Published online Sep 28, 2014. doi: 10.4329/wjr.v6.i9.636
Revised: March 18, 2014
Accepted: July 15, 2014
Published online: September 28, 2014
Processing time: 257 Days and 15 Hours
Transcranial sonography (TCS) is an ultrasound-based imaging technique, which allows the identification of several structures within the brain parenchyma. In the past it has been applied for bedside assessment of different intracranial pathologies in children. Presently, TCS is also used on adult patients to diagnose intracranial space occupying lesions of various origins, intracranial hemorrhage, hydrocephalus, midline shift and neurodegenerative movement disorders, in both acute and chronic clinical settings. In comparison with conventional neuroimaging methods (such as computed tomography or magnetic resonance), TCS has the advantages of low costs, short investigation times, repeatability, and bedside availability. These noninvasive characteristics, together with the possibility of offering a continuous patient neuro-monitoring system, determine its applicability in the monitoring of multiple emergency and non-emergency settings. Currently, TCS is a still underestimated imaging modality that requires a wider diffusion and a qualified training process. In this review we focused on the main indications of TCS for the assessment of acute neurologic disorders in intensive care unit.
Core tip:Transcranial sonography (TCS) is an ultrasound-based imaging technique, which allows the identification of several structures within the brain parenchyma, not only in neonates, but also in adult patients. It can be used to diagnose intracranial space occupying lesions of various origins, intracranial hemorrhage, hydrocephalus and midline shift. In comparison with computed tomography scan, TCS has the advantages of low costs, short investigation times, repeatability, and bedside availability. These noninvasive characteristics, together with the possibility of offering a continuous patient neuro-monitoring system, determine its applicability in multiple emergency settings.
- Citation: Caricato A, Pitoni S, Montini L, Bocci MG, Annetta P, Antonelli M. Echography in brain imaging in intensive care unit: State of the art. World J Radiol 2014; 6(9): 636-642
- URL: https://www.wjgnet.com/1949-8470/full/v6/i9/636.htm
- DOI: https://dx.doi.org/10.4329/wjr.v6.i9.636
In the last years, due to new ultrasounds technology, echographic imaging of the brain parenchyma has been obtained not only in children, but also in adults. Several authors have found a good visualization of cerebral structures using transcranial B-mode ultrasounds through a transtemporal approach [transcranial sonography (TCS)].
In the past, the skull was considered unsuitable for sonographic examination because of its thick structure. Aaslid et al[1] described a “temporal window”, the thinner part of the temporal bone located just above the zygomatic arch, and observed that low-frequency ultrasounds may well penetrate inside the skull in this zone. Since then, TCS has been proposed for bedside identification of many different intracranial pathologies, in both acute and chronic settings, such as intracranial space occupying lesions of various origins (intracranial hemorrhage), hydrocephalus, midline shift and neurodegenerative movement disorders. In comparison with conventional neuroimaging methods such as computed tomography (CT) and Magnetic Resonance, TCS has the advantages of low costs, short investigation times, repeatability, and bedside availability. These noninvasive characteristics, together with the possibility of offering a continuous patient neuro-monitoring system, determine its wide applicability in the monitoring of multiple emergency settings including Intensive Care Units, trauma centers and the context of emergency transportations (i.e., aeromedical flights, helicopter transfers, etc.)[2,3].
The main limitation of TCS is its dependence to an adequate temporal acoustic window. In fact, between 5%-18% of patients the exam is not feasible due to a particularly thick structure of the temporal bone[4]. Higher percentage of failure rate was described in people of Asian ethnic origin[5].
In this context, patients with skull defects, such as those who underwent decompressive craniectomy, allow a very accurate assessment of brain parenchyma by TCS[2].
In this review, we summarize the usefulness of this technique for the assessment of acute neurological disorders in the intensive care unit, describing proposed indications, technical considerations, main advantages and limitations.
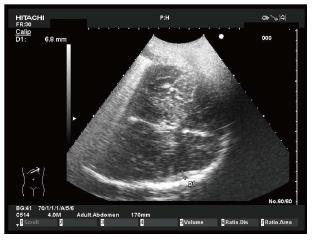
The patient lies in a supine position, and the examiner usually sits at the head of the examination table, firmly positioning the ultrasound probe on the temporal zone. The location of the acoustic window may be variable. In fact, it can be either located in the anterior part of the temporal bone, close to the vertical portion of the zygomatic bone, or, more frequently, posteriorly and close to the pinna of the ear. A low-frequency probe with a 2.0-2.5 MHz phased array transducers is appropriate to insonate the brain through the intact skull. In case of decompressive craniectomy, a standard abdominal convex phased-array probe with a mean central frequency of 4 MHz and an abdominal setting can be used.
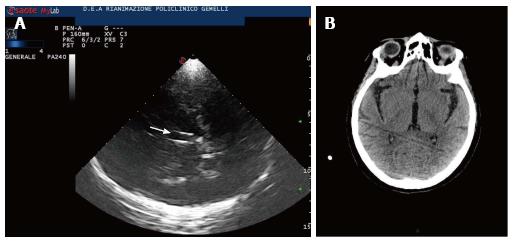
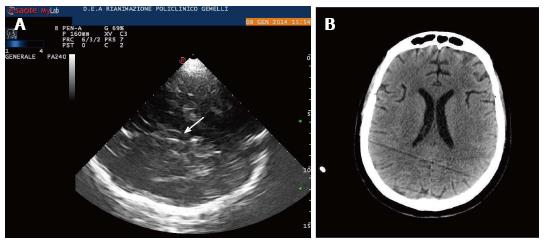
Usually, the examination starts with the identification of the mesencephalic brainstem in the axial plane parallel to the “orbitomeatal line”, so to obtain CT-like images (Midbrain transverse scan; Figures 1 and 2). The butterfly-shaped mesencephalic brainstem surrounded by the echogenic basal cisterns is the “landmark” of this scan, and can be observed in 90%-95% of the patients.
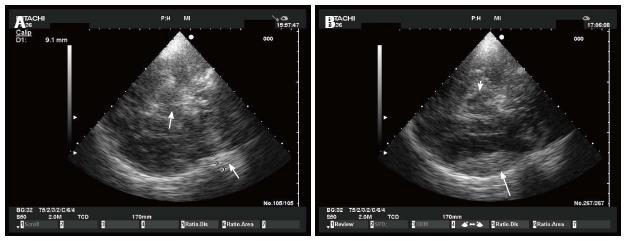
Tilting the probe about 10° upwards, a diencephalic transverse scan may be obtained. In this section, the third ventricle can be visualized as a highly echogenic double-line image, due to ipsilateral and controlateral inner layer of the hyperechogenic ependima (Figures 2-4).
Just posteriorly, thalami are depicted as hypoecogen/hysoecogen structures surrounding the third ventricle (Figure 2). Anteriorly, the frontal horn of the contralateral lateral ventricle is visualized as hypoechogenic structure, well visible between two parallel lines corresponding to the medial and lateral layer of the ependima (Figure 4). At this plane, the largest transverse diameters of the third ventricle and of the frontal horns of the contralateral lateral ventricle may be measured[6,7]. It may be useful to pay attention that image is generated by a sectorial probe, and the proportions are different in the central and in the lateral part of the image. Thus, lateral ventricle ipsilateral to the probe is often depicted at the same depth of the third ventricle.
The insonation planes are usually the midbrain and diencephalic transverse ones, even though the coronal orientation has been described. A free hand multiplanar approach has been observed, especially on surgically decompressed patients[2], and attempts of standardized approaches have been reported[8]. A standardization of insonation planes would be very useful for comparison and follow-up of sonographic findings.
With the blind technique, landmarks regularly visualized, even in moderate sonographic conditions (identification rates of > 75%) are mesencephalon, pons, third ventricle, lateral ventricles, falx, thalamus, basal ganglia, pineal gland and temporal lobe[7]. Moreover, ultrasound (US) perfusion imaging can be enhanced by the application of echo-contrast harmonic imaging modalities[9,10].
In spontaneous or traumatic cerebral hemorrhage (ICH), hematoma enlargement is the most important modifiable prognostic factor; thus, monitoring of the volume of the hemorrhage is the first priority in the acute phase[11,12].
CT’s widespread acute availability makes it the primary diagnostic modality for ICH. However, in the first hours after the diagnosis, TCS may be very useful to monitor an early ICH enlargement. In fact, TCS allows the visualization of acute ICH, as an hyperechoic sharply demarcated mass within the brain parenchyma. The accuracy is limited to the first 4-6 d after the onset of the ICH, when the hematoma remains more echogenic than the surrounding brain tissue.
Several authors studied the correlation between CT and TCS in cerebral hemorrhage. Seidel confirmed CT diagnosis by TCS in 18/23 cases (78%)[9]. Mäurer et al[13] published a study on TCS in 151 stroke patients correctly differentiating between ischemia and hemorrhage in 95%. 12% had an insufficient temporal bone window for transcranial insonation.
Perez et al[14] prospectively studied 46 patients with supratentorial ICH evaluated within 3 h of onset. In 8 cases ICH was not observed by TCS: 5 patients showed a small-sized ICH on CT, and in 3 cases hematoma was located in brainstem or in cerebellum. In the remaining patients a very good correlation was observed for each diameter of the mass and for total hematoma volume (r = 0.82, P < 0.001).
TCS was also evaluated to detect hemorrhagic transformation in the early phase of ischemic stroke. Seidel et al[15] found an excellent correlation between TCS and CT on 20 patients with hemorrhagic transformation; in 2 cases small cortical hematoma was not diagnosed.
From these data, TCS seems an interesting option for ICH monitoring; actually, its accuracy appears insufficient to support therapeutic decisions in the acute setting.
Recent studies evaluated the impact of echo contrast agents on visualization of ICH by TCS. By using ultrasound perfusion imaging, Kern et al[16] observed a reduction in contrast agent arrival in the ICH core, which led to better delineation of the lesion borders from adjacent tissue. Correlation with CT was very good (r = 0.94, 95%CI: 0.81-0.98, P < 0.001). Similar results were reported by Vicenzini et al[17] and Kern et al[18].
US perfusion imaging has a wide diffusion in myocardial, renal and musculoskeletal tissue, and might be an option even for brain under difficult insonation conditions; actually, the real advantage of this technique on TCS is still unknown.
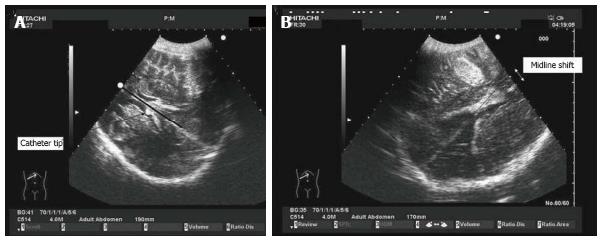
Epidural and subdural hematoma (EDH, SDH) are potentially life-threatening complications after severe, moderate and mild traumatic brain injury. If undetected and untreated, they may lead to progressive transtentorial herniation with loss of consciousness, pupillary dilation, and further neurologic deficits. In EDH-patients, the CT scan remains the diagnostic gold standard, but early bedside detection of acute EDH by TCS has been described[19]. By using a midbrain transverse scan, contralateral skull became well visible even in absence of decompressive craniectomy, and an epidural hematoma can be observed as an hyperechogenic image just inside the skull (Figures 5-7). Prospective data on usefulness of this technique for EDH detection are lacking and should be encouraged.
The extent of SDH has also been diagnosed and monitored by TCS [20]. In particular, SDH has been quantified by measuring the distance between the skull and the dural border of the arachnoid, described as a highly echogenic membrane. In this context, Niesen et al[20] reliably detected SDH in 22 of the 25 patients with confirmed SDH (88%). In the remaining 3 patients, the temporal bone window was insufficient for TGS investigation. Extent of SDH measured by CT and TCS correlated linearly (r = 0.849)[20].
In conclusion, TCS, when performed by a trained sonographer, may represent a possible method for noninvasively monitoring early hematoma growth at the bedside of patients with or without skull defects, with the role of complementing the CT scan diagnostic technique.
In the diencephalic transverse scan, midline dislocation (MLD) and hydrocephalus can be diagnosed through TCS scanning. The MLD can be observed and measured through two different methods.
According to the method described by Seidel et al[7], the third ventricle should be considered as a marker of the midline. The distance between third ventricle and external side of the temporal bone (A), needs to be measured. The same calculation can be repeated for the contralateral side (B). A MLD of the third ventricle is then estimated according to the formula MLD = (A - B)/2.
In that study, a reproducibility of sonographic MLD measurements corresponding to 0.3 ± 0.2 mm was reached in 10 healthy volunteers. This technique has been widely investigated by several studies in patients with acute cerebrovascular disease and after traumatic brain injury, and a very good correlation between sonographic and CT measurement of MLD are reported[21-23].
After decompressive craniectomy this method may be difficult. Bone defects, temporal cephalhematomas, or changes in intracranial anatomy secondary to trauma may all induce bias in the measure. In such a condition, Caricato et al[2] described a further method to visualize the MLD. This technique has shown an excellent agreement with CT scan measurements. In an axial plane, the midline, defined as the line between the two lateral ventricles, is measured by a convex probe with an abdominal preset. After localizing the falx cerebri, both on frontal and occipital sides, the distance between the extension of falx and the interventricular line is assessed; the present measurement is the MLD (Figure 8). The last method, which is still to be externally validated, seems rather simple and accurate because measurements are obtained on direct observation of the images and not by indirect mathematical calculations.
Posthemorrhagic hydrocephalus is a frequent complication after subarachnoid hemorrhage or parenchymal hemorrhage; furthermore external ventricular drainage may be necessary after severe traumatic injury to control intracranial hypertension. In these conditions, direct visualization of cerebral ventricles may be required, and critical patients have to be moved to radiology for CT scan.
In this context, TCS may be an useful option. In fact, previous studies compared sonographic and CT measurements of ventricular diameters, founding a good agreement. This was observed in particular for the measurement of third ventricle, that is depicted in a plane orthogonal to the probe, and doesn’t need angle correction. As we reported above, direct measurement of lateral ventricles is more difficult since its angle with the probe, and a generally moderate correlation with CT scan is reported. Actually, Kiphuth et al[21] observed that TCS was a reliable technique to predict the need of cerebrospinal fluid drainage. In patients with external ventricular drainage (EVD), they estimated that a cut-off value of an increase of 5.5 mm in ventricle width after clamping had an high sensitivity (100%) and negative predictive value (100%). They suggested that an increase in ventricular width lower than the cut-off was an indication for a safe removal of EVD.
In conclusion, even if the technique still requires a wide validation, it seems to be an interesting option when repetitive CT measurement have to be performed to monitor obstructive hydrocephalus in intensive care Unit.
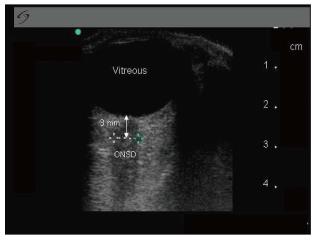
Optic nerve sheath diameter: Measurement of optic nerve sheath diameter has been proposed as a measure of increased intracranial pressure in a variety of settings[24-26]. In fact, the sheath around the optic nerve is a continuation of the dura; thus, a rise in ICP is transmitted to the optic nerve, eventually resulting in swelling of the optic disc and in a sheath diameter grater than the normal. The technique is easy and a quick learning curve is described. According with Cennamo et al[27], patients were examined in the supine position. Using a 7.5-MHz linear probe on the closed upper eyelid, the optic nerve was visualized as a linear hypoechoic structure with clearly defined margins posterior to the globe. Sheath diameter was measured 3.00 mm behind the globe, and a value greater than 5.00 mm was considered abnormal.
The technique has been described more than 20 years ago; even if some criticism should be considered[28], it is proposed as screening test to rule out intracranial hypertension noninvasively at the bedside.
In neurointensive care transcranial Doppler is often used for the evaluation of the cerebral blood flow, diagnosis and monitoring of vasospasm, and autoregulation in patients with different types of brain injury. Beyond the classic indications of transcranial doppler, B-mode ultrasounds can be used as imaging technique to monitor patients in ICU, and may often reduce the indication to CT scan. In this review we summarized the main indications for TCS in intensive care unit. In our opinion, it is a still underestimated imaging modality that requires a wider diffusion. As for any other sonographic assessment, TCS is a highly user-dependent technique, and requires expertise to perform accurate evaluation. In this context, physicians working in neurologic intensive care medicine should be trained not only to apply Doppler methods for investigation of cerebral vessels but also in transcranial B-mode sonography; further studies should be encouraged for a better comprehension of usefulness and limits of this technique as option to brain CT.
P- Reviewer: Brigo F, Llompart-Pou J, Zanini MA S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
| 1. | Aaslid R, Markwalder TM, Nornes H. Noninvasive transcranial Doppler ultrasound recording of flow velocity in basal cerebral arteries. J Neurosurg. 1982;57:769-774. [PubMed] |
| 2. | Caricato A, Mignani V, Bocci MG, Pennisi MA, Sandroni C, Tersali A, Antonaci A, de Waure C, Antonelli M. Usefulness of transcranial echography in patients with decompressive craniectomy: a comparison with computed tomography scan. Crit Care Med. 2012;40:1745-1752. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 38] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 3. | Libert N, Boutonnet M, Giraud N, Tourtier JP, de Rudnicki S. Transcranial echography: an interesting tool for aeromedical evacuations. Crit Care Med. 2012;40:3331-3332; author reply 3332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 4. | Wijnhoud AD, Franckena M, van der Lugt A, Koudstaal PJ, Dippel ED. Inadequate acoustical temporal bone window in patients with a transient ischemic attack or minor stroke: role of skull thickness and bone density. Ultrasound Med Biol. 2008;34:923-929. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 91] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 5. | Yoshimura S, Koga M, Toyoda K, Mukai T, Hyun BH, Naganuma M, Nagatsuka K, Minematsu K. Frontal bone window improves the ability of transcranial color-coded sonography to visualize the anterior cerebral artery of Asian patients with stroke. AJNR Am J Neuroradiol. 2009;30:1268-1269. [PubMed] |
| 6. | Seidel G, Kaps M, Gerriets T. Potential and limitations of transcranial color-coded sonography in stroke patients. Stroke. 1995;26:2061-2066. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 93] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 7. | Seidel G, Kaps M, Gerriets T, Hutzelmann A. Evaluation of the ventricular system in adults by transcranial duplex sonography. J Neuroimaging. 1995;5:105-108. [PubMed] |
| 8. | Kern R, Perren F, Kreisel S, Szabo K, Hennerici M, Meairs S. Multiplanar transcranial ultrasound imaging: standards, landmarks and correlation with magnetic resonance imaging. Ultrasound Med Biol. 2005;31:311-315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 21] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 9. | Seidel G, Meyer-Wiethe K, Berdien G, Hollstein D, Toth D, Aach T. Ultrasound perfusion imaging in acute middle cerebral artery infarction predicts outcome. Stroke. 2004;35:1107-1111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 43] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 10. | Bartels E, Bittermann HJ. Transcranial contrast imaging of cerebral perfusion in patients with space-occupying intracranial lesions. J Ultrasound Med. 2006;25:499-507. [PubMed] |
| 11. | Brouwers HB, Greenberg SM. Hematoma expansion following acute intracerebral hemorrhage. Cerebrovasc Dis. 2013;35:195-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 193] [Article Influence: 16.1] [Reference Citation Analysis (0)] |
| 12. | Dowlatshahi D, Demchuk AM, Flaherty ML, Ali M, Lyden PL, Smith EE. Defining hematoma expansion in intracerebral hemorrhage: relationship with patient outcomes. Neurology. 2011;76:1238-1244. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 512] [Cited by in RCA: 487] [Article Influence: 34.8] [Reference Citation Analysis (0)] |
| 13. | Mäurer M, Shambal S, Berg D, Woydt M, Hofmann E, Georgiadis D, Lindner A, Becker G. Differentiation between intracerebral hemorrhage and ischemic stroke by transcranial color-coded duplex-sonography. Stroke. 1998;29:2563-2567. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 50] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 14. | Pérez ES, Delgado-Mederos R, Rubiera M, Delgado P, Ribó M, Maisterra O, Ortega G, Alvarez-Sabin J, Molina CA. Transcranial duplex sonography for monitoring hyperacute intracerebral hemorrhage. Stroke. 2009;40:987-990. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 37] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 15. | Seidel G, Cangür H, Albers T, Burgemeister A, Meyer-Wiethe K. Sonographic evaluation of hemorrhagic transformation and arterial recanalization in acute hemispheric ischemic stroke. Stroke. 2009;40:119-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 20] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 16. | Kern R, Kablau M, Sallustio F, Fatar M, Stroick M, Hennerici MG, Meairs S. Improved detection of intracerebral hemorrhage with transcranial ultrasound perfusion imaging. Cerebrovasc Dis. 2008;26:277-283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 17. | Vicenzini E, Delfini R, Magri F, Puccinelli F, Altieri M, Santoro A, Giannoni MF, Bozzao L, Di Piero V, Lenzi GL. Semiquantitative human cerebral perfusion assessment with ultrasound in brain space-occupying lesions: preliminary data. J Ultrasound Med. 2008;27:685-692. [PubMed] |
| 18. | Kern R, Krogias C, Meyer-Wiethe K, Renault G, Kablau M, Sallustio F, Eyding J, Meves S, Seidel G, Meairs S: Diagnosis of acute ischemic vs. hemorrhagic stroke with transcranial ultrasound imaging – a prospective multi-center study. Cerebrovasc Dis. 2006;21:34. |
| 19. | Caricato A, Mignani V, Sandroni C, Pietrini D. Bedside detection of acute epidural hematoma by transcranial sonography in a head-injured patient. Intensive Care Med. 2010;36:1091-1092. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 20. | Niesen WD, Burkhardt D, Hoeltje J, Rosenkranz M, Weiller C, Sliwka U. Transcranial grey-scale sonography of subdural haematoma in adults. Ultraschall Med. 2006;27:251-255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 21. | Kiphuth IC, Huttner HB, Struffert T, Schwab S, Köhrmann M. Sonographic monitoring of ventricle enlargement in posthemorrhagic hydrocephalus. Neurology. 2011;76:858-862. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 35] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 22. | Stolz E, Gerriets T, Fiss I, Babacan SS, Seidel G, Kaps M. Comparison of transcranial color-coded duplex sonography and cranial CT measurements for determining third ventricle midline shift in space-occupying stroke. AJNR Am J Neuroradiol. 1999;20:1567-1571. [PubMed] |
| 23. | Llompart Pou JA, Abadal Centellas JM, Palmer Sans M, Pérez Bárcena J, Casares Vivas M, Homar Ramírez J, Ibáñez Juvé J. Monitoring midline shift by transcranial color-coded sonography in traumatic brain injury. A comparison with cranial computerized tomography. Intensive Care Med. 2004;30:1672-1675. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 30] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 24. | Newman WD, Hollman AS, Dutton GN, Carachi R. Measurement of optic nerve sheath diameter by ultrasound: a means of detecting acute raised intracranial pressure in hydrocephalus. Br J Ophthalmol. 2002;86:1109-1113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 192] [Cited by in RCA: 202] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 25. | Moretti R, Pizzi B, Cassini F, Vivaldi N. Reliability of optic nerve ultrasound for the evaluation of patients with spontaneous intracranial hemorrhage. Neurocrit Care. 2009;11:406-410. [PubMed] |
| 26. | Dubost C, Le Gouez A, Jouffroy V, Roger-Christoph S, Benhamou D, Mercier FJ, Geeraerts T. Optic nerve sheath diameter used as ultrasonographic assessment of the incidence of raised intracranial pressure in preeclampsia: a pilot study. Anesthesiology. 2012;116:1066-1071. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 74] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 27. | Cennamo G, Gangemi M, Stella L: The comparison between endocranial pressure and optic nerve diameter: an ultrasonographic study. Doc Ophthalmol Proc Ser. 1987;48:603-606. [RCA] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 10] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 28. | Copetti R, Cattarossi L. Optic nerve ultrasound: artifacts and real images. Intensive Care Med. 2009;35:1488-1489; author reply 1488-1489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 52] [Article Influence: 3.3] [Reference Citation Analysis (0)] |