.14% ± 16.90%, 33.15% ± 16.62%, 33.13% ± 16.60% and 33.46% ± 16.78%. There was no statistical difference between the ODI score and the grade of LRS on lumbar level L5/S1 on the left.
We observed a very weak statistically significant positive correlation between ODI and LRS at lumbar levels L4/5 and L5/S1, each bilaterally.
L4/5 left and ODI: rho < 0.105, P < 0.01; L4/5 right and ODI: rho < 0.111, P < 0.01; L5/S1 left and ODI: rho 0.128, P < 0.01; L5/S1 right and ODI: rho < 0.157, P < 0.001.
Despite the high prevalence of LSS and that the combination of clinical and imaging findings are the standard diagnostic tools[17] clinical and imaging findings often do not correlate. Haig et al[9] and Geisser et al[18] could not find any difference between symptomatic and asymptomatic patients based on the size of the lumbar spinal canal measured on MR images. Lohmann et al[19] did also not detect a correlation between clinical findings and LSS on computed tomography (CT) images.
The aim of our study was to verify if the results of these studies which focused on central LSS, do also apply to LRS. In the presented study with a cohort of more than 900 patients we found only a very weak positive correlation between the severity of LBP and the severity of LRS. Our findings are supported by the results of Kuittinen et al[20]: By MR imaging and electromyography they evaluated 140 nerve roots of 14 patients, who were selected for surgical treatment of LRS. The findings were correlated with each other as well as with the clinical symptoms, measured by different tests including the ODI. In this little cohort they revealed a positive correlation between MR-findings and EMG and between EMG and patient symptoms. But they revealed no correlation between MR findings and patient symptoms. The study is limited by the very small cohort of patients and the fact that also neuroforaminal stenosis was included.
It is unclear why clinical and imaging findings do often not correlate. The compression of the nerve root is considered to be one of the main causes of symptoms in patients with LRS[21-23]. In an experimental study Lacroix-Fralish et al[24] observed that a nerve root ligation in a rat model produced mechanical allodynia. Mechanical root compression in a dog model revealed intraradicular edema and Wallerian degeneration[25]. Using a silicon tube Saal[26] and Xue et al[27] produced lumbar nerve root compression in a rat model, which resulted in disappearing of the myelin sheath and activation of microglia, which is assumed to participate in the genesis and maintenance of pain[24].
Thus, it must be considered that a possible reason for the discrepancy between MRI findings and patient symptoms could be that MRI does not sufficiently identify nerve compression. Bartynski et al[8] assessed the accuracy of MRI in 26 patients with symptomatic nerve root compression in the LR at lumbar levels L2/3 - L5/S1. Each patient underwent MRI, conventional myelograpy and CT myelography; the root compression was confirmed surgically and a post-operative pain improvement could be observed. In MRI the root compression was underestimated in nearly 30%.
LSS, in addition, has an important dynamic component. MRI was performed, as usual, with the patient lying in the supine position. Yet it is known and even a key feature for LSS that patient symptoms increase under axial loading and lumbar extension while they decrease under axial distraction and flexion[17,28]. This can be explained by anatomic alterations: Flexion and extension can change the size of the central lumbar canal, the LR and the neural foramen and can consecutively result in changes of the cauda equina as well as in isolated nerve root compression in the LR[29]. In experimental studies axial loading has caused alterations of the size of the lumbar canal and the neural foramen[30]. In the upright position axial loading can cause displacement of peridiscal structures that lead to a nerve root compression which is not observable in the supine position[31]. In addition the pressure in the lumbar canal can be altered by postural changes[32,33].
Two other aspects should be considered as possible explanations for the weak correlation. On the one hand the nerve root can be compressed without clinical symptoms. On the other hand clinical symptoms can be evident without imaging findings of root compression. Although there are single studies which reveal nerve root compression in approximately 20% of asymptomatic individuals[34], there is in total only a small number of asymptomatic individuals who reveal nerve root compression in MRI. In a study presented by Weishaupt et al[35] with 60 asymptomatic volunteers only one single root compression was observed in MRI by one of the readers. A study of nearly 100 asymptomatic elite junior tennis players revealed a nerve root compression in only 2%[36]. Boos et al[37] reported a “major nerve deformation” in 4% of asymptomatic adults.
A possible explanation for clinical symptoms without evident nerve root compression in imaging is the inflammation of the nerve root caused by inflammatory mediators[38,39], for example, Interleukin β1[40]. It is hypothesized, that these substances can diffuse in the spinal canal from the facet joints, the ligamentum flavum[40] and from the intervertebral disc[26,41].
Beside the nerve root nearly all lumbar structures are potential sources of LBP, such as the facet joints, the intervertebral discs, bones, fascial structures and muscles[42]. Especially facet joint osteoarthritis is known for radiating pain without evidence of nerve root compression[43,44]. Because of the fact that LRS is based on facet joint osteoarthritis, intervertebral disc degeneration, ligamentum flavum hypertrophy and endplate spur we have to consider that in our study each of these structures could be the crucial factor for patient symptoms.
LBP rarely causes objective endpoints so outcomes are best measured with patient-reported metrics[45]. We assessed patient symptoms by means of the ODI. It is one of the most commonly used measures of disability in back pain[46]. It has established psychometric properties, is easy to use and has a low administrative burden[46]. Yet, based on self-reported symptoms, the ODI remains subjective. Furthermore it does not measure nerve root level specific symptoms. A limitation of the presented study is that results of clinical, more objective, examinations were not included and that we assessed no nerve root level specific symptoms. In addition the LRS were not proved surgically.
In conclusion, in our broad study population we only found a very weak statistically significant positive correlation between LBP and LRS on MR-images, thus confirming the well-known problem that in the context of diagnosing LBP clinical and imaging findings often do not correlate. Our results underline the necessity not to evaluate LRS isolated on imaging but in relation to clinical findings.
Low back pain (LBP) is an important issue for healthcare systems all over the world. One reason of LBP is lumbar spinal stenosis (LSS), with lateral recess stenosis (LRS) not gaining as much attention as central spinal stenosis, a fact that is assumed to be the main reason for failed back surgery. Concerning imaging techniques magnetic resonance imaging (MRI) is the standard imaging tool for evaluating LSS. However in the daily routine people frequently experience a mismatch between LBP and MRI results. The aim of this study was to verify this mismatch regarding LBP and LRS.
The problem that in the context of LBP clinical and imaging findings often do not correlate has been the objective of numerous studies in the past. Yet the LRS as one reason of LBP is underrepresented and most studies have a small study population.
The authors assessed the correlation between LBP and LRS in a very broad study population including nearly 1000 patients. Functional status was assessed by means of the Oswestry Disability Index (ODI), and LRS was assessed on axial magnetic resonance images of lumbar level L4/5 and L5/S1 by evaluating the nerve root in the lateral recess on a 4 point grading scale. The authors revealed a very weak statistically significant positive correlation between ODI and LRS at the L4/5 segment as well as the L5/S1 segment.
The presented findings underline the necessity not to evaluate LRS isolated on imaging but in relation with the clinical findings.
Lateral recess stenosis: It describes the stenosis of the lateral part of the lumbar spinal canal that is bordered laterally by the pedicle, posteriorly by the superior articular facet, and anteriorly by the vertebral body, endplate margin, and disc margin. It is most commonly caused by degenerative changes; Oswestry Disability Index: The Oswestry Disability Index is one of the principle outcome measure questionnaires for low back pain focussing on disability and pain.
The authors studied the correlation of lumbar recess stenosis in MRI with clinical symptoms.
Manuscript source: Invited manuscript
Specialty type: Radiology, nuclear medicine and medical imaging
Country of origin: Germany
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Cerwenka HR, Gao BL S- Editor: Song XX L- Editor: A E- Editor: Li D
| 1. | From the Centers for Disease Control and Prevention. Prevalence of disabilities and associated health conditions among adults--United States, 1999. JAMA. 2001;285:1571-1572. [PubMed] |
| 2. | Balagué F, Mannion AF, Pellisé F, Cedraschi C. Non-specific low back pain. Lancet. 2012;379:482-491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1022] [Cited by in RCA: 1116] [Article Influence: 85.8] [Reference Citation Analysis (0)] |
| 3. | Freburger JK, Holmes GM, Agans RP, Jackman AM, Darter JD, Wallace AS, Castel LD, Kalsbeek WD, Carey TS. The rising prevalence of chronic low back pain. Arch Intern Med. 2009;169:251-258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 861] [Cited by in RCA: 977] [Article Influence: 61.1] [Reference Citation Analysis (0)] |
| 4. | Verbiest H. A radicular syndrome from developmental narrowing of the lumbar vertebral canal. J Bone Joint Surg Br. 1954;36-B:230-237. [PubMed] |
| 5. | Burton CV, Kirkaldy-Willis WH, Yong-Hing K, Heithoff KB. Causes of failure of surgery on the lumbar spine. Clin Orthop Relat Res. 1981;191-199. [PubMed] |
| 6. | Lee CK, Rauschning W, Glenn W. Lateral lumbar spinal canal stenosis: classification, pathologic anatomy and surgical decompression. Spine (Phila Pa 1976). 1988;13:313-320. [PubMed] |
| 7. | Andreisek G, Hodler J, Steurer J. Uncertainties in the diagnosis of lumbar spinal stenosis. Radiology. 2011;261:681-684. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 41] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 8. | Bartynski WS, Lin L. Lumbar root compression in the lateral recess: MR imaging, conventional myelography, and CT myelography comparison with surgical confirmation. AJNR Am J Neuroradiol. 2003;24:348-360. [PubMed] |
| 9. | Haig AJ, Geisser ME, Tong HC, Yamakawa KS, Quint DJ, Hoff JT, Chiodo A, Miner JA, Phalke VV. Electromyographic and magnetic resonance imaging to predict lumbar stenosis, low-back pain, and no back symptoms. J Bone Joint Surg Am. 2007;89:358-366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 82] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 10. | Sasiadek MJ, Bladowska J. Imaging of degenerative spine disease--the state of the art. Adv Clin Exp Med. 2012;21:133-142. [PubMed] |
| 11. | Malfair D, Beall DP. Imaging the degenerative diseases of the lumbar spine. Magn Reson Imaging Clin N Am. 2007;15:221-238, vi. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 32] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 12. | Andreisek G, Deyo RA, Jarvik JG, Porchet F, Winklhofer SF, Steurer J. Consensus conference on core radiological parameters to describe lumbar stenosis - an initiative for structured reporting. Eur Radiol. 2014;24:3224-3232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 56] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 13. | Andreisek G, Imhof M, Wertli M, Winklhofer S, Pfirrmann CW, Hodler J, Steurer J. A systematic review of semiquantitative and qualitative radiologic criteria for the diagnosis of lumbar spinal stenosis. AJR Am J Roentgenol. 2013;201:W735-W746. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 64] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 14. | Deyo RA, Battie M, Beurskens AJ, Bombardier C, Croft P, Koes B, Malmivaara A, Roland M, Von Korff M, Waddell G. Outcome measures for low back pain research. A proposal for standardized use. Spine (Phila Pa 1976). 1998;23:2003-2013. [PubMed] |
| 15. | Mannion AF, Junge A, Fairbank JC, Dvorak J, Grob D. Development of a German version of the Oswestry Disability Index. Part 1: cross-cultural adaptation, reliability, and validity. Eur Spine J. 2006;15:55-65. [PubMed] |
| 16. | Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine (Phila Pa 1976). 2000;25:2940-2952; discussion 2952. [PubMed] |
| 17. | Genevay S, Atlas SJ. Lumbar spinal stenosis. Best Pract Res Clin Rheumatol. 2010;24:253-265. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 275] [Cited by in RCA: 246] [Article Influence: 16.4] [Reference Citation Analysis (0)] |
| 18. | Geisser ME, Haig AJ, Tong HC, Yamakawa KS, Quint DJ, Hoff JT, Miner JA, Phalke VV. Spinal canal size and clinical symptoms among persons diagnosed with lumbar spinal stenosis. Clin J Pain. 2007;23:780-785. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 84] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 19. | Lohman CM, Tallroth K, Kettunen JA, Lindgren KA. Comparison of radiologic signs and clinical symptoms of spinal stenosis. Spine (Phila Pa 1976). 2006;31:1834-1840. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 78] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 20. | Kuittinen P, Sipola P, Aalto TJ, Määttä S, Parviainen A, Saari T, Sinikallio S, Savolainen S, Turunen V, Kröger H. Correlation of lateral stenosis in MRI with symptoms, walking capacity and EMG findings in patients with surgically confirmed lateral lumbar spinal canal stenosis. BMC Musculoskelet Disord. 2014;15:247. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 21. | Shobeiri E, Khalatbari MR, Taheri MS, Tofighirad N, Moharamzad Y. Magnetic resonance imaging characteristics of patients with low back pain and those with sciatica. Singapore Med J. 2009;50:87-93. [PubMed] |
| 22. | Ciric I, Mikhael MA, Tarkington JA, Vick NA. The lateral recess syndrome. A variant of spinal stenosis. J Neurosurg. 1980;53:433-443. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 87] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 23. | Epstein JA EN. Lumbar spondylosis and spinal stenosis. editor Neurosurgery. New York: McGraw Hill 1996; 3831-3840. |
| 24. | Lacroix-Fralish ML, Tawfik VL, Tanga FY, Spratt KF, DeLeo JA. Differential spinal cord gene expression in rodent models of radicular and neuropathic pain. Anesthesiology. 2006;104:1283-1292. [PubMed] |
| 25. | Kobayashi S, Yoshizawa H, Yamada S. Pathology of lumbar nerve root compression. Part 1: Intraradicular inflammatory changes induced by mechanical compression. J Orthop Res. 2004;22:170-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 75] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 26. | Saal JS. The role of inflammation in lumbar pain. Spine (Phila Pa 1976). 1995;20:1821-1827. [PubMed] |
| 27. | Xue F, Wei Y, Chen Y, Wang Y, Gao L. A rat model for chronic spinal nerve root compression. Eur Spine J. 2014;23:435-446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 28. | Schönström N, Lindahl S, Willén J, Hansson T. Dynamic changes in the dimensions of the lumbar spinal canal: an experimental study in vitro. J Orthop Res. 1989;7:115-121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 145] [Article Influence: 4.0] [Reference Citation Analysis (1)] |
| 29. | Penning L, Wilmink JT. Posture-dependent bilateral compression of L4 or L5 nerve roots in facet hypertrophy. A dynamic CT-myelographic study. Spine (Phila Pa 1976). 1987;12:488-500. [PubMed] |
| 30. | Nowicki BH, Yu S, Reinartz J, Pintar F, Yoganandan N, Haughton VM. Effect of axial loading on neural foramina and nerve roots in the lumbar spine. Radiology. 1990;176:433-437. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 45] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 31. | Beattie PF, Meyers SP, Stratford P, Millard RW, Hollenberg GM. Associations between patient report of symptoms and anatomic impairment visible on lumbar magnetic resonance imaging. Spine (Phila Pa 1976). 2000;25:819-828. [PubMed] |
| 32. | Olmarker K, Rydevik B, Hansson T, Holm S. Compression-induced changes of the nutritional supply to the porcine cauda equina. J Spinal Disord. 1990;3:25-29. [PubMed] |
| 33. | Takahashi K, Kagechika K, Takino T, Matsui T, Miyazaki T, Shima I. Changes in epidural pressure during walking in patients with lumbar spinal stenosis. Spine (Phila Pa 1976). 1995;20:2746-2749. [PubMed] |
| 34. | van Rijn JC, Klemetso N, Reitsma JB, Majoie CB, Hulsmans FJ, Peul WC, Bossuyt PM, Heeten GJ, Stam J. Symptomatic and asymptomatic abnormalities in patients with lumbosacral radicular syndrome: Clinical examination compared with MRI. Clin Neurol Neurosurg. 2006;108:553-557. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 32] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 35. | Weishaupt D, Zanetti M, Hodler J, Boos N. MR imaging of the lumbar spine: prevalence of intervertebral disk extrusion and sequestration, nerve root compression, end plate abnormalities, and osteoarthritis of the facet joints in asymptomatic volunteers. Radiology. 1998;209:661-666. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 352] [Cited by in RCA: 298] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 36. | Rajeswaran G, Turner M, Gissane C, Healy JC. MRI findings in the lumbar spines of asymptomatic elite junior tennis players. Skeletal Radiol. 2014;43:925-932. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 37] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 37. | Boos N, Rieder R, Schade V, Spratt KF, Semmer N, Aebi M. 1995 Volvo Award in clinical sciences. The diagnostic accuracy of magnetic resonance imaging, work perception, and psychosocial factors in identifying symptomatic disc herniations. Spine (Phila Pa 1976). 1995;20:2613-2625. [PubMed] |
| 38. | Cavanaugh JM. Neural mechanisms of lumbar pain. Spine (Phila Pa 1976). 1995;20:1804-1809. [PubMed] |
| 39. | Siddall PJ, Cousins MJ. Pain mechanisms and management: an update. Clin Exp Pharmacol Physiol. 1995;22:679-688. [PubMed] |
| 40. | Igarashi A, Kikuchi S, Konno S. Correlation between inflammatory cytokines released from the lumbar facet joint tissue and symptoms in degenerative lumbar spinal disorders. J Orthop Sci. 2007;12:154-160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 69] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 41. | McCarron RF, Wimpee MW, Hudkins PG, Laros GS. The inflammatory effect of nucleus pulposus. A possible element in the pathogenesis of low-back pain. Spine (Phila Pa 1976). 1987;12:760-764. [PubMed] |
| 42. | Allegri M, Montella S, Salici F, Valente A, Marchesini M, Compagnone C, Baciarello M, Manferdini ME, Fanelli G. Mechanisms of low back pain: a guide for diagnosis and therapy. F1000Res. 2016;5:pii: F1000 Faculty Rev-1530. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 27] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 43. | Epstein JA, Epstein BS, Rosenthal AD, Carras R, Lavine LS. Sciatica caused by nerve root entrapment in the lateral recess: the superior facet syndrome. J Neurosurg. 1972;36:584-589. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 63] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 44. | V. M. Facet syndrome. In: Weinstein JN WS, eds., editor The lumbar spine: The International Society for the Study of the Lumbar Spine. Philadelphia: WB Saunders Company, 1990: 422-441. . |
| 45. | Werneke M. A proposed set of metrics for standardized outcome reporting in the management of low back pain. Acta Orthop. 2016;87:88. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 46. | Smeets R, Köke A, Lin CW, Ferreira M, Demoulin C. Measures of function in low back pain/disorders: Low Back Pain Rating Scale (LBPRS), Oswestry Disability Index (ODI), Progressive Isoinertial Lifting Evaluation (PILE), Quebec Back Pain Disability Scale (QBPDS), and Roland-Morris Disability Questionnaire (RDQ). Arthritis Care Res (Hoboken). 2011;63 Suppl 11:S158-S173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 172] [Article Influence: 13.2] [Reference Citation Analysis (0)] |