Published online Dec 28, 2016. doi: 10.4329/wjr.v8.i12.928
Peer-review started: April 27, 2016
First decision: July 5, 2016
Revised: July 26, 2016
Accepted: August 17, 2016
Article in press: August 18, 2016
Published online: December 28, 2016
Processing time: 237 Days and 10.5 Hours
This case study reports the successful outcome of horizontal root fractures of two different patients, which took place in permanent incisors. Report 1 describes a case of a 29-year-old patient who suffered a mandibular trauma affecting mainly the lower central incisors, caused by a car accident. A panoramic radiograph was taken right after the accident and showed a horizontal root fracture in the middle third of tooth 42, which went untreated. Report 2 illustrates a case of a 17-year-old male patient who searched for orthodontic therapy and the periapical radiograph showed horizontal root fracture in tooth 11 caused by a previous trauma, which went untreated as well. There was healing through the reestablishment of pulp activity and dental coloration without professional intervention.
Core tip: The innovative arguments of this paper is the importance of the follow up procedure conceding the biological response of each patient facing root fractures; especially apex remodeling, calcification and root resorptions. Dentists must be aware that such biological responses may happen without professional interference, which, made previously, might have a complete different outcome.
- Citation: Silva L, Álvares P, Arruda JA, Silva LV, Rodrigues C, Sobral APV, Silveira M. Horizontally root fractured teeth with pulpal vitality - two case reports. World J Radiol 2016; 8(12): 928-932
- URL: https://www.wjgnet.com/1949-8470/full/v8/i12/928.htm
- DOI: https://dx.doi.org/10.4329/wjr.v8.i12.928
Horizontal root fractures have been more frequently detected in the maxillary upper anterior region, affecting mainly the second life decade of the male patient group[1]. They usually occur in fully erupted teeth with complete root formation[2,3]; frequently seen in the middle third of the root followed by apical and coronal third fractures[4]. This paper aims to describe two cases of root fracture with pulpal vitality which healed without professional intervention.
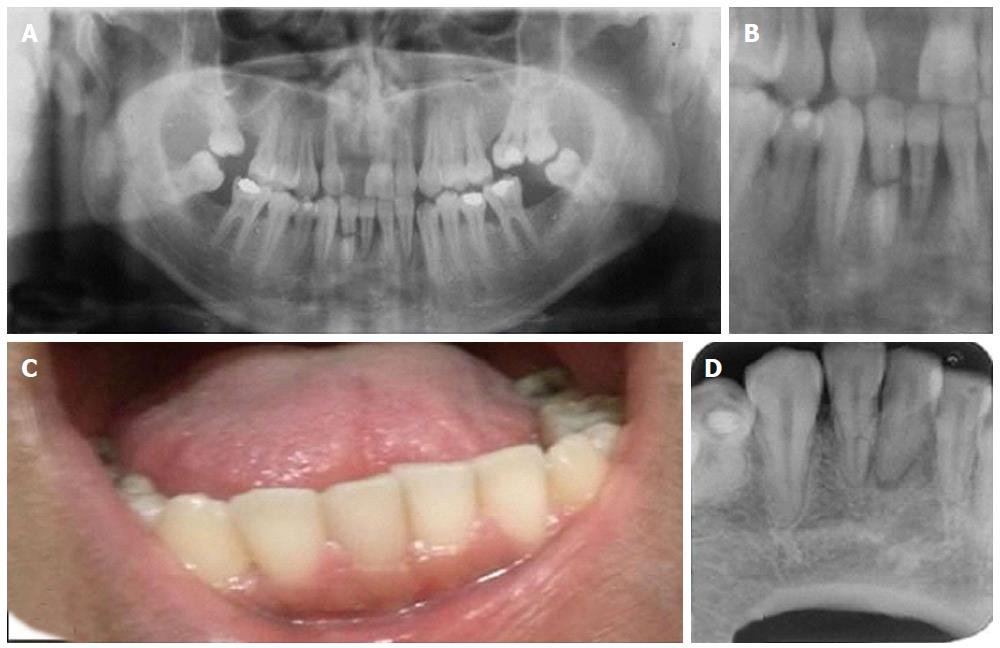
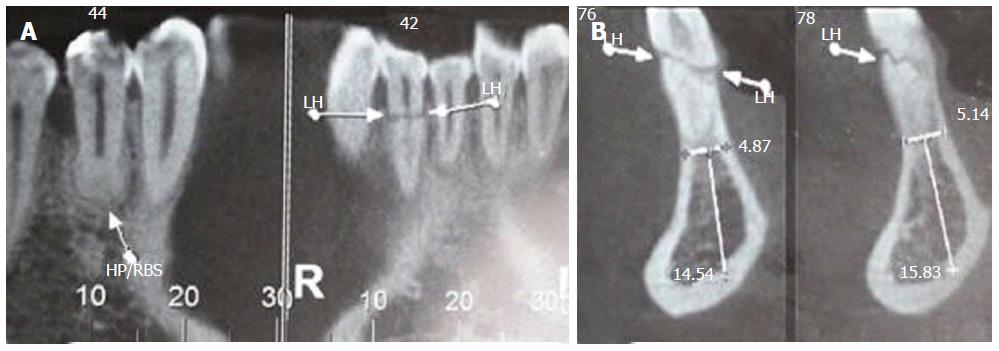
A 29-year-old male patient searched for dental assistance on September 2009 for extraction of the tooth 42 by his own will. He had suffered a trauma caused by a car accident back in May 2008. A panoramic radiograph taken at the time of the accident showed a two fragment middle third horizontal root fracture in tooth 42 (Figure 1A). After intraoral examination, normal aspects were observed in tooth 42, including color, absence of mobility and positive response to pulp sensibility test (EndoFrost®) (Figure 1B and C); Tooth 41 was slightly grayish, responding negatively to sensibility test. Periapical radiograph (Figure 1D) and cone beam tomography showed hypodense image in the periapex in tooth 41. Tooth 42 showed a hypodense image in the middle third of the root confirming a fracture with no hypodense lesions in the periodontium. As the tooth 42 responded positively to pulp sensibility test, the hypodense line was interpreted as cicatricial fibrosis (Figure 2). Tooth 44 showed external dentinal root resorption plus remodeling of the apex, also showing a calcification spot in the apical third of the root canal, while tooth 43 had its apical third obliterated. The sensibility test to cold was negative. After the diagnosis the patient did not return for the accomplishment of the endodontic treatment.
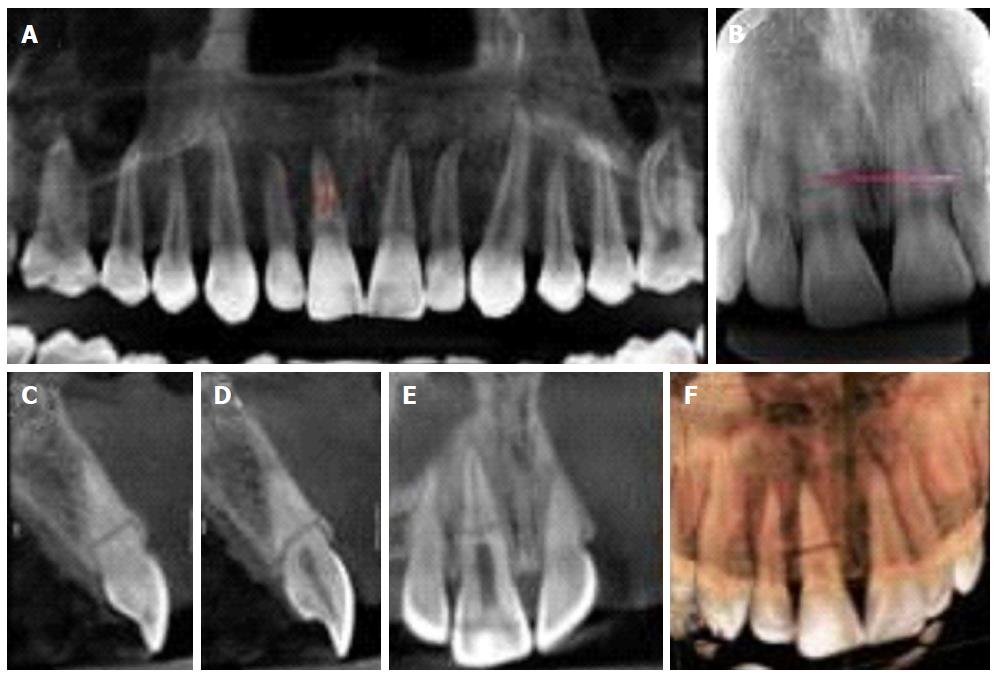
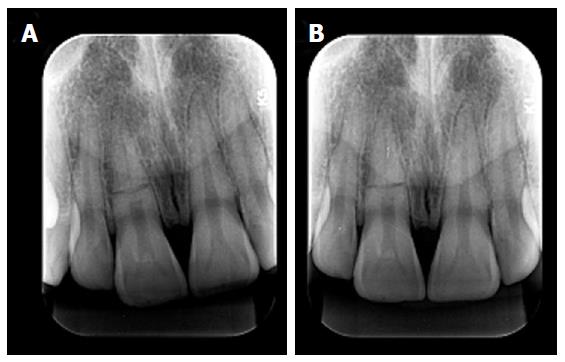
A 17-year-old male patient’s periapical radiographic examination for orthodontic purposes showed a horizontal radiolucent line in the root of tooth 11, suggesting root fracture. The pulp chamber and the cervical third showed normal aspects, as well as the periapex. The patient reported trauma in the region back in 2006. In 2008 in a routine dental appointment the horizontal root fracture was then detected. The tooth was vital and thus a clinical and radiographic follow-up took place in September 2015. A cone beam tomography was then requested and confirmed horizontal root fracture in tooth 11 with fragments discreetly not aligned, showing no signs of resorption in the root and the periapical bone tissue around the fracture (Figure 3A). The root segments were juxtaposed and aligned in the mesio-distal direction (Figure 3B, D and F) and slightly misaligned in buccolingual direction (Figure 3C and D). In Figure 4, observed horizontally root fractured in the radiographic takings distoradial and ortoradial. Clinically, the tooth showed no crown mobility or discoloration and its vitality continued to be demonstrated by the sensibility test.
The outcomes for traumatized teeth can be altered by many situations, such as the stage of root formation, periodontal conditions and trauma type and intensity. Normally, when the patients search for dental care in the case of a trauma, current literature instructs to immobilize the tooth with a semi-rigid splint for 4 wk up to 4 mo (Table 1)[5-9]. Sensibility tests, immediately performed in the post trauma, are not indicated since they might worsen the clinical condition after the accident[2,5].
| Time | Root fracture | Alveolar fracture |
| 4 wk | Splint removal1, clinical and radiographic control | Splint removal and clinical and radiographic controls |
| 6-8 wk | Clinical and radiographic control | Clinical and radiographic control |
| 4 mo | Splint removal2 and radiographic control | Clinical and radiographic control |
| 6 mo | Clinical and radiographic control | Clinical and radiographic control |
| 1 yr | Clinical and radiographic control | Clinical and radiographic control |
| Yearly for 5 yr | Clinical and radiographic control | Clinical and radiographic control |
It is also possible that, in the cases described in this paper, the connective tissue of the pulp has not been ruptured at all, although a cleavage has affected the root. Particularly in report 1, the initial radiograph suggests that the traumatized tooth was free of mechanical forces by the absence of the antagonist tooth. The apex was closed, and its potential entrance for blood vessels no longer existed. Therefore, the only possible entrance available was the connective tissue from the periodontal ligament accessed by the fracture.
A similar situation took place in report 2. The impact seems to have been greater so that the fragments became apart, and a new blood supply seems to have been independently formed in both fragments. Paradoxically, it was the fracture itself that was the likely responsible for the existence of an additional blood supply in both cases. Another interesting fact is that in both cases, the fractured teeth were not the main cause that made the patients visit the dentist. In report 1, tooth 41 was the one with the best prognosis, and had a final completely paradoxal outcome, presenting a periapical lesion and the need of endodontic treatment due to pulp necrosis. On the other hand, patient in report 2 had no complaint at all. It is worth mentioning that in both cases the teeth remained untreated and were not splinted[10].
The study of orthodontics combined with root fractured teeth orthodontic movement is crucial because pressure applied on traumatized teeth displays small risks of resorption when pulp condition is normal. However, whether treating or not teeth with root fractures is still an endodontic clinical dilemma[11].
According to Brin et al[11] previously traumatized teeth are most prone to developing root resorptions, although in a moderate way, followed by the group of patients with intact incisors and the group of children who underwent traumatic history in the upper incisors, and they concluded that the combination of trauma and orthodontic tipping is more susceptible to complications, being the most common root resorption and loss of vitality. When roots are fractured there may be the formation of hard, connective or granulomatous tissues in the fracture line, which is related to the kind of injury[12]. As for what concerns orthodontics, it is possible to move a fractured tooth, since due care and follow ups are taken[13-15].
In order to offer the patient a better chance of healing, an appropriate plan of treatment is essential after an injury, basically because dentoalveolar traumatic outcomes must be assessed with the aid of clinical and imaginological sources[15,16].
Healey et al[15] presented 2 case reports concerning orthodontic movement of two teeth with root fractures, showing that it is possible to accomplish the movement but suggested a period of rest for the teeth affected because of the real possibility of increased root resorption risks. They added that such rest period is necessary for the dissipation of the stress inflicted to the periodontal ligament, in order to achieve the recovery of the inflamed tissues.
When a tooth undergoes trauma, the composing tissues may respond to it in different ways or with associations, such as those detected in the cone beam tomography of report 1, in which teeth 44 and 43 responded with partial pulp calcification; in tooth 44 it can also be observed external root resorption with apex remodeling, being possible the visualization of hypodense area suggestive of the periodontal ligament maintenance. In tooth 44, it can also be observed external root resorption with apex remodeling. Tooth 41 showed hypodense image in the periapex suggestive of apical radioluscence, while tooth 42 showed hypodense image suggestive of fracture and due to the vital response of the pulp it can be interpreted as cicatricial fibrosis. Electrical pulp test, as well as thermal tests are indicated right after an injury, and the absence of a positive result in the first weeks does not mean that a tooth needs treatment[5,7,9,17]. Therefore, our paper concludes that only clinical evaluation with visual inspection, pulp sensibility tests and periodical image assessment are able to direct the conduct and/or treatment to be taken for traumatized teeth.
A 29-year-old and a 17-year-old patients with no significant history presented horizontal root fractures detected by routine clinical examination, which went untreated, and undetected until the moment of the dental appointment.
Both patients were asymptomatic and the fractures were detected by routine examinations.
Root perforation, periodontal disease, pulpitis.
Panoramic radiograph in case one taken at the moment of the accident showed horizontal fractures in the middle third of tooth 42. Periapical radiograph at the moment of the appointment showed a thin radiolucent image and cone beam tomography showed oblique fracture with signs of healing.
Horizontal root fractures.
Horizontal root fractures are more common in anterior teeth and may heal spontaneously or under professional intervention.
Horizontal and vertical fractures are the most common traumatic dental injuries whereas crown fractures are the second most commonly reported.
Horizontal root fractures usually offer bad prognosis for the teeth involved; which may result in dental extractions. When the professional is aware of the fracture at the time it happened he may interfere endodontically or by splitting the teeth together to stimulate healing. This article shows that sometimes not interfering professionally may be a choice when dealing with root fractures.
This is a well-structured case report.
Manuscript source: Unsolicited manuscript
Specialty type: Radiology, nuclear medicine and medical imaging
Country of origin: Brazil
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Gonzalez-Reimers E, Sheikh-Nezami M, Vieyra JP S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
| 1. | Cavalleri G, Zerman N. Traumatic crown fractures in permanent incisors with immature roots: a follow-up study. Endod Dent Traumatol. 1995;11:294-296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 54] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 2. | Levin L, Zadik Y. Education on and prevention of dental trauma: it is time to act! Dent Traumatol. 2012;28:49-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 52] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 3. | Hovland EJ. Horizontal root fractures. Treatment and repair. Dent Clin North Am. 1992;36:509-525. [PubMed] |
| 4. | Bramante CM, Menezes R, Moraes IG, Bernardinelli N, Garcia RB, Letra A. Use of MTA and intracanal post reinforcement in a horizontally fractured tooth: a case report. Dent Traumatol. 2006;22:275-278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Diangelis AJ, Andreasen JO, Ebeleseder KA, Kenny DJ, Trope M, Sigurdsson A, Andersson L, Bourguignon C, Flores MT, Hicks ML. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 1. Fractures and luxations of permanent teeth. Dent Traumatol. 2012;28:2-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 327] [Cited by in RCA: 290] [Article Influence: 41.4] [Reference Citation Analysis (0)] |
| 6. | Cohenca N, Karni S, Eidlitz D, Nuni E, Moshonov J. [New treatment protocols for avulsed teeth]. Refuat Hapeh Vehashinayim (1993). 2004;21:48-53, 98. [PubMed] |
| 7. | American Association of Endodontics. Treatment of the avulsed permanent tooth: recommended guidelines of the American Association of Endodontics. Chicago: AAE publication 2014; . |
| 8. | Ram D, Cohenca N. Therapeutic protocols for avulsed permanent teeth: review and clinical update. Pediatr Dent. 2004;26:251-255. [PubMed] |
| 9. | Andreasen JO, Ahrensburg SS, Tsilingaridis G. Root fractures: the influence of type of healing and location of fracture on tooth survival rates - an analysis of 492 cases. Dent Traumatol. 2012;28:404-409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 39] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 10. | Orhan K, Orhan AI, Oz FT. Management of untreated traumatized permanent incisors with crown and root fractures: a case report. Quintessence Int. 2009;40:647-654. [PubMed] |
| 11. | Brin I, Ben-Bassat Y, Heling I, Engelberg A. The influence of orthodontic treatment on previously traumatized permanent incisors. Eur J Orthod. 1991;13:372-377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 54] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 12. | Zachrisson BU, Jacobsen I. Response to orthodontic movement of anterior teeth with root fractures. Trans Eur Orthod Soc. 1974;207-214. [PubMed] |
| 13. | Hovland EJ, Dumsha TC, Gutmann JL. Orthodontic movement of a horizontal root fractured tooth. Br J Orthod. 1983;10:32-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Erdemir A, Ungor M, Erdemir EO. Orthodontic movement of a horizontally fractured tooth: a case report. Dent Traumatol. 2005;21:160-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (1)] |
| 15. | Healey DL, Plunkett DJ, Chandler NP. Orthodontic movement of two root fractured teeth: a case report. Int Endod J. 2006;39:324-329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 16. | Bhaskar SN, Rappaport HM. Dental vitality tests and pulp status. J Am Dent Assoc. 1973;86:409-411. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 70] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 17. | Tronstad L. Root resorption--etiology, terminology and clinical manifestations. Endod Dent Traumatol. 1988;4:241-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 394] [Cited by in RCA: 372] [Article Influence: 10.1] [Reference Citation Analysis (0)] |