Published online Jul 28, 2014. doi: 10.4329/wjr.v6.i7.417
Revised: March 27, 2014
Accepted: May 28, 2014
Published online: July 28, 2014
Processing time: 219 Days and 0.6 Hours
Surgical extraction of the third molar is the most commonly performed surgical procedure in the clinical practice of oral surgery. Third molar surgery is warranted when there is inadequate space for eruption, malpositioning, or risk for cyst or odontogenic tumor formation. Preoperative assessment should include a detailed morphologic analysis of the third molar and its relationship to adjacent structures and surrounding tissues. Due to developments in medical engineering technology, computed tomography (CT) now plays a critical role in providing the clear images required for adequate assessment prior to third molar surgery. Removal of the maxillary third molar is associated with a risk for maxillary sinus perforation, whereas removal of the mandibular third molar can put patients at risk for a neurosensory deficit from damage to the lingual nerve or inferior alveolar nerve. Multiple factors, including demographic, anatomic, and treatment-related factors, influence the incidence of nerve injury during or following removal of the third molar. CT assessment of the third molar prior to surgery can identify some of these risk factors, such as the absence of cortication between the mandibular third molar and the inferior alveolar canal, prior to surgery to reduce the risk for nerve damage. This topic highlight presents an overview of the clinical significance of CT assessment in third molar surgery.
Core tip: Surgical extraction of the third molar is the most commonly performed procedure in oral surgery. Careful preoperative examinations, including the use of computed tomography (CT) assessment, assist in the planning of in predicting the risks related to surgical interventions. The clinical significance of CT assessment in relation to third molar surgery is therefore reviewed and discussed.
- Citation: Nakamori K, Tomihara K, Noguchi M. Clinical significance of computed tomography assessment for third molar surgery. World J Radiol 2014; 6(7): 417-423
- URL: https://www.wjgnet.com/1949-8470/full/v6/i7/417.htm
- DOI: https://dx.doi.org/10.4329/wjr.v6.i7.417
Surgical extraction of the third molar is the most common procedure performed by oral surgeons. Appropriate surgical procedures should be determined based on findings from the preoperative examinations that critically assess the morphology of the third molar, and its relationships with adjacent structures [particularly the inferior alveolar canal (IAC) ] and surrounding tissues.
Preoperative imaging assessments have typically included conventional intraoral radiography or orthopantomography (OPG). Following more recent developments in medical engineering technology, computed tomography (CT) now serves as an integral method to provide clear images for use in clinical practice. Multi-detector CT (MDCT) and cone-beam CT (CBCT) imaging of oral and maxillofacial regions serve as essential methods for diagnosis and treatment planning. Recently, the clinical importance of preoperative CT assessments in third molar surgery has been reported[1-3]. In this article, the general problems related to third molar surgery are reviewed. In addition, current topics associated with the clinical significance of CT assessment for third molar surgery are discussed.
Third molars should be extracted when there is inadequate space for eruption in the retromolar region, between the second molar and the mandibular ramus. This can lead to a disturbed eruption of the third molar, which may create a flap of gingival tissue around the partially erupted tooth, or a pericoronal pocket, which can potentially develop into pericoronitis. In addition, Rahman et al[4] recently reported that asymptomatic pericoronal tissue associated with impacted teeth showed a high rate of squamous metaplasia and proliferative activity. Although impacted teeth with pericoronal tissue can lead to cyst formation or odontogenic tumors, the prophylactic removal of disease-free third molars is still controversial[5,6]. Extraction is also warranted when there is mesioangular or “horizontal” malpositioning of the third molar. Such malpositioning can lead to difficulties in plaque control between the second and third molars and may occasionally lead to second molar dental caries. Furthermore, this form of malpositioning may also affect the dental arch shape and result in tooth crowding.
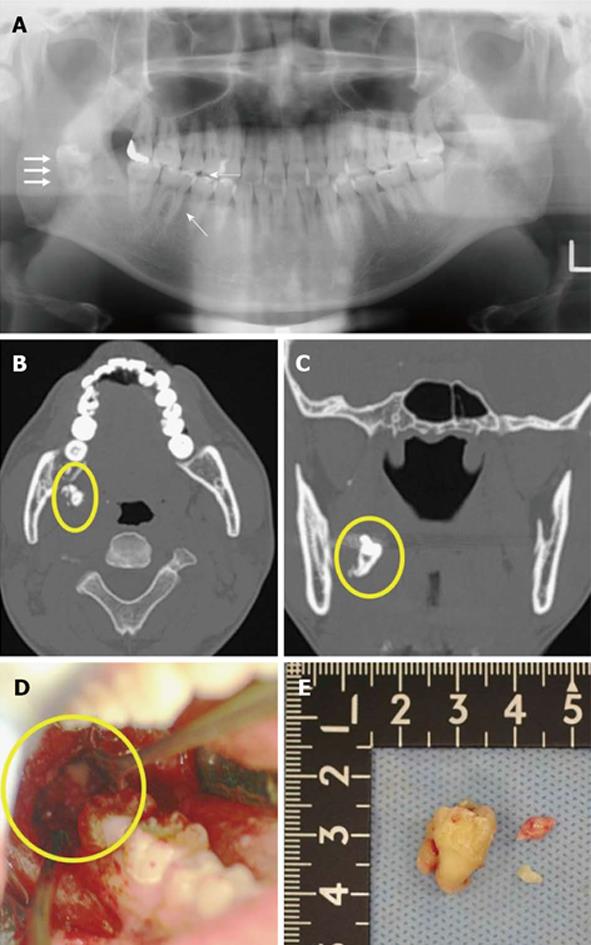
Careful preoperative evaluation of the relationship between the maxillary third molar (UM3) and the maxillary sinus is critical in order to prevent perforation of this sinus. For example, a patient is at risk for perforation in the absence of cortication between the UM3 and the maxillary sinus. It is important to note that excessive curettage at the base of the root apex region should be avoided (Figure 1). Removal of the mandibular third molar (LM3) can put patients at risk for serious neurosensory deficits, particularly due to injury of the lingual nerve (LN) and the inferior alveolar nerve (IAN). Lastly, if the third molar is fully or partially impacted in the alveolar bone, bone removal and tooth sectioning are required. Such surgically invasive procedures may cause postoperative pain, edema, and limited opening or mobility of the mouth due to muscle spasms.
LN and IAN nerve injuries are thought to be due to mechanical irritations from surgical intervention and are influenced by several demographic, anatomic, and treatment-related factors[7,8]. Risk for injury is increased with the age of the patient because of technical difficulties during surgery, decreased bone elasticity, or increased incidence of tooth hypercementosis. In addition, age may contribute to a reduced capacity for damaged nerve fiber recovery. Furthermore, elderly patients with evidence of sclerotic change are at a considerably higher risk for pathologic osteomyelitis around the impacted tooth[9]. Nakagawa et al[10] reported that female patients are at a higher risk for IAN injuries due to decreased buccolingual thickness of the mandible. The risk for damage is increased with a thinner mandible as there is less space between the IAC and LM3. Additional anatomic risk factors for injury from surgery include tooth angulation, the presence of a distal overhang, and the degree of impaction, which are integrally related to the need for surgical intervention. Treatment-related risk factors include injection of local anesthesia, mucoperiosteal incision and elevation of the mucoperiosteal flap, bur usage during alveolar bone removal and tooth sectioning, stretching of the nerve during surgery, and accidental fractures of the lingual cortical bone of the mandible[11]. These treatment-related risk factors are associated with the surgeon’s level of experience[12,13].
The lingual split technique for third molar extraction is highly associated with a risk for LN deficit, though the associated risk for LN morbidity remains controversial[11,12]. Therefore, the most widely used technique in clinical practice to decrease the risk of LN injury is the buccal approach. Preoperative imaging assessments can also be employed to limit nerve injury occurrence. Ultrasonography should be used to detect the LN, since the location of the nerve in the mandible prohibits detection by CT imaging[14]. As the IAN is located within the IAC, it can be indirectly evaluated through radiographic assessment of the IAC. Importantly, preoperative radiographic assessment provides increased information on the relationship between the LM3 and the IAC and can be used to identify whether risk factors for IAN injury are present prior to LM3 extraction. In cases where preoperative examination has identified a high-risk factor, surgeons may consider the use of special surgical approaches, including coronectomy[15,16], multistep extraction[17,18], or orthodontic extraction techniques[19-21] to decrease the risk for IAN injuries.
There are several different radiology procedures that can be used prior to third molar surgery. Conventional intraoral radiography provides surgeons with detailed information regarding structures at the exposed site. If two structures are superimposed, a parallax technique can be applied to determine the buccolingual relationship. However, it is sometimes difficult to position films or an imaging plate at an ideal position, as the LM3 is predominantly located posterior to the mandible.
OPG is widely used during treatment planning for third molar surgery because it enables assessment of the two-dimensional relationship between the tooth and the IAC. Rood and Shebab have outlined seven important findings that can be obtained from OPG images: darkening of the root, deflected roots, narrowing of the root, dark and bifid roots, interruption of the white line(s), and diversion and narrowing of the IAC[22]. These authors concluded that the diversion of IAC, darkening of the root and interruption of the white line were significantly related to IAN injuries. There have been several OPG assessment studies which support the usefulness of these seven findings[3,23-25]. According to a meta-analysis study, three signs-darkening of the root or increased radiolucency, interruption of radiopaque borders of the mandibular canal, and diversion of the mandibular canal-have been implicated as the most significant predictive factors of a close relationship between the IAN and the LM3[26]. It should be noted, though, that the statistical results from these analyses had various levels of specificity and sensitivity (Table 1).
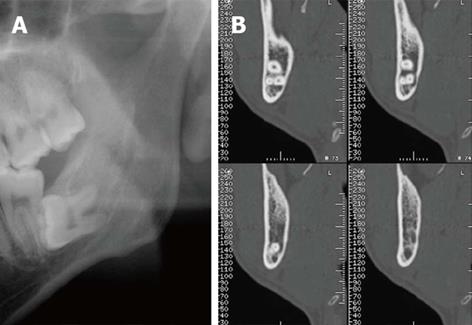
Recent research indicated that high-risk signs identified by OPG are significantly associated with absence of the cortication between LM3 and IAC[27,28]. In particular, darkening of the root is closely related to cortical bone loss and/or grooving of the root[27,29-31] (Figure 2). Furthermore, interruption of radiopaque borders has been attributed to loss of cortical structure of the canal. A sign for diversion of the mandibular canal is classified by a nerve running between the roots or the interposition between the root and the mandibular cortical bone.
CT and/or CBCT examinations enable easy assessment of three-dimensional anatomic relationships between the third molar and adjacent structures and surrounding tissues, as well as for detection of the mental foramen and bifid mandibular canal[32-34]. Furthermore, if the third molar becomes dislocated during surgery, the CT image is a useful tool for detecting the dislocated tooth (Figure 3).
The accuracy of measurement by CT was evaluated by a comparative study of the skull, showing that medical CT (single-detector CT or MDCT) or CBCT is sufficient if preoperative CTs have been taken[35,36]. Accurate assessment of the IAC position is important in the field of oral surgery, and several studies have reported the clinical significance of the position of the IAC with respect to LM3[10,32,37]. When the IAN is positioned at the lingual site of the LM3, and sandwiched between the LM3 and the lingual cortex, it may become compressed during LM3 extraction. Several studies have reported that the predictive value of CT assessment for IAN injuries was approximately 20%-30%[1,37-39], and 30% when the nerve-vascular bundle was observed[40].
CT images of reconstructed cross-sectional (or coronal) views have been used for assessment of the cortical status around the IAC. Two studies have suggested a predictive value for cortication status in IAN injuries[2,41], which currently appears to be the gold standard finding for predicting signs of IAN injuries. In our own retrospective and prospective studies, the absence of cortication between LM3 and the IAC was a requirement for IAN injuries[38,42,43]. In addition, Susarla et al[39] reported that the estimated cortical defect size, computed by counting the number of consecutive slice images with interruptions in the white line around the IAC, was closely related to IAN injury. If reconstruction software is unavailable, a reformatted coronal view can be obtained through reconstruction of the perpendicular image of the IAC, which is based on the axial and sagittal vertical planes[38].
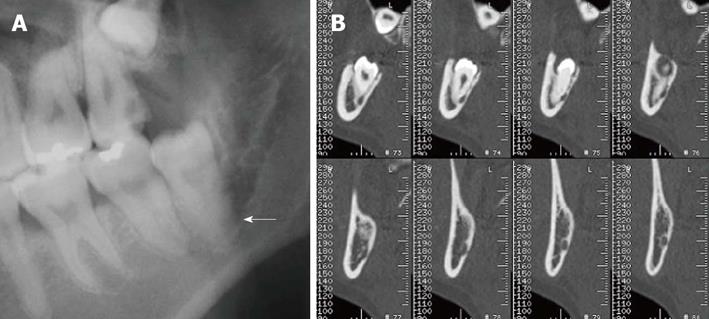
The shape of the IAC has become a significant new finding for estimating the proximity between the IAC and LM3[38,42,44]. Although high-risk signs from OPG findings indicated a relationship with lost cortication, some alterations have been recognized in the IAC without the OPG finding (Figure 4). All IAC shapes are initially round/oval near the mandibular foramen, although some canals change shape toward the anterior aspect of the mandible[42]. Alteration of canals is observed most often at the section closest to LM3 (Figure 4B). The altered canal shapes are described as “teardrop-shaped”, “dumbbell-shaped”[42], or as an invagination[44]. Collectively, the alteration indicates the degree of proximity between the IAC and LM3.
The number and shape of the LM3 roots can also be assessed by CT examination and should be recommended to surgeons seeking important clinical information. For instance, if the LM3 has three roots, a root-sectioning technique may be needed. However, the number of LM3 roots does not correlate with the incidence of IAN injury. A grooved root shape is intimated due to the close relationship between the root and IAC (Figure 5).
Preoperative CT examination is now considered an important assessment tool for third molar surgery. Despite this, standard eligibility criteria have not yet been established to necessitate the use of CT examination[45,46]. Furthermore, standardized significant findings have not been put in place for third molar surgery. This may be due to the low incidence of complications during third molar surgery. To resolve these issues, multi-institutional studies and development of a uniform protocol are needed.
P- Reviewer: Bernardin L, Bishnuhari P, Jain S, Mesquita RA, Morimoto Y, Sepahdari AR S- Editor: Song XX L- Editor: A E- Editor: Lu YJ
| 1. | Susarla SM, Dodson TB. Preoperative computed tomography imaging in the management of impacted mandibular third molars. J Oral Maxillofac Surg. 2007;65:83-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 67] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 2. | Palma-Carrió C, García-Mira B, Larrazabal-Morón C, Peñarrocha-Diago M. Radiographic signs associated with inferior alveolar nerve damage following lower third molar extraction. Med Oral Patol Oral Cir Bucal. 2010;15:e886-e890. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 28] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 3. | Monaco G, Montevecchi M, Bonetti GA, Gatto MR, Checchi L. Reliability of panoramic radiography in evaluating the topographic relationship between the mandibular canal and impacted third molars. J Am Dent Assoc. 2004;135:312-318. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 131] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 4. | Rahman F, Bhargava A, Tippu SR, Kalra M, Bhargava N, Kaur I, Srivastava S. Analysis of the immunoexpression of Ki-67 and Bcl-2 in the pericoronal tissues of impacted teeth, dentigerous cysts and gingiva using software image analysis. Dent Res J (Isfahan). 2013;10:31-37. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 5. | Leone SA, Edenfield MJ, Cohen ME. Correlation of acute pericoronitis and the position of the mandibular third molar. Oral Surg Oral Med Oral Pathol. 1986;62:245-250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 45] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 6. | Weir S, Lopes V, Malden N. Influence of SIGN guidelines on removal of third molars in The Lothians, Scotland, a clinical audit. Oral Surg. 2010;3:57-60. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 7. | Leung YY, Cheung LK. Risk factors of neurosensory deficits in lower third molar surgery: an literature review of prospective studies. Int J Oral Maxillofac Surg. 2011;40:1-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 77] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 8. | Renton T, Yilmaz Z, Gaballah K. Evaluation of trigeminal nerve injuries in relation to third molar surgery in a prospective patient cohort. Recommendations for prevention. Int J Oral Maxillofac Surg. 2012;41:1509-1518. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 56] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 9. | Miyamoto I, Ishikawa A, Morimoto Y, Takahashi T. Potential risk of asymptomatic osteomyelitis around mandibular third molar tooth for aged people: a computed tomography and histopathologic study. PLoS One. 2013;8:e73897. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Nakagawa Y, Ishii H, Nomura Y, Watanabe NY, Hoshiba D, Kobayashi K, Ishibashi K. Third molar position: reliability of panoramic radiography. J Oral Maxillofac Surg. 2007;65:1303-1308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 97] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 11. | Boffano P, Roccia F, Gallesio C. Lingual nerve deficit following mandibular third molar removal: review of the literature and medicolegal considerations. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;113:e10-e18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 12. | Cheung LK, Leung YY, Chow LK, Wong MC, Chan EK, Fok YH. Incidence of neurosensory deficits and recovery after lower third molar surgery: a prospective clinical study of 4338 cases. Int J Oral Maxillofac Surg. 2010;39:320-326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 160] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 13. | Jerjes W, Upile T, Shah P, Nhembe F, Gudka D, Kafas P, McCarthy E, Abbas S, Patel S, Hamdoon Z. Risk factors associated with injury to the inferior alveolar and lingual nerves following third molar surgery-revisited. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:335-345. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 99] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 14. | Benninger B, Kloenne J, Horn JL. Clinical anatomy of the lingual nerve and identification with ultrasonography. Br J Oral Maxillofac Surg. 2013;51:541-544. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 30] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 16. | Renton T. Update on coronectomy. A safer way to remove high risk mandibular third molars. Dent Update. 2013;40:362-364, 362-364. [PubMed] |
| 17. | Landi L, Manicone PF, Piccinelli S, Raia A, Raia R. Staged removal of horizontally impacted third molars to reduce risk of inferior alveolar nerve injury. J Oral Maxillofac Surg. 2010;68:442-446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 18. | Landi L, Manicone PF, Piccinelli S, Raia A, Raia R. A novel surgical approach to impacted mandibular third molars to reduce the risk of paresthesia: a case series. J Oral Maxillofac Surg. 2010;68:969-974. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 27] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 19. | Park W, Park JS, Kim YM, Yu HS, Kim KD. Orthodontic extrusion of the lower third molar with an orthodontic mini implant. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;110:e1-e6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 20. | Wang Y, He D, Yang C, Wang B, Qian W. An easy way to apply orthodontic extraction for impacted lower third molar compressing to the inferior alveolar nerve. J Craniomaxillofac Surg. 2012;40:234-237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 21. | Ma ZG, Xie QY, Yang C, Xu GZ, Cai XY, Li JY. An orthodontic technique for minimally invasive extraction of impacted lower third molar. J Oral Maxillofac Surg. 2013;71:1309-1317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 18] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 22. | Rood JP, Shehab BA. The radiological prediction of inferior alveolar nerve injury during third molar surgery. Br J Oral Maxillofac Surg. 1990;28:20-25. [PubMed] |
| 23. | Blaeser BF, August MA, Donoff RB, Kaban LB, Dodson TB. Panoramic radiographic risk factors for inferior alveolar nerve injury after third molar extraction. J Oral Maxillofac Surg. 2003;61:417-421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 133] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 24. | Kim JW, Cha IH, Kim SJ, Kim MR. Which risk factors are associated with neurosensory deficits of inferior alveolar nerve after mandibular third molar extraction? J Oral Maxillofac Surg. 2012;70:2508-2514. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 62] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 25. | Szalma J, Lempel E, Jeges S, Szabó G, Olasz L. The prognostic value of panoramic radiography of inferior alveolar nerve damage after mandibular third molar removal: retrospective study of 400 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:294-302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 71] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 26. | Atieh MA. Diagnostic accuracy of panoramic radiography in determining relationship between inferior alveolar nerve and mandibular third molar. J Oral Maxillofac Surg. 2010;68:74-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 62] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 27. | Umar G, Bryant C, Obisesan O, Rood JP. Correlation of the radiological predictive factors of inferior alveolar nerve injury with cone beam computed tomography findings. Oral Surg. 2010;3:72-82. [RCA] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 36] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 28. | Shahidi S, Zamiri B, Bronoosh P. Comparison of panoramic radiography with cone beam CT in predicting the relationship of the mandibular third molar roots to the alveolar canal. Imaging Sci Dent. 2013;43:105-109. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 29. | Tantanapornkul W, Okochi K, Bhakdinaronk A, Ohbayashi N, Kurabayashi T. Correlation of darkening of impacted mandibular third molar root on digital panoramic images with cone beam computed tomography findings. Dentomaxillofac Radiol. 2009;38:11-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 57] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 30. | Szalma J, Vajta L, Lempel E, Jeges S, Olasz L. Darkening of third molar roots on panoramic radiographs: is it really predominantly thinning of the lingual cortex? Int J Oral Maxillofac Surg. 2013;42:483-488. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 31. | Harada N, Vasudeva SB, Joshi R, Seki K, Araki K, Matsuda Y, Okano T. Correlation between panoramic radiographic signs and high risk anatomical factors for impacted mandibular third molars. Oral Surg. 2013;6:129-136. [RCA] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 32. | Yamada T, Ishihama K, Yasuda K, Hasumi-Nakayama Y, Ito K, Yamaoka M, Furusawa K. Inferior alveolar nerve canal and branches detected with dental cone beam computed tomography in lower third molar region. J Oral Maxillofac Surg. 2011;69:1278-1282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 33. | Naitoh M, Hiraiwa Y, Aimiya H, Gotoh K, Ariji E. Accessory mental foramen assessment using cone-beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:289-294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 105] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 34. | Neves FS, Nascimento MC, Oliveira ML, Almeida SM, Bóscolo FN. Comparative analysis of mandibular anatomical variations between panoramic radiography and cone beam computed tomography. Oral Maxillofac Surg. 2013;Aug 24; Epub ahead of print. [PubMed] |
| 35. | Williams FL, Richtsmeier JT. Comparison of mandibular landmarks from computed tomography and 3D digitizer data. Clin Anat. 2003;16:494-500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 40] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 36. | Ludlow JB, Laster WS, See M, Bailey LJ, Hershey HG. Accuracy of measurements of mandibular anatomy in cone beam computed tomography images. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:534-542. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 208] [Cited by in RCA: 194] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 37. | Xu GZ, Yang C, Fan XD, Yu CQ, Cai XY, Wang Y, He D. Anatomic relationship between impacted third mandibular molar and the mandibular canal as the risk factor of inferior alveolar nerve injury. Br J Oral Maxillofac Surg. 2013;51:e215-e219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 64] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 38. | Shiratori K, Nakamori K, Ueda M, Sonoda T, Dehari H. Assessment of the shape of the inferior alveolar canal as a marker for increased risk of injury to the inferior alveolar nerve at third molar surgery: a prospective study. J Oral Maxillofac Surg. 2013;71:2012-2019. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 26] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 39. | Susarla SM, Sidhu HK, Avery LL, Dodson TB. Does computed tomographic assessment of inferior alveolar canal cortical integrity predict nerve exposure during third molar surgery? J Oral Maxillofac Surg. 2010;68:1296-1303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 32] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 40. | Tay AB, Go WS. Effect of exposed inferior alveolar neurovascular bundle during surgical removal of impacted lower third molars. J Oral Maxillofac Surg. 2004;62:592-600. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 94] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 41. | Nakayama K, Nonoyama M, Takaki Y, Kagawa T, Yuasa K, Izumi K, Ozeki S, Ikebe T. Assessment of the relationship between impacted mandibular third molars and inferior alveolar nerve with dental 3-dimensional computed tomography. J Oral Maxillofac Surg. 2009;67:2587-2591. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 67] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 42. | Ueda M, Nakamori K, Shiratori K, Igarashi T, Sasaki T, Anbo N, Kaneko T, Suzuki N, Dehari H, Sonoda T. Clinical significance of computed tomographic assessment and anatomic features of the inferior alveolar canal as risk factors for injury of the inferior alveolar nerve at third molar surgery. J Oral Maxillofac Surg. 2012;70:514-520. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 52] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 43. | Nakamori K, Fujiwara K, Miyazaki A, Tomihara K, Tsuji M, Nakai M, Michifuri Y, Suzuki R, Komai K, Shimanishi M. Clinical assessment of the relationship between the third molar and the inferior alveolar canal using panoramic images and computed tomography. J Oral Maxillofac Surg. 2008;66:2308-2313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 62] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 44. | Selvi F, Dodson TB, Nattestad A, Robertson K, Tolstunov L. Factors that are associated with injury to the inferior alveolar nerve in high-risk patients after removal of third molars. Br J Oral Maxillofac Surg. 2013;51:868-873. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 42] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 45. | Lübbers HT, Matthews F, Damerau G, Kruse AL, Obwegeser JA, Grätz KW, Eyrich GK. Anatomy of impacted lower third molars evaluated by computerized tomography: is there an indication for 3-dimensional imaging? Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;111:547-550. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 32] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 46. | Roeder F, Wachtlin D, Schulze R. Necessity of 3D visualization for the removal of lower wisdom teeth: required sample size to prove non-inferiority of panoramic radiography compared to CBCT. Clin Oral Investig. 2012;16:699-706. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 24] [Article Influence: 1.7] [Reference Citation Analysis (0)] |