Published online Jul 28, 2016. doi: 10.4329/wjr.v8.i7.716
Peer-review started: March 7, 2016
First decision: April 15, 2016
Revised: April 16, 2016
Accepted: May 7, 2016
Article in press: May 9, 2016
Published online: July 28, 2016
Processing time: 141 Days and 21.5 Hours
Although intraoral radiographs still remain the imaging method of choice for the evaluation of endodontic patients, in recent years, the utilization of cone beam computed tomography (CBCT) in endodontics showed a significant jump. This case series presentation shows the importance of CBCT aided diagnosis and treatment of complex endodontic cases such as; root resorption, missed extra canal, fusion, oblique root fracture, non-diagnosed periapical pathology and horizontal root fracture. CBCT may be a useful diagnostic method in several endodontic cases where intraoral radiography and clinical examination alone are unable to provide sufficient information.
Core tip: The use of cone beam computed tomography in endodontics is increasing rapidly. Units with small field of views offering high-resolution images of teeth and related structures are specifically recommended in cases where two-dimensional systems fail to provide sufficient information. Future research should be directed towards developing units that offer higher-definition dental images with lower effective doses.
- Citation: Yılmaz F, Kamburoglu K, Yeta NY, Öztan MD. Cone beam computed tomography aided diagnosis and treatment of endodontic cases: Critical analysis. World J Radiol 2016; 8(7): 716-725
- URL: https://www.wjgnet.com/1949-8470/full/v8/i7/716.htm
- DOI: https://dx.doi.org/10.4329/wjr.v8.i7.716
Radiology has always been an important diagnostic tool in endodontic treatment. Intraoral imaging provides the highest spatial resolution of any imaging method currently available in clinical endodontics. However, since spatial information is lost when it is collapsed into a two-dimensional (2D) image, two or three intraoral radiographs taken from different angles are recommended in many cases. In addition, the diagnostic effectiveness of intraoral radiography is influenced by a number of variables, including beam angulation, exposure time, receptor sensitivity, processing, viewing and display conditions, superimposition of anatomic structures along with tooth and lesion location[1-4]. In contrast to intraoral techniques, which can provide only limited information about lesion origin, location, size and extent, cone beam computed tomography (CBCT) devices are able to acquire three dimensional (3D) reconstructions of the dento-maxillofacial region with high levels of hard tissue detail. Whereas conventional CT scanners emit a fan-shaped X-ray beam and require a stack of multiple slices to obtain a complete image, CBCT systems operate by focusing a cone-shaped beam on a 2D detector that performs one pass or less around the patient’s head to produce a series of 2D images. A reconstruction algorithm is then applied to the image data set and thereby reconstructed data sets can be oriented in a versatile way, and then visualized and reformatted for an optimal assessment. The main advantages of CBCT over medical CT are the size of the scanner, the cost and its ease of use for dental applications along with lower effective radiation doses[5,6].
Although intraoral radiographs still remain the imaging method of choice for the evaluation of endodontic patients the use of CBCT in endodontics showed a significant jump in recent years. Limited field of view (FOV) CBCT with relatively low patient doses and small voxel sizes should be considered the imaging modality of choice for diagnosis in patients who present with contradictory or non-specific clinical signs and symptoms associated with untreated or previously endodontically-treated teeth[7].
The purpose of these case series was to show the importance of CBCT aided diagnosis, and treatment of complex endodontic cases. We present 6 different cases diagnosed and treated with the aid of CBCT. Our case series included an external root resorption (ERR), a periapical pathology in a missed extraroot canal of a mandibular premolar, an oblique root fracture in a maxillary molar, a fusion in a mandibular second molar, a missed periapical pathology in a canine and a horizontal root fracture (HRF) in a central incisor that occurred due to an accident.
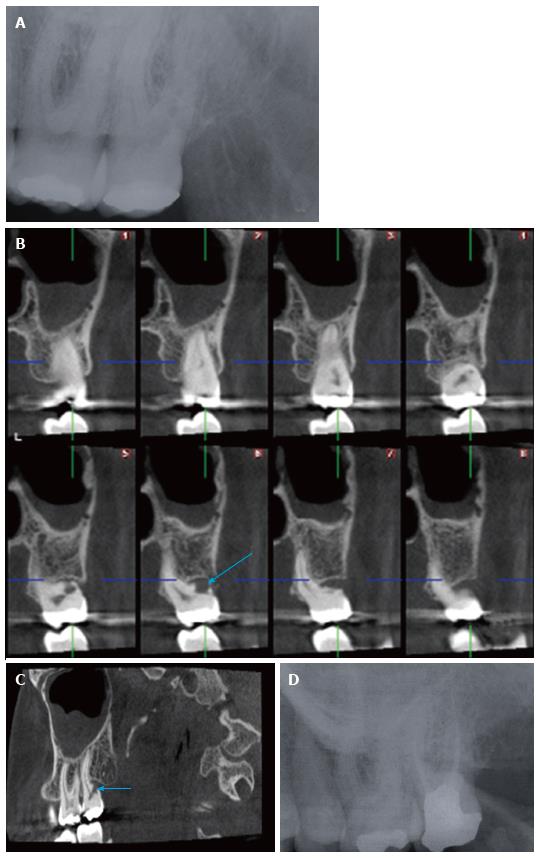
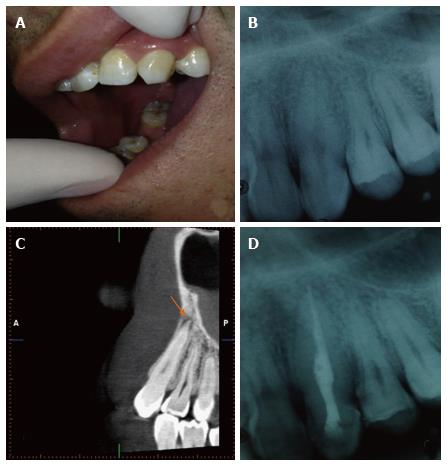
A 40 years old female patient was referred to our clinic with a recent history of an acute pain in the left maxillary posterior region. Maxillary left second molar tooth was tender to percussion and its distal soft tissues were painful on palpation. Also, there was a > periodontal pocket when probbed distally. The tooth responded to sensitivity tests (cold test and electric pulp test) positively. Periapical radiographic findings did not show caries or any periapical pathology (Figure ). A detailed radiological assessment with CBCT images showed the presence of an ERR in relation with the whole buccodistal root (Figure 1B and C). At this initial visit pulp tissue was removed and available root canals were prepared and filled with calcium hydroxide. A week later, all clinical symptoms disappeared. Resorptive buccodistal root canal was then obturated with mineral trioxide aggregate (MTA)-Angelus (Angelus, , ) orthogradically. Other canals were finally obturated with gutta-percha and AH Plus (Dentsply DeT-rey GmbH, ). The coronal portion of the tooth was restored with amalgam. The patient was followed up for 1 year. The tooth was completely asymptomatic and no radiographic signs of pathology were evident on periapical radiography taken after 1 year (Figure 1D).
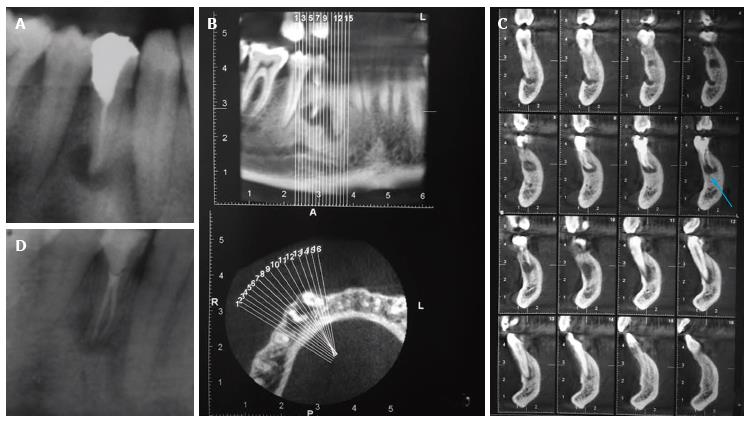
A 35 years old male patient was referred to our clinic with an acute pain in his right mandibular first premolar tooth that was treated two years earlier. The tooth was sensitive to vertical percussion. Periapical radiography of the tooth showed a radiolucent area at the periapical region. The root canal treatment seemed to be properly conducted (Figure ). However, panoramic/axial CBCT images (Figure 2B) and cros-sectional CBCT images (Figure ) showed that there was one more non-treated root canal along with a periapical lesion. At this initial visit root canals were prepared and then filled in with calcium hydroxide (Sultan Healthcare Inc., NJ, ). A week later root canal was finally obturated with gutta-percha and AH Plus (Dentsply DeT-rey GmbH, ). The tooth was restorated with composite resin (Figure 2D). At six months follow up the tooth was completely asymptomatic and there was no pathological change on radiographic assessment.
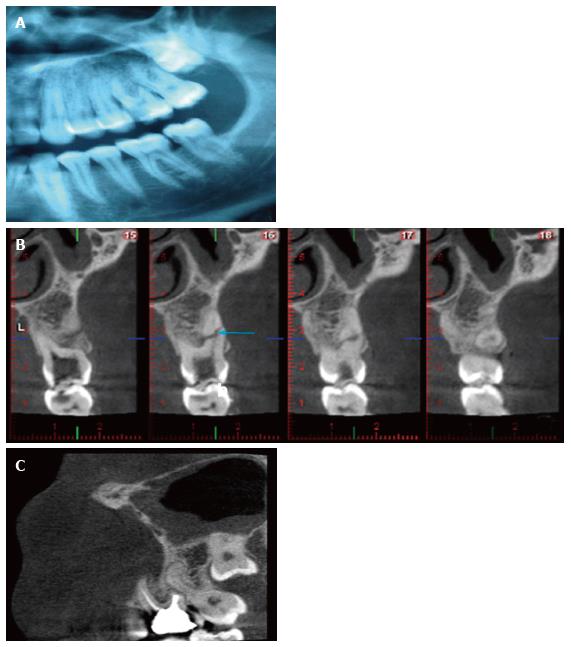
A 22 years old male patient was referred to our clinic with the complaint of persistent pain on left maxillary molar tooth during mastication. Patient history revealed that he used to punch on his left chick molar region when he got annoyed. Clinical and panoramic radiographic examination showed a carious maxillary 1st molar tooth (Figure ). The tooth responded to sensitivity tests (cold test and electric pulp test) positively. During root canal treatment the clinician felt as if buccodistal root canal was very short and she was unclear about the pathway of the root canal after taking a periapical radiography. Therefore, a CBCT scanning was requested and cross-sectional CBCT images revealed an oblique radiolucent root fracture line in the middle third of the buccodistal root (Figure 3B). At this initial visit root canals were prepared and filled in with calcium hydroxide. A week later firstly fracture line was sealed and filled with MTA-Angelus (Angelus, Londrina, Paraná, Brazil) and finally root canals were obturated with gutta-percha and AH Plus (Dentsply DeT-rey GmbH, Bensheim, Germany). The coronal portion of the tooth was restorated with composite resin. Another CBCT image was obtained in order to assess the fractured region 1 year after the initial treatment. CBCT imaging showed no resorption or fracture at 1 year follow up (Figure ). The tooth was also clinically asymptomatic at 2 year follow up.
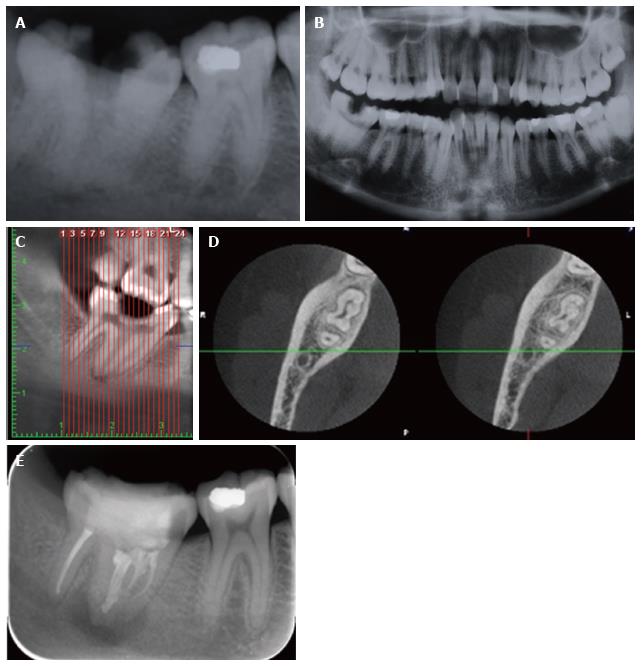
A 18 years old female patient presented to our clinic with the complaint of persistent pain on right mandibular molar tooth. Upon clinical intraoral examination, a fused mandibular second molar tooth with an occlusal caries was noticed. Percussion created an increase in the intensity of pain. The tooth was non-responsive to sensitivity tests with cold and electric. On periapical radiography, presence of caries was detected and presence of a periapical lesion was suspected (Figure ). The left mandibular second molar appeared to be normal in shape on panoramic radiography (Figure 4B). CBCT imaging was obtained in order to assess the complex canal morphology in detail. Panoramic and axial CBCT images showed that mandibular 2nd and 3rd molars were fused and there was apparent periapical radiolucency (Figure and D). Root canals were prepared and filled in with calcium hydroxide/iodoform paste (Vitapex; Neo Dental Chemical Products Co. Ltd., ). A week later, all clinical symptoms disappeared. Root canals were finally obturated using single cone technique with guta percha and AH Plus. The coronal portion of the teeth was restorated with amalgam. The tooth was re-evaluated six months later with periapical radiography (Figure 4E). Radiographically there was no sign of periapical pathology and clinically tooth was asymptomatic.
A 22 years old male patient was referred to our clinic with the complaint of persistent pain on left maxillary canine tooth when biting. On clinical examination, the tooth seemed to be intact (Figure ). However, sensitivity tests were negative. Periapical radiographic findings showed no periapical pathology or a carious lesion (Figure 5B). Sagittal CBCT images showed a periapical radiolucency (Figure ). At this initial visit, root canal was prepared and filled with calcium hydroxide (Sultan Healthcare Inc., NJ, ). A week later, all clinical symptoms disappeared. Root canal was finally obturated using single cone technique with guta percha and AH Plus (Figure 5D). The coronal portion of the tooth was restorated with composite resin. The patient did not come to regular periodic examinations.
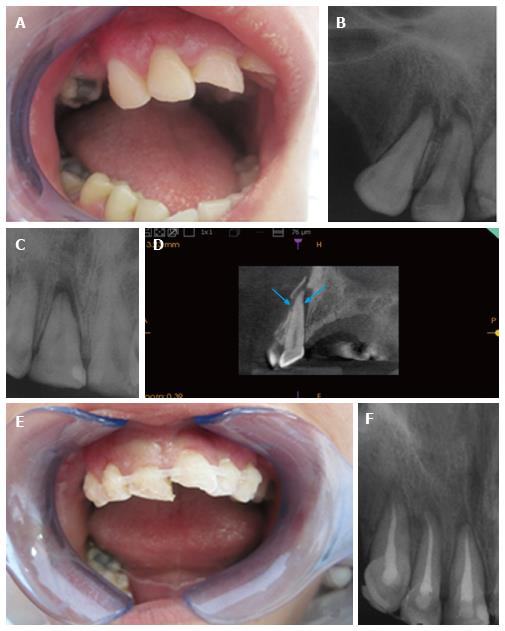
A 25 years old female patient came to our clinic 1 wk after a car accident. She had pain and mobility in her right canine and incisors and there was an incisal crown fracture in right central incisor (Figure ). Canine and incisor teeth did not respond to cold and electric tests. Intraoral radiographs taken from two different angels showed periapical radiolucencies in canine and incisors but they were unable to show a suspected HRF (Figure 6B and C). However, with CBCT Kodak 9000 3D (Eastman Kodak Co, Rochester, NY, United States) CMOS sensor with optical fiber, offering a single × FOV at voxel we managed to detect a HRF in right central incisor along with alveolar bone fracture in cross-sectional views (Figure 6D). Canine and incisors were splinted with orthodontic wire and composite resin for 2 wk (Figure 6E) and then obturated using single cone technique with guta percha and AH Plus (Figure ).
Units with small FOVs offering high-resolution images of teeth and related structures with relatively low radiation dose are specifically recommended in cases where 2D systems fail to provide sufficient information regarding peri-treatment decision-making and surveillance of periapical tissues over time[7]. According to AAE and AAOMR Joint Position Statement published in 2015, several application areas were included for the use of limited FOV CBCT in endodontics. Assessment of complex root canal morphology and dental anomaly, evaluation of consistent periapical pathosis and differentiation between radiolucencies mimicking apical lesions and persistent idiopathic facial pain were among useful indications. Pre-surgical assessment by determining the exact location of root apices in relation to adjacent anatomical structures such as mandibular canal and maxillary sinus was also recommended. CBCT may help in identifying endodontic treatment complications, such as overextended obturation material, separated endodontic instruments, calcified canals and perforations. Besides, follow up of non-healing endodontic treatment and decision of further treatment plan with CBCT was recommended. A CBCT image was suggested in the diagnosis and management of dentoalveolar trauma. Finally, the use of CBCT was recommended in order to localize and differentiate between external and internal root resorption and invasive cervical resorption[7].
ERR is defined as the loss of mineralized dental tissue. Inflammation or infection and pressure caused by impacted teeth, masses, or orthodontic movement are among the etilogical factors related to pathological ERR[8]. The current technique for diagnosing ERR is intraoral periapical radiography. Most cases are discovered during routine examinations and are usually in their late stages resulting in tooth extraction. Therefore, the early and accurate diagnosis is very important, in terms of treatment planning and prognosis. Intraoral periapical radiography may not provide sufficient information regarding location, size and extent of resorptive lesions due to projection of the lingual and buccal cortices, multiple roots, and adjacent anatomical structures[9,10]. In case 1, periapical radiography was unable to show any resorption cavity due to inherent limitations of the technique. CBCT provided very useful information regarding the exact location, size and extent of the resorption cavity. As the lesion involved only 1 root, treatment with MTA was conducted. MTA was used as the repair material in this case due to its capacity to promote hard tissue formation and to inhibit osteoclastic bone resorption[11].
The thorough knowledge of root canal space anatomy is a basic prerequisite for the successful completion of endodontic treatment[12], especially in cases where extra root canals are suspected[13]. Proper care and attention must be given in identifying extra roots and canals[14]. Mandibular premolars are the most difficult teeth for endodontic treatment due to their complicated root canal anatomy[15]. In case 2, we detected an extra canal along with periapical radiolucency in a mandibular premolar tooth by using CBCT imaging. CBCT images facilitated better visualization of the extra canal that was not visible on periapical radiography and enabled treatment of the extra canal.
Vertical-oblique root fracture is an important threat to prognosis of the tooth during and after root canal treatment[16,17]. Clinically, it may be confused with periodontal disease or a failed root canal treatment[18,19]. Radiographic diagnosis is also difficult since not all the classical radiographic signs of root fracture may be present in every case. CBCT has been used in recent studies with a high accuracy and sensitivity in detecting root fracture[20,21]. Film and digital periapical radiographs have many limitations in the detection of root fractures because of their 2D nature, especially when fractures are mesiodistally originated. In case 3, CBCT imaging facilitated visualization of the oblique fracture in 3D. Besides, a one year follow up CBCT image taken after treatment in order to assess any resorption or fracture in the region revealed no apparenet pathology.
Fusion of teeth is a developmental anomaly, which stem from the union of two teeth originating both in primary and the permanent dentition. Fusion rarely occurs in the mandibular posterior teeth[22,23]. The union of two discrete tooth germs results in fusion, leading to the formation of a single tooth that show separate pulp cavities[24]. Physical forces which produce close contact between two developing teeth have an influence in its formation along with hereditary factors for rendering[25]. In case 4, we detected that mandibular 2nd and 3rd molars were fused and we observed caries along with periapical radiolucency. CBCT images facilitated better visualization of complex root canal orifice and thereby risk of complications during treatment was eliminated to some extent.
Apical periodontitis (AP) is a chronic inflammatory disorder of periradicular tissues caused by etiological agents of endodontic origin[26]. Advanced stage AP is characterized by inflammation and changes of periapical bone structure[27]. Periapical lesions may only become visible on intraoral radiographs when they produce nearly 30%-50% of mineral bone loss[28]. In case 5, a periapical radiography was unable to show any periapical radiolucency. Therefore, a CBCT image was obtained in order to determine the exact etiology of the pain.
HRF is most frequently observed in the maxillary anterior region of male patients due to trauma associated with accidents, sports injuries and fights. The diagnosis of HRF is based on the radiographic demonstration of a fracture line or lines and/or mobility of the coronal segment of the tooth. Fracture can be overlooked when the X-ray beam does not pass along the fracture line, and therefore in many cases, two or three intraoral radiographs taken from different angles are recommended. The interpretation of root fracture on intraoral radiographs can be problematic, particularly where displacement of the fragments has not yet occurred due to edema or granulation tissue[3,29]. In case 6, 1 wk after a traumatic accident we were unable to detect a HRF line on two differently angulated periapical radiographs. This may be due to angulation of the beam. It is also possible that displacement of the fragments did not occur at the time of imaging.
Due to differences in technical factors, radiation doses from different CBCT scans can vary between devices. The reported effective doses for the CBCT unit used in the present case series is in the range 28 to 122 μSv[30]. This is higher than the effective doses from periapical radiography taken with E-speed film with rectangular collimation (1 to 3 μSv) and round collimation (1 to 5 μSv)[31]. Not only endodontic diagnosis can be made better using CBCT when compared to periapical radiography, but also lesions can be assessed in several views. However, comparative radiation dosages should be weighed against diagnostic benefits in selecting the appropriate imaging modality for specific purposes.
Effective doses with CBCT units are still higher when compared to intraoral imaging. Although, limited FOV which is suggested for endodontic purposes offers less radiation in comparison to large FOV, clinicians should use caution when prescribing CBCT imaging. It can be expected that the development of units that offer higher-definition dental images with lower effective doses, dose-risk relationships at low radiation levels and patient treatment outcome after CBCT scanning will lead to further refinement of referral criteria and this would help clinician to more reliably and frequently refer patients for CBCT examination[5].
Root resorption, missed extra canal, fusion, oblique root fracture, non-diagnosed periapical pathology and horizontal root fracture.
Pain, discomfort and sometimes swelling.
Resorption, caries, and fractures can be thougt for differential diagnosis.
Conventional two dimensional methods and cone beam computed tomography (CBCT) were utilizied.
Resorption, periapical pathology and root fracture.
Root canal treatment was the main method of choice.
This study presents several cases which are useful for a clinician to better understand the use of CBCT for clinical diagnosis and treatment planning.
CBCT: Cone beam computed tomography; MTA: Mineral trioxide aggregarate.
This case series presentation shows the importance of CBCT aided diagnosis and treatment of complex endodontic cases.
This is a good paper.
Manuscript Source: Invited manuscript
Specialty Type: Radiology, Nuclear Medicine and Medical Imaging
Country of Origin: Turkey
Peer-Review Report Classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Ferreira MM, Schoenhagen P, Sener RN, Tsalafoutas IA S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
| 1. | Kamburoğlu K, Barenboim SF, Kaffe I. Comparison of conventional film with different digital and digitally filtered images in the detection of simulated internal resorption cavities--an ex vivo study in human cadaver jaws. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;105:790-797. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 2. | Kamburoğlu K, Tsesis I, Kfir A, Kaffe I. Diagnosis of artificially induced external root resorption using conventional intraoral film radiography, CCD, and PSP: an ex vivo study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:885-891. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 31] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 3. | Kamburoğlu K, Ilker , Gröndahl HG. Effectiveness of limited cone-beam computed tomography in the detection of horizontal root fracture. Dent Traumatol. 2009;25:256-261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 56] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 4. | Tsesis I, Kamburoğlu K, Katz A, Tamse A, Kaffe I, Kfir A. Comparison of digital with conventional radiography in detection of vertical root fractures in endodontically treated maxillary premolars: an ex vivo study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:124-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 60] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 5. | Pauwels R, Jacobs R, Bosmans H, Schulze R. Future prospects for dental cone beam CT imaging. Imaging Med. 2012;4:551-563. [RCA] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 6. | Scarfe WC, Li Z, Aboelmaaty W, Scott SA, Farman AG. Maxillofacial cone beam computed tomography: essence, elements and steps to interpretation. Aust Dent J. 2012;57 Suppl 1:46-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 130] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 7. | Special Committee to Revise the Joint AAE/AAOMR Position Statement on use of CBCT in Endodontics. AAE and AAOMR Joint Position Statement: Use of Cone Beam Computed Tomography in Endodontics 2015 Update. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015;120:508-512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 198] [Article Influence: 19.8] [Reference Citation Analysis (0)] |
| 8. | Fuss Z, Tsesis I, Lin S. Root resorption--diagnosis, classification and treatment choices based on stimulation factors. Dent Traumatol. 2003;19:175-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 291] [Cited by in RCA: 283] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 9. | Patel S, Dawood A, Wilson R, Horner K, Mannocci F. The detection and management of root resorption lesions using intraoral radiography and cone beam computed tomography - an in vivo investigation. Int Endod J. 2009;42:831-838. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 169] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 10. | Patel S, Dawood A, Ford TP, Whaites E. The potential applications of cone beam computed tomography in the management of endodontic problems. Int Endod J. 2007;40:818-830. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 346] [Cited by in RCA: 326] [Article Influence: 18.1] [Reference Citation Analysis (0)] |
| 11. | Hashiguchi D, Fukushima H, Yasuda H, Masuda W, Tomikawa M, Morikawa K, Maki K, Jimi E. Mineral trioxide aggregate inhibits osteoclastic bone resorption. J Dent Res. 2011;90:912-917. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 12. | Rödig T, Hülsmann M. Diagnosis and root canal treatment of a mandibular second premolar with three root canals. Int Endod J. 2003;36:912-919. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 28] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 13. | Sikri VK, Sikri P. Mandibular premolars: aberrations in pulp space morphology. Indian J Dent Res. 1994;5:9-14. [PubMed] |
| 14. | Mushtaq M, Farooq R, Rashid A, Robbani I. Spiral computed tomographic evaluation and endodontic management of a mandibular first molar with three distal canals. J Conserv Dent. 2011;14:196-198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 15. | Slowey RR. Root canal anatomy. Road map to successful endodontics. Dent Clin North Am. 1979;23:555-573. [PubMed] |
| 16. | Wang P, He W, Sun H, Lu Q, Ni L. Detection of vertical root fractures in non-endodontically treated molars using cone-beam computed tomography: a report of four representative cases. Dent Traumatol. 2012;28:329-333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 17. | Bernardes RA, de Moraes IG, Húngaro Duarte MA, Azevedo BC, de Azevedo JR, Bramante CM. Use of cone-beam volumetric tomography in the diagnosis of root fractures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108:270-277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 110] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 18. | Varshosaz M, Tavakoli MA, Mostafavi M, Baghban AA. Comparison of conventional radiography with cone beam computed tomography for detection of vertical root fractures: an in vitro study. J Oral Sci. 2010;52:593-597. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 43] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 19. | Valizadeh S, Khosaravi M, Azizi Z. Diagnostic accuracy of conventional, digital and cone beam computed tomography in vertical root fracture detection. Endod J. 2011;6:15-20. |
| 20. | Edlund M, Nair MK, Nair UP. Detection of vertical root fractures by using cone-beam computed tomography: a clinical study. J Endod. 2011;37:768-772. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 90] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 21. | Zou X, Liu D, Yue L, Wu M. The ability of cone-beam computerized tomography to detect vertical root fractures in endodontically treated and nonendodontically treated teeth: a report of 3 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;111:797-801. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 22. | Neville BW, Damm DD, Allen CM, Bouquot J. Oral and Maxillofacial Pathology. 3rd ed. Abnormalities of teeth. : Saunders 2009; 54-111. |
| 23. | Acs G, Cozzi E, Pokala P. Bilateral double primary molars: case report. Pediatr Dent. 1992;14:115-116. [PubMed] |
| 24. | Hernandez-Guisado JM, Torres-Lagares D, Infante-Cossio P, Gutierrez-Perez JL. Dental gemination: report of case. Med Oral. 2002;7:231-236. [PubMed] |
| 25. | Tsesis I, Steinbock N, Rosenberg E, Kaufman AY. Endodontic treatment of developmental anomalies in posterior teeth: treatment of geminated/fused teeth--report of two cases. Int Endod J. 2003;36:372-379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 26] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 26. | Nair PN. Pathogenesis of apical periodontitis and the causes of endodontic failures. Crit Rev Oral Biol Med. 2004;15:348-381. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 559] [Cited by in RCA: 648] [Article Influence: 30.9] [Reference Citation Analysis (0)] |
| 27. | Nair PN, Sjögren U, Figdor D, Sundqvist G. Persistent periapical radiolucencies of root-filled human teeth, failed endodontic treatments, and periapical scars. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;87:617-627. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 135] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 28. | Bender IB, Seltzer S. Roentgenographic and direct observation of experimental lesions in bone. J American Dent Assoc. 1961;62:152-160. [RCA] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 118] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 29. | Kamburoglu K, Onder B, Murat S, Avsever H, Yüksel S, Paksoy CS. Radiographic detection of artificially created horizontal root fracture using different cone beam CT units with small fields of view. Dentomaxillofac Radiol. 2013;42:20120261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 30. | Pauwels R, Beinsberger J, Collaert B, Theodorakou C, Rogers J, Walker A, Cockmartin L, Bosmans H, Jacobs R, Bogaerts R. Effective dose range for dental cone beam computed tomography scanners. Eur J Radiol. 2012;81:267-271. [RCA] [DOI] [Full Text] [Cited by in Crossref: 393] [Cited by in RCA: 418] [Article Influence: 32.2] [Reference Citation Analysis (0)] |
| 31. | Gijbels F, Jacobs R, Sanderink G, De Smet E, Nowak B, Van Dam J, Van Steenberghe D. A comparison of the effective dose from scanography with periapical radiography. Dentomaxillofac Radiol. 2002;31:159-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 1.0] [Reference Citation Analysis (0)] |