Published online Mar 28, 2017. doi: 10.4329/wjr.v9.i3.126
Peer-review started: August 24, 2016
First decision: October 20, 2016
Revised: December 12, 2016
Accepted: January 2, 2017
Article in press: January 3, 2017
Published online: March 28, 2017
Processing time: 212 Days and 3.8 Hours
To determine diagnostic performance of magnetic resonance arthrography (MRA) in evaluating rotator cuff tears (RCTs) using Snyder’s classification for reporting.
One hundred and twenty-six patients (64 males, 62 females; median age 55 years) underwent shoulder MRA and arthroscopy, which represented our reference standard. Surgical arthroscopic reports were reviewed and the reported Snyder’s classification was recorded. MRA examinations were evaluated by two independent radiologists (14 and 5 years’ experience) using Snyder’s classification system, blinded to arthroscopy. Agreement between arthroscopy and MRA on partial- and full-thickness tears was calculated, first regardless of their extent. Then, analysis took into account also the extent of the tear. Interobserver agreement was also calculated the quadratically-weighted Cohen kappa statistics.
On arthroscopy, 71/126 patients (56%) had a full-thickness RCT. The remaining 55/126 patients (44%) had a partial-thickness RCT. Regardless of tear extent, out of 71 patients with arthroscopically-confirmed full-thickness RCTs, 66 (93%) were correctly scored by both readers. All 55 patients with arthroscopic diagnosis of partial-thickness RCT were correctly assigned as having a partial-thickness RCT at MRA by both readers. Interobserver reproducibility analysis showed total agreement between the two readers in distinguishing partial-thickness from full-thickness RCTs, regardless of tear extent (k = 1.000). With regard to tear extent, in patients in whom a complete tear was correctly diagnosed, correct tear extent was detected in 61/66 cases (92%); in the remaining 5/66 cases (8%), tear extent was underestimated. Agreement was k = 0.955. Interobserver agreement was total (k = 1.000).
MRA shows high diagnostic accuracy and reproducibility in evaluating RCTs using the Snyder’s classification for reporting. Snyder’s classification may be adopted for routine reporting of MRA.
Core tip: In the present study we determined the diagnostic performance of magnetic resonance arthrography (MRA) in evaluating rotator cuff tears (RCTs) using Snyder’s classification for reporting. One hundred and twenty-six patients underwent MRA and arthroscopy, which represented our reference standard. Agreement between arthroscopy and MRA on partial- and full-thickness tears was calculated. Arthroscopy findings: 71/126 patients (56%) had a full-thickness RCTs, while 55/126 patients (44%) had a partial-thickness RCTs. MRA showed high diagnostic accuracy and reproducibility in evaluating RCTs using the Snyder’s classification for reporting. Snyder’s classification may be adopted for routine reporting of MRA.
- Citation: Aliprandi A, Messina C, Arrigoni P, Bandirali M, Di Leo G, Longo S, Magnani S, Mattiuz C, Randelli F, Sdao S, Sardanelli F, Sconfienza LM, Randelli P. Reporting rotator cuff tears on magnetic resonance arthrography using the Snyder’s arthroscopic classification. World J Radiol 2017; 9(3): 126-133
- URL: https://www.wjgnet.com/1949-8470/full/v9/i3/126.htm
- DOI: https://dx.doi.org/10.4329/wjr.v9.i3.126
The shoulder joint is a complex anatomic structure consisting of static and dynamic stabilizers, which confers functional stability and high degree of mobility at the same time[1]. Rotator cuff (RC) acts as a dynamic stabilizer contributing to shoulder stability: It consists of four muscles (supraspinatus, subscapularis, infraspinatus and teres minor), which tendons fuse to form a continuous structure near their insertions. Together with long head of biceps tendon, RC tendons create an ideal configuration to actively compress the humeral head into the glenoid’s cavity[2]. Nevertheless, due to the glenohumeral joint high-grade of mobility, RC tears (RCTs) are commonly encountered, implying shoulder pain and dysfunction, often associated with loss of biomechanical balance and instability and subacromial impingement[3,4]. The prevalence of full-thickness RCTs is almost 25% of individuals in their 60s and 50% of individuals in their 80s, with the supraspinatus being the most frequently involved tendon[5].
Both ultrasound and magnetic resonance imaging (MRI) are accurate techniques in identifying shoulder pathologic conditions and RCTs[6,7]. Magnetic resonance arthrography (MRA) has been shown to improve diagnostic performance of conventional MRI, as contrast material distends the joint capsule and outlines intra-articular structures; thus, MRA is particularly useful for RC partial-thickness tears as well as labrum and glenohumeral ligament tears and degeneration[7,8].
Several orthopaedic classifications of RCTs were proposed throughout years. In 1934, Codman[9] described the development of supraspinatus partial-thickness tears. In 1983, Neer[10] classified RCTs into three progressive stages of impingement. In 1984, DeOrio and Cofield[11] used the length of the greatest diameter of the tear to categorize the tear in four degrees. In 1990, Ellman[12] further developed the classification of Neer, popularizing for the first time a system to classify partial thickness tears based on intra-operative findings. Recently, Davidson and Burkhart[13] developed a geometric classification system based on pre-operative (MRI)[14]. At our institution, shoulder orthopaedic surgeons use the Snyder’s arthroscopic classification of RCTs, which includes three parameters: The location of the lesion, the extent of the lesion, i.e., partial-thickness or full-thickness - and the number of involved tendons (Table 1)[15,16]. In particular, Snyder’s classification separates RCTs into articular-sided, bursal-sided, and complete tears.
| Location | |
| A | Articular side |
| B | Bursal side |
| C | Full-thickness tears, connecting A and B sides |
| Severity of partial tears (A and B side) | |
| 0 | Normal cuff, with smooth coverings of synovium and bursa |
| 1 | Minimal, superficial bursal or synovial irritation or slight capsular fraying in a small, localized area; usually < 1 cm |
| 2 | Actually fraying and failure of some rotator cuff fibres in addition to synovial, bursal, or capsular injury; usually < 2 cm |
| 3 | More severe rotator cuff injury, including fraying and fragmentation of tendons fibers, often involving the whole surface of a cuff tendon; usually < 3 cm |
| 4 | Very severe partial rotator cuff tear that usually contains, in addition to fraying and fragmentation of tendon tissue, a sizable flap tear and often encompasses more than a single tendon |
| Severity of complete tears (C) | |
| 1 | Small, complete tear, such as a puncture wound |
| 2 | Moderate tear, (usually < 2 cm) that still encompasses only one of the rotator cuff tendons with no retraction of the torn ends |
| 3 | Large, complete tear involving an entire tendon with minimal retraction of the torn edge; usually 3 to 4 cm |
| 4 | Massive rotator cuff tear involving two or more rotator cuff tendons, frequently with associated retraction and scarring of the remaining tendon |
Despite many orthopaedic classifications, these never entered into radiological practice and radiologists still descriptively report tears of the RC[17]. A recent study from Bosmans et al[18] showed that, although radiology report remains an indispensable tool for medical practice, there is still a consistent percentage of referring physicians that remains unsatisfied with them. In fact, communication is a critical aspect when providing medical care, and a discrepancy in the language used between physicians (i.e., radiologists and orthopaedic surgeons) may not convey the correct message and generate confusion[19]. Thus, the aim of our study was to evaluate the diagnostic performance of MRA in evaluating RCTs using the Snyder’s classification system for reporting MRA findings, having arthroscopy as reference standard.
This retrospective study was reviewed and approved by the Institutional Review Board (Comitato Etico ASL Milano Due) and patients’ informed consent was waived. Between June 2006 and December 2013, a series of 1324 consecutive shoulder MRA were performed at our institution in patients presenting with pain and functional limitation of the shoulder. From this database, we selected all patients who underwent arthroscopic surgery at our Institution, for a total of 126 patients (64 males and 62 females; age range 15-79 years; median age 55 years; 25th-75th percentile 38-63 years). Inclusion criteria for the study were: (1) MRA performed at our Institution following a standardised protocol; and (2) surgery performed at our Institution.
Intra-articular injection of contrast agent was performed under ultrasound-guidance using a high frequency probe with anterior approach, as described by Sconfienza et al[20] and Messina et al[21]. Patients were positioned supine with the shoulder under investigation slightly extra-rotated, with the arm outstretched along the body. After careful skin disinfection, a 19-G needle was introduced in the joint and contrast material was injected. The procedure ended after injection of up to 20 mL of 0.0025 mmol/mL of gadoterate meglumine (Gd-DOTA, Dotarem pre-filled syringes; Guerbet, Paris, France). After injection, patient’s arm was gently intra and extra-rotated for better contrast distribution into the joint capsule.
MRA was performed within 10 min from contrast agent injection using a 1.5-T system (Magnetom Sonata Maestro Class, Siemens Medical Solution, Erlangen, Germany) equipped with a 40 mT/m gradient power and a dedicated phased-array surface coil. The following imaging protocol was acquired: 3 plane (axial, coronal oblique and sagittal oblique) turbo spin-echo T1-weighted fat-saturated sequences (TR/TE = 763/15 ms; slice thickness = 4 mm; FOV = 190 mm × 190 mm; matrix = 256 × 256); oblique coronal turbo spin-echo T2-weighted fat-saturated sequences (TR/TE = 4000/74 ms; slice thickness = 4 mm with 0.8-mm interslice gap; FOV = 240 mm × 240 mm; matrix = 256 × 256); three-timensional dual echo steady state (3D-DESS, TR/TE = 17/6 ms, slice thickness = 0.8 mm, voxel = 0.8 mm × 0.8 mm × 0.8 mm).
As a pilot attempt to classify RCTs using Snyder’s classification, in the present study we only considered RCTs involving the supraspinatus tendon. The Snyder’s arthroscopic classification (Table 1) was used as reference for evaluating complete tears. For partial-thickness tears, the Snyder’s classification was modified according to what reported in Table 2. Images were reviewed by two independent radiologists with 14 (reader 1) and 5 years’ (reader 2) experience in musculoskeletal MRA, respectively, blinded to arthroscopic findings.
| Lesion's grade | Severity of partial tears (A or B lesion) |
| 1 | Subtle irregularities of the tendon surface with preserved thickness |
| 2 | Major irregularities of the tendon surface with preserved thickness |
| 3 | Lesions involve less than 50% of tendon diameter and lesion extension is less than 3 cm |
| 4 | Lesions involve more than 50% of tendon's diameter with an extension of more than 3 cm or the lesion involves two tendons |
Arthroscopy was performed by one of three orthopaedic surgeons with 5 to 17 years’ experience in shoulder arthroscopy. Surgical reports were reviewed and the reported Snyder’s classification was recorded.
For analysis of lesion extent accuracy, data obtained by the most experiences reader (reader 1) was used and compared to reference standard. We calculated first the agreement between arthroscopy and MRA on partial- and full-thickness tears, regardless of their extent. Then, we performed a deeper analysis taking into account also the extent of the tear, still separately for partial- and full-thickness tears. Interobserver agreement was also calculated the quadratically-weighted Cohen kappa statistics was used.
Arthroscopy was performed after a median of 137 d from MRA (25th-75th percentile 72-211 d). At arthroscopic assessment, 71/126 patients (56%) had a full-thickness RCT with different severity grade: C1, n = 27; C2, n = 25; C3, n = 15; C4, n = 4. The remaining 55/126 patients (44%) had a partial-thickness RCT. Distribution of the articular and bursal location of the tear is reported in Table 3 according to the most experienced reader (reader 1).
| Articular side tear | ||||||
| A0 | A1 | A2 | A3 | A4 | ||
| Bursal side tear | B0 | - | 1 | 1 | 2 | 1 |
| B1 | 3 | 8 | 0 | 0 | 0 | |
| B2 | 4 | 5 | 5 | 3 | 1 | |
| B3 | 0 | 0 | 1 | 5 | 2 | |
| B4 | 0 | 0 | 0 | 1 | 12 | |
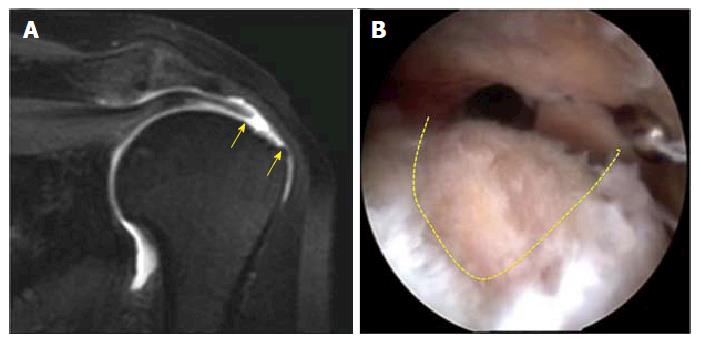
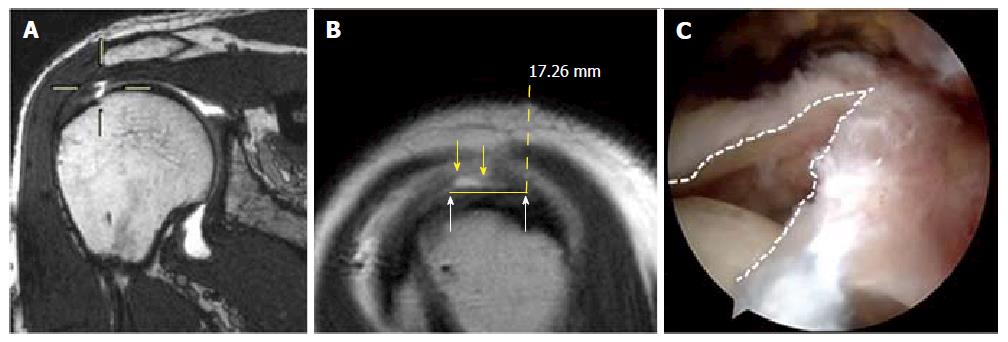
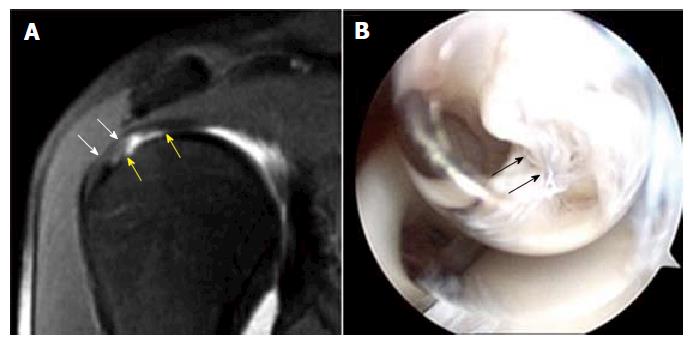
Out of 71 patients with arthroscopically-confirmed full-thickness RCTs, 66 (93%) were correctly scored by both readers; in the remaining 5 patients (7%), both readers assigned a partial-thickness tear instead of a full-thickness tear. Table 4 shows data about the 5 patients with a complete tear at arthroscopy who were assigned with a partial score by the most experienced reader (reader 1). Figures 1-3 show MRA findings and corresponding arthroscopic confirmation.
| Reader 1 | Reference standard | |
| Articular side | Bursal side | Complete tear |
| A 2 | B 1 | C 1 |
| A 3 | B 4 | C 1 |
| A 2 | B 3 | C 1 |
| A 4 | B 4 | C 1 |
| A 4 | B 4 | C 1 |
All 55 patients with arthroscopic diagnosis of partial-thickness tear were correctly assigned as having a partial-thickness tear at MRA by both readers (Figure 3).
Interobserver reproducibility analysis showed total agreement between the two readers in distinguishing partial-thickness from full-thickness RCTs, regardless of tear extent (k = 1.000).
In patients in whom a complete tear was correctly diagnosed, correct tear extent was detected in 61/66 cases (92%); in the remaining 5/66 cases (8%), tear extent was underestimated, as both readers assigned C1 instead of C2. Agreement with arthroscopy was k = 0.955. Interobserver agreement was total (k = 1.000).
In 55 patients in whom a partial-thickness tear was diagnosed, agreement in terms of tear extent was k = 0.878 for the articular side and k = 0.837 for the bursal side, respectively. Full data are reported in Tables 5 and 6, respectively. Regarding interobserver agreement, the two readers disagreed at maximum for 1 degree for either articular or bursal side of the supraspinatus tendon, with k = 0.947 and k = 0.969, respectively.
| Reader 1 | ||||||
| A0 | A1 | A2 | A3 | A4 | ||
| Arthroscopy | A0 | 7 | 0 | 0 | 0 | 0 |
| A1 | 8 | 6 | 0 | 0 | 0 | |
| A2 | 2 | 2 | 3 | 0 | 0 | |
| A3 | 0 | 0 | 4 | 7 | 0 | |
| A4 | 0 | 0 | 0 | 8 | 8 | |
| Reader 1 | ||||||
| B0 | B1 | B2 | B3 | B4 | ||
| Arthroscopy | B0 | 5 | 0 | 0 | 0 | 0 |
| B1 | 7 | 4 | 0 | 0 | 0 | |
| B2 | 4 | 7 | 7 | 0 | 0 | |
| B3 | 0 | 0 | 3 | 5 | 0 | |
| B4 | 0 | 0 | 0 | 3 | 10 | |
When managing a patient affected with a RCT, both clinical and imaging evaluation play a crucial role[22]. The role of diagnostic imaging is to help in the choice between surgical or nonsurgical treatment. Ultrasound, unenhanced MR and MRA have become the most common imaging techniques by which a RCT is diagnosed. Ultrasound is as accurate as unenhanced MR, but MRA remains the most sensitive and specific technique and is generally performed in cases in which ultrasound and unenhanced MR are not definitive[7].
The use of a common RCTs classification by radiologists and orthopaedists may allow for a more direct comparison, leading to better clinical diagnosis and letting the patient to decide a treatment option with clearer information. Snyder proposed a classification system for the evaluation of RCTs measuring both their extent and number of tendons involved, providing indications for surgery or conservative treatment on the basis of the obtained score[16]. In the present study we adopted the Snyder’s classification as it was already successfully used by orthopaedics surgeons at our Institution, as a tentative to achieve a better communication with them.
In our study we found a high agreement in diagnosing RCTs for both radiologists having arthroscopy as reference standards. These results are in line with what is already reported in a recent systematic review about the accuracy of MRA in diagnosing RCTs using conventional descriptive reporting systems[23]. Moreover, we found a very high interobserver reproducibility between the two readers, with a perfect agreement for full-thickness RCTs; regarding partial-thickness RCTs, the two readers rarely disagreed. This means that also the less experienced reader showed a very good diagnostic performance. As a consequence, we can think that the Snyder’s classification system may have a value also when used in reporting MRA, even though originally created for arthroscopy.
A deeper analysis of the results showed that radiologists tend to underestimate the damage of the tendon, for both full-thickness and partial-thickness RCTs. This data deserves some considerations. The margins of a tendon tear are usually made by degenerated tendon matrix. During arthroscopy, the orthopaedic surgeon debrides the degenerated area to have more consistent margins for repair[24]. Thus, final evaluation of tear extent by the orthopaedic surgeon may be larger compared to what previously seen on MRA.
Regarding partial-thickness RCTs, reproducibility of MRA is still high but lower than for full-thickness RCTs. This was expected, as it is known that both MRI and MRA have higher performance in assessing the full-thickness RCTs rather than partial-thickness RCTs[25-27]. However, the difference between the radiologist and the arthroscopy was only 1 degree in the majority of cases and 2 degrees in a few patients: These discrepancies are expected to not affect significantly the patients’ management[28]. Moreover, similarly to what happens for full-thickness RCTs, the radiologist always tends to underestimate the lesion degree of partial RCTs. Again, the main reason for this underestimation may be related to the fact that partial-tear tendon debridement procedure could be performed by the surgeon on wider area of the tendon, with a consequent extension of the Snyder’s arthroscopic score[28]. Overall, we should also consider the time elapsed from MRA to surgery (median delay 137 d) which could represent a factor for progression of mild damage of the tendon. It is known that tendon injuries, if left untreated, can progress by determining the transition from small partial injury to a greater degree and from partial to complete tears[29].
This study has some limitations. First, it was performed retrospectively. Second, arthroscopy was performed by several orthopaedic surgeons with different experience in RCTs repair. Thus, certain degree of variability in RCTs scoring at the reference standard may be expected and may have slightly influenced our results. The same can be said for the delay between MRA and arthroscopy, which limited the reliability of the reference standard. In fact, the median delay of 137 d between MRA and arthroscopy could be seen as a long time between the two exams; nevertheless, this kind of delays may be common in everyday hospital practice, as patients usually attempt conservative treatments before undergoing surgery.
In conclusion, our study demonstrates high reproducibility of MRA in evaluating RCTs using the Snyder’s classification as a method for reporting. This allows to conclude that not only MRA but also the Snyder’s classification has an intrinsic high diagnostic value. Even though originally created for arthroscopy, Snyder’s classification is well suitable and may be adopted for routine reporting of MRA.
The shoulder joint is a complex anatomic structure consisting of static and dynamic stabilizers, which confers functional stability and high degree of mobility at the same time. Rotator cuff acts as a dynamic stabilizer contributing to shoulder stability. Rotator cuff tears (RCTs) are commonly encountered, implying shoulder pain and dysfunction, often associated with loss of biomechanical balance and instability and subacromial impingement.
Magnetic resonance arthrography (MRA) is particularly useful for rotator cuff partial-thickness tears as well as labrum and glenohumeral ligament tears and degeneration. Several orthopaedic classifications of RCTs were proposed throughout years; At the authors’ institution, shoulder orthopaedic surgeons use the Snyder’s arthroscopic classification of RCTs, which includes three parameters: The location of the lesion, the extent of the lesion - and the number of involved tendons.
Despite many orthopaedic classifications, these never entered into radiological practice and radiologists still descriptively report tears of the RC, with referring physicians that may remains unsatisfied with them. The authors evaluated the diagnostic performance of MRA in evaluating RCTs using the Snyder’s classification system for reporting MRA findings, evaluating its accuracy using arthroscopy as reference standard.
MRA showed high diagnostic accuracy and reproducibility in evaluating RCTs using the Snyder’s classification for reporting. Snyder’s classification may be adopted for routine reporting of MRA.
MRA is an examination of magnetic resonance imaging that is performed after the injection of contrast material (gadolinium) into the joint, with the aim to increase its diagnostic performance. RCTs may involve the articular or bursal side, and can be classified as partial or complete according to thickness tendon involvement.
The authors evaluate the diagnostic performance of MRA in evaluating RCTs using the Snyder’s classification system for reporting MRA findings, evaluating its accuracy using arthroscopy as reference standard. They demonstrated high reproducibility of MRA in evaluating RCTs using the Snyder’s classification as a method for reporting.
Manuscript source: Invited manuscript
Specialty type: Radiology, nuclear medicine and medical imaging
Country of origin: Italy
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Gao BL, Li YZ S- Editor: Gong XM L- Editor: A E- Editor: Li D
| 1. | Huegel J, Williams AA, Soslowsky LJ. Rotator cuff biology and biomechanics: a review of normal and pathological conditions. Curr Rheumatol Rep. 2015;17:476. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 55] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 2. | Longo UG, Berton A, Papapietro N, Maffulli N, Denaro V. Biomechanics of the rotator cuff: European perspective [Internet]. In: Rotator Cuff Tear. 2011. [cited 2016; Aug 17] Available from: http://www.ncbi.nlm.nih.gov/pubmed/21986041. |
| 3. | Gombera MM, Sekiya JK. Rotator cuff tear and glenohumeral instability : a systematic review. Clin Orthop Relat Res. 2014;472:2448-2456. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 99] [Cited by in RCA: 78] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 4. | Longo S, Corradi A, Michielon G, Sardanelli F, Sconfienza LM. Ultrasound evaluation of the subacromial space in healthy subjects performing three different positions of shoulder abduction in both loaded and unloaded conditions. Phys Ther Sport. 2016; Aug 12; Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Tashjian RZ. Epidemiology, natural history, and indications for treatment of rotator cuff tears. Clin Sports Med. 2012;31:589-604. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 328] [Cited by in RCA: 447] [Article Influence: 34.4] [Reference Citation Analysis (0)] |
| 6. | Corazza A, Orlandi D, Fabbro E, Ferrero G, Messina C, Sartoris R, Perugin Bernardi S, Arcidiacono A, Silvestri E, Sconfienza LM. Dynamic high-resolution ultrasound of the shoulder: how we do it. Eur J Radiol. 2015;84:266-277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 44] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 7. | de Jesus JO, Parker L, Frangos AJ, Nazarian LN. Accuracy of MRI, MR arthrography, and ultrasound in the diagnosis of rotator cuff tears: a meta-analysis. AJR Am J Roentgenol. 2009;192:1701-1707. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 410] [Cited by in RCA: 430] [Article Influence: 26.9] [Reference Citation Analysis (0)] |
| 8. | Hodler J, Kursunoglu-Brahme S, Snyder SJ, Cervilla V, Karzel RP, Schweitzer ME, Flannigan BD, Resnick D. Rotator cuff disease: assessment with MR arthrography versus standard MR imaging in 36 patients with arthroscopic confirmation. Radiology. 1992;182:431-436. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 184] [Cited by in RCA: 154] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 9. | Codman EA. The shoulder: rupture of the supraspinatus tendon and other lesions in or about the subacromial bursa. Boston, United States: Thomas Todd 1934; 123-177. |
| 10. | Neer CS. Impingement lesions. Clin Orthop Relat Res. 1983;70-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 456] [Cited by in RCA: 366] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 11. | DeOrio JK, Cofield RH. Results of a second attempt at surgical repair of a failed initial rotator-cuff repair. J Bone Joint Surg Am. 1984;66:563-567. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 590] [Cited by in RCA: 634] [Article Influence: 15.5] [Reference Citation Analysis (0)] |
| 12. | Ellman H. Diagnosis and treatment of incomplete rotator cuff tears. Clin Orthop Relat Res. 1990;64-74. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 197] [Cited by in RCA: 169] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 13. | Davidson J, Burkhart SS. The geometric classification of rotator cuff tears: a system linking tear pattern to treatment and prognosis. Arthroscopy. 2010;26:417-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 152] [Cited by in RCA: 143] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 14. | Sconfienza LM, Orlandi D, Fabbro E, Ferrero G, Martini C, Savarino E, Silvestri E. Ultrasound assessment of the rotator cuff cable: comparison between young and elderly asymptomatic volunteers and interobserver reproducibility. Ultrasound Med Biol. 2012;38:35-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 15. | Snyder S. Arthroscopic classification of rotator cuff lesions and surgical decision making. Wilkins LW. Philadelphia: Shoulder Arthroscopy 2003; 201-207. |
| 16. | Millstein ES, Snyder SJ. Arthroscopic management of partial, full-thickness, and complex rotator cuff tears: indications, techniques, and complications. Arthroscopy. 2003;19 Suppl 1:189-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 52] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 17. | Robertson PL, Schweitzer ME, Mitchell DG, Schlesinger F, Epstein RE, Frieman BG, Fenlin JM. Rotator cuff disorders: interobserver and intraobserver variation in diagnosis with MR imaging. Radiology. 1995;194:831-835. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 88] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 18. | Bosmans JM, Weyler JJ, De Schepper AM, Parizel PM. The radiology report as seen by radiologists and referring clinicians: results of the COVER and ROVER surveys. Radiology. 2011;259:184-195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 167] [Cited by in RCA: 167] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 19. | Larson DB, Froehle CM, Johnson ND, Towbin AJ. Communication in diagnostic radiology: meeting the challenges of complexity. AJR Am J Roentgenol. 2014;203:957-964. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 43] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 20. | Sconfienza LM, Serafini G, Silvestri E. Ultrasound-guided musculoskeletal procedures - the upper limb. Milan, Italy: Springer-Verlag Mailand 2012; . |
| 21. | Messina C, Banfi G, Aliprandi A, Mauri G, Secchi F, Sardanelli F, Sconfienza LM. Ultrasound guidance to perform intra-articular injection of gadolinium-based contrast material for magnetic resonance arthrography as an alternative to fluoroscopy: the time is now. Eur Radiol. 2016;26:1221-1225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 46] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 22. | Lansdown DA, Feeley BT. Evaluation and treatment of rotator cuff tears. Phys Sportsmed. 2012;40:73-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 23. | Lenza M, Buchbinder R, Takwoingi Y, Johnston RV, Hanchard NC, Faloppa F. Magnetic resonance imaging, magnetic resonance arthrography and ultrasonography for assessing rotator cuff tears in people with shoulder pain for whom surgery is being considered. Cochrane Database Syst Rev. 2013;CD009020. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 97] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 24. | Castagna A, Borroni M, Garofalo R, Rose GD, Cesari E, Padua R, Conti M, Gumina S. Deep partial rotator cuff tear: transtendon repair or tear completion and repair? A randomized clinical trial. Knee Surg Sports Traumatol Arthrosc. 2015;23:460-463. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 43] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 25. | Aliprandi A, Sdao S, Cannaò PM, Khattak YJ, Longo S, Sconfienza LM, Sardanelli F. Imaging of shoulder pain in overhead throwing athletes. Sport Sci Health. 2013;9:81-88. [RCA] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 26. | Waldt S, Bruegel M, Mueller D, Holzapfel K, Imhoff AB, Rummeny EJ, Woertler K. Rotator cuff tears: assessment with MR arthrography in 275 patients with arthroscopic correlation. Eur Radiol. 2007;17:491-498. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 95] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 27. | Magee T, Shapiro M, Williams D. Comparison of high-field-strength versus low-field-strength MRI of the shoulder. AJR Am J Roentgenol. 2003;181:1211-1215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 42] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 28. | Fukuda H. The management of partial-thickness tears of the rotator cuff. J Bone Joint Surg Br. 2003;85:3-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 168] [Cited by in RCA: 152] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 29. | Yamanaka K, Matsumoto T. The joint side tear of the rotator cuff. A followup study by arthrography. Clin Orthop Relat Res. 1994;68-73. [PubMed] |