Published online Apr 28, 2017. doi: 10.4329/wjr.v9.i4.206
Peer-review started: June 17, 2016
First decision: July 27, 2016
Revised: August 10, 2016
Accepted: October 17, 2016
Article in press: October 18, 2016
Published online: April 28, 2017
Processing time: 318 Days and 1.2 Hours
To evaluate the association between C-reactive protein (CRP) and radiological evidence of lower respiratory tract infection (LRTI) in infants.
All patients aged less than 4 years who presented with suspected lower respiratory tract infection, who received a peri-presentation chest radiograph and CRP blood measurement over an 18-mo period were included in the study. Age, gender, source of referral, CRP, white cell count, neutrophil count along with the patients’ symptoms and radiologist’s report were recorded.
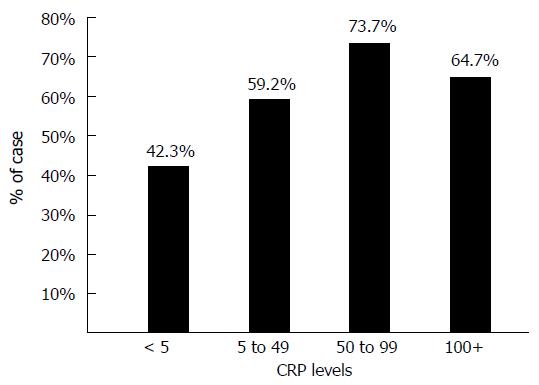
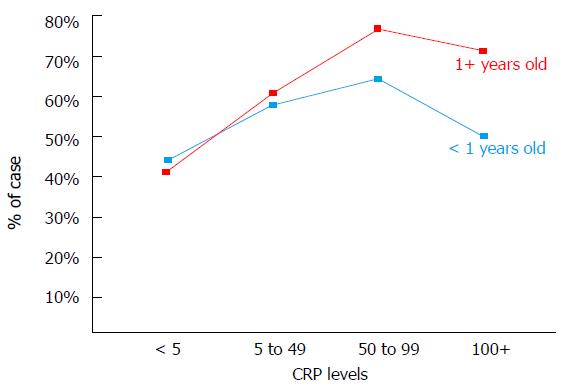
Three hundred and eleven patients met the inclusion criteria. Abnormal chest radiographs were more common in patients with elevated CRP levels (P < 0.01). Radiologic signs of LRTI were identified in 73.7% of chest radiographs when a patient had a CRP level between 50-99 mg/L. CRP levels were a better predictor of positive chest radiograph findings for those aged greater than I year compared to those 1 year or less.
CRP may be used in patients with suspected LRTI diagnosis to select those who are likely to have positive findings on chest radiograph, thus reducing unnecessary chest radiographs.
Core tip: Abnormal chest radiograph findings are significantly more common in patients with elevated C-reactive protein (CRP) levels. Young children are most likely to have abnormal chest radiograph findings if they have all three of the following; a CRP level of 50-99 mg/L, respiratory symptoms and if they are aged greater than 1 year.
- Citation: Twomey M, Fleming H, Moloney F, Murphy KP, Crush L, O’Neill SB, Flanagan O, James K, Bogue C, O’Connor OJ, Maher MM. C-reactive protein and radiographic findings of lower respiratory tract infection in infants. World J Radiol 2017; 9(4): 206-211
- URL: https://www.wjgnet.com/1949-8470/full/v9/i4/206.htm
- DOI: https://dx.doi.org/10.4329/wjr.v9.i4.206
Despite the very low effective dose imparted during the acquisition of a chest radiograph this investigation is common and may be subject to excessive and unjustified use. Children have a greater risk of cancer when exposed to diagnostic ionizing radiation due to their larger proportion of dividing cells and also due to their longer life expectancy during which a potential radiation induced cancer can be expressed[1-3]. Post natal exposure to diagnostic ionizing radiation is associated with an increased risk of childhood acute lymphoblastic leukaemia[1] and brain neoplasms[3] and therefore use of all diagnostic imaging modalities which employ ionizing radiation should be limited and justified in young patients. There is also the issue of cost associated with performance of unnecessary radiological tests an also the issue of stress to patients and parents of performing radiological examinations in infants and young children.
In addition to chest radiography, non-specific serum inflammatory markers are commonly requested in paediatric patients with suspected lower respiratory tract infection (LRTI). Measurement of C-reactive protein (CRP) in these patients is commonplace and often helps to substantiate the clinical diagnosis, to establish the severity of infection and in some cases to monitor the therapeutic management of LRTI[4-11]. Routinely measured CRP levels may potentially be of additional clinical use to physicians and radiologists if they could aid in the selection and justification of performance of chest radiography in the setting of infantile lower respiratory tract infection. No previous study has examined the association between CRP and objective radiological evidence of LRTI in infants. Therefore we designed a retrospective study to determine whether an increased CRP level in paediatric patients presenting with acute respiratory symptoms, is associated with abnormal findings on chest radiography and to determine if other haematological and clinical parameters may additionally predict the presence of chest radiograph abnormalities.
This institutional ethical review board approved, retrospective study was conducted between January 2009 and August 2011. Infants aged between 28 d and 4 years who presented to a single institution with clinically suspected lower respiratory tract infection and who had undergone chest radiography and CRP blood measurement within a 24-h period were included in the study. Patients with chronic lung diseases such as cystic fibrosis were excluded from the study. Presenting symptoms were recorded from the patient medical records for each patient and CRP level, white cell count and neutrophil count were recorded in all cases from the hospital electronic laboratory database. The presence of consolidation, pneumonic infiltrates, bronchial wall thickening, peribronchial cuffing, collapse or effusion were retrospectively recorded in each case by 2 reviewers in consensus (HF, 2-year experience; SON, 4-year experience) following examination of the radiology reports in an unblinded fashion. The CRP level in all patients was measured in mg/L (normal 0-5 mg/L) using the Beckman Coulter Latex Enhanced Turbidometric assay.
Data analysis involved the use of both descriptive and inferential statistics using SPSS 17 (IBM Computers, New York, United States). Descriptive methods employed included one-way and two-way frequencies along with mean and standard deviation. Inferential statistics consisted of χ2 tests and t tests. Correlation coefficient tests explored the relationship between quantitative measures. A threshold P value value below 0.05 was deemed as statistically significant. Numerical averages are presented as mean ± SD unless otherwise stated.
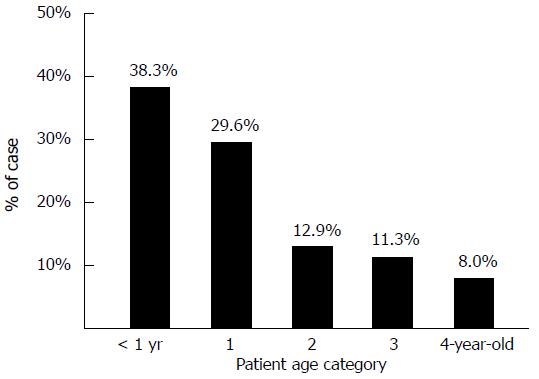
Three hundred and eleven patients were included in the study. There were 164 males (52.7%) and 147 females (47.3%) with ages ranging from 28 d to 4 years (mean age 1.2 years ± 1.3) (Figure 1). The distribution of age was very similar for both genders, with females being just slightly older (1.3 ± 1.3 years) than males (1.1 ± 1.3 years).
Over half of all cases (53.2%) had been admitted directly to hospital following general practitioner (GP) referral, 37.2% were from the emergency department (ED) and the remaining 9.6% were outpatients. Patients aged less than one year of age were significantly more likely to be inpatients (P < 0.01). Forty-seven point five percent of all children who were inpatients were aged less than one year whereas 17.2% of all outpatients and 33% of all ED cases were in this age category. Outpatients were on average over double the age of inpatient cases. This age discrepancy by location is likely explained by a high rate of direct hospital admissions following GP referral, for younger patients as per hospital policy.
Twenty-five point one percent of all CRP measurements were in the “normal” range (0-5 mg/L), 40.2% were in the range 5-49 mg/L, 18.3% were in the 50-99 mg/L range and 16.4% of patients had a CRP of greater than 100 mg/L (Table 1).
| CRP category (mg/L) | Frequency (n) | Percentage |
| < 5 | 78 | 25.1 |
| 5-49 | 125 | 40.2 |
| 50-99 | 57 | 18.3 |
| > 100 | 51 | 16.4 |
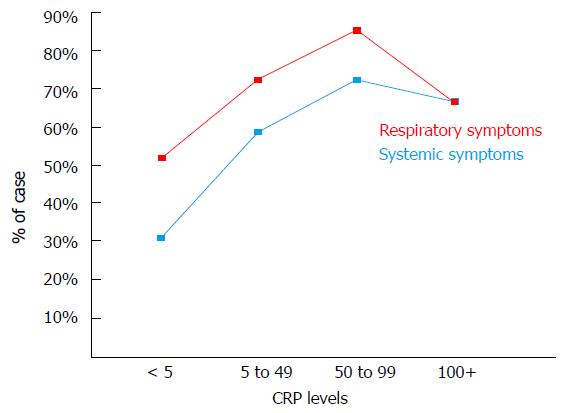
Fifty point four percent had both respiratory and systemic symptoms whereas 24.8% had respiratory symptoms alone. The remainder (24.8%) had no respiratory symptoms and CRP and chest radiograph were performed for investigation of fever. CRP levels were significantly higher in patients with systemic symptoms (68.6 ± 86.2 mg/L vs 32.7 ± 55.2 mg/L) (P < 0.01). Patients who were seen initially in the ED had statistically significant lower CRP readings (28.5 ± 38.6 mg/L) than inpatients (57.8 ± 66.0 mg/L) (P < 0.001) or outpatients (74.6 ± 108.6 mg/L) (P < 0.001). This could reflect lower threshold for performance of chest radiography in the ED setting.
Serum white cell count (WCC) (normal range: 4-11 × 109/L) ranged from 3.1-55.6 × 109/L, with a mean of 13.9 ± 7.2 × 109/L. Serum neutrophil levels (normal range: 1.8-8 × 109/L) ranged from 0.6 to 38.1 × 109/L with a mean of 8.2 ± 5.7 × 109/L. There was no significant difference in WCC or neutrophil counts between inpatient, outpatients and ED patients. CRP levels correlated positively and strongly with WCC and neutrophil counts (P < 0.001).
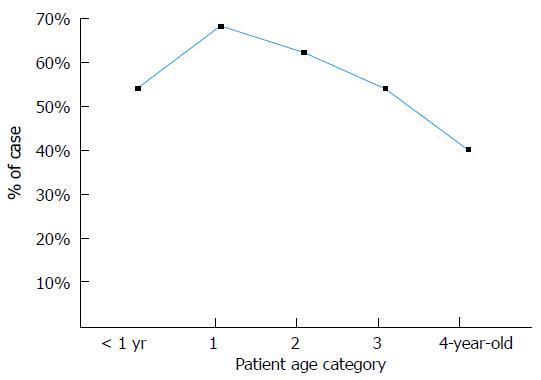
Fifty-eight point five percent of all chest radiographs were abnormal and abnormal findings were most frequently encountered in 1-year-old patients (68.5%) (Figure 2). Abnormal chest radiograph findings were significantly more common in patients with elevated CRP levels (P < 0.01) (Figure 3). However, when patients were sub-grouped according to their age it was found that an elevated CRP level was significantly predictive of an abnormal findings on chest radiography in patients greater than 1 year of age (P < 0.01) but was not predictive of an abnormal chest radiograph in patients aged less than 1 year of age (P = 0.56). It is worth noting that a CRP of > 100 mg/L was less predictive of an abnormal chest radiograph than a CRP level of 55-99 mg/L (Figure 3). This was especially true in patients under one year of age where only 37.5% of chest radiographs were positive when the CRP exceeded 100 mg/L (Figure 4). Interestingly WCC and neutrophil counts were not predictive of an abnormal chest radiograph across the entire cohort or in sub-groups aged less than or greater than 1 year.
The presence of respiratory symptoms (cough, wheeze, tachypnea, respiratory distress, dyspnoea) was more predictive of an abnormal chest radiograph than systemic symptoms alone (Figure 5). Infants aged less than one year with both respiratory symptoms and elevated CRP levels of 50-99 mg/L, were significantly more likely to have an abnormal chest radiograph (P < 0.01) (Figure 5). The combination of these 2 elements yielded a positive predictive value (PPV) of 62% for an abnormal chest radiograph whereas the absence of either had a negative predictive value (NPV) of 62%. Those aged 1-4 years presenting with both respiratory symptoms and a CRP of 50-99 mg/L had a PPV of 64% for an abnormal chest radiograph and the absence of either yielded a NPV of 75% for chest radiograph findings.
The major finding of our study is that abnormal chest radiograph findings were significantly more common in patients with elevated CRP levels. This finding suggests that CRP levels may predict findings on chest radiographs in infants with suspected LRTI. A CRP range of 50-99 mg/L was most predictive of an abnormal chest radiograph. We also found that patients who were less than 1 year frequently have normal chest radiographs in the presence of CRP level elevations above 100 mg/L. This finding may be explained by the fact that the presenting complaints of patients aged less than 1 year may often be non-specific and possibly that those aged less than one year have an increased likelihood of having other possible infectious pathologies such as gastroenteritis or urinary tract infection, which are both common in this age group. The presence of respiratory symptoms was, as expected, a predictor of positive chest radiograph findings along with systemic symptoms. Patients aged greater than 1 year were also more likely to yield a finding on chest radiograph.
A single prospective case control study by Almirall et al[12] of patients greater than 14 years complements our own results by finding that CRP was an independent predictor of LRTI. It concluded that a serum CRP level > 33 mg/L can differentiate patients with true alveolar infection from patients with LRTI other than pneumonia. In our study, patients with a CRP of > 33 mg/L had a 68.2% likelihood of an abnormal chest radiograph, as opposed to a 24.7% chance of a normal radiograph. A CRP level of < 33 mg/L in children aged 1 to 4 had an NPV of 50% in predicting a normal chest radiograph. Almirall et al[12] also found that patients requiring inpatient care had higher CRP levels than outpatients and that CRP levels varied significantly with patient age in keeping with our findings.
In another study involving the adult population, Hopstaken et al[7] found that both ESR and CRP had a higher odds ratio at predicting pneumonia than clinical signs alone and therefore concluded that CRP along with clinical signs had sufficient sensitivity to predict the presence of LRTI. The authors of that study advise that it may be possible to safely withhold antibiotic treatment in adult patients with a CRP value of < 20 mg/L among other criteria. Again, this complements our findings in a pediatric setting, which suggest that a normal CRP may negate the need for chest radiography in patients aged 1 to 4, particularly in the absence of respiratory symptoms. Chest radiograph omission would have a beneficial impact in terms of radiation dose reduction to infants and their parents, workload reduction for radiographers/radiology technicians in a cohort of patients in which chest radiography can be challenging, decreased stress to sick infants and reduced economic costs.
Numerous previous studies examined the utility of non-specific inflammatory markers such as CRP and findings on chest radiographs in determining the nature of the infectious pathogen responsible for LRTI. These studies found little or no value of CRP levels or chest radiograph findings in the differentiation between bacterial and viral pneumonia[4,5,10,11]. As a result of these previous studies, attempts at differentiating between viral and bacterial pathogens was not undertaken in our study.
The issue of investigation and management of community-acquired pneumonia (CAP) in children has been extensively investigated recently. Recent studies, including a study by Neuman et al[13], have investigated the use of investigations including chest radiography and subsequent management of children presenting to hospital with CAP. The study investigated a mean of 375000 ED visits for CAP annually, during the study period from 2001-2009. Among children discharged from EDs with CAP, full blood count was performed during 30% of visits, chest radiography during 83%, and viral testing in only 13%[13]. A recommendation from the study was that efforts should be made to reduce the performance of certain diagnostic testing, such as a full blood count and chest radiography[13]. Anther very recent study by Florin et al[14] examined variability across hospitals in diagnostic test utilisation for children diagnosed with CAP during ED evaluation and to determine if test utilisation is associated with hospitalisation and ED revisits. This study analysed a total of 100615 ED visits were analysed. Full blood count (28.7%), blood culture (27.9%), and chest radiograph (75.7%) were the most commonly ordered ED diagnostic tests. There was significant variation in the utilisation of these investigations between hospitals. An interesting finding was that hospitals, which had increased rates of utilisation of these investigations, had increased likelihood of hospital admission compared to hospitals that utilised these investigations less frequently. However, ED revisits between the low- and high-utilising hospitals were not significant. The study concluded that an opportunity exists to reduce diagnostic testing for CAP without negatively affecting outcomes[14]. Recently, the Pediatric Infectious Diseases Society, have published guidelines on the management of CAP in infants and children older than 3 mo of age[15]. These guidelines suggest that routine chest radiographs are not necessary for the confirmation of suspected CAP in patients well enough to be treated in the outpatient setting and that chest radiography (posteroanterior and lateral) should only be obtained in children with suspected or documented hypoxemia or significant respiratory distress and in those with failed initial antibiotic therapy, to verify the presence or absence of complications of pneumonia, including parapneumonic effusions, necrotising pneumonia, and pneumothorax[15]. The findings of our study would suggest that serum CRP levels may play a role in guiding the decision of whether to perform or not perform a chest radiograph in this setting.
Limitations of our study include the retrospective design and that reviewers retrospectively analysed chest radiograph reports and findings. Prospective data collection may be more applicable in normal clinical practice than double or consensus read interpretations. Although CRP elevation is a useful biomarker for infection in the immunocompromised patient[16], we did not attempt to identify and separate individuals who might be particularly at risk of complications from a respiratory tract infection (such as those with immunodeficiency) and we cannot confidently state that our findings apply to children with a known history of immunodeficiency or malignancy. Ideally, further studies in a larger cohort of patients should be considered to evaluate the role of CRP in the triage and justification of chest radiography in the diagnosis and follow-up of LRTI in the infant population.
In conclusion, this study found that abnormal chest radiograph findings were significantly more common in patients with elevated CRP levels. Young children are most likely to have abnormal chest radiograph findings if they have all three of the following; a CRP level of 50-99 mg/L, respiratory symptoms and if they are aged greater than 1 year. We found no association between an abnormal chest radiograph and elevated WCC and neutrophil count.
There is an on-going and laudable drive to lower patient exposure to ionising radiation whenever possible. This is especially true when dealing with infants and young children who are at higher risk of malignancy from ionising radiation exposure. The authors acknowledge that the radiation exposure associated with chest radiography is very low. There is however, also the issue of cost associated with performance of unnecessary radiological tests and also the issue of stress to patient and parents of performing radiological examinations in infants and young children. For those reasons, the performance of radiological studies should be limited to clinical situations where it will aid diagnosis or alter management in a young patient cohort. The authors undertook a retrospective study to examine the relationship between serum C-reactive protein (CRP) levels to abnormal findings on chest radiographs to ascertain if raised CRP levels could predict abnormal chest radiograph findings.
A previous study in adults had shown that low CRP levels could help predict those that require antibiotic treatment for lower respiratory tract infection. No previous studies have looked at using CRP levels in a pediatric population to predict those that may or may not require chest radiography.
The results of this study found that children aged between 1-4 with an elevated CRP were significantly more likely to have an abnormal chest radiograph. Conversely, the negative predictive value of a normal CRP in a patient with respiratory symptoms or a raised CRP without respiratory symptoms in this age group was 75%.
The authors’ findings may help guide clinicians regarding the need to perform chest imaging when dealing with a child presenting with respiratory symptoms but without hypoxaemia or severe respiratory distress. The ultimate goal being the reduction of unnecessary ionising radiation exposure and reducing cost and potential stress to young patients and their parents.
CRP is an acute phase protein released into the blood stream from the liver under the influence of circulating interleukin-6, secreted by T-cell and macrophages. It is used as a marker for inflammation.
The authors investigated CRP and radiographic findings of lower respiratory tract infection in infants. It is a well written paper.
Manuscript source: Unsolicited manuscript
Specialty type: Radiology, nuclear medicine and medical imaging
Country of origin: Ireland
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Gao BL, Gumustas OG, van Beek S- Editor: Gong XM L- Editor: A E- Editor: Wu HL
| 1. | Bartley K, Metayer C, Selvin S, Ducore J, Buffler P. Diagnostic X-rays and risk of childhood leukaemia. Int J Epidemiol. 2010;39:1628-1637. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 86] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 2. | Brenner DJ, Hall EJ. Computed tomography--an increasing source of radiation exposure. N Engl J Med. 2007;357:2277-2284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6212] [Cited by in RCA: 5789] [Article Influence: 321.6] [Reference Citation Analysis (3)] |
| 3. | Pearce MS, Salotti JA, Little MP, McHugh K, Lee C, Kim KP, Howe NL, Ronckers CM, Rajaraman P, Sir Craft AW. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet. 2012;380:499-505. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2528] [Cited by in RCA: 2629] [Article Influence: 202.2] [Reference Citation Analysis (1)] |
| 4. | Clark JE, Hammal D, Spencer D, Hampton F. Children with pneumonia: how do they present and how are they managed? Arch Dis Child. 2007;92:394-398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 37] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 5. | Don M, Valent F, Korppi M, Canciani M. Differentiation of bacterial and viral community-acquired pneumonia in children. Pediatr Int. 2009;51:91-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 72] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 6. | Esposito S, Bosis S, Cavagna R, Faelli N, Begliatti E, Marchisio P, Blasi F, Bianchi C, Principi N. Characteristics of Streptococcus pneumoniae and atypical bacterial infections in children 2-5 years of age with community-acquired pneumonia. Clin Infect Dis. 2002;35:1345-1352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 73] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 7. | Hopstaken RM, Muris JW, Knottnerus JA, Kester AD, Rinkens PE, Dinant GJ. Contributions of symptoms, signs, erythrocyte sedimentation rate, and C-reactive protein to a diagnosis of pneumonia in acute lower respiratory tract infection. Br J Gen Pract. 2003;53:358-364. [PubMed] |
| 8. | Korppi M, Heiskanen-Kosma T, Leinonen M. White blood cells, C-reactive protein and erythrocyte sedimentation rate in pneumococcal pneumonia in children. Eur Respir J. 1997;10:1125-1129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 102] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 9. | Korppi M. Non-specific host response markers in the differentiation between pneumococcal and viral pneumonia: what is the most accurate combination? Pediatr Int. 2004;46:545-550. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 57] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 10. | Nohynek H, Valkeila E, Leinonen M, Eskola J. Erythrocyte sedimentation rate, white blood cell count and serum C-reactive protein in assessing etiologic diagnosis of acute lower respiratory infections in children. Pediatr Infect Dis J. 1995;14:484-490. [PubMed] |
| 11. | Virkki R, Juven T, Rikalainen H, Svedström E, Mertsola J, Ruuskanen O. Differentiation of bacterial and viral pneumonia in children. Thorax. 2002;57:438-441. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 231] [Cited by in RCA: 209] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 12. | Almirall J, Bolíbar I, Toran P, Pera G, Boquet X, Balanzó X, Sauca G. Contribution of C-reactive protein to the diagnosis and assessment of severity of community-acquired pneumonia. Chest. 2004;125:1335-1342. [PubMed] |
| 13. | Neuman MI, Shah SS, Shapiro DJ, Hersh AL. Emergency department management of childhood pneumonia in the United States prior to publication of national guidelines. Acad Emerg Med. 2013;20:240-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 45] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 14. | Florin TA, French B, Zorc JJ, Alpern ER, Shah SS. Variation in emergency department diagnostic testing and disposition outcomes in pneumonia. Pediatrics. 2013;132:237-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 119] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 15. | Bradley JS, Byington CL, Shah SS, Alverson B, Carter ER, Harrison C, Kaplan SL, Mace SE, McCracken GH, Moore MR. The management of community-acquired pneumonia in infants and children older than 3 months of age: clinical practice guidelines by the Pediatric Infectious Diseases Society and the Infectious Diseases Society of America. Clin Infect Dis. 2011;53:e25-e76. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1086] [Cited by in RCA: 1076] [Article Influence: 76.9] [Reference Citation Analysis (0)] |
| 16. | Pepys MB, Hirschfield GM. C-reactive protein: a critical update. J Clin Invest. 2003;111:1805-1812. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 1211] [Article Influence: 55.0] [Reference Citation Analysis (2)] |