Published online Dec 28, 2014. doi: 10.4329/wjr.v6.i12.919
Revised: November 2, 2014
Accepted: November 17, 2014
Published online: December 28, 2014
Processing time: 82 Days and 6 Hours
Beckwith-Wiedemann syndrome (BWS) is an overgrowth syndrome associated with increased risk to develop malignancies including adrenocortical carcinoma. Ovarian thecal metaplasia of the adrenal gland is a rare tumor-like mesenchymal lesion in BWS patients that lacks detailed radiological description. We report a 17-year-old female patient with BWS, associated with bilateral Wilms tumor, hepatic hemangiomatosis, pancreatic neuroendocrine tumor, and a phyllodes tumor of the right breast. Surveillance abdominal ultrasound identified a right adrenal mass that was further characterized by computed tomography and magnetic resonance imaging. Radiologically, this mass displayed features that overlap with adrenocortical carcinoma and pheochromocytoma but after pathological examination this proved to be an ovarian thecal metaplasia of the adrenal gland. Adrenal masses in BWS should raise the suspicion for adrenocortical carcinoma though other adrenal tumors including ovarian thecal metaplasia can be seen in these patients.
Core tip: This paper represents radiological features of the unique adrenal pathology in a premenopausal woman with Beckwith Wiedemann syndrome (BWS), although adrenal masses in BWS should raise the suspicion for adrenocortical carcinoma, yet other adrenal tumors including ovarian thecal metaplasia should be considered.
- Citation: Wassal EY, Habra MA, Vicens R, Rao P, Elsayes KM. Ovarian thecal metaplasia of the adrenal gland in association with Beckwith-Wiedemann syndrome. World J Radiol 2014; 6(12): 919-923
- URL: https://www.wjgnet.com/1949-8470/full/v6/i12/919.htm
- DOI: https://dx.doi.org/10.4329/wjr.v6.i12.919
Ovarian thecal metaplasia (OTM) of the adrenal gland is a rare mesenchymal lesion with an incidence of 2.4% to 4.3% in surgical specimens and 0.35% in autopsy series[1,2].
When first discovered, OTM was described as a wedge-shaped lesion composed of ovarian-like stroma resembling theca that shows continuity with the capsule of the adrenal gland[2]. We report a case of Beckwith-Wiedemann syndrome (BWS) with OTM of the right adrenal gland which was incidentally discovered on imaging.
To the best of our knowledge, this is the first report describing OTM in the context of BWS with detailed imaging description of this entity.
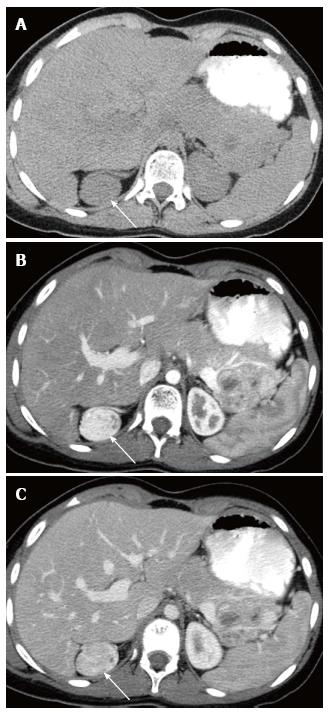
A 17-year-old female patient previously diagnosed with BWS, associated with bilateral Wilms tumor, hepatic hemangiomatosis, pancreatic neuroendocrine tumor, and a phyllodes tumor of the right breast, presented for periodic surveillance ultrasound examinations of both kidneys, which revealed a suspicious hypoechoic nodule in the right adrenal gland (Figure 1). The patient had no significant pain. There were no signs to suggest hormonal overproduction. Computed tomography (CT) scanning of the abdomen and pelvis was performed including non-contrast, arterial and venous post-contrast phases. On CT, this mass appeared as a well circumscribed oval shaped lesion measuring 3.5 cm × 2.6 cm in maximal transaxial dimensions abutting the upper pole of the right kidney. The mass was isodense to the kidney on non-contrast images (measuring 39 HU), demonstrated intense enhancement similar to the renal cortex on arterial phaseimages (measuring 221 HU), with decreased enhancement during the portal venous phase (169 HU) (Figure 2). No internal calcifications were seen on the non-contrast images.
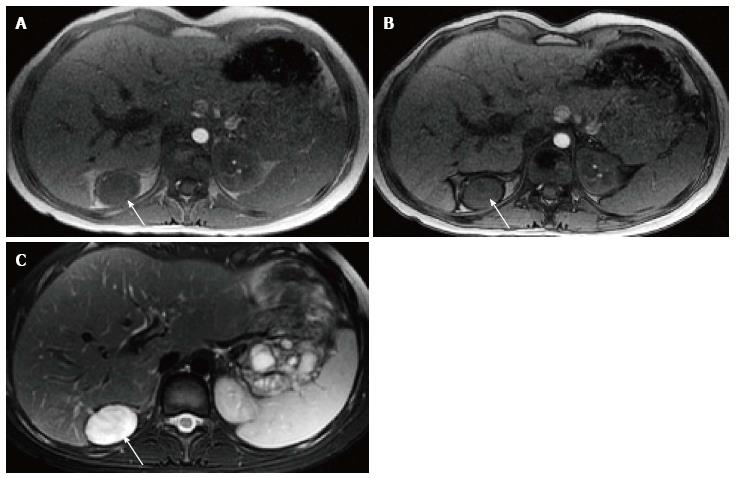
Magnetic resonance imaging revealed the right adrenal mass lesion (Figure 3), which was markedly hyperintense on T2-weighted images and isointense to the muscle on T1-weighted images. There was no difference in signal characteristics between the in-phase and out-of-phase images to indicate the presence of microscopic fat. The mass demonstrated intense inhomogeneous enhancement on post-contrast series. In addition, a large lobulated mass was noted to involve the pancreatic tail.
She previously underwent bilateral partial nephrectomy for Wilms tumor, cleft palate and lip repair, surgical resection of a right breast Phyllodes tumor and abdominal laparotomy with resection of right perirenal/adrenal tumor, distal pancreatectomy for the neuro-endocrine tumor and splenectomy.
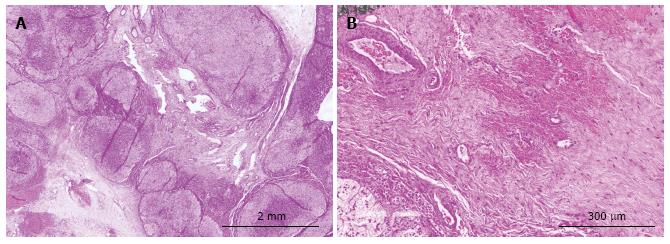
The right adrenalectomy specimen weighed 35.6 g. Grossly, there was a well circumscribed brown tumor measuring 4.1 cm identified. Histologically, the lesion was composed of bland adrenal cortical cells without areas of necrosis or increased mitotic activity. There was no capsular or lymphovascular invasion noted. The adrenal cortical adenoma was positive for inhibin, calretinin and MART-1 and was negative for S-100 and WT-1, which confirmed the diagnosis. In addition to the adenoma there was a fibroblastic “radial-scar”-like spindle cell proliferation noted admixed with the adrenal cortical tissue and in continuity with the capsule. The spindle cell proliferation was positive for WT-1 and focally positive for inhibin and calretinin. The histologic features were consistent with adrenal ovarian thecal metaplasia (Figure 4).
The adrenal gland is very close to gonadal tissue embryologically as both originate in the region of the urogenital ridge. The existence of ectopic adrenal tissue in the peri-ovarian region has been observed frequently. However, the existence of ovarian tissue in the adrenal gland is an extremely rare finding[1,3].
The pathogenesis of OTM is not fully known. It has been reported mostly in postmenopausal women and has been suggested that the foci of theca-like stroma in the adrenal gland may represent metaplasia from undifferentiated but embryologically competent mesenchymal cells of the adrenal capsule as a response to the elevated gonadotropin postmenopausal women[3,4].
The clinical significance of these lesions is largely not yet understood; they can be functional and still may undergo neoplastic transformation[4].
Pathologically, OTM appears as ahyalinized spindle cell nodule that is in direct continuity with the adrenal capsule and contains entrapped adrenal parenchymal cells with dystrophic calcifications[5]. It encloses a spectrum of fibroblastic-myofibroblastic proliferations that may rarely contain true ovarian stromal elements[2,5]. Since the features resemble a radial scar and there is no evidence of steroidogenic differentiation in most cases, the term “radial scar-like spindle cell myofibroblastic nodule of the adrenal gland” more accurately describes these lesions[2].
BWS is an overgrowth syndrome with annual incidence of 1 in 13700 newborns[6]. BWS is associated with an increased risk of childhood cancer. The cardinal features of BWS include macroglossia, macrosomia, midline abdominal wall defects, ear creases or ear pits, neonatal hypoglycemia, and less commonly cleft palate, mid-face hypoplasia, and hemihypertrophy. Our case had cleft palate, cleft lip and mid-face hypoplasia[7].
Various adrenal lesions have been reported in association with BWS, including adrenocortical carcinoma, cortical hyperplasia, fetal cortical cytomegaly, pheochromocytoma, adrenal calcification, cystic adrenal hemorrhage, and neuroblastoma[8].
In our case, OTM of the adrenal gland was seen as well circumscribed smooth mass which demonstrated intense enhancement on arterial and venous phases of contrast enhanced CT (up to 222 HU and 169 HU respectively) and, which is significantly higher than what would be expected for adenoma (mean arterial and venous enhancement of adenomas at 37 HU (-6 to 85 HU) and 60 HU (16-133 HU) and still higher than what would be expected for pheochromocytoma (mean arterial and venous enhancement of pheochromocytoma are 104 HU (42-190 HU) and 119 HU (61-195 HU)[9].
On MRI, the mass demonstrated markedly increased signal intensity on T2-weighted images, without signal difference between in-phase and out-of-phase pulse sequences. These features are not characteristic for adenoma, and have been only reported with pheochromocytoma, adrenocortical carcinoma and metastases. In our case, there was no biochemical evidence of pheochromocytoma, thus the diagnosis of pheochromocytoma was ruled out clinically and biochemically[9,10].
The imaging features were indeterminate and overlapped with those seen in adrenocortical carcinoma, metastasis and pheochromocytoma. Thus, surgical resection was indicated especially with the known association between BWS and adrenocortical carcinoma.
Surgical excision remains the treatment of choice for these masses because there is no definite preoperative method of identifying these masses and differentiating them from adrenocortical carcinoma and metastasis.
In our case, the right adrenalectomy specimen weighed 35.6 g. Grossly, there was a well circumscribed brown tumor measuring 4.1 cm identified. Histologically, the lesion was composed of bland adrenal cortical cells without areas of necrosis or increased mitotic activity. There was no capsular or lymphovascular invasion noted. The adrenal cortical adenoma was positive for inhibin, calretinin and MART-1 and was negative for S-100 and WT-1, which confirmed the diagnosis. In addition to the adenoma there was a fibroblastic “radial-scar”-like spindle cell proliferation noted admixed with the adrenal cortical tissue and in continuity with the capsule. The spindle cell proliferation was positive for WT-1 and focally positive for inhibin and calretinin. The histologic features were consistent with adrenal ovarian thecal metaplasia.
In conclusion, we presented the first case report describing imaging features of OTM involving adrenal gland, which occurred in a 17-year-old female with a BWS. OTM is diagnosis is possible only after histological examination as the imaging features of OTM overlap with those seen in adrenocortical carcinoma and pheochromocytoma.
A 17-year-old female previously diagnosed with Beckwith-Wiedemann syndrome (BWS) presented for periodic surveillance ultrasound examinations of both kidneys.
Asymmetry of the left cheek, left is fuller than the right, mild hemihypertrophy noted between right and left upper limbs and right hand is longer than the left.
Adrenocortical carcinoma, pheochromocytoma and adrenal metastases.
WBC 10 k/μL; HGB 13.3 mg/dL; plasma metanephrine and 24-h urinary collection for catecholamines and metanephrines were within normal limits.
US showed suspicious hypoechoic nodule in the right adrenal gland, which appeared in computed tomography as an isodense mass to the kidney on non-contrast images with intense enhancement on arterial phase images, in magnetic resonance imaging the mass was markedly hyperintense on T2-weighted images and isointense to the muscle on T1-weighted images, with no difference in signal characteristics between the in-phase and out-of-phase images.
Grossly, there was a 4.1 cm well circumscribed brown tumor. Histologically, the lesion was composed of bland adrenal cortical cells without areas of necrosis or increased mitotic activity. There was no capsular or lymphovascular invasion noted. The adrenal cortical adenoma was positive for inhibin, calretinin and MART-1 and was negative for S-100 and WT-1. In addition to the adenoma there was a fibroblastic “radial-scar”-like spindle cell proliferation noted admixed with the adrenal cortical tissue and in continuity with the capsule. The spindle cell proliferation was positive for WT-1 and focally positive for inhibin and calretinin.
The patient underwent surgical excision of the adrenal gland.
To the best of the knowledge, this is the first case report describing Ovarian thecal metaplasia (OTM) in the context of BWS with detailed imaging description of this entity. However OTM diagnosis is possible only after histological examination as the imaging features of OTM overlap with those seen in adrenocortical carcinoma and pheochromocytoma.
Beckwith Wiedemann syndrome, previously called exomphalos-macroglossia-gigantism
This case report represents radiological features of a unique adrenal pathology in Beckwith Wiedemann syndrome, ovarian thecal metaplasia of the adrenal gland should be considered in patients with BWS beside adrenocortical carcinoma.
The paper is well written and sustained by appropriate iconography.
P- Reviewer: Boy C, Baglaj MS, Storto G S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
| 1. | Giorgadze TA, Roy S, Fraker DL, Brooks JS, Livolsi VA. Pathologic quiz case: a 49-year-old woman with an adrenal mass. Pancreatic tissue with nesidiodysplasia, adrenocortical adenoma, and ovarian thecal metaplasia in the adrenal gland. Arch Pathol Lab Med. 2004;128:1294-1296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 2. | Mete O, Raphael S, Pirzada A, Asa SL. Is adrenal ovarian thecal metaplasia a misnomer? Report of three cases of radial scar-like spindle cell myofibroblastic nodule of the adrenal gland. Endocr Pathol. 2011;22:222-225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 3. | Wont TW, Warner NE. Ovarian thecal metaplasia in the adrenal gland. Arch Pathol. 1971;92:319-328. [PubMed] |
| 4. | Fidler WJ. Ovarian thecal metaplasia in adrenal glands. Am J Clin Pathol. 1977;67:318-323. [PubMed] |
| 5. | Lack EE. Tumors of the adrenal gland and extra-adrenal paraganglia. Washington, D.C. : Armed Forces Institute of Pathology 1997; . |
| 6. | DeBaun MR, Tucker MA. Risk of cancer during the first four years of life in children from The Beckwith-Wiedemann Syndrome Registry. J Pediatr. 1998;132:398-400. [PubMed] |
| 7. | Thorburn MJ, Wright ES, Miller CG, Smith-Read EH. Exomphalos-macroglossia-gigantism syndrome in Jamaican infants. Am J Dis Child. 1970;119:316-321. [PubMed] |
| 8. | Taide DV, Bendre PS, Redkar R, Hambarde S. Adrenal masses associated with Beckwith Wiedemann syndrome in the newborn. Afr J Paediatr Surg. 2010;7:209-210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Northcutt BG, Raman SP, Long C, Oshmyansky AR, Siegelman SS, Fishman EK, Johnson PT. MDCT of adrenal masses: Can dual-phase enhancement patterns be used to differentiate adenoma and pheochromocytoma? AJR Am J Roentgenol. 2013;201:834-839. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 52] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 10. | Berland LL, Silverman SG, Gore RM, Mayo-Smith WW, Megibow AJ, Yee J, Brink JA, Baker ME, Federle MP, Foley WD. Managing incidental findings on abdominal CT: white paper of the ACR incidental findings committee. J Am Coll Radiol. 2010;7:754-773. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 624] [Cited by in RCA: 606] [Article Influence: 40.4] [Reference Citation Analysis (0)] |