Published online Sep 28, 2015. doi: 10.4329/wjr.v7.i9.253
Peer-review started: March 31, 2015
First decision: April 27, 2015
Revised: May 14, 2015
Accepted: July 21, 2015
Article in press: July 23, 2015
Published online: September 28, 2015
Processing time: 197 Days and 18.2 Hours
Spine fractures account for a large portion of musculoskeletal injuries worldwide. A classification of spine fractures is necessary in order to develop a common language for treatment indications and outcomes. Several classification systems have been developed based on injury anatomy or mechanisms of action, but they have demonstrated poor reliability, have yielded little prognostic information, and have not been widely used. For this reason, the Arbeitsgemeinschaftfür Osteosynthesefragen (AO) committee has classified thorocolumbar spine injuries based on the pathomorphological criteria into3 types (A: Compression; B: Distraction; C: Axial torque and rotational deformity). Each of these types is further divided into 3 groups and 3 subgroups reflecting progressive scale of morphological damage and the degree of instability. Because of its highly detailed sub classifications, the AO system has shown limited interobserver variability. It is similar to its predecessors in that it does not incorporate the patient’s neurologic status.The need for a reliable, reproducible, clinically relevant, prognostic classification system with an optimal balance of ease of use and detail of injury description contributed to the development of a new classification system, the thoracolumbar injury classification and severity score (TLICS). The TLICS defines injury based on three clinical characteristics: injury morphology, integrity of the posterior ligamentous complex, and neurologic status of the patient. The severity score offers prognostic information and is helpful in decision making about surgical vs nonsurgical management.
Core tip: The thoracolumbar injury classification and severity score (TLICS) is the recent thoracolumbar injury grading scale to combine injury morphology, evaluation of mechanical strength pertinent to the posterior ligamentous complex, and neurologic condition into a method efficient of directing injury management. The TLICS provides the best available predictor of surgical vs nonsurgical management. Radiologists should use the key components of the TLICS to analyze, evaluate, and report spine injuries.
- Citation: Gamanagatti S, Rathinam D, Rangarajan K, Kumar A, Farooque K, Sharma V. Imaging evaluation of traumatic thoracolumbar spine injuries: Radiological review. World J Radiol 2015; 7(9): 253-265
- URL: https://www.wjgnet.com/1949-8470/full/v7/i9/253.htm
- DOI: https://dx.doi.org/10.4329/wjr.v7.i9.253
Spinal injuries constitute a significant proportion of musculoskeletal injuries across the world. Nearly 75% to 90% of spinal fractures occur in the thoracic and lumbar regions, most commonly involving at the thoracolumbar junction (T10-L2)[1-3]. Despite the high frequency of thoracolumbar fractures, there is no single definite consensus on classification and management of such injuries. An ideal classification system is one that is explanatory and analytical, is informal to learn and apply in medical practice, based on a naive algorithm with constant radiologic and clinical features. Furthermore, the classification must give information on severity and expected description of an injury configuration. Lastly, for injury prediction, the classification must help decision-making. Such a classification system would be instrumental clinical research. Numerous thoracolumbar spine injury classification methods have been established to direct clinical and surgical management[4-6].
Watson-Jones[7] defined three patterns of spinal injury: Simple wedge fracture, comminuted fracture, and fracture-dislocation. This classification system was the first of its kind which served as a guide for treatment. This system proposed different reduction methods for the management of different spinal fractures. Chance[8] described a special type of injury caused by forceful forward flexion. The flexion anteriorly was coupled with distraction injury at the level of posterior elements, and was also known as a seat-belt injury. This distraction injury is characterized by a compression fracture of the anterior part of the vertebral body, a transverse fracture line through the posterior part of the vertebral body which extends into the posterior elements of the spine. Nicoll[9] reported a series of 166 thoracolumbar injuries in coal miners and categorized these fractures into following categories: (1) anterior wedge fractures; (2) lateral wedge fractures; (3) fracture dislocations; and (4) isolated neural arch fractures. Nicoll, for the first time, defined stable vs unstable fractures based on the integrity of the interspinous ligament is a major determinant of stability. This served as a basis for subsequent classifications. Holdsworth[10], described two-column theory. The anterior column comprises of anterior longitudinal ligament (ALL), body of the vertebra and the adjacent intervertebral disc and the posterior longitudinal ligament (PLL). The posterior column includes pedicles, facet joints, transverse processes, Ligamentum flavum, spinous processes and the interspinous and supraspinous ligaments. He also suggested that the posterior column is the major determinant of spinal stability. Kelly and Whiteside[11] further added to a two-column theory of Holdsworth, described the anterior vertebral bodies as solid column and the neural arches as a hollow posterior column. They highlighted the significance of the posterior elements in the stability the spine, and also described that greater instability reflects moreserious type of injury. Denis[12] later described a three column theory and devised a sagittal profile of the spine into 3 columns: He added the middle column to the anterior and posterior columns described earlier. In this theory, the middle column, constituted by the posterior half of the vertebral body, the PLL, the posterior half of disc and the posterior annulus, is in the neutral axis of the spine.
The middle column is believed to contribute the maximum to mechanical stability and tolerate the maximum axial load during flexion and extension movement. The concept of middle column has introduced 2 distinct fracture types compression and burst fractures. Compression fractures involve only the anterior column whereas burst fractures involve both the anterior and the middle columns. A chance fracture is subsequently re-defined as a transverse injury that involving all anterior, middle and posterior columns[13].
The AO classification[14] was the next major development in spinal injury classification and uses the three column concept proposed by Denis[12].
It categorizes thoracolumbar spinal injuries into three categories based on the patho-morphological criteria: compression injury (Group A), distraction injury (Group B), and translation or rotation injury (Group C), with up to nine subtypes in each category based on morphology, fracture site, osseous or ligamentous disruption, and direction of displacement. One of its principle rationales is that groups A through C represent a continuum of progressively increasing injury severity and instability, with a concomitant increasing likelihood of the need for surgical stabilization. The AO system emphasizes the importance of injuries to soft-tissue structures such as the posterior ligamentous complex, intervertebral discs, and anterior longitudinal ligament with respect to spine instability.
The most recent classification TLICS was developed by the Spine Trauma Study Group[15]. According to this system an injury severity score is calculated based on three components: Injury morphology, posterior ligamentous complex integrity, and neurologic status of the patient. In each category, a score is calculated with a smaller score assigned to an injury of lesser severity and a higher score is assigned to an injury of more severity requiring urgent management.
The total score serves as a guide to deciding surgical vs nonsurgical management. The TLICS emphasizes the role of magnetic resonance imaging in assessing PLC injury.
This article reviews the functional anatomy of the thoracolumbar spine, the AO and TLICS classification of spine injuries, highlights the CT and MR imaging appearances of spine injuries and a pattern-based approach for imaging interpretation and communication with spine surgeons.
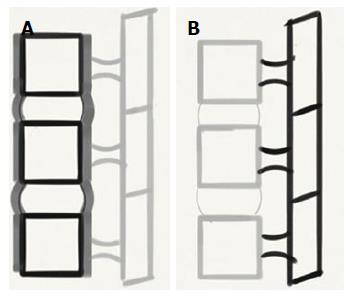
The two vertebrae and the interlinking soft tissues forms the functional component of the spine[16]. The anterior portion of the functional unit contains two aligned vertebral bodies, the intervertebral disc, and the anterior and posterior longitudinal ligaments. The posterior portion consists of the vertebral arches, facet joints and posterior elements (Figure 1). The posterior ligamentous complex (PLC) is comprised of the supraspinous ligament, interspinous ligaments, articular facet capsules and ligamentum flavum (Figure 2), serves as posterior tension band of the spinal column. The supraspinous ligament extends from C7 to the sacrum, connecting the tips of the spinous processes. The interspinous ligaments are membranous structures, which are fragile and thin, that connect the adjacent spinous processes. Both the supraspinous and interspinous ligaments have a high collagen content, and their high tensile strength limits flexion of the spine[16]. The ligamentum flavum is a thick broad structure that connects the laminae of the adjacent vertebrae. It has high elastin content and exerts a contractile force on the vertebral arches when it is elongated during flexion. The contractile force of the ligamentum flavum presses the vertebrae together and keeps them aligned[17]. The facet joints are continuations of the laminae and are covered with hyaline cartilage on their articulating surfaces. They are the primary elements that act against rotational or torsional forces. In active extension, the facets function as a fulcrum, thereby reducing the load on the anterior column[17,18]. Axial loading is supported primarily by the vertebral bodies and intervertebral discs[16]. Because the axis of rotation is immediately anterior to or just within the anterior half of the vertebral body in the erect posture, there is a constant counterbalancing of the posterior ligament and erector spinae muscle forces at rest and at motion to resist compressive forces on the vertebral bodies[19].
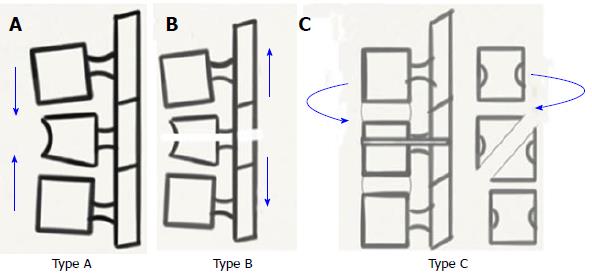
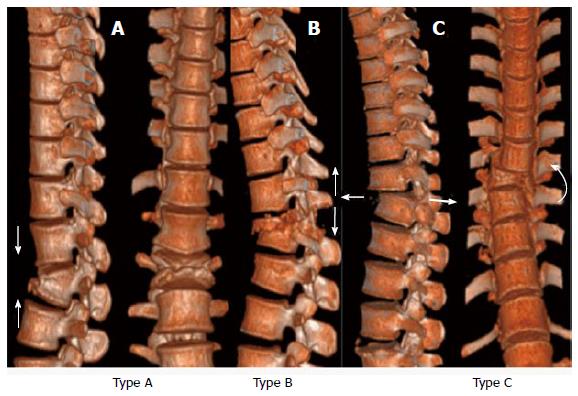
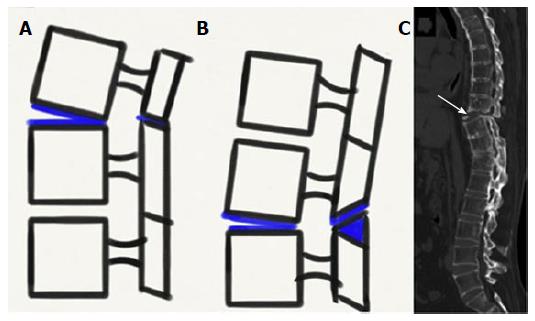
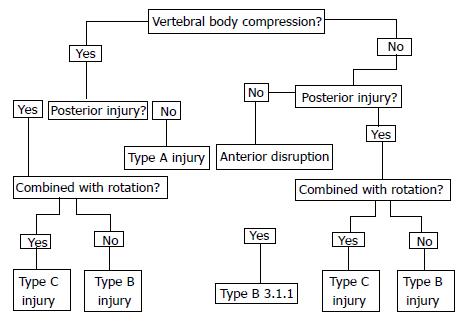
AO classifies thoracolumbar spine injuries into three categories based on the mechanical forces causing these injuries (Figures 3 and 4): (1) type A: Compressive force results in compression and burst injuries; (2) type B: Distraction (tensile) force results in transverse disruption injuries; and (3) type C: Axial torque forces results in translation or rotation injuries.
These three types (A, B, C) are further classified into 3 divisions and 3 subdivisions arranged in an increasing scale of morphological damage and instability (Table 1, Table 2 and Table 3).
| Type A: Vertebral body compression |
| A1. Impaction fractures |
| A1.1. Endplate impaction |
| A1.2. Wedge impaction fractures |
| A1.2.1. Superior wedge impaction fracture |
| A1.2.2. Lateral wedge impaction fracture |
| A1.2.3. Inferior wedge impaction fracture |
| A1.3. Vertebral body collapse |
| A2. Split fractures |
| A2.1. Sagittal split fracture |
| A2.2. Coronal split fracture |
| A2.3. Pincer fracture |
| A3. Burst fractures |
| A3.1. Incomplete burst fracture |
| A3.1.1. Superior incomplete burst fracture |
| A3.1.2. Lateral incomplete burst fracture |
| A3.1.3. Inferior incomplete burst fracture |
| A3.2. Burst-split fracture |
| A3.2.1. Superior burst-split fracture |
| A3.2.2. Lateral burst-split fracture |
| A3.2.3. Inferior burst-split fracture |
| A3.3. Complete burst fracture |
| A3.3.1. Pincer burst fracture |
| A3.3.2. Complete flexion burst fracture |
| A3.3.3. Complete axial burst fracture |
| Type B: Anterior and posterior element injury with distraction |
| B1. Posterior disruption predominantly ligamentous (flexion-distraction injury) |
| B1.1. With transverse disruption of the disc |
| B1.1.1. Flexion-subluxation |
| B1.1.2. Anterior dislocation |
| B1.1.3. Flexion-subluxation/anterior dislocation with fracture of the articular processes |
| B1.2. With type A fracture of the vertebral body |
| B1.2.1. Flexion-subluxation + type A fracture |
| B1.2.2. Anterior dislocation + type A fracture |
| B1.2.3. Flexion-subluxation/anterior dislocation with fracture of the articular processes + type A fracture |
| B2. Posterior disruption predominantly osseous (flexion-distraction injury) |
| B2.1. Transverse bicolumn fracture |
| B2.2. With transverse disruption of the disc |
| B2.2.1. Disruption through the pedicle and disc |
| B2.2.2. Disruption through the parsinterarticularis and disc (flexion- spondylolysis) |
| B2.3. With type A fracture of the vertebral body |
| B2.3.1. Fracture through the pedicle + type A fracture |
| B2.3.2. Fracture through the parsinterarticularis (flexion-spondylolysis) + type A fracture |
| B3. Anterior disruption through the disc (hyperextension-shear injury) |
| B3.1. Hyperextension-subluxations |
| B3.1.1. Without injury of the posterior column |
| B3.1.2. With injury of the posterior column |
| B3.2. Hyperextension-spondylolysis |
| B3.3. Posterior dislocation |
| Type C: Anterior and posterior element injury with rotation |
| C1. Type A injuries with rotation(compression injuries with rotation) |
| C1.1. Rotational wedge fracture |
| C1.2. Rotational split fractures |
| C1.2.1. Rotational sagittal split fracture |
| C1.2.2. Rotational coronal split fracture |
| C1.2.3. Rotational pincer fracture |
| C1.2.4. Vertebral body separation |
| C1.3. Rotational burst fractures |
| C1.3.1. Incomplete rotational burst fractures |
| C1.3.2. Rotational burst-split fracture |
| C1.3.3. Complete rotational burst fracture |
| C2. Type B injuries with rotation |
| C2.1. B1 injuries with rotation (flexion-distraction injuries with rotation) |
| C2.1.1. Rotational flexion subluxation |
| C2.1.2. Rotational flexion subluxation with unilateral articular process fracture |
| C2.1.3. Unilateral dislocation |
| C2.1.4. Rotational anterior dislocation without/with fracture of articular processes |
| C2.1.5. Rotational flexion subluxation without/with unilateral articular process + type A fracture |
| C2.1.6. Unilateral dislocation + type A fracture |
| C2.1.7. Rotational anterior dislocation without/with fracture of articular processes + type A fracture |
| C2.2. B2 injuries with rotation (flexion distraction injuries with rotation) |
| C2.2.1. Rotational transverse bicolumn fracture |
| C2.2.2. Unilateral flexion spondylolysis with disruption of the disc |
| C2.2.3. Unilateral flexion spondylolysis + type A fracture |
| C2.3. B3 injuries with rotation (hyperextension-shear injuries with rotation) |
| C2.3.1. Rotational hyperextension-subluxation without/with fracture of posterior vertebral elements |
| C2.3.2. Unilateral hyperextension-spondylolysis |
| C2.3.3. Posterior dislocation with rotation |
| C3. Rotational-shear injuries |
| C3.1. Slice fracture |
| C3.2. Oblique fracture |
Type A injuries involve the vertebral body. No or insignificant injury to posterior column is noted
Type B injuries indicate transverse disruptions with increase of the distance between adjacent vertebrae. In B1 and B2 the distance between posterior elements increases and in B3 distance between anterior vertebral elements increases. The B1 and B2 injuries are further sub grouped depending on the type of injury to the vertebral body.
Type C injury that results from axial torque, and is most frequently combined with either type A or B fractures. Therefore further subdivision of type C injuries depends on the associated type A/B subtype. While shear refers to force which is parallel to the surface in question, torsion refers to twisting force. Such shearing forces in association with twisting forces are also classified under type C category.
In general, type A fractures only affect a single column (anterior), where as type B and C fractures involve either two or all three columns.
The axial compression with or without flexion injury affects practically solely the vertebral body. Common imaging findings comprise: (1) loss of height of anterior part of vertebral body; (2) at times decrease in height of the posterior wall of the vertebral body, if it is fractured; (3) increased horizontal distance between pedicles due to a vertical split of the lamina; and (4) increased distance between spinous processes even if posterior wall is intact.
However, if the interspinous distance is considerably increased, it usually indicates that a posterior distraction injury is present. Additionally, although fracture fragments of the posterior wall may be displaced posteriorly into the spinal canal, no cranio-caudal migration or rotation of these fragments is seen. On a computed tomography (CT) scan, displaced fragment have sharp, dense, smooth posterior margin and indistinct anterior margin. Translational dislocation in the horizontal plane does not occur in type A injuries.
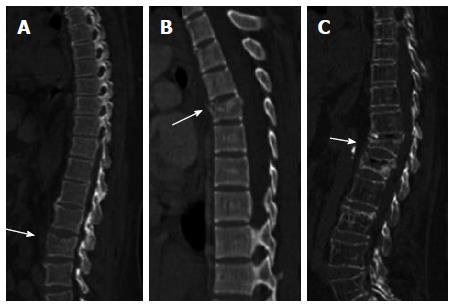
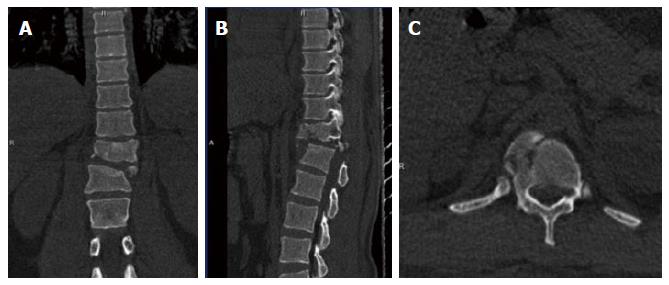
The type A1 (Figure 5) injuries are impaction fractures which results in deformity of the vertebral body due to compression of the cancellous bone There is no fragmentation of bone. These fractures are associated with intact posterior column, and there is no narrowing of spinal canal, therefore neurological deficit is very rare. These are stable injuries.
The subgroup A.1.1 comprises impaction of endplates; A.1.2 is a wedge impaction fracture and A.1.3 is a vertebral body collapse in osteoporotic spines.
The type A2 (Figure 6) injuries result from splitting of the vertebral body having either a sagittal split (A 2.1), a coronal split fracture(A 2.2) or may have disc material entrapped within (pincer) (A2.3). Neurological deficit is uncommon and posterior column is intact.
The highest frequency and severity among type A fractures is that of burst sub-type of fractures, i.e., A3-lesion (Figure 7) with the subgroups of A 3.1 (incomplete), A 3.2 (burst split) and A 3.3 (complete) burst fractures. In burst fractures, vertebral body is partly or completely fragmented resulting in centrifugal spread and retropulsion of fragments into the spinal canal. However, PLC is intact. A vertical split through the lamina or spinous process is usually the only injury to the arch, if present.
As mentioned earlier, type B injury is one in which there is transverse disruption with increase of the inter-vertebral distance either posteriorly (B1, B2) or anteriorly (B3). Type B1 and B2 indicate Flexion-distraction injuries where as type B3 is a hyperextension injury.
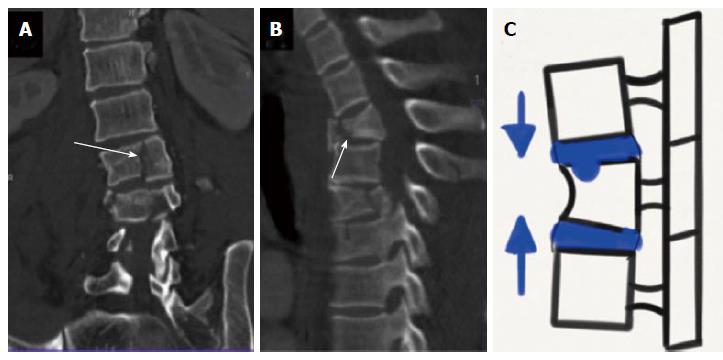
In B1 injuries, there is PLC disruption with subluxation/dislocation/fracture involving facet joints. B1 injuries are further subdivided into B1.1 where the anterior lesion is through soft tissues (through the disc) and B1.2 where the anterior lesion is bony (type A fracture) (Figure 8).
In B2 injuries (Figure 9), there is osseous posterior disruption, i.e., fracture line traversing through the laminae and pedicles or the isthmi. B2 injuries are further subdivided (as in B1 lesions) into B2.2 where the anterior lesion is through soft tissues (disc) and B2.3 where the anterior lesion is bony (type A fracture). The severity of instability and neurological deficit are slightly higher than in B1 injuries except for the transverse bicolumn fracture (B2.1).
Posterior disruption may involve the erector spinae muscles, fascia and even subcutaneous tissue in severe cases of B1 and B2 injuries.
The extent of instability varies from partial to complete, and there is a significantly higher incidence of neurological damage in comparison to type A injuries. Typical radiographic signs of B1 and B2 injuries include, kyphotic deformity with considerably increased inter-spinous distance; anterolisthesis; bilateral subluxation /dislocation/fracture involving facet joints or other posterior vertebral elements, avulsion fracture of the supraspinous ligament, anterior end plate shear chip fracture; avulsion of the posterior edge of the vertebral body.
When B1 and B2 injuries are seen in association with burst fractures, the fracture fragment is displaced posteriorly as well as cranially unlike in type A burst fractures. In contrast to type A burst fractures, posterior border is indistinct, and irregular than smooth, dense anterior border on CT scan. This sign is described as “inverse cortical sign”.
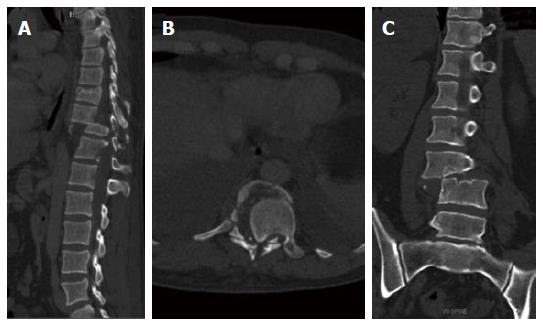
In B3 injuries (Hyperextension type injury) (Figure 10), the disruption in the transverse plane begins anteriorly and may proceed posteriorly depending on the severity of injury. Anterior displacement may be seen in B3.1 and B3.2 injuries, and posterior displacement is characteristic of B3.3 type injury.
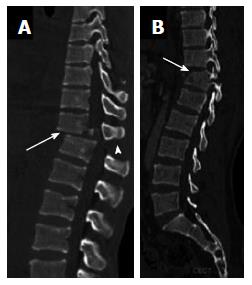
Type C injuries (Figures 11-13) are the most severe thoracolumbar injuries and are accompanied with the maximum degree of neurological deficit. Spinal injury is caused by compression of the spinal cord either by the fragments dislodged into the spinal canal with or without infringement of the spinal canal subsequent to translational displacement. Characteristic features include rotation of two vertebrae against each other, ALL and PLL disruption, disc disruption, articular process fracture (usually unilateral), fracture of transverse processes, rib fractures in proximity to their vertebral end, asymmetrical fractures of the neural arch, and irregular vertebral body fractures. Transverse process fractures are the major indicators of a rotational component of lumbar spine fractures. In presence of transverse process fractures, even if they appear isolated, one should always make a concentrated effort for identifying a concealed type injury. These typical findings of axial rotation are usually seen in association with either type A or type B lesions. The C1 lesion is a rotational injury combined with type A-lesion. The C2-lesion is axial rotation in combination with a type B injury whereas the C3-lesion is characterized by multilevel and shear injuries.
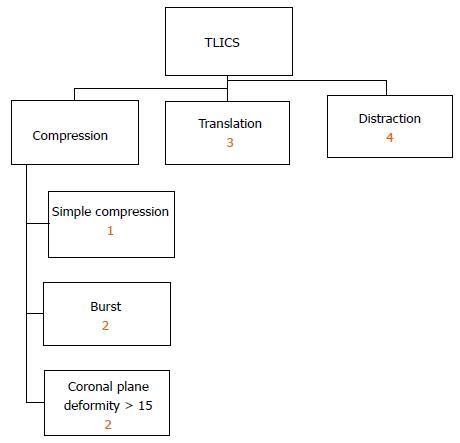
The TLICS, developed by the Spine Trauma Study Group, is both a scoring and a classification system (Figure 14). The system is based on three injury categories: (1) injury morphology; (2) PLC integrity; and (3) involvement of the neuraxis[15]. Within each category, subgroups are arranged from least to most significant, with a numeric value assigned to each injury pattern. Point values from these injury categories are totaled and a comprehensive severity score is calculated (Table 4). The TLICS helps in predicting biomechanical and neurologic spinal stability, thereby facilitating appropriate treatment recommendations. Joaquim et al[20], found correlation between the TLICS and the AO classification in a retrospective study.
| Injury category | Point value |
| Injury morphology | |
| Compression | 1 |
| Burst | 2 |
| Translation or rotation | 3 |
| Distraction | 4 |
| PLC Status | |
| Intact | 0 |
| Injury suspected or indeterminate | 2 |
| Injured | 3 |
| Neurologic status | |
| Intact | 0 |
| Nerve root involvement | 2 |
| Spinal cord or conusmedullaris injury | |
| Incomplete | 2 |
| Complete | 3 |
| Cauda equina syndrome | 3 |
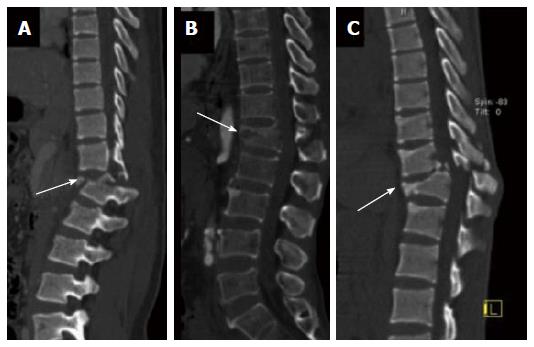
The TLICS uses straightforward morphologic descriptions based on findings at radiography, CT, or MR imaging. Compression injuries are described at imaging as a loss of vertebral body height or disruption of the endplate[21]. Milder forms of compression injuries implicate only the anterior part of the vertebral body and increasing severity results in burst fractures. In TLICS injury morphology scoring, compression injury receives 1 point and burst fracture receives 2 points. Compression injuries with a coronal plane distortion of over 15° are allocated a score of 2 points. Translation injuries (3 points) are defined at imaging as a horizontal displacement or rotation of one vertebral body with respect to another. These injuries result from torsional and shear forces and are characterized by rotation of the spinous processes, unilateral or bilateral facet fracture-dislocation, and vertebral subluxation[15]. Anteroposterior or sagittal translational instability is best seen on lateral radiographs or sagittal CT or MR images, while instability in the mediolateral or coronal plane is best seen on anteroposterior radiographs and coronal CT images. Distraction injuries (4 points) are identified at imaging as anatomic dissociation along the vertical axis. The disruption may involve anterior and posterior supporting ligaments, osseous elements, or a combination of both. When more than one single injury morphology is seen in combination, the single injury with the largest score is used. If the injury involves multiple levels of injury, each injury is scored independently[15].
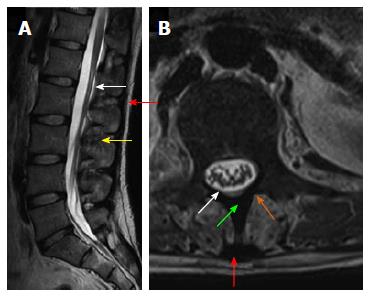
The PLC serves as the tension band of the spinal column and protects the spine from excessive flexion, rotation, translation, and distraction. Once disrupted, the injured segment of the PLC usually requires surgical intervention because of its poor healing potential. Without surgery, an injured PLC can result in kyphotic progression and subsequent vertebral collapse[22]. PLC integrity is categorized in the TLICS as intact, indeterminate, or disrupted. Disruption of the PLC is inferred on radiographs or CT images that show widening of the space between adjacent spinous processes, avulsion fracture of the superior or inferior aspects of contiguous spinous processes, widening of the facet joints, “naked” facet joints where the joint is uncovered, perched or dislocated facet joints, or vertebral body translation or rotation (Figure 15)[15,23]. Unlike CT, MR imaging allows direct visualization of the PLC and thus is considered the imaging standard of reference for detecting PLC injury. The ligamentum flavum and supraspinous ligament are best seen on sagittal T1- or T2-weighted MR images as low-signal-intensity continuous black stripes (Figure 2). The interspinous ligaments are best evaluated with sagittal short inversion time inversion-recovery (STIR) or fat-saturated T2-weighted sequences[24,25]. Axial fat-saturated T2-weighted MR images should be evaluated for facet capsular edema or fluid. The most reliable signs of PLC injury are disruption of the low-signal-intensity black stripe on sagittal T1- or T2-weighted MR images, a finding that indicates a supraspinous ligament or ligamentum flavum tear, and fluid in the facet capsules or edema in the interspinous region on fluid-sensitive MR images, findings that reflect a capsular or interspinous ligament injury, respectively[26]. An intact PLC is assigned a score of 0 points on the TLICS, and definite ligamentous injury is allocated 3 points. Isolated edema without clear ligament disruption is considered an indeterminate finding and is given a score of 2. A recent prospective analysis of MR imaging accuracy in diagnosis of traumatic PLC injuries has reported overall sensitivity and specificity of 91% and 100% respectively, with 100% accuracy in diagnosis of surgical fractures[27]. MR imaging accuracy has been reported to be higher for detecting supraspinous ligament and ligamentum flavum injuries, where the grading is typically either “intact” or “disrupted”, and slightly lower for interspinous ligament and facet capsular injuries, which fall into the “indeterminate” category because they may include a finding of edema without clear disruption[28].
The patient’s neurologic status is a critical indicator of the degree of spinal column injury. The TLICS defines five categories of neurologic status based on deficit severity and the patient’s recovery potential. Intact neurologic status at clinical examination is assigned a score of 0 points, 2 points are assigned to nerve injury or complete injury to the spinal cord. Contrary to expectation, a higher score (3 points) is allocated to incomplete spinal cord injury and cauda equina syndrome because patients with this type of injury may receive greater potential benefit from surgical decompression than patients with complete spinal cord injury or no initial neurologic injury[4]. Although clinical neurologic status cannot be directly determined at imaging, a cord or nerve root injury should be evaluated on MR images.
The TLICS total score helps surgeons evaluate injury severity and decide between surgical and nonsurgical management (Table 5). A TLICS total score of 3 or lower generally indicates nonsurgical management with immobilization with brace and active patient mobilization. A score of 5 or higher warrants surgical intervention with correction of deformity, neurologic decompression if necessary, and stabilization. A score of 4 indicates an intermediate zone where surgical or nonsurgical treatment depends on the surgeon’s clinical judgment and discretion[22]. In addition to helping determine the need for surgical intervention, the TLICS can help guide the surgical approach. The surgical approach should be based primarily on the patient’s neurologic status and the integrity of the PLC (Table 6). Patients with incomplete spinal cord injury with anterior compression will usually require an anterior surgical approach, while patients with an injured PLC will require posterior surgical stabilization. An anterior surgical approach allows more predictable and complete decompression of the neural elements, avoids damage to the posterior stabilizing structures, and reduces the risk of iatrogenic injury from posterior-approach manipulation of the dural sac[29]. Patients with both a neurologic deficit and an injured PLC often require a combined anterior and posterior surgical approach.
| TLICS score | Treatment recommendation |
| 0-3 | Nonsurgical |
| 4 | Nonsurgical or surgical |
| ≥ 5 | Surgical |
| Neurologic status | Surgical approach | |
| Intact PLC | Disrupted PLC | |
| Intact or nerve root injury | Posterior | Posterior |
| Incomplete cord injury | Anterior | Combined |
| Complete cord injury | Anterior or posterior | Combined or posterior |
Multidetector CT (MDCT), currently, is the imaging modality of choice, when there is a high or moderate index of suspicion of spine injury in a trauma setting. Radiographs are not usually obligatory prior to CT for acute spinal trauma, since a negative radiograph does not exclude getting a spine CT, if the clinical index is high. Recent literature has shown MDCT to be more accurate at identification of thoracolumbar injuries than plain X-ray[30,31]. In many level I trauma centers, including our center as well, CT has replaced plain radiographs as the initial modality for evaluation of spinal trauma[32]. CT images are acquired using thinnest collimation of 0.6 mm and images are reconstructed using both bone and soft tissue algorithms. Reformation is done in sagittal and coronal planes. Images are viewed in all three planes and in both soft tissue and bone window on CT workstation for final analysis and reporting. Intravenous contrast administration is indicated if the CT is done for suspected injuries in other body parts like chest, abdomen and pelvis. In such conditions the coverage of those scans should be modified to include the spine, eliminating twofold irradiation. If patients had undergone CT scan for other body parts, and with raw data still available, then every effort should be made to reconstruct images from the raw data and create reformatted images of the spine. The most critical drawback of CT modality is the failure to recognize ligamentous and spinal cord injuries.
Magnetic resonance imaging (MRI) is the modality of choice for identification of injuries to soft tissue structures like posterior ligamentous complex, spinal cord, intervertebral disks and adjacent muscles. The MR protocol for spine trauma includes sagittal T1W, sagittal T2W, and sagittal STIR images, as well as localized axial imaging (T1W and Gradient Echo). STIR sequence helps in detection of soft tissue injuries where as gradient echo sequence helps in identifying hemorrhagic contusion of the cord, which has prognostic implication. Any patient believed to have spinal cord injury deserves MR imaging examination at earliest possible opportunity. MR imaging has the ability to identify the location, extent, severity of the cord lesion and also cause of cord compression. These information are very useful from management point view where in surgical intervention may prevent further worsening[33]. Various types of spinal cord injuries seen include hemorrhagic contusion, non-hemorrhagic contusion, compression by epidural hematoma, a bone fragment or herniated disk material, and complete transection of the cord[34]. Of the spinal hematomas, those in epidural locations are most common. Preoperative diagnostic localization of the hematoma informs the surgeon of the need to open the dura or arachnoid, particularly in cases complicated by the coexistence of epidural and subdural hematomas. MR imaging also helps in prognostication. Neurological recovery is generally poor in patients with hemorrhagic contusion or cord transection than in patients with simple cord edema or non-hemorrhagic contusion[35,36].
Spine injuries are relatively uncommon with the frequency of 2% to 5% of all spine injuries[37]. The flexibility of spine, the growth potential and other biological variations between children and adults manifest in distinctive fracture patterns. The notion of spinal cord injury without radiological abnormality in children is known by the abbreviation SCIWORA. New MR sequences such as diffusion-weighted MR imaging (DWI) and diffusion tensor imaging may help in predicting the severity of spinal cord injury and prognosticate the recovery from SCIWORA[35].
A basic description of injury and extent includes the degree of comminution, percentage of vertebral height loss, retropulsion distance, percentage of canal compromise, and other contiguous or noncontiguous vertebral injuries. The anterior vertebral body compression percentage is the percentage of anterior vertebral body compression with respect to the average height of the anterior vertebral bodies immediately cephalad and caudal to the injury level[38,39]. Osseous retropulsion or canal effacement should be reported with the percentage of spinal canal narrowing. Retropulsion is the distance of a line drawn between the posterior margins of the adjacent vertebral bodies and the most posterior margin of the bone fragment. The distance between the posterior canal border and the anterior canal border represents the sagittal canal diameter. The posterior canal border is the point of convergence of the left and right laminae at the midline of the spinous process. The anterior canal border is the posterior extent of the retropulsed midvertebral body. The proportion of spinal canal compromise is estimated using the formula: a = (1 - x/y) × 100, where a = percentage of spinal canal compromise, x = midsagittal diameter of the spinal canal at the level of injury, and y = mean of the midsagittal diameter of the spinal canal one segment above and one segment below the level of injury[40]. PLC integrity is predicted based on CT findings of facet joint widening, interspinous distance widening, spinous process avulsion fracture, and vertebral body or facet subluxation or dislocation but it should be directly assessed with MRI if there is clinical concern[41,42]. Table 7 represents the checklist of findings to be evaluated in CT.
| Injury morphology |
| Primary injury pattern (compression, burst, translation, flexion-distraction) |
| Basic morphologic description of lesion |
| Vertebral height loss (approximate percentage) |
| Retropulsion with central spinal canal narrowing (approximate percentage) |
| Other contiguous or noncontiguous injuries |
| Degree of kyphosis |
| PLC injury predictors |
| Facet joint widening |
| Interspinous distance widening |
| Spinous process avulsion fracture |
| Vertebral body subluxation or dislocation |
The patient’s PLC status should be reported as injured, intact, or indeterminate. Findings of potential spinal cord injury, epidural hematoma, and other ligamentous or disk injuries are also recorded. Although the radiology report may include the TLICS total score if there is clear imaging evidence of neurologic injury, generally the report will not include the total score if the patient’s clinical neurologic status is unknown (Table 8).
| Osseous (similar to injury morphology noted at CT) and soft tissue injuries |
| PLC status (intact, indeterminate, or disrupted) |
| Supraspinous ligament |
| Ligamentumflavum |
| Interspinous ligaments |
| Facet capsule |
| Disks |
| Anterior and posterior longitudinal ligaments |
| Neurologic injuries |
| Spinal cord and conusmedullaris |
| Cauda equina |
| Nerve root injury |
| Epidural hematoma |
The AO classification is the broadest and the most rational classification system devised till date, which represents a gradual progression of morphological injury using which the extent of instability is determined. A higher category within this system thus indicates more severity, thus greater instability and therefore also gives an indication of the type of treatment and prognosis of the injury. This classification system can also be made concise without much loss of information, making it handy and easy to use in clinical practice. In short by facilitating recognition of a broad injury pattern, it provides an algorithm which serves as a useful guide in for radiologists/ clinicians in training (Figure 16).
The TLICS is the recent thoracolumbar injury grading scale to combine injury morphology, assessment of mechanical stability, and neurologic status into a single system which can guide injury management. The TLICS provides the best available predictor of surgical vs nonsurgical management. Radiologists should use the key components of the TLICS to analyze, evaluate, and report spine injuries and to help guide decisions about surgical management.
P- Reviewer: Chen F, Razek AAKA, Tsushima Y S- Editor: Tian YL L- Editor: A E- Editor: Wu HL
| 1. | Hu R, Mustard CA, Burns C. Epidemiology of incident spinal fracture in a complete population. Spine (Phila Pa 1976). 1996;21:492-499. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 320] [Cited by in RCA: 290] [Article Influence: 10.0] [Reference Citation Analysis (1)] |
| 2. | Wood KB, Buttermann GR, Phukan R, Harrod CC, Mehbod A, Shannon B, Bono CM, Harris MB. Operative compared with nonoperative treatment of a thoracolumbar burst fracture without neurological deficit: a prospective randomized study with follow-up at sixteen to twenty-two years. J Bone Joint Surg Am. 2015;97:3-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 101] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 3. | Gertzbein SD. Scoliosis Research Society. Multicenter spine fracture study. Spine (Phila Pa 1976). 1992;17:528-540. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 316] [Cited by in RCA: 268] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 4. | Sethi MK, Schoenfeld AJ, Bono CM, Harris MB. The evolution of thoracolumbar injury classification systems. Spine J. 2009;9:780-788. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 38] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 5. | Ferguson RL, Allen BL. A mechanistic classification of thoracolumbar spine fractures. Clin Orthop Relat Res. 1984;77-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 55] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | McAfee PC, Yuan HA, Fredrickson BE, Lubicky JP. The value of computed tomography in thoracolumbar fractures. An analysis of one hundred consecutive cases and a new classification. J Bone Joint Surg Am. 1983;65:461-473. [PubMed] |
| 7. | Watson-Jones R. The Results of Postural Reduction of Fractures of the Spine. J Bone JtSurg. 1938;20:567-586. |
| 8. | Chance GQ. Note on a type of flexion fracture of the spine. Br J Radiol. 1948;21:452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 281] [Cited by in RCA: 200] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 9. | Nicoll EA. Fractures of the dorso-lumbar spine. J Bone Joint Surg Br. 1949;31B:376-394. [PubMed] |
| 10. | Holdsworth F. Fractures, dislocations, and fracture-dislocations of the spine. J Bone Joint Surg Am. 1970;52:1534-1551. [PubMed] |
| 11. | Kelly RP, Whitesides TE. Treatment of lumbodorsal fracture-dislocations. Ann Surg. 1968;167:705-717. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 56] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 12. | Denis F. The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine (Phila Pa 1976). 1983;8:817-831. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1792] [Cited by in RCA: 1418] [Article Influence: 33.8] [Reference Citation Analysis (0)] |
| 13. | White AA, Panjabi MM. The basic kinematics of the human spine. A review of past and current knowledge. Spine (Phila Pa 1976). 1978;3:12-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 310] [Cited by in RCA: 247] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 14. | Magerl F, Aebi M, Gertzbein SD, Harms J, Nazarian S. A comprehensive classification of thoracic and lumbar injuries. Eur Spine J. 1994;3:184-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1406] [Cited by in RCA: 1135] [Article Influence: 36.6] [Reference Citation Analysis (0)] |
| 15. | Vaccaro AR, Lehman RA, Hurlbert RJ, Anderson PA, Harris M, Hedlund R, Harrop J, Dvorak M, Wood K, Fehlings MG. A new classification of thoracolumbar injuries: the importance of injury morphology, the integrity of the posterior ligamentous complex, and neurologic status. Spine (Phila Pa 1976). 2005;30:2325-2333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 597] [Cited by in RCA: 526] [Article Influence: 26.3] [Reference Citation Analysis (0)] |
| 16. | DirSci MN, Frankel VH. Basic Biomechanics of the Musculoskeletal System. 3 Sub ed. Philadelphia: Lippincott Williamsand Wilkins 2001; 496. |
| 17. | Audigé L, Bhandari M, Hanson B, Kellam J. A concept for the validation of fracture classifications. J Orthop Trauma. 2005;19:401-406. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 81] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 18. | Leone A, Guglielmi G, Cassar-Pullicino VN, Bonomo L. Lumbar intervertebral instability: a review. Radiology. 2007;245:62-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 178] [Cited by in RCA: 192] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 19. | Asmussen E, Klausen K. Form and function of the erect human spine. Clin Orthop. 1962;25:55-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 28] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 20. | Joaquim AF, Fernandes YB, Cavalcante RA, Fragoso RM, Honorato DC, Patel AA. Evaluation of the thoracolumbar injury classification system in thoracic and lumbar spinal trauma. Spine (Phila Pa 1976). 2011;36:33-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 51] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 21. | Patel AA, Dailey A, Brodke DS, Daubs M, Harrop J, Whang PG, Vaccaro AR. Thoracolumbar spine trauma classification: the Thoracolumbar Injury Classification and Severity Score system and case examples. J Neurosurg Spine. 2009;10:201-206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 58] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 22. | Rihn JA, Anderson DT, Harris E, Lawrence J, Jonsson H, Wilsey J, Hurlbert RJ, Vaccaro AR. A review of the TLICS system: a novel, user-friendly thoracolumbar trauma classification system. Acta Orthop. 2008;79:461-466. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 31] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 23. | Harris MB, Stelly MV, Villarraga ML, Schroeder AC, Thomas KA. Modeling of the naked facet sign in the thoracolumbar spine. J Spinal Disord. 2001;14:252-258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 24. | Haba H, Taneichi H, Kotani Y, Terae S, Abe S, Yoshikawa H, Abumi K, Minami A, Kaneda K. Diagnostic accuracy of magnetic resonance imaging for detecting posterior ligamentous complex injury associated with thoracic and lumbar fractures. J Neurosurg. 2003;99:20-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 39] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 25. | Lee JY, Vaccaro AR, Schweitzer KM, Lim MR, Baron EM, Rampersaud R, Oner FC, Hulbert RJ, Hedlund R, Fehlings MG. Assessment of injury to the thoracolumbar posterior ligamentous complex in the setting of normal-appearing plain radiography. Spine J. 2007;7:422-427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 71] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 26. | Pizones J, Zúñiga L, Sánchez-Mariscal F, Alvarez P, Gómez-Rice A, Izquierdo E. MRI study of post-traumatic incompetence of posterior ligamentous complex: importance of the supraspinous ligament. Prospective study of 74 traumatic fractures. Eur Spine J. 2012;21:2222-2231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 41] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 27. | Pizones J, Izquierdo E, Alvarez P, Sánchez-Mariscal F, Zúñiga L, Chimeno P, Benza E, Castillo E. Impact of magnetic resonance imaging on decision making for thoracolumbar traumatic fracture diagnosis and treatment. Eur Spine J. 2011;20 Suppl 3:390-396. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 78] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 28. | Pizones J, Sánchez-Mariscal F, Zúñiga L, Álvarez P, Izquierdo E. Prospective analysis of magnetic resonance imaging accuracy in diagnosing traumatic injuries of the posterior ligamentous complex of the thoracolumbar spine. Spine (Phila Pa 1976). 2013;38:745-751. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 43] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 29. | Wood KB, Khanna G, Vaccaro AR, Arnold PM, Harris MB, Mehbod AA. Assessment of two thoracolumbar fracture classification systems as used by multiple surgeons. J Bone Joint Surg Am. 2005;87:1423-1429. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 67] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 30. | Hauser CJ, Visvikis G, Hinrichs C, Eber CD, Cho K, Lavery RF, Livingston DH. Prospective validation of computed tomographic screening of the thoracolumbar spine in trauma. J Trauma. 2003;55:228-234; discussion 234-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 106] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 31. | Wintermark M, Mouhsine E, Theumann N, Mordasini P, van Melle G, Leyvraz PF, Schnyder P. Thoracolumbar spine fractures in patients who have sustained severe trauma: depiction with multi-detector row CT. Radiology. 2003;227:681-689. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 142] [Cited by in RCA: 111] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 32. | Looby S, Flanders A. Spine trauma. Radiol Clin North Am. 2011;49:129-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 56] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 33. | Forster BB, Koopmans RA. Magnetic resonance imaging of acute trauma of the cervical spine: spectrum of findings. Can Assoc Radiol J. 1995;46:168-173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 34. | Van Goethem JW, Ozsarlak O, Parizel PM. Cervical spine fractures and soft tissue injuries. JBR-BTR. 2003;86:230-234. [PubMed] |
| 35. | Shen H, Tang Y, Huang L, Yang R, Wu Y, Wang P, Shi Y, He X, Liu H, Ye J. Applications of diffusion-weighted MRI in thoracic spinal cord injury without radiographic abnormality. Int Orthop. 2007;31:375-383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 54] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 36. | Rajasekaran S, Kanna RM, Shetty AP. Diffusion tensor imaging of the spinal cord and its clinical applications. J Bone Joint Surg Br. 2012;94:1024-1031. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 35] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 37. | Reynolds R. Pediatric spinal injury. Curr Opin Pediatr. 2000;12:67-71. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 38] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 38. | Keynan O, Fisher CG, Vaccaro A, Fehlings MG, Oner FC, Dietz J, Kwon B, Rampersaud R, Bono C, France J. Radiographic measurement parameters in thoracolumbar fractures: a systematic review and consensus statement of the spine trauma study group. Spine (Phila Pa 1976). 2006;31:E156-E165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 133] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 39. | Vaccaro AR, Nachwalter RS, Klein GR, Sewards JM, Albert TJ, Garfin SR. The significance of thoracolumbar spinal canal size in spinal cord injury patients. Spine (Phila Pa 1976). 2001;26:371-376. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 43] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 40. | Mohanty SP, Bhat NS, Abraham R, Ishwara Keerthi C. Neurological deficit and canal compromise in thoracolumbar and lumbar burst fractures. J Orthop Surg (Hong Kong). 2008;16:20-23. [PubMed] |
| 41. | Khurana B, Sheehan SE, Sodickson A, Bono CM, Harris MB. Traumatic thoracolumbar spine injuries: what the spine surgeon wants to know. Radiographics. 2013;33:2031-2046. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 25] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 42. | Radcliff K, Su BW, Kepler CK, Rubin T, Shimer AL, Rihn JA, Harrop JA, Albert TJ, Vaccaro AR. Correlation of posterior ligamentous complex injury and neurological injury to loss of vertebral body height, kyphosis, and canal compromise. Spine (Phila Pa 1976). 2012;37:1142-1150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 64] [Article Influence: 4.9] [Reference Citation Analysis (0)] |