Published online Dec 28, 2015. doi: 10.4329/wjr.v7.i12.531
Peer-review started: June 1, 2015
First decision: August 4, 2015
Revised: October 20, 2015
Accepted: November 3, 2015
Article in press: November 4, 2015
Published online: December 28, 2015
Processing time: 213 Days and 4.6 Hours
AIM: To gather existing radiographic classifications of mandibular canals branching, considering the criteria on which these were based.
METHODS: The search for studies on mandibular canals based on imaging exams included literature reviews, epidemiological studies of prevalence, descriptive studies, or case reports. An electronic search in the MEDLINE (OvidSP), PubMed, EMBASE (OvidSP), Web of Science (Thompson Reuters), and Scopus (Elsevier) databases was performed, as well as a manual evaluation of the references of the selected articles. Combinations of key words were placed in each database. No restrictions were imposed regarding the year of publication or language. References collected in duplicate were removed by the authors. A table was drawn up, containing the included studies and respective interest data.
RESULTS: Six classifications of mandibular canals branching were selected for the present literature review. Four were based on two-dimensional radiographic exams, and two were performed based on three-dimensional tomographic exams. Three-dimensional classifications were determined based on the analysis found in the least number of exams, comparatively to two-dimensional studies. The prevalence of mandibular canal branching varied from 0% to 38.75% in the works based on two-dimensional exams, while those found in three-dimensional exams ranged from 15.6% to 65%. The studies were mostly referred to branches that began in the mandibular ramus. Just one classification considered the branches that began in the mandibular body region.
CONCLUSION: Three-dimensional exams appear to be the best method to view mandibular canal branching. Further studies are warranted to determine its true prevalence and questions concerning to associations.
Core tip: The identification of the mandibular canal and its branching are important for the planning of dental procedures. Due to the limitations of the two-dimensional exams, the three-dimensional view of the structures provided by computed tomography (CT) exams allowed for greater sensitivity for the detection and evaluation of mandibular canals. Nevertheless, some studies performed with CT exams continued to use the classifications based on two-dimensional exams. Given the variability of information on this aspect, this study aimed to gather existing information in an attempt to provide researchers and clinical professionals with a stronger basis for their studies and procedures.
- Citation: Castro MAA, Lagravere-Vich MO, Amaral TMP, Abreu MHG, Mesquita RA. Classifications of mandibular canal branching: A review of literature. World J Radiol 2015; 7(12): 531-537
- URL: https://www.wjgnet.com/1949-8470/full/v7/i12/531.htm
- DOI: https://dx.doi.org/10.4329/wjr.v7.i12.531
Mandibular canals are intraosseous ducts, normally unique in each hemimandible. These begin in the mandibular foramen, located in the lingual surfaces of the mandibular bodies and stretch until they emerge in the mental foramen, in a vestibular direction in the pre-molar region. Located inside of these canals is the inferior alveolar neurovascular bundle, the largest ramus of the mandibular division of the trigeminal nerve, responsible for the innervation of the posterior teeth, of the surrounding bone structure, and of the mucosa of the tongue coating of the posterior region[1].
The identification of the mandibular canal is important for the planning of a wide range of dental procedures, especially surgical procedures. The insertion of implants, extraction of impacted teeth, surgical planning of biopsies, enucleations of pathologies, orthognathic surgeries, and the defining of differential diagnoses are only a few examples of the clinical importance of its localization[2-7]. The occurrence of anatomical branching in mandibular canals constitutes a complicating factor and requires care for the proper planning of such cases in order to avoid inferior alveolar neurovascular bundle lesions.
As this study treats intraosseous anatomic structures, imaging exams are recognized as the main diagnostic resource for their localization and evaluation. The radiographic study of human fetal mandibles, performed by Chávez-Lomeli et al[8], detected that bifid or trifid canals are the main anatomical branching of the mandibular canals. For this reason, radiographic classifications were developed according to conventional exams. These systems considered their origins, localization, aspect, and direction as core criteria[1,9-12]. Due to the limitation inherent to the two-dimensional exams, Langlais et al[11] contemplated the possibility of the existence of undetected or undescribed canals.
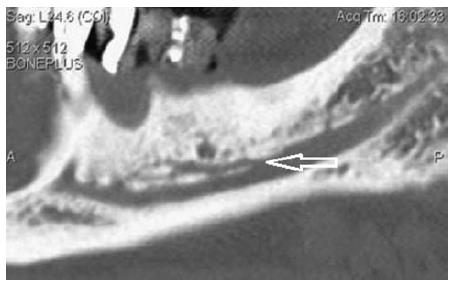
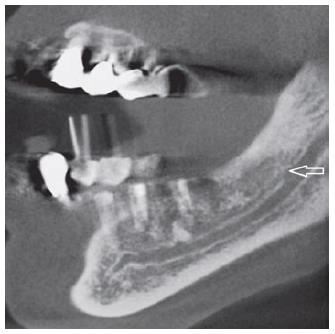
The three-dimensional view of the structures provided by computed tomography (CT) exams allowed for greater sensitivity for the detection and evaluation of mandibular canals, in addition to the three-dimensional classification of the mandibular canal. CT studies have presented different prevalence levels and other types of mandibular canal branches (Figure 1)[13-15]. Nevertheless, some studies performed with CT exams continued to use the classification of the variation of mandibular canals based on two-dimensional exams[14,16].
Bearing this finding in mind, the present review seeks to list the classifications and descriptions of the branching of existing mandibular canals, considering the applied diagnostic resources and the criteria on which these were based. Given the variability of information on this aspect, as well as the prevalence and classification, this study aimed to gather existing information in an attempt to provide researchers and clinical professionals with a stronger basis for their studies and procedures.
This literature review proposed the search for radiographic studies on mandibular canals in humans, based on conventional and digital two-dimensional exams and on CT exams. This work included literature reviews, epidemiological studies of prevalence, descriptive studies, or case reports. No letters to the editor, animal studies, abstracts, or personal opinions were included.
This study performed an electronic search in the PubMed, Embase, Web of Science (Thompson Reuters), and Scopus (Elsevier) databases. The references of the selected articles were also manually evaluated to detect relevant studies that might have been lost in the electronic search. A complementary search was also conducted using Google Search and Google Scholar search tools.
Combinations of key words were placed in each database, using the following key words: Mandible, mandibular nerve, inferior alveolar nerve, mandibular canal, bifid mandibular canal, bifid canals, radiography, panoramic radiography, cone-beam computed tomography, dental implant, and anatomic variation. No restrictions were imposed regarding the year of publication or language. References collected in duplicate were removed by the authors.
After having removed the duplicates, the abstracts of all of the chosen articles were read to verify the appropriateness of the theme. The main objective was to find articles that defined the classification of mandibular canal branching. After having selected the articles that met the eligibility criteria, these were read in full and incorporated into the present review.
A table of the included studies was drawn up, containing the following data: Authors’ names, year of publication, sample size, exam per image used in each study, prevalence of mandibular canal branching, and description of the defined classification, including the name adopted for the branches, the frequency of each type, the location of origin, aspect, direction, and end location.
Six radiographic classifications of the branching in mandibular canals were selected for the present literature review (Table 1)[1,9-12,14,15].
| Ref. | Exam | Sample | Prevalence (mandibular canal branching) | Classification | Frequency of the types | Region of origin | Aspect | Direction | Local of termination |
| Carter et al[10] (1971) | Unilateral radiographs and dissection | 80 | 38.75% | Type I | 61.25% | Ramus region, from a single Mandibular Foramen | Single large structure with very short dental branches | Superior to the tips of molars roots | Mental arborization |
| Type II | 13.75% (types 1 or 2) | Ramus region, from a single Mandibular Foramen | Substantially lower down, with dental branches given off more posteriorly, longer and oblique | Oblique, toward the tips of molars roots | Mental arborization | ||||
| Type III | 25% (types 2 or 3) | Ramus region, from a single Mandibular Foramen | Two large branches initiated posteriorly | Uppers like alveolar branches | Upper to the tips of the roots; Lower to mental forame | ||||
| Nortjé et al[1] (1977) | Panoramic radiographs | 3612 | 0.9 | Type Ia | 30.3% of duplication cases | Ramus region, from a single Mandibular Foramen | Two canals of a similar width (lower slightly narrower) | Inferior narrower | |
| Type Ib | Ramus region, from a single Mandibular Foramen | Double (Superior narrower) | Anterior | ||||||
| Type II | Ramus region, from a single Mandibular Foramen | Duplo (Superior shorter) | Anterior | Superior: toward 2nd and 3rd molars and inferior: toward mental foramen | |||||
| Type III | Ramus region, from separated Mandibular Foramens | Double (Join in the molars region) | Anterior | Molars region | |||||
| Nortjé et al[9] (1977) | 3612 | Type IV | Ramus region, from a single Mandibular Foramen | Double (Superior narrower than the main canal) | Anterior | Ramus region | |||
| Langlais et al[11] (1985) | Radiografias panorâmicas convencionais | 6000 | 0.95 | Type I | 38.6% | Ramus region, from a single Mandibular Foramen | Double (Superior shorter) | Anterior | 3rd molar and adjacente region |
| Type II | 54.4% | Ramus region, from a single Mandibular Foramen | Double (Joining anteriorly) | Anterior | Ramus or mandibular body regions | ||||
| Type III | 3.5% | Ramus region, from a single Mandibular Foramen | Double (Combination of types II and III) | Anterior | Ramus, retromolar ou 3rd molar regions | ||||
| Type IV | 3.5% | Ramus region, from separated Mandibular Foramens | Double (Joining anteriorly) | Inferior | Ramus region | ||||
| Kieser et al[12] (2005) | Oclusal and unilateral radiographs and dissection | 107 mandibles (25 radiographic exams) | 0% | Type I (detected by mean of dissections and radiographs) | Ramus region, from a single Mandibular Foramen | Single, without branches | Anterior | Mental foramen region | |
| Type II (detectado em dissecações) | Mandibular body region | Series of individual branches | Superior | Alveolar process (Edentulous mandibles) | |||||
| Type III (detectado em dissecações) | Molars region | Molar plexus | Superior | Molar region (Edentulous mandibles) | |||||
| Type IV (detectado em dissecações) | Distal and proximal regions | Distal and proximal plexus | Distal plexus forward. Proximal plelxus toward superior | Alveolar process (Edentulous mandibles) | |||||
| Naitoh et al[15] (2009) | CBCT | 122 | 65% | Type I Retromolar | 29.8% | Ramus region | Superior | Superior | Retromolar region |
| Type II Dental Canal (3º molar) | 7% | Ramus region | Superior | Anterior | Root Apex of the third molar | ||||
| Type II Dental Canal (2º molar) | 1.8% | Ramus region | Superior | Anterior | Root Apex of the second molar | ||||
| Type III Forward Canal (with confluence) | 4.5% | Ramus region | Superior (Joining to the main canal) | Anterior | Mandibular body | ||||
| Type III Forward Canal (without confluence) | 55.3% | Ramus region | Superior | Anterior | Mandibular body | ||||
| Type IV Buccal or lingual canal | 1.8% | Ramus region | Lateral | Inferior (Buccal or lingual) | Ramus region | ||||
| Kuribayashi et al[14] (2010) | CBCT | 301 unilateral exams from 252 patients | 15.60% | Less than 50% of the diameter of the main canal | 51% | Narrower (Less than 50% of the diameter of the main canal) | |||
| Equal or bigger than 50% of the diameter of the main canal | 49% | Equal or bigger than 50% of the diameter of the main canal |
Within the listed classification, four were defined by evaluating the canals and their branching in two-dimensional radiographic exams[1,9-12], and two were performed based on three-dimensional CT exams. Two of the classifications based on two-dimensional evaluations also conducted dissections of the anatomical parts[10,12].
The classifications based on two-dimensional exams were carried out by analyzing the samples with the highest number of exams (9717 in total, with an average of 2429.25 exams). Nortjé et al[1,9] evaluated 3612 panoramic radiographs, while Langlais et al[11] evaluated 6000 exams. Three-dimensional classifications were determined based on the analysis found in the least number of exams (374 in total, with an average of 187 CT exams).
The prevalence of the mandibular canal branching varied from 0% to 38.75% in the works based on two-dimensional exams, with an average of 10.15%. The prevalence of branches found in CT exams ranged from 15.6% to 65%, with an average of 40.3%.
Only the classification defined by Kieser et al[12] considered the branches that began in the mandibular body. All others referred to those initiated in the mandibular ramus.
Radiographic studies of the prevalence branching in mandibular canals presents variability, ranging from 0.08%[17] to 38.75%[10] when based on two-dimensional exams, and from 15.6%[14] to 65%[15]. This variability is related to the use of different methods, including panoramic radiographic evaluations and CT exams.
Claeys et al[18] warned that, although panoramic radiographs offer diagnostic conditions, the recognition of the branching in mandibular canals is rare. The authors defined that the cross-sectional cuts of the mandibular bodies, made possible through CT exams, were the best method to identify and locate their route. In an attempt to establish a more efficient method, capable of detecting the real prevalence and localization of these alterations, the CT exam has truly sparked great progress and has proven to be better as regards the limitations presented by the panoramic radiographs[3,15,19]. For this reason, it is recommended as the method of choice for the planning of a wide range of surgical procedures in dentistry[20].
However, the comparison among the methods reaches beyond that referent to the absolute prevalence of the occurrence of anatomical branching in mandibular canals. The comparison of the prevalence of different types of canals detected in panoramic radiographs and in the three-dimensional exams is of outmost importance due to the highest and lowest clinical significance that each type can represent. Furthermore, this comparison is made more difficult by the lack of a standardization of the classifications adopted in the different studies. The classification of the branches detected through tomographic exams (Figure 2)[15,16,21,22], though similar to those from two-dimensional exams, presented some differences and some new criteria[1,10-12].
In one three-dimensional exam, Kuribayashi et al[14], although they had defined an additional classification criterion by evaluating the diameter of the branches of the mandibular canals in relation to the main canal, primarily used the two-dimensional classification set forth by Nortjé et al[1] for detected canals. Their results pointed towards a greater prevalence of mandibular canal branching when compared to that found by Nortjé et al[1] Moreover, when compared to the diverse types of branches, a difference could also be observed regarding the most prevalent type of canal. While Nortjé et al[1] found greater prevalence for type I bifid canals (78.8%), Kuribayashi et al[14] found a greater prevalence of type II branches (13.2%).
Likewise, Correr et al[16] used the two-dimensional classification, as defined by Langlais et al[11], for a tomographic evaluation of mandibular canal branching. It was not possible to compare the prevalence of these studies, given that the samples evaluated by Correr et al[16] consisted, in its totality, of previously diagnosed exams referent to the occurrence of branches. However, as regards the proportion among the different types of branches, differences were observed. The type I standard was the most commonly detected in tomographic exams (72.6%), followed by the type II (19.3%), whereas the types I and II were detected in 38.6% and 54.4% of the panoramic radiographs, respectively. No type IV branches were detected in the scans.
These results reveal the existence of differences in the diagnostic accuracy of the methods. Nevertheless, the analysis of the different two- and three-dimensional classifications calls attention to some other relevant differences. As regards the evaluation of the diameters of the branches referent to the main canals[14], this can contribute to the greater or lesser relevance of the findings. While higher caliber branches may represent a greater risk of injury, one must also bear in mind that the branches of a lesser volume may be referent to nutrient canals, such as that found in the dissections performed by Carter and Keen[10].
Another aspect to be considered refers to the direction of the branches. Whereas the two-dimensional classification includes the description of the direction only in the anteroposterior and superoinferior directions, the three-dimensional classification set forth by Naitoh et al[15] is also concerned with the situation of the branches in the vestibular-lingual direction. This is an important factor to be considered in the surgical planning of cases[2,6,23,24] thus contributing to improvements in the definition of the localization of the surgical access route as well as better estimations of the risk of injury to the surrounding anatomical structures.
In conclusion, the detection of mandibular canal branching is important to determine the proper conduct to be taken with patients with dental problems, and imaging exams represent the standard method to view these alterations. Three-dimensional exams appear to be the best method, however, further studies are warranted to determine the true prevalence these alterations, some possible associated factor, and other such questions concerning three-dimensional systems.
Mandibular canals are intraosseous ducts that contain the inferior alveolar neurovascular bundle, responsible for the innervation of the posterior teeth and of the surrounding structures of the posterior region. The identification of the mandibular canal is important for the planning of a wide range of dental surgical procedures. The occurrence of mandibular canals branching constitutes a complicating factor and requires care for the proper planning of the procedures in order to avoid neurovascular lesions. The present review seeks to list the classifications and descriptions of the mandibular canal branching, considering the applied diagnostic resources and the criteria on which these were based. Given the variability of information on this aspect, this study aimed to gather existing information in an attempt to provide researchers and clinical professionals with a stronger basis for their studies and procedures.
Bifid or trifid canals are the main anatomical branching of the mandibular canals, according Chávez-Lomeli et al (1996). As the mandibular canals are intraosseous anatomic structures, imaging exams are recognized as the main diagnostic resource for their localization and evaluation. Radiographic classifications were mainly developed according to conventional exams. Due to the limitation of the two-dimensional exams, Langlais et al (1985) contemplated the possibility of the existence of undescribed canals.
The three-dimensional view of the structures provided by computed tomography (CT) exams allowed for greater sensitivity for the detection and evaluation of mandibular canals, in addition to the three-dimensional classification of the mandibular canal. CT studies have presented different prevalence levels and other types of mandibular canal branches. Nevertheless, some studies performed with CT exams continued to use the classification of the variation of mandibular canals based on two-dimensional exams.
This review suggests that three-dimensional exams appear to be the best method to view mandibular canal branching. Further studies are warranted to determine its true prevalence, new classifications and questions concerning to associations.
Both cone beam computed tomography and CT exams were equally referred as the generic term CT in this study. These types of three-dimensional exams have greater sensitivity for the detection of mandibular canal branching in comparison to two-dimensional exams and a comparative evaluation of the sensitivity of these methods was not a goal of this review.
In this paper the authors conducted an internet based search on the different radiographic classifications as regards the identification of the mandibular canal and its branching. The review is concise and well written one.
P- Reviewer: Abdel-Salam OME, Stoetzer M S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
| 1. | Nortjé CJ, Farman AG, Grotepass FW. Variations in the normal anatomy of the inferior dental (mandibular) canal: a retrospective study of panoramic radiographs from 3612 routine dental patients. Br J Oral Surg. 1977;15:55-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 138] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 2. | Juodzbalys G, Wang HL, Sabalys G. Injury of the Inferior Alveolar Nerve during Implant Placement: a Literature Review. J Oral Maxillofac Res. 2011;2:e1. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 59] [Cited by in RCA: 80] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 3. | Kim TS, Caruso JM, Christensen H, Torabinejad M. A comparison of cone-beam computed tomography and direct measurement in the examination of the mandibular canal and adjacent structures. J Endod. 2010;36:1191-1194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 40] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 4. | Hori M, Sato T, Kaneko K, Okaue M, Matsumoto M, Sato H, Tanaka H. Neurosensory function and implant survival rate following implant placement with nerve transpositioning: a case study. J Oral Sci. 2001;43:139-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | González-Santana H, Peñarrocha-Diago M, Guarinos-Carbó J, Balaguer-Martínez J. Pain and inflammation in 41 patients following the placement of 131 dental implants. Med Oral Patol Oral Cir Bucal. 2005;10:258-263. [PubMed] |
| 6. | Mizbah K, Gerlach N, Maal TJ, Bergé SJ, Meijer GJ. The clinical relevance of bifid and trifid mandibular canals. Oral Maxillofac Surg. 2012;16:147-151. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 39] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 7. | Simonton JD, Azevedo B, Schindler WG, Hargreaves KM. Age- and gender-related differences in the position of the inferior alveolar nerve by using cone beam computed tomography. J Endod. 2009;35:944-949. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 40] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 8. | Chávez-Lomeli ME, Mansilla Lory J, Pompa JA, Kjaer I. The human mandibular canal arises from three separate canals innervating different tooth groups. J Dent Res. 1996;75:1540-1544. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 103] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 9. | Nortjé CJ, Farman AG, de V Joubert JJ. The radiographic appearance of the inferior dental canal: an additional variation. Br J Oral Surg. 1977;15:171-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 28] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Carter RB, Keen EN. The intramandibular course of the inferior alveolar nerve. J Anat. 1971;108:433-440. [PubMed] |
| 11. | Langlais RP, Broadus R, Glass BJ. Bifid mandibular canals in panoramic radiographs. J Am Dent Assoc. 1985;110:923-926. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 102] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 12. | Kieser J, Kieser D, Hauman T. The course and distribution of the inferior alveolar nerve in the edentulous mandible. J Craniofac Surg. 2005;16:6-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 34] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 13. | Rouas P, Nancy J, Bar D. Identification of double mandibular canals: literature review and three case reports with CT scans and cone beam CT. Dentomaxillofac Radiol. 2007;36:34-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 46] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 14. | Kuribayashi A, Watanabe H, Imaizumi A, Tantanapornkul W, Katakami K, Kurabayashi T. Bifid mandibular canals: cone beam computed tomography evaluation. Dentomaxillofac Radiol. 2010;39:235-239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 84] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 15. | Naitoh M, Nakahara K, Hiraiwa Y, Aimiya H, Gotoh K, Ariji E. Observation of buccal foramen in mandibular body using cone-beam computed tomography. Okajimas Folia Anat Jpn. 2009;86:25-29. [PubMed] |
| 16. | Correr GM, Iwanko D, Leonardi DP, Ulbrich LM, Araújo MR, Deliberador TM. Classification of bifid mandibular canals using cone beam computed tomography. Braz Oral Res. 2013;27:510-516. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 17. | Grover PS, Lorton L. Bifid mandibular nerve as a possible cause of inadequate anesthesia in the mandible. J Oral Maxillofac Surg. 1983;41:177-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 71] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 18. | Claeys V, Wackens G. Bifid mandibular canal: literature review and case report. Dentomaxillofac Radiol. 2005;34:55-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 65] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 19. | Muinelo-Lorenzo J, Suárez-Quintanilla JA, Fernández-Alonso A, Marsillas-Rascado S, Suárez-Cunqueiro MM. Descriptive study of the bifid mandibular canals and retromolar foramina: cone beam CT vs panoramic radiography. Dentomaxillofac Radiol. 2014;43:20140090. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 38] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 20. | Tyndall DA, Price JB, Tetradis S, Ganz SD, Hildebolt C, Scarfe WC. Position statement of the American Academy of Oral and Maxillofacial Radiology on selection criteria for the use of radiology in dental implantology with emphasis on cone beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;113:817-826. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 255] [Cited by in RCA: 268] [Article Influence: 22.3] [Reference Citation Analysis (0)] |
| 21. | Orhan AI, Orhan K, Aksoy S, Ozgül O, Horasan S, Arslan A, Kocyigit D. Evaluation of perimandibular neurovascularization with accessory mental foramina using cone-beam computed tomography in children. J Craniofac Surg. 2013;24:e365-e369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 29] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 22. | Kang JH, Lee KS, Oh MG, Choi HY, Lee SR, Oh SH, Choi YJ, Kim GT, Choi YS, Hwang EH. The incidence and configuration of the bifid mandibular canal in Koreans by using cone-beam computed tomography. Imaging Sci Dent. 2014;44:53-60. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 49] [Cited by in RCA: 64] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 23. | Tay AB, Zuniga JR. Clinical characteristics of trigeminal nerve injury referrals to a university centre. Int J Oral Maxillofac Surg. 2007;36:922-927. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 105] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 24. | Miller CS, Nummikoski PV, Barnett DA, Langlais RP. Cross-sectional tomography. A diagnostic technique for determining the buccolingual relationship of impacted mandibular third molars and the inferior alveolar neurovascular bundle. Oral Surg Oral Med Oral Pathol. 1990;70:791-797. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 69] [Article Influence: 2.0] [Reference Citation Analysis (0)] |