Published online Sep 28, 2013. doi: 10.4329/wjr.v5.i9.349
Revised: July 30, 2013
Accepted: August 12, 2013
Published online: September 28, 2013
Processing time: 140 Days and 20.4 Hours
We present a case of left ectopic ureter insertion into the left seminal vesicle which is a rare anomaly. The incidence of ectopic insertion of the ureter is more common in females and is usually associated with incontinence, leading to the diagnosis, while in males it is present with infection. Ectopic ureter is defined as abnormal insertion of the ureter, occurring in the posterior urethra in approximately 50% of cases in males. Other sites include the seminal vesicle (approximately one-third), vas deferens, bladder neck, prostate and epididymis, while the urethra and vagina are commonly affected in females. Management is usually addressed to the upper tract only; if there is incontinence it requires removal of the ureteric stump. Our case was initially diagnosed by magnetic resonance imaging and the diagnosis confirmed by computed tomography (CT) guided seminal vesiculography as transrectal guidance for seminal vesiculography was refused by the patient. CT guided seminal vesiculography is less painful and more tolerable than the transrectal route.
Core tip: We present the role of the traditional technique of computed tomography seminal vesiculography in the diagnosis of the rare anomaly of ectopic insertion of the ureter into the seminal vesicle in a male patient.
- Citation: El-Ghar MA, El-Diasty T. Ectopic insertion of the ureter into the seminal vesicle. World J Radiol 2013; 5(9): 349-351
- URL: https://www.wjgnet.com/1949-8470/full/v5/i9/349.htm
- DOI: https://dx.doi.org/10.4329/wjr.v5.i9.349
Ectopic insertion of the ureter is defined as abnormal insertion of the ureter, usually distal to the trigone into the urethra in male in approximately 50% of cases[1]. Other sites include the seminal vesicle (approximately one-third), vas deferens, bladder neck, prostate and epididymis, while the urethra and vagina are commonly affected in females. Ectopic insertion of the ureter in the genital tract is a rare anomaly. Its incidence, as reported by Fraser, is about 1:130000. It is more common in females and is usually associated with incontinence, leading to the diagnosis, while in males, it is present with infection
We present a case of ectopic insertion of the left ureter into the seminal vesicle (SV). It was initially diagnosed by magnetic resonance imaging (MRI) and confirmed by computed tomography (CT) seminal vesiculography.
A twenty eight year old male presented with terminal hematuria of 1 mo duration, with a history of left simple nephrectomy 25 years ago and open heart surgery for a ventricular septal defect 15 years ago. Clinical examination and laboratory investigations were free.
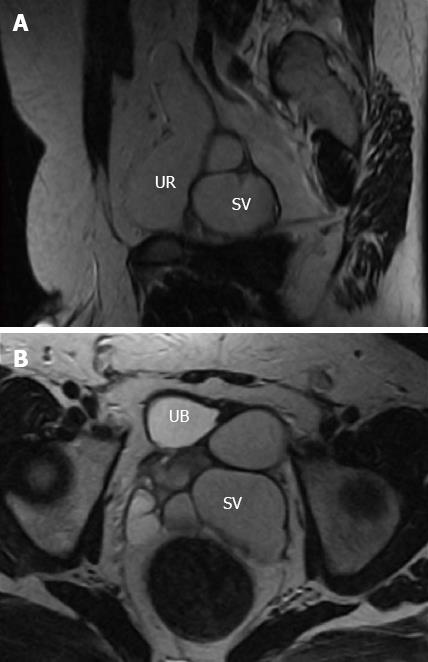
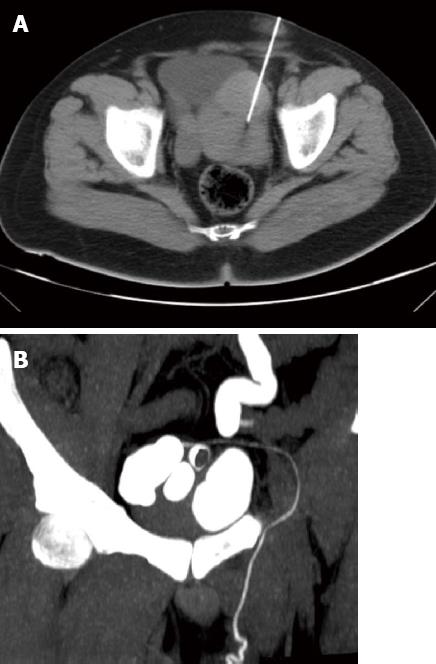
Pelvic ultrasound (US) showed a multilocular cystic lesion posterior to the bladder to the left (Figure 1). Ascending cystogram was free. MRI showed a tubular structure at the left representing the ureteric stump of the nephrectomized left kidney inserted into the dilated left seminal vesicle (Figure 2A). The left seminal vesicle showed altered fluid content (Figure 2B). CT guided puncture of the dilated left SV was done with injection of contrast inside (Figure 3A). Imaging of the abdomen and pelvis after SV puncture showed opacification of the left SV, the left ureter stump and the left vas deferens (Figure 3B).
There is an association between congenital anomalies of the seminal vesicle and urinary tract anomalies due to their close embryological relationship[2]. CT and MRI are used for accurate delineation of the ureteral insertion, while MRI is the modality of choice for seminal vesicle evaluation. The difficulty in the diagnosis of ectopic insertion of the ureter usually occurs when it is not dilated and its insertion cannot be identified; in this case, CT or MRI with contrast is required to confirm the diagnosis.
In a case of ectopic ureter, pelvic US can show the dilated SV as a cystic mass at the pelvis posterior to the bladder and also with dilated ipsilateral ureter if there is an associated kidney anomaly. Transrectal ultrasound (TRUS) allows better delineation of the cystic lesion wall and its relationship to the adjacent structures[3,4]. TRUS can also used in the puncture of the SV with contrast injection for further CT imaging.
Intravenous urography (IVU) may be of no value if the affected kidney is non-functioning. There may be smooth indentation of the bladder by the cystic lesion at IVU and ascending cystogram[3,4]. In our case, the seminal vesicle was not enlarged enough to indent the bladder at the cystogram.
CT shows the cystic lesion with low fluid density posterior to the bladder with no post-contrast enhancement and it can also diagnose associated renal anomalies[3-5].
MRI has a superior soft tissue contrast that easily allows differentiation of the pelvic structures and associated pelvic anomalies. At MRI, the seminal vesicles appear as elongated cystic structures with thin septa. It displays low signal intensity (SI) at T1-weighted and high SI at T2-weighted MRI. The SI may be altered if the SV fluid contains high protein[3,4]. MRI with gadolinium can delineate the ureteric course in the normal functioning kidney in the excretory phase and can also diagnose associated seminal vesicle abnormalities.
P- Reviewers Chen HW, Kaya C, Triantopoulou C, Wang PH S- Editor Gou SX L- Editor Roemmele A E- Editor Liu XM
| 1. | Cooper CS, Snyder HM. The ureter. 4th ed. In: Gillenwater JY, Grayhack JT, Howards SS, Mitchell ME, editors. Philadelphia: Lippincott Williams and Wilkins 2002; 2155. |
| 2. | Berrocal T, López-Pereira P, Arjonilla A, Gutiérrez J. Anomalies of the distal ureter, bladder, and urethra in children: embryologic, radiologic, and pathologic features. Radiographics. 2002;22:1139-1164. [PubMed] |
| 3. | Lebowitz RL, Olbing H, Parkkulainen KV, Smellie JM, Tamminen-Möbius TE. International system of radiographic grading of vesicoureteric reflux. International Reflux Study in Children. Pediatr Radiol. 1985;15:105-109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 815] [Cited by in RCA: 787] [Article Influence: 19.7] [Reference Citation Analysis (0)] |
| 4. | Rizzoni G, Perale R, Bui F, Pitter M, Pavanello L, Boscolo R, Passerini Glazel G, Macri C. Radionuclide voiding cystography in intrarenal reflux detection. Ann Radiol (Paris). 1986;29:415-420. [PubMed] |