Published online Dec 28, 2014. doi: 10.4329/wjr.v6.i12.907
Revised: October 7, 2014
Accepted: November 7, 2014
Published online: December 28, 2014
Processing time: 67 Days and 19.4 Hours
AIM: To assess and compare the image quality of 4% sorbitol and diluted iodine 2% (positive oral contrast agent) in abdomino-pelvic multi-detector computed tomography.
METHODS: Two-hundred patients, referred to the Radiology Department of a central educational hospital for multi-detector row abdominal-pelvic computed tomography, were randomly divided into two groups: the first group received 1500 mL of 4% sorbitol solution as a neutral contrast agent, while in the second group 1500 mL of meglumin solution as a positive contrast agent was administered in a one-way randomized prospective study. The results were independently reviewed by two radiologists. Luminal distension and mural thickness and mucosal enhancement were compared between the two groups. Statistical analysis of the results was performed by Statistical Package for the Social Sciences software version 16 and the Mann-Whitney test at a confidence level of 95%.
RESULTS: Use of neutral oral contrast agent significantly improved visualization of the small bowel wall thickness and mural appearance in comparison with administration of positive contrast agent (P < 0.01). In patients who received sorbitol, the small bowel showed better distention compared with those who received iodine solution as a positive contrast agent (P < 0.05).
CONCLUSION: The results of the study demonstrated that oral administration of sorbitol solution allows better luminal distention and visualization of mural features than iodine solution as a positive contrast agent.
Core tip: In this study, performed on 200 cases, we randomly divided the cases into two groups receiving either meglumin as a positive contrast or sorbitol as a negative contrast for abdominal and pelvic computed tomography. Our study showed that luminal distension and mural thickness was significantly better delineated with neutral contrast agent compared with positive contrast solution.
- Citation: Hashemi J, Davoudi Y, Taghavi M, Pezeshki Rad M, Moghadam AM. Improvement of distension and mural visualization of bowel loops using neutral oral contrasts in abdominal computed tomography. World J Radiol 2014; 6(12): 907-912
- URL: https://www.wjgnet.com/1949-8470/full/v6/i12/907.htm
- DOI: https://dx.doi.org/10.4329/wjr.v6.i12.907
The standard method to distend the gastrointestinal tract (GIT) in multi-detector computed tomography (CT) [multiple detector computed tomography (MDCT)] is administration of high-attenuation contrast agents such as barium or diluted iodine (DI) to visualize the stomach and small bowel[1,2]. However, a search for different contrast materials to improve the image quality in abdominal MDCT is desired[3]. This is important for better mural enhancement and depiction of bowel wall vs intraluminal content[4]. Use of neutral or non-radiopaque contrast agents can help to improve visualization of bowel wall and image quality[5]. It has previously been shown that neutral agents are beneficial in the CT diagnosis of Crohn’s disease, neoplasms, bowel ischemia, and hemorrhage[6,7]. Neutral agents are also used in the diagnosis of pancreatic and biliary tract disease, by providing better delineation and distention of the duodenum[8]. There are a number of neutral contrast agents that have been used widely throughout years. Whole milk, often used for this purpose, may not be well-tolerated by many patients and is difficult to store, which limits its usage[9]. The unfavorable taste of methylcellulose solution makes it unpopular; and polyethylene glycol solution, despite its excellent bowel distention, is cathartic[10]. Manitol, another neutral contrast agent, is available only in hospitals in Iran, so its administration is limited in the outpatient ward[11-13]. The most prevalent neutral contrast material, which is used extensively, is water[14]. Water has a slow intestinal transit that gives it a good contrast capacity in the upper part of the GIT. However, rapid absorption by the distal part of the small bowel, limits its usage in this part of the GIT[15-17]. Adding high-osmolality materials to water might slow down its absorption. One of these additive agents is sorbitol, a cost-effective, neutral oral contrast agent[18]. Sorbitol has been applied with low-density barium (Volumen) for detection of small bowel disorders[14,19]. To our knowledge, sorbitol alone has not been previously used as a neutral oral contrast agent for abdominal MDCT in a large non-homogenous group of patients. Paying attention to cost-effectiveness of sorbitol and lack of the availability of Volumen in our country, we decided to assess and compare the image quality of 4% sorbitol and diluted iodine 2% (positive oral contrast agent) in abdomino-pelvic MDCT.
A randomized clinical study using a random-numbers table was performed on 200 patients with various gastrointestinal or abdominal complaints, who were referred to out teaching hospital for a MDCT.
Patients older than 18 years old were selected and divided into two groups of equal number, undergoing 100 CT scan examination with positive contrast agent and another 100 with neutral contrast. Patient exclusion criteria were acute intestinal obstruction; acute intestinal inflammatory or infectious disease; recent bowel surgery; fluid-restricted diet; inability to drink; and gastrointestinal perforation. Groups were pair-matched in demographic characteristics such as age and weight. Patients were asked not to eat or drink for at least 6 h before radiologic examination. There were equal number of male and female subjects in both groups.
This one-way blinded randomized prospective study was approved by our institutional Ethics Committee. The study protocol was explained to all patients, and after obtaining written informed consent, they were entered into the study.
Patients were divided into two groups and randomly received neutral or positive oral contrast agents. The total volume of contrast agent consumption for each patient was recorded in order to estimate compliance. Standard protocol was used for contrast agent administration. For each group, 1500 mL of contrast agent was administered over 60 min. Patients were observed closely by a trained nurse for the possible complications such as allergic reactions or gastrointestinal symptoms. The positive oral contrast group received 2% DI solution which had been compounded by diluting 20 mL of meglumin diatrizoate compound in 1480 mL of water (each meglumin vial contains 370 mg/mL iodine). In the second group, a 4% sorbitol solution was administered as a neutral oral contrast and prepared using 60 g of sorbitol sugar mixed in 1500 mL of water. For sorbitol sugar, we used 12 sachets of sorbitol, each containing 5 g of sorbitol.
All MDCT examinations were conducted on the same equipment, a 16-detector unit (Neusoft Inc., China). The procedure lasted 30-35 min and was conducted using the same technique for all patients. Patients lay in the supine position on the CT table and modifications in the general abdominal scan protocol were minimal. After obtaining topograms, a single phase acquisition in 60-90 s was performed from diaphragm to the symphysis pubis. Each axial section was 5 mm thick, with a gap of 5 mm between slices. Coronal images with 1.5 mm thickness and 2 mm gap were reconstructed automatically; this view was referred to as the space between the anterior abdominal wall and the paravertebral muscles. Sagittal reconstructions were generated as required. In each group, 1500 mL of contrast agent was administered within 60 min. Before imaging, an intravenous line was placed in all patients and 120 mL of intravenous contrast material with concentration of 300 mg/mL iodine was administered by a power injector at rate of 3-4 mL/severe central canal narrowing followed by infusion of 50 mL of normal saline. At the end of the imaging, all cases were coded, identifiers were deleted, and the studies were maintained for further analysis.
Two radiologists interpreted and re-reviewed the data independently. Both radiologists had five years of experience in body imaging. Because we designed the study to compare neutral and positive contrast agents, we were unable to blind our reviewers/radiologists to the type of material used. A five-point scale (0 = worst, 4 = best) was used to determine the quality of images as well as the intestinal wall delineation. The latter was classified from indistinguishable (0) to completely visible (4). Overall image quality was varied from unspecified (0) to perfect (4) according to Likert Scale[14]. The maximum horizontal diameter of duodenum, jejunum, and terminal ileum were measured from one inner margin wall to the other one.
Data was analyzed by SPSS version 16. Descriptive statistical analysis of the demographics was performed. To compare the reported scores of the neutral oral contrast and positive contrast groups for intestinal distention and overall image quality by the radiologists, the Mann-Whitney U-test was performed. The difference between the overall image quality scores of both groups was also compared by performing the Mann-Whitney U-test (P = 0.05). Inter-observer variability was tested by Cohen’s kappa correlation test.
All 200 patients tolerated the contrast agents well, and none of the patients developed gastrointestinal symptoms or allergic reactions to any of the oral contrast agents. No serious side effects were reported. The mean duodenal, jejunal and ileal diameter reported by both radiologists is shown in Table 1. The mean diameter after neutral contrast material was significantly higher than that of positive contrast agent for duodenum (first radiologist: 9.1 vs 13.3; second radiologist 9.08 vs 12.88) and ileum (first radiologist: 15.6 vs 18.1; second radiologist 15.4 vs 18.1). However, the difference was not statistically significant for jejunum (first radiologist: 15.3 vs 14.7; second radiologist 15.3 vs 14.6). The inter-observer variability for wall thickness of intestinal loops was reasonably good with Spearman correlation values of 0.997-0.989.
| Duodenum mean± SD | Mann Whitney P value | Jejunum mean ± SD | Mann Whitney P value | Ileum mean± SD | Mann Whitney P value | |
| First radiologist | 0.009 | 0.62 | 0.014 | |||
| Positive | 9.1 ± 0.633 | 15.3 ± 0.81 | 15.6 ± 0.66 | |||
| Neutral | 13.3 ± 1.09 | 14.76 ± 0.75 | 18.1 ± 0.71 | |||
| Total | 11.2 ± 0.66 | 15.03 ± 0.55 | 16.8 ± 0.5 | |||
| Second radiologist | 0.018 | 0.59 | 0.02 | |||
| Positive | 9.08 ± 0.65 | 15.3 ± 0.88 | 15.4 ± 0.65 | |||
| Neutral | 12.88 ± 1.07 | 14.68 ± 0.76 | 18.1 ± 0.65 | |||
| Total | 11.0 ± 0.65 | 14.99 ± 0.55 | 16.77 ± 0.48 | |||
| Spearman correlation | 0.997 | 0.989 | 0.997 | |||
In Table 2, radiologists’ satisfaction with the quality of imaging was compared. Both agreed that it was significantly higher in the neutral contrast agent group. Wall delineation was significantly better in the neutral contrast group, as well (Table 3). Inter-observer agreement evaluated by kappa statistics demonstrated that there was no significant difference between the two observers regarding visibility of the wall (P = 0.894) and image satisfaction (P = 0.839).
| Score | First radiologist | Second radiologist | ||||
| Neutral | Positive | P value | Neutral | Positive | P value | |
| Satisfaction | ||||||
| 0 | 0 | 48 | 2 | 50 | ||
| 1 | 8 | 6 | < 0.000 | 4 | 8 | < 0.000 |
| 2 | 6 | 34 | 8 | 30 | ||
| 3 | 0 | 4 | 2 | 6 | ||
| 4 | 86 | 8 | 84 | 6 | ||
| Kappa correlation | 0.839 | |||||
| Score | First radiologist | Second radiologist | ||||
| Positive | Neutral | P value | Positive | Neutral | P value | |
| Wall delineation | ||||||
| 0 | 62 | 0 | 66 | 2 | ||
| 1 | 14 | 10 | < 0.000 | 14 | 8 | 0.004 |
| 2 | 22 | 10 | 18 | 10 | ||
| 3 | 2 | 0 | 0 | 80 | ||
| 4 | 0 | 80 | 2 | |||
| Kappa correlation | 0.894 | |||||
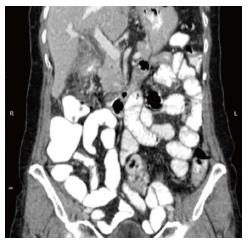
In Figures 1 and 2, a sample coronal reconstruction of an abdominal-pelvic CT scan using neutral and positive contrast agents is shown. As can be seen in Figure 1, the coronal reconstruction of the abdominal and pelvic CT scan using a neutral oral contrast agent, there is excellent visualization of the wall of the small intestine and good distention of the bowel loops. However, in Figure 2, which was performed with positive contrast agent, there is poor distention of the bowel loops and poor visualization of the small intestine wall.
Our study demonstrated that small bowel distention is significantly improved by the usage of neutral contrast agent (sorbitol solution), especially for duodenum and ileum. It also demonstrated the value of a neutral contrast agent in displaying the intestinal wall. We used a 4% sorbitol solution as a neutral contrast agent hypothesizing that sorbitol’s osmolarity would lead to better luminal distention, higher differentiation between the bowel wall and the hypo-dense intraluminal content, and detailed delineation and evaluation of mural features. Our results showed that administration of neutral luminal oral contrast agent combined with use of multi-detector CT scanners leads to improved assessment of the bowel wall and its vascularity[7].
While the volume of the oral contrast agent administered in our study was less than the 1800 mL used in other studies such as in Shanmuganathan[8], we were still able to obtain radiologic images of excellent quality. To optimize the contrast agent’s performance, two-thirds of the total volume (900-1000 mL) administered was in divided doses consumed over the period of 20-30 min before scanning, and the remaining third (200-300 mL) was consumed when the patients entered the scanning suite. In the traditional oral contrast administration protocol, this stage lasts 45-60 min. In this study, acceleration without decreasing image quality improved patients’ compliance. Naeger emphasized the role of positive oral contrast in identifying normal appendices[19]. Megibow et al[20] showed that Volumen would be a good contrast agent for gastrointestinal wall visualization. Sample size in the current study was larger than in Megibow et al[20]. Additionally, patients studied by Megibow et al[20] were limited to those who had pancreatic or biliary disease. We performed this study in a tertiary referral academic hospital, so that the studied population could be representative of the general population.
Oliva et al[21] concluded that orally administered neutral barium suspension resulted in better visualization and distention of the gastrointestinal tract in comparison with positive barium sulphate suspension or water. The same findings were obtained in our study due to higher osmolarity of sorbitol in comparison with diluted iodine. While DI does not induce osmotic gap, and the solution is absorbed by the GI tract and therefore bowel distension is decreased in the distal parts, sorbitol solution is a non-digestible agent which increases the volume of physiologic fluids secreted by the upper GI tract, due to its osmotic effect. Moreover, many studies confirmed that low-density barium suspension with sorbitol was better-tolerated in patients who required oral contrast agents[15,22]. Otero et al[23] evaluated the effect of low-density neutral contrast agent on image quality in patients with malignancy undergoing positron emission tomography/CT, and showed that this agent improved image quality without any side effects[23]. In some of the previous studies, such as Berther et al[24] and Meindl et al[25], 3% mannitol was used as a neutral contrast agent. The final results of this study were similar to ours, and confirmed that no matter what type of neutral contrast agent was used, image quality is enhanced, compared with those using positive contrast agents.
In conclusion, the results of this study demonstrate that neutral oral contrast agents provide better distention and visualization of gastrointestinal mural features when compared with positive oral contrast agents; both radiologists agreed completely with these results. Administration of neutral oral contrast did not diminish visualization of the bowel wall as induced by positive oral contrast materials. Thus, we concluded that the combination of MDCT technology and the radiologist’s supervision, besides evaluation of reconstructed images as required, can facilitate the detection and delineation of mural characteristics, especially by administration of neutral oral contrast agents. Our findings show that sorbitol is a safe, cost-effective, and easy-to-use neutral contrast agent which enhances image quality and is suitable for patients with various GIT disorders.
We would like to thank the research committee of the Mashhad University of Medical Science for their support, and also would like to thank all the patients who took part in our research and made this study possible.
Distending the bowel lumen is very important for visualization of bowel wall in multi-detector computed tomography (MDCT). For this purpose we can use positive contrast agents or neutral ones. There has always been a challenge about the advantages of using either of these agents. There are a number of neutral contrast agents using worldwide, the most popular being water. However, water is rapidly absorbed in the distal parts of small bowel and needs some high-osmolality additives.
Sorbitol is one the additives that might slow down the water absorption in the distal parts of gastrointestinal tract (GIT). However, Sorbitol alone has not been previously used as a neutral oral contrast agent for abdominal MDCT in a large non-homogenous group of patients. In the area of using neutral contrast agents in MCDT of GIT, the hot spot of this study was to assess and compare the image quality of 4% sorbitol and diluted iodine 2% (positive oral contrast agent) in abdomino-pelvic MDCT.
This study demonstrated that small bowel distention is significantly improved by the usage of neutral contrast agent (sorbitol solution), especially for duodenum and ileum. It also demonstrated the value of a neutral contrast agent in displaying the intestinal wall. While the volume of the oral contrast agent administered in this study was less than the 1800 mL used in other studies the authors were still able to obtain radiologic images of excellent quality. In this study, acceleration without decreasing image quality improved patients’ compliance. In some of the previous studies, 3% mannitol was used as a neutral contrast agent. The final results of this study were similar to theirs, and confirmed that no matter what type of neutral contrast agent the authors use; image quality is enhanced, compared with using positive contrast agents.
This study shows that sorbitol (as a neutral contrast agent) has a better capacity in distending bowel wall and therefore better delineates of the bowel wall in MCDT compared with positive contrast agents. This finding is more considerable in duodenum and ileum.
A Neutral contrast agent is a type of contrast material which is used in evaluation of the bowel wall in abdominal imaging. Unlike positive contrast materials, these type of contrasts are not iodinated based and do not increase the density of the bowel lumen. Sorbitol is a cost-effective, neutral oral contrast agent.
This is a good research study in which the authors assessed and compared the image quality of 4% sorbitol and diluted iodine 2% (positive oral contrast agent) in abdomino-pelvic MDCT.
P- Reviewer: Nouh MR, Tsalafoutas IA S- Editor: Qi Y L- Editor: A E- Editor: Lu YJ
| 1. | Horton KM, Fishman EK. Multidetector-row computed tomography and 3-dimensional computed tomography imaging of small bowel neoplasms: current concept in diagnosis. J Comput Assist Tomogr. 2004;28:106-116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 72] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 2. | Cademartiri F, Raaijmakers RH, Kuiper JW, van Dijk LC, Pattynama PM, Krestin GP. Multi-detector row CT angiography in patients with abdominal angina. Radiographics. 2004;24:969-984. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 32] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 3. | Anderson BA, Salem L, Flum DR. A systematic review of whether oral contrast is necessary for the computed tomography diagnosis of appendicitis in adults. Am J Surg. 2005;190:474-478. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 71] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 4. | Vandenbroucke F, Mortelé KJ, Tatli S, Pelsser V, Erturk SM, De Mey J, Silverman SG. Noninvasive multidetector computed tomography enterography in patients with small-bowel Crohn’s disease: is a 40-second delay better than 70 seconds? Acta Radiol. 2007;48:1052-1060. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 25] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 5. | Smevik B, Westvik J. Iohexol for contrast enhancement of bowel in pediatric abdominal CT. Acta Radiol. 1990;31:601-604. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 6. | Lafferty B. Oral contrast omission in the computed tomographic evaluation of blunt abdominal trauma: a literature review. J Trauma Nurs. 2012;19:E1-E4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Hekimoglu K, Yildirim UM, Karabulut E, Coskun M. Comparison of combined oral and i.v. contrast-enhanced versus single i.v. contrast-enhanced mdct for the detection of acute appendicitis. JBR-BTR. 2011;94:278-282. [PubMed] |
| 8. | Shanmuganathan K. Multi-detector row CT imaging of blunt abdominal trauma. Semin Ultrasound CT MR. 2004;25:180-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 52] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 9. | Allen TL, Mueller MT, Bonk RT, Harker CP, Duffy OH, Stevens MH. Computed tomographic scanning without oral contrast solution for blunt bowel and mesenteric injuries in abdominal trauma. J Trauma. 2004;56:314-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 55] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 10. | Fakhry SM, Brownstein M, Watts DD, Baker CC, Oller D. Relatively short diagnostic delays (< 8 hours) produce morbidity and mortality in blunt small bowel injury: an analysis of time to operative intervention in 198 patients from a multicenter experience. J Critical Care. 2000;48:408-415. [RCA] [DOI] [Full Text] [Cited by in Crossref: 238] [Cited by in RCA: 225] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 11. | Pal JD, Victorino GP. Defining the role of computed tomography in blunt abdominal trauma: use in the hemodynamically stable patient with a depressed level of consciousness. Arch Surg. 2002;137:1029-1032; discussion 1029-1132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 51] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 12. | Holmes JF, Offerman SR, Chang CH, Randel BE, Hahn DD, Frankovsky MJ, Wisner DH. Performance of helical computed tomography without oral contrast for the detection of gastrointestinal injuries. Ann Emerg Med. 2004;43:120-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 33] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 13. | Rodriguez C, Barone JE, Wilbanks TO, Rha CK, Miller K. Isolated free fluid on computed tomographic scan in blunt abdominal trauma: a systematic review of incidence and management. J Trauma. 2002;53:79-85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 63] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 14. | Lee CH, Haaland B, Earnest A, Tan CH. Use of positive oral contrast agents in abdominopelvic computed tomography for blunt abdominal injury: meta-analysis and systematic review. Eur Radiol. 2013;23:2513-2521. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 32] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 15. | Halsted MJ, Racadio JM, Emery KH, Kreymerman P, Poe SA, Bean JA, Donnelly LF. Oral contrast agents for CT of abdominal trauma in pediatric patients: a comparison of dilute hypaque and water. AJR Am J Roentgenol. 2004;182:1555-1559. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 16. | Lim BK, Bux SI, Rahmat K, Lam SY, Liew YW. Evaluation of bowel distension and mural visualisation using neutral oral contrast agents for multidetector-row computed tomography. Singapore Med J. 2012;53:732-736. [PubMed] |
| 17. | Hebert JJ, Taylor AJ, Winter TC, Reichelderfer M, Weichert JP. Low-attenuation oral GI contrast agents in abdominal-pelvic computed tomography. Abdom Imaging. 2006;31:48-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 26] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 18. | Young BM, Fletcher JG, Booya F, Paulsen S, Fidler J, Johnson CD, Huprich J, Barlow J, Trout A. Head-to-head comparison of oral contrast agents for cross-sectional enterography: small bowel distention, timing, and side effects. J Comput Assist Tomogr. 2008;32:32-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 65] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 19. | Naeger DM, Chang SD, Kolli P, Shah V, Huang W, Thoeni RF. Neutral vs positive oral contrast in diagnosing acute appendicitis with contrast-enhanced CT: sensitivity, specificity, reader confidence and interpretation time. Br J Radiol. 2011;84:418-426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 20. | Megibow AJ, Babb JS, Hecht EM, Cho JJ, Houston C, Boruch MM, Williams AB. Evaluation of bowel distention and bowel wall appearance by using neutral oral contrast agent for multi-detector row CT. Radiology. 2006;238:87-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 91] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 21. | Oliva MR, Erturk SM, Ichikawa T, Rocha T, Ros PR, Silverman SG, Mortele KJ. Gastrointestinal tract wall visualization and distention during abdominal and pelvic multidetector CT with a neutral barium sulphate suspension: comparison with positive barium sulphate suspension and with water. JBR-BTR. 2012;95:237-242. [PubMed] |
| 22. | Cadenas Rodríguez L, Martí de Gracia M, Saturio Galán N, Pérez Dueñas V, Salvatierra Arrieta L, Garzón Moll G. [Use of multidetector computed tomography for locating the site of gastrointestinal tract perforations]. Cir Esp. 2013;91:316-323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 23. | Otero HJ, Yap JT, Patak MA, Erturk SM, Israel DA, Johnston CJ, Sakellis C, Rybicki FJ, Van den Abbeele AD, Ros PR. Evaluation of low-density neutral oral contrast material in PET/CT for tumor imaging: results of a randomized clinical trial. AJR Am J Roentgenol. 2009;193:326-332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 24. | Berther R, Patak MA, Eckhardt B, Erturk SM, Zollikofer CL. Comparison of neutral oral contrast versus positive oral contrast medium in abdominal multidetector CT. Eur Radiol. 2008;18:1902-1909. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 25. | Meindl TM, Hagl E, Reiser MF, Mueller-Lisse UG. Comparison of 2 different protocols for ingestion of low-attenuating oral contrast agent for multidetector computed tomography of the abdomen. J Comput Assist Tomogr. 2007;31:218-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |