Published online Oct 28, 2015. doi: 10.4329/wjr.v7.i10.336
Peer-review started: April 13, 2015
First decision: August 15, 2015
Revised: August 25, 2015
Accepted: September 10, 2015
Article in press: September 16, 2015
Published online: October 28, 2015
Processing time: 197 Days and 18.5 Hours
As one kind of infectious diseases of adrenal gland, adrenal tuberculosis can result in a life-threatening disorder which is called primary adrenal insufficiency (PAI) due to the destruction of adrenal cortex. Computed tomography (CT) and magnetic resonance imaging (MRI) play significant roles in the diagnosis of this etiology of PAI based on the CT and MRI appearances of the adrenal lesions. In this mini-review, we intend to study the CT and MRI features of adrenal tuberculosis, which could be helpful to both endocrinologist and radiologist to establish a definitive diagnosis for adrenal tuberculosis resulting in PAI.
Core tip: Adrenal tuberculosis is an important cause of the primary adrenal insufficiency (PAI) due to the destruction of adrenal cortex. Computed tomography (CT) and magnetic resonance imaging (MRI) play vital roles in the diagnosis of this etiology of PAI based on the CT and MRI appearances of the adrenal lesions. We herein discuss the CT and MRI technique, manifestations, the role of CT and MRI in a definitive diagnosis for adrenal tuberculosis resulting in PAI.
- Citation: Huang YC, Tang YL, Zhang XM, Zeng NL, Li R, Chen TW. Evaluation of primary adrenal insufficiency secondary to tuberculous adrenalitis with computed tomography and magnetic resonance imaging: Current status. World J Radiol 2015; 7(10): 336-342
- URL: https://www.wjgnet.com/1949-8470/full/v7/i10/336.htm
- DOI: https://dx.doi.org/10.4329/wjr.v7.i10.336
Primary adrenal insufficiency (PAI), manifesting as clinically inadequate production or action of glucocorticoids, is a life-threatening disorder when at least 90 percent of adrenal cortex has been destroyed[1,2]. As first depicted by Thomas Addison in 1855[3], the clinical manifestation of adrenal insufficiency were characterized by weakness, malaise, nausea, fatigue, anorexia and abdominal pain, together with orthostatic hypotension, constipation, weight losing, salt craving and characteristic hyperpigmentation of the skin[4-6]. The acute syndrome appears as a medical emergency since adrenal insufficiency may result in a severe hypotensive crisis and clouded sensorium[7]. But most of the symptoms are not so specific that may delay diagnosis.
Adrenal tuberculosis has been regarded as an important cause of PAI since the first reports by Thomas Addison[4,8]. During the past decades, incidence of adrenal tuberculosis has been greatly decreased due to the introduction of antituberculosis drugs. It is reported that PAI results from adrenal tuberculosis accounting for only 15%-20% patients in developed countries[9]. However, adrenal tuberculosis is still the primary cause of PAI in developing countries[10].
In the traditional diagnostic workup for adrenal insufficiency, basal detection of cortisol and adrenocorticotropic hormone (ACTH) is sufficient for the diagnosis in most cases, but rarely the corticotropin test is required in primary failure[11]. To confirm or rule out adrenal insufficiency, plasma cortisol can initially be measured between 8 and 9 am[12]. The morning plasma cortisol concentrations of ≤ 3 μg/dL (83 nmol/L) are indicative of adrenal insufficiency, whereas concentrations of ≥ 19 μg/dL (525 nmol/L) rule out this disorder[13,14]. The patients with plasma cortisol concentrations of 3-19 μg/dL need the ACTH stimulation test. Additionally, basal plasma corticotropin should be measured in patients with possible PAI, and it can be found that plasma corticotropin concentrations invariably exceed 100 pg/mL (22 pmol/L), even though the plasma cortisol concentration is in the normal range[1]. As for the ACTH stimulation test, the corticotrophin should be given intravenously or intramuscularly, and the serum cortisol level is usually measured before injection of 250 μg corticotrophin, and 30 or 60 min after this injection[12,15]. Adrenal function is considered to be normal if the basal or the post-corticotropin plasma cortisol concentration is at least 18 μg/dL (500 nmol/L), or at least 20 μg/dL (550 nmol/L)[12]. Most physicians use the highest plasma cortisol value before or after the injection of corticotropin as the criterion of normality and not the absolute increase in plasma cortisol after this injection.
With the laboratory diagnostic procedures, however, the causes of PAI caused by infectious diseases such as tuberculous adrenalitis cannot be recognized for appropriately essential therapy. Computed tomography (CT) and magnetic resonance imaging (MRI) play significant roles in evaluation of this etiology because the CT and MRI appearances of the underlying diseases depend not only on the pathologic nature but also on the duration of the illness and the type of treatment[2,16,17]. Thus, we reviewed the CT and MRI features of tuberculous adrenalitis resulting in PAI for appropriate treatments.
CT has been regarded as the modality of choice for identificating and characterizating tuberculous adrenalitis resulting in PAI[18-22]. Prior to CT scan, opacification of the bowel should be carried out routinely with oral contrast materials, and 800-1000 mL of 1% solution of sodium diatrizoate is used as oral contrast material in our hospital. To show the adrenal tuberculosis, 3 mm helical collimation with the field of view targeted to the adrenal gland and 3 mm reconstruction interval was recommended for clinical examination[18,23].
With the development of CT scanners, multidetector row CT (MDCT) has been used to depict the lesions of adrenal glands more and more frequently. In our institution, 16-row MDCT (Aquilion, Toshiba Medical Systems, Tokyo, Japan) has been used to detect the adrenal tuberculosis. Owing to the improvement of spatial resolution, small adrenal lesions can be detected on images of multiplanar reformation[9]. Dual-energy CT was first utilized to evaluate the attenuation difference of adrenal lesions by Gupta et al[24].
There are two CT techniques including non-contrast and contrast-enhanced CT. Non-contrast CT scan can be performed to illustrate the calcified tissue. For well depicting tuberculous adrenalitis in the majority of patients with adrenal insufficiency, the non-contrast CT examination should be followed by a contrast enhanced study, which is performed 60-80 s after intravenously administrating 80-100 mL of a contrast agent with 300 mg/mL of iodine at a rate of 3 mL/s by using a power injector.
MRI has been proven useful for evaluating the adrenal glands due to its advantages of superior contrast resolution and tissue characterization potential[25-28]. Body coil is used for both excitation and reception of MR signal. Adrenal MRI should include T1-weighted axial images for showing the adrenal anatomy in detail, and T2-weighted axial images for showing the lesions[29]. In our hospital, 1.5-T and 3.0-T MR scanners (Signa Excite; GE Medical System, Milwaukee, WI, United States) were used to detect the adrenal lesions, and adrenal MRI sequences include spin-echo or flash T1-weighted plain scan, and fast spin-echo T2-weighted scan. The adrenal MR images are acquired with a field of view of 35-45 cm, and 5-8 mm contiguous slice thickness. Enhanced T1-weighted images are acquired after intravenous administration of a bolus of 0.1 mmol/kg gadolinium diethylene triamine pentaacetic acid in our hospital. Because multiplanar imaging particularly including coronal section on all scanning series helps to detect extension of adrenal lesions into adjacent structures, the image planes are axial and coronal section on all scanning sequences at our institution. In addition, chemical-shift MRI with T1-weighted in-phase and out-of-phase gradient-echo pulse sequences and gadolinium-enhanced images is of great importance to evaluate the adrenal lesions[30].
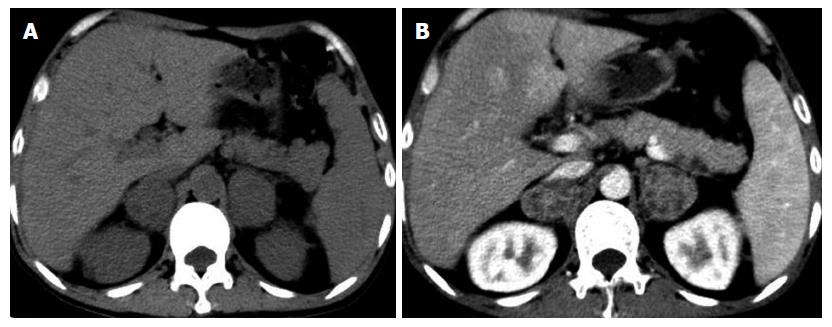
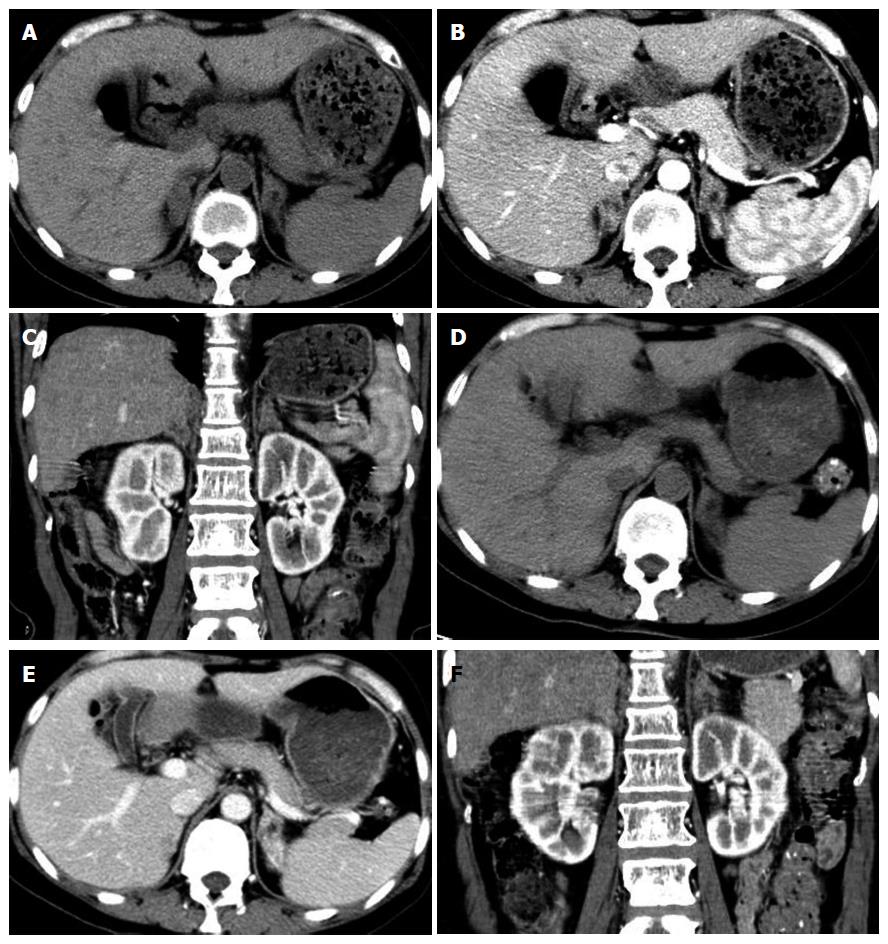
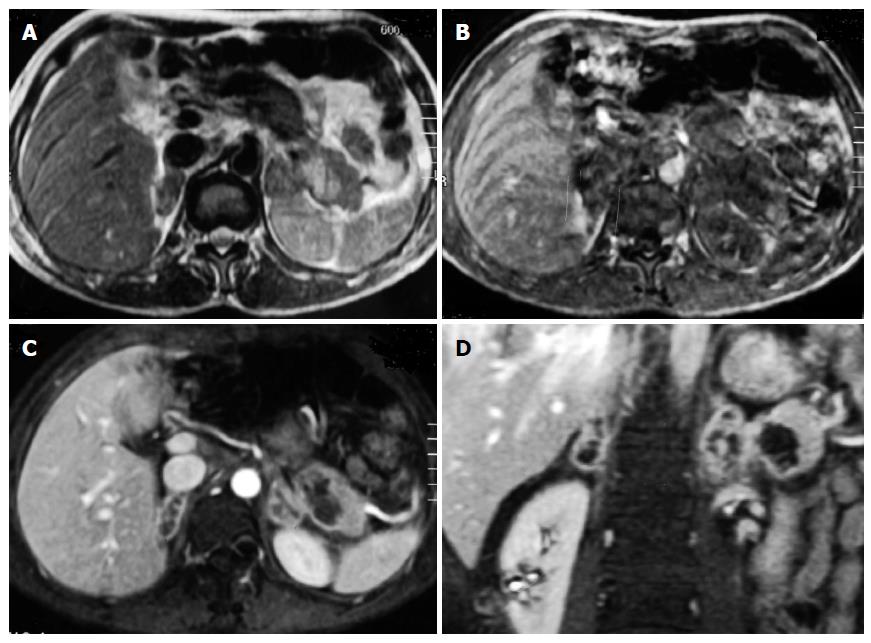
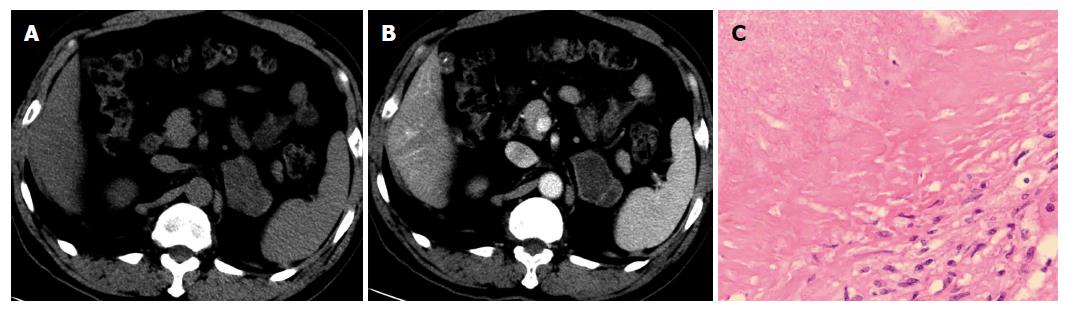
Adrenal tuberculosis occurs more commonly in bilateral glands (Figure 1, Figure 2 and Figure 3) than in unilateral gland (Figure 4), and the occurrence of bilateral involvement is more than 80%[2,9,23,31]. This predominant anatomic distribution may be explained by the reason that either of adrenal glands can be susceptible to infection by tubercle bacilli from the primary infection via hematogenous or lymph routes in equal incidence[8]. The pathological changes of adrenal tuberculosis include tuberculous granuloma, caseous necrosis, fibrosis, cicatrix and calcification, and different CT and MR manifestations reflect the corresponding pathological changes.
Concerning on the adrenal contour, it varies during the courses of the adrenal tuberculosis. At early stage, the mass-like enlargement of the adrenals with tuberculosis can be frequently found on CT and MRI (Figures 1-4), but the contour of adrenal glands preserve[2,9,23]. The radiologic appearances are pathologically based on the adrenals caseous necrosis area and tuberculous granuloma resulting from the destruction of the cortex by tuberculous mycobacteria[32]. The mean course might be approximately 3 years after the infection[9,23].
At late stage, the enlarged tuberculous adrenal glands lessen or normalize pathologically in size or configuration due to the increase of fibrosis, fibrous cicatrix, and calcified tissue in the glands[8,32,33]. When the continuous antituberculosis therapy is subsequently performed, the initially enlarged adrenal glands with smooth rounded contours become small with irregular margins (Figure 2) on follow-up CT and MRI[8,9,23,32,34-37]. The adrenal glands become atrophic, and the pathological mechanism can be that the gland tissue is almost completely substituted with fibrous tissue or calcification[2,35-37]. In general, small or atrophic adrenals indicate tuberculosis with long duration of adrenal insufficiency or quiescent adrenal tuberculosis, whereas enlarged adrenals suggest adrenal tuberculosis at early stage or active adrenal tuberculosis[32,33,38-41].
As for adrenal calcification, it may be diffuse, localized or punctuated, and its incidence increases with the course of adrenal tuberculosis. The calcification, predominantly occurring at late stage of tuberculosis, cannot be well illustrated on MRI but on CT, and the incidence of calcification is more than one half when the diagnosis of adrenal tuberculosis is made[33,41,42]. This manifestation may be due to the reason that the encapsulated granuloma becomes quiescent, and calcium salts deposit within the caseous regions at this stage[9,23].
Another manifestation of adrenal tuberculosis is the density and enhancement on CT, or the signal intensity and enhancement on MRI at different stages. At early stage, the enlarged adrenals (Figures 1, 2 and 4) demonstrate central low density or homogeneous density on non-contrast CT scans, and peripheral enhancement with low density in the central area is observed on the contrast-enhanced scans in most of patients with adrenal tuberculosis[9,23,42]. On MRI, the involved adrenals (Figure 3) appear as hypointense or isointense on T1-weighed images and hyperintense on T2-weighted images, and the glands with caseous necrosis in the central area appear as peripheral rim enhancement on non-contrast CT[2]. The enlarged adrenals without necrosis tissues in central zone display homogeneous enhancement on contrast-enhanced scans[9]. The radiologic features reflect the pathologic feature of central caseous necrosis surrounded by fibrous tissue and granulomatous inflammatory tissue[32,33,41,42].
If continuous antituberculosis therapy has been carried out, the adrenal lesions demonstrate homogeneous density (Figures 2D-F) or calcification in the center on CT scans, and the specific center with hypointense or isointense on T2 weighed images would appear on MRI due to a large amount of fibrous tissue, cicatrix, or calcification[2,35-37]. When the lesions are completely substituted with fibrous tissue or calcification, the glands would show hypointense on all MR images[2]. The probability of the presence of peripheral rim enhancement decreases on enhanced CT and MRI with the decrease of granuloma and caseating necrosis at late stage[9,23]. In addition, contrast enhancement of adrenal tuberculosis could be quantitatively measured. As demonstrated by Ma et al[9], the difference in average density of the central zone of the enlarged adrenal glands between nonenhanced and enhanced CT scans is significantly less than that of peripheral zone (29 ± 2 HU vs 36 ± 11 HU).
Generally, the contrast-enhanced CT and MRI features of adrenal tuberculosis can provide information for the adrenal tuberculosis resulting in PAI, and might be useful for indicating the clinical duration of adrenal tuberculosis. However, some radiological features of adrenal tuberculosis could be similar with those of adrenal fungal infections such as adrenal histoplasmosis. The diagnosis of adrenal tuberculosis should be considered in patients who has the CT and MRI features, and who has resided in an area where tuberculosis is not well controlled. Sometimes, biopsy is necessary for the diagnosis.
Adrenal tuberculosis can result in PAI. CT and MRI play important roles in the diagnosis of adrenal tuberculosis. Speed and availability of CT are of great importance to the diagnosis, and MRI can avoid the ionizing radiation and perform multiparametric imaging and good spatial resolution. The radiological tools can well depict adrenal tuberculosis based on their pathologic nature and the duration of the illness, and the type of treatment. Understanding the imaging characteristics of adrenal tuberculosis is of great importance for correcting diagnosis and timely essential treatment of PAI secondary to adrenal tuberculosis.
P- Reviewer: Chu JP, Garcia-Elorriaga G, Gumustas OG, Kumar J, Stanciu C S- Editor: Qiu S L- Editor: A E- Editor: Jiao XK
| 1. | Oelkers W. Adrenal insufficiency. N Engl J Med. 1996;335:1206-1212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 597] [Cited by in RCA: 507] [Article Influence: 17.5] [Reference Citation Analysis (0)] |
| 2. | Zhang XC, Yang ZG, Li Y, Min PQ, Guo YK, Deng YP, Dong ZH. Addison’s disease due to adrenal tuberculosis: MRI features. Abdom Imaging. 2008;33:689-694. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 3. | Addison T. On the constitutional and local effects of disease of the supra-renal capsules (special ed 9th), 1855; Samuel Highley, London. . |
| 4. | Løvås K, Husebye ES. Addison’s disease. Lancet. 2005;365:2058-2061. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 38] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 5. | Kong MF, Jeffcoate W. Eighty-six cases of Addison’s disease. Clin Endocrinol (Oxf). 1994;41:757-761. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 115] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 6. | Nomura K, Demura H, Saruta T. Addison’s disease in Japan: characteristics and changes revealed in a nationwide survey. Intern Med. 1994;33:602-606. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 36] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 7. | Hahner S, Loeffler M, Bleicken B, Drechsler C, Milovanovic D, Fassnacht M, Ventz M, Quinkler M, Allolio B. Epidemiology of adrenal crisis in chronic adrenal insufficiency: the need for new prevention strategies. Eur J Endocrinol. 2010;162:597-602. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 203] [Cited by in RCA: 227] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 8. | Dunlop D. Eighty-six cases of addison’s disease. Br Med J. 1963;2:887-891. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 135] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 9. | Ma ES, Yang ZG, Li Y, Guo YK, Deng YP, Zhang XC. Tuberculous Addison’s disease: morphological and quantitative evaluation with multidetector-row CT. Eur J Radiol. 2007;62:352-358. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 10. | Kinjo T, Higuchi D, Oshiro Y, Nakamatsu Y, Fujita K, Nakamoto A, Owan I, Miyagi S, Kuba M, Fujita J. Addison’s disease due to tuberculosis that required differentiation from SIADH. J Infect Chemother. 2009;15:239-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Schmidt IL, Lahner H, Mann K, Petersenn S. Diagnosis of adrenal insufficiency: Evaluation of the corticotropin-releasing hormone test and Basal serum cortisol in comparison to the insulin tolerance test in patients with hypothalamic-pituitary-adrenal disease. J Clin Endocrinol Metab. 2003;88:4193-4198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 98] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 12. | Grinspoon SK, Biller BM. Clinical review 62: Laboratory assessment of adrenal insufficiency. J Clin Endocrinol Metab. 1994;79:923-931. [PubMed] |
| 13. | Hägg E, Asplund K, Lithner F. Value of basal plasma cortisol assays in the assessment of pituitary-adrenal insufficiency. Clin Endocrinol (Oxf). 1987;26:221-226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 159] [Cited by in RCA: 159] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 14. | Deutschbein T, Unger N, Mann K, Petersenn S. Diagnosis of secondary adrenal insufficiency: unstimulated early morning cortisol in saliva and serum in comparison with the insulin tolerance test. Horm Metab Res. 2009;41:834-839. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 38] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 15. | Oelkers W, Diederich S, Bähr V. Diagnosis and therapy surveillance in Addison’s disease: rapid adrenocorticotropin (ACTH) test and measurement of plasma ACTH, renin activity, and aldosterone. J Clin Endocrinol Metab. 1992;75:259-264. [PubMed] |
| 16. | Kawashima A, Sandler CM, Fishman EK, Charnsangavej C, Yasumori K, Honda H, Ernst RD, Takahashi N, Raval BK, Masuda K. Spectrum of CT findings in nonmalignant disease of the adrenal gland. Radiographics. 1998;18:393-412. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 75] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 17. | Charmandari E, Nicolaides NC, Chrousos GP. Adrenal insufficiency. Lancet. 2014;383:2152-2167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 387] [Cited by in RCA: 402] [Article Influence: 36.5] [Reference Citation Analysis (0)] |
| 18. | Mayo-Smith WW, Boland GW, Noto RB, Lee MJ. State-of-the-art adrenal imaging. Radiographics. 2001;21:995-1012. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 263] [Cited by in RCA: 198] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 19. | Peña CS, Boland GW, Hahn PF, Lee MJ, Mueller PR. Characterization of indeterminate (lipid-poor) adrenal masses: use of washout characteristics at contrast-enhanced CT. Radiology. 2000;217:798-802. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 309] [Cited by in RCA: 267] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 20. | Arlt W, Allolio B. Adrenal insufficiency. Lancet. 2003;361:1881-1893. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 652] [Cited by in RCA: 587] [Article Influence: 26.7] [Reference Citation Analysis (0)] |
| 21. | Neary N, Nieman L. Adrenal insufficiency: etiology, diagnosis and treatment. Curr Opin Endocrinol Diabetes Obes. 2010;17:217-223. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 112] [Cited by in RCA: 97] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 22. | Husebye E, Løvås K. Pathogenesis of primary adrenal insufficiency. Best Pract Res Clin Endocrinol Metab. 2009;23:147-157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 39] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 23. | Guo YK, Yang ZG, Li Y, Ma ES, Deng YP, Min PQ, Yin LL, Hu J, Zhang XC, Chen TW. Addison’s disease due to adrenal tuberculosis: contrast-enhanced CT features and clinical duration correlation. Eur J Radiol. 2007;62:126-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 50] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 24. | Gupta RT, Ho LM, Marin D, Boll DT, Barnhart HX, Nelson RC. Dual-energy CT for characterization of adrenal nodules: initial experience. AJR Am J Roentgenol. 2010;194:1479-1483. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 85] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 25. | Gnannt R, Fischer M, Goetti R, Karlo C, Leschka S, Alkadhi H. Dual-energy CT for characterization of the incidental adrenal mass: preliminary observations. AJR Am J Roentgenol. 2012;198:138-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 59] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 26. | Schultz CL, Haaga JR, Fletcher BD, Alfidi RJ, Schultz MA. Magnetic resonance imaging of the adrenal glands: a comparison with computed tomography. AJR Am J Roentgenol. 1984;143:1235-1240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 58] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 27. | Glazer GM, Woolsey EJ, Borrello J, Francis IR, Aisen AM, Bookstein F, Amendola MA, Gross MD, Bree RL, Martel W. Adrenal tissue characterization using MR imaging. Radiology. 1986;158:73-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 135] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 28. | Reinig JW, Doppman JL, Dwyer AJ, Johnson AR, Knop RH. Adrenal masses differentiated by MR. Radiology. 1986;158:81-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 118] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 29. | Outwater EK, Siegelman ES, Huang AB, Birnbaum BA. Adrenal masses: correlation between CT attenuation value and chemical shift ratio at MR imaging with in-phase and opposed-phase sequences. Radiology. 1996;200:749-752. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 111] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 30. | Woo S, Cho JY, Kim SY, Kim SH. Adrenal adenoma and metastasis from clear cell renal cell carcinoma: can they be differentiated using standard MR techniques? Acta Radiol. 2014;55:1120-1128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 31. | Bilbey JH, McLoughlin RF, Kurkjian PS, Wilkins GE, Chan NH, Schmidt N, Singer J. MR imaging of adrenal masses: value of chemical-shift imaging for distinguishing adenomas from other tumors. AJR Am J Roentgenol. 1995;164:637-642. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 105] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 32. | Efremidis SC, Harsoulis F, Douma S, Zafiriadou E, Zamboulis C, Kouri A. Adrenal insufficiency with enlarged adrenals. Abdom Imaging. 1996;21:168-171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 23] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 33. | Vita JA, Silverberg SJ, Goland RS, Austin JH, Knowlton AI. Clinical clues to the cause of Addison’s disease. Am J Med. 1985;78:461-466. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 86] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 34. | Ammini AC, Gupta R, Mukopadhyay C, Shah P, Sandhu MS, Vijayaraghavan M, Berry M. Computed tomography morphology of the adrenal glands of patients with Addison’s disease. Australas Radiol. 1996;40:38-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 35. | Fan ZM, Zeng QY, Huo JW, Bai L, Liu ZS, Luo LF, Yang JC, Zhou XH. Macronodular multi-organs tuberculoma: CT and MR appearances. J Gastroenterol. 1998;33:285-288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 33] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 36. | Murata Y, Yamada I, Sumiya Y, Shichijo Y, Suzuki Y. Abdominal macronodular tuberculomas: MR findings. J Comput Assist Tomogr. 1996;20:643-646. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 32] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 37. | Kawamori Y, Matsui O, Kitagawa K, Kadoya M, Takashima T, Yamahana T. Macronodular tuberculoma of the liver: CT and MR findings. AJR Am J Roentgenol. 1992;158:311-313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 56] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 38. | Gülmez I, Keleştimur F, Durak AC, Ozesmi M. Changes in the size of adrenal glands in acute pulmonary tuberculosis with therapy. Endocr J. 1996;43:573-576. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 39. | Doppman JL, Gill JR, Nienhuis AW, Earll JM, Long JA. CT findings in Addison’s disease. J Comput Assist Tomogr. 1982;6:757-761. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 54] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 40. | Villabona CM, Sahun M, Ricart W, Serres X, Maroto A, Fernandez-Real JM, Gómez JM, Soler J. Tuberculous Addison’s disease. Utility of CT in diagnosis and follow-up. Eur J Radiol. 1993;17:210-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 41. | Wang YX, Chen CR, He GX, Tang AR. CT findings of adrenal glands in patients with tuberculous Addison’s disease. J Belge Radiol. 1998;81:226-228. [PubMed] |
| 42. | Yang ZG, Guo YK, Li Y, Min PQ, Yu JQ, Ma ES. Differentiation between tuberculosis and primary tumors in the adrenal gland: evaluation with contrast-enhanced CT. Eur Radiol. 2006;16:2031-2036. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 32] [Article Influence: 1.7] [Reference Citation Analysis (0)] |