Published online Sep 28, 2012. doi: 10.4329/wjr.v4.i9.413
Revised: September 2, 2012
Accepted: September 9, 2012
Published online: September 28, 2012
AIM: To evaluate cystic malformations of the cystic duct.
METHODS: Over a 2-year period, we came across 10 cases of cystic malformation of the cystic duct among patients who were investigated in our radiology department with ultrasonography, multidetector computed tomography, or magnetic resonance imaging for abdominal complaints. Radiological diagnosis of cystic malformation of the cystic duct was made on the basis of a dilated, nonvascular cystic structure near the porta hepatis, and visualization of a clear communication with either the gallbladder, normal caliber cystic duct and/or common bile duct (CBD) on at least one imaging modality.
RESULTS: Four of 10 patients had saccular dilatation of the cystic duct. Six patients had fusiform dilatation of the cystic duct, and two of these had only mild fusiform dilatation. Two patients had associated CBD dilatation and one had associated cystic duct calculi and malignancy.
CONCLUSION: Cystic malformations of the cystic duct should be recognized as a distinct type of choledochal cyst and should be added as type VI cyst in Todani’s classification.
- Citation: Maheshwari P. Cystic malformation of cystic duct: 10 cases and review of literature. World J Radiol 2012; 4(9): 413-417
- URL: https://www.wjgnet.com/1949-8470/full/v4/i9/413.htm
- DOI: https://dx.doi.org/10.4329/wjr.v4.i9.413
Congenital dilatation of the extrahepatic biliary tract with or without dilatation of the intrahepatic biliary tract is known as choledochal cyst[1]. Cystic malformations of the main biliary tract are rare, but well known and classified. Cystic malformations of the cystic duct are extremely rare and not well recognized[2]. Cystic duct malformations are often misdiagnosed or undiagnosed preoperatively[3-5]. However carefully performed ultrasonography (USG) alone or in combination with multidetector computed tomography (MDCT) or magnetic resonance cholangiopancreatography (MRCP) suggests the correct diagnosis most of the time. Awareness of this type of malformation as a distinct type of choledochal cyst would help in correct preoperative diagnosis and appropriate management.
Over a 2-year period, we came across 10 cases of cystic malformation of the cystic duct among patients who were investigated in our radiology department with USG, MDCT or magnetic resonance imaging (MRI) for abdominal complaints. Abdominal pain with or without jaundice was the main presenting symptom. USG was the first imaging modality in six cases. MDCT was the first imaging modality in four cases. A radiological diagnosis of cystic malformation of the cystic duct was made on the basis of a dilated, nonvascular cystic structure near the porta hepatis and visualization of clear communication with either the gallbladder, normal caliber cystic duct and/or common bile duct (CBD) on at least one imaging modality. Cystic duct diameter greater than that of the CBD in subjective terms and > 5 mm in objective terms was considered abnormal. A diameter of > 5 mm but < 10 mm was considered as mild dilatation.
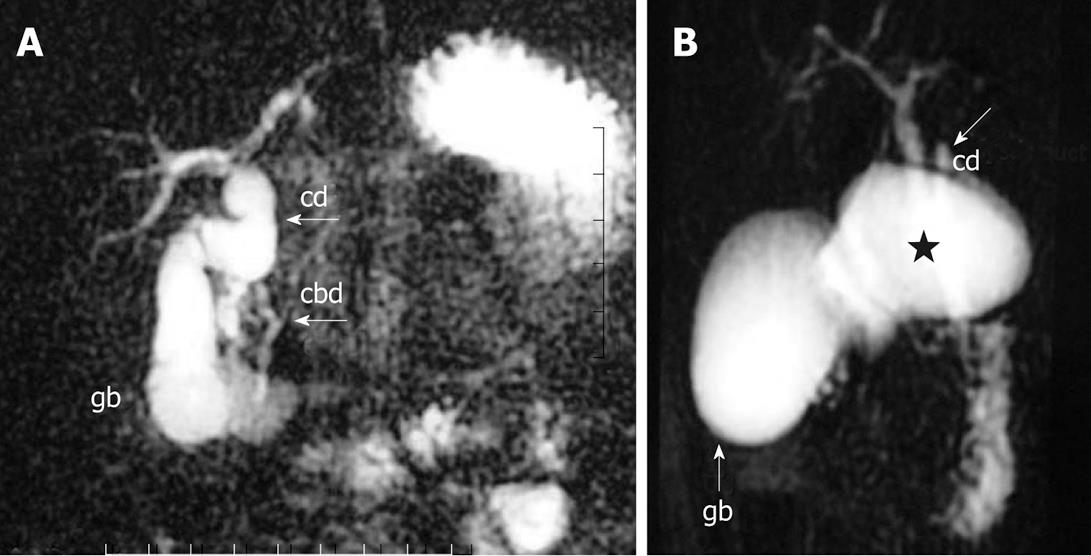
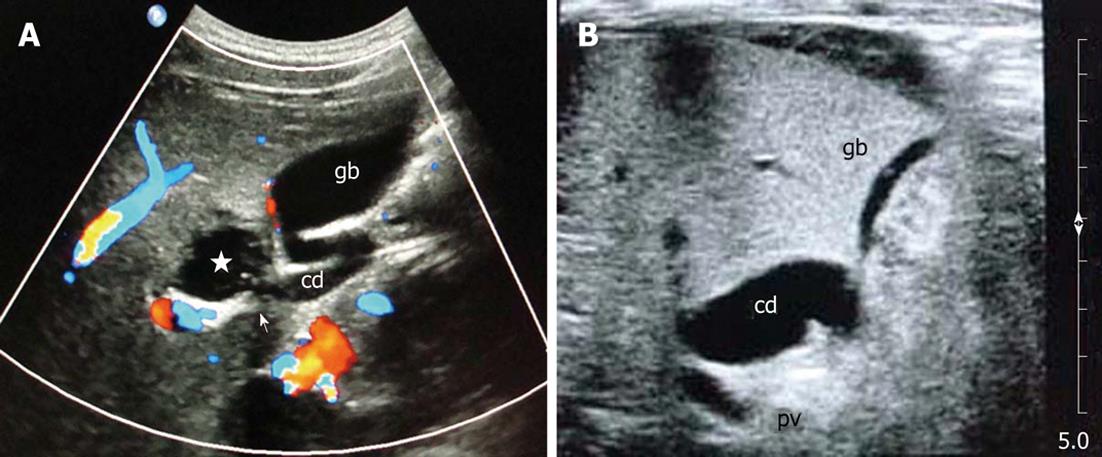
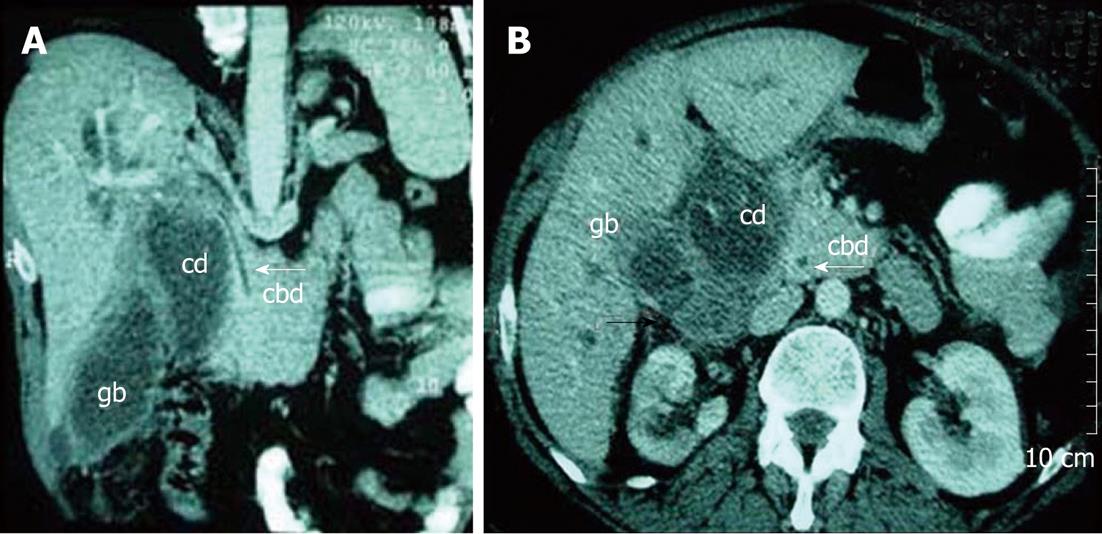
Patient age ranged from 6 d to 75 years, and there were five male and five female patients (Table 1). Six patients had fusiform cystic duct dilatation. Figure 1A shows fusiform dilatation of the cystic duct in a 7-year-old female child (Patient 6) complaining of recurrent abdominal pain. Note the high insertion of cystic duct and normal caliber CBD. Four patients had saccular cystic duct dilatation. Figure 2A shows focal saccular dilatation of the cystic duct in a 23-year-old male patient (Patient 7) complaining of right hypochondrium pain. Communication of the cyst with the normal proximal cystic duct was clearly seen on USG. Patients 1 and 2 showed a mild fusiform dilatation of the cystic duct. Figure 2B shows mild fusiform dilatation of the cystic duct in a 6-d-old female child (Patient 1) being investigated for neonatal jaundice, vomiting and abdominal distension. Patients 3 and 5 had associated fusiform CBD dilatation. Figure 3 shows fusiform dilatation of CBD and cystic duct in a 3-year-old female child (Patient 3) complaining of abdominal pain. Patient 8 had calculi and malignancy in a dilated cystic duct. Figure 4 shows saccular dilatation of cystic duct in a 55-year-old female patient (Patient 8) complaining of right hypochondrium pain and obstructive jaundice. A normal, distinctly separate CBD was seen (white arrow). Black arrow points to abnormal soft tissue suggesting malignancy.
| Patient | Age | Sex | Imaging | Cystic duct dilatation | Associated findings |
| 1 | 6 d | F | USG, MRCP | Mild fusiform | Gastric perforation |
| 2 | 4 mo | M | USG, MRCP | Mild fusiform | |
| 3 | 3 yr | F | USG, MRCP | Fusiform | Fusiform CBD dilatation |
| 4 | 4 yr | M | USG | Fusiform | |
| 5 | 4 yr | F | USG, MDCT | Fusiform | Fusiform CBD dilatation |
| 6 | 7 yr | F | MDCT, MRCP | Fusiform | |
| 7 | 23 yr | M | USG, MRCP | Saccular | |
| 8 | 55 yr | F | MDCT | Saccular | Cystic duct calculi and malignancy |
| 9 | 64 yr | M | MDCT, MRCP | Saccular | |
| 10 | 75 yr | M | MDCT, MRCP | Saccular |
Findings were confirmed at surgery in Patients 1, 3 and 5-8. Patient 1 had free intraperitoneal air on MRI. Surgery revealed gastric perforation. Intraoperative cholangiography confirmed mild dilatation of the cystic duct as seen on USG and MRI, however, it was not operated upon by the surgeon. Patient 2 had nonspecific complaints and the significance of the radiological finding of mildly dilated cystic duct was not clear, therefore, the patient was advised to undergo follow-up. Patient 4 had abnormal fusiform dilatation of the cystic duct on USG, but refused any further work-up. Patients 9 and 10 had a distinct saccular dilatation of the cystic duct evident on MDCT and MRCP. Figure 1B shows saccular dilatation of proximal cystic duct in a 75-year-old male patient (Patient 10) being investigated for non-related symptoms. Normal caliber distal cystic duct was also seen clearly. This was only an incidental finding on MDCT performed for nonrelated symptoms, and considering the patient’s age and absence of any obvious complication, only follow-up was advised.
Choledochal cyst is a congenital dilatation of the extrahepatic biliary tract with or without dilatation of the intrahepatic biliary tract[1]. Estimated prevalence of choledochal cysts varies from 1 in 13 000 to 1 in 2 million, and they are rare in the west and far more common in Japan and Asia. Type I choledochal cyst is the most common type (80%-90%)[6]. There is a female preponderance with a female to male ratio of 3-4:1. Choledochal cyst can present at any age. About two-thirds of patients are clinically symptomatic before the age of 10 years. The classic clinical triad of abdominal pain, jaundice and a palpable right upper quadrant mass is present in 30%-60% of patients presenting in the first decade of life and only in 20% of patients presenting later in life[1].
Choledochal cysts were originally classified into three types by Alonso-LEJ et al[7] in 1959. Other variations were subsequently recognized and the above classification was modified by Todani et al[8], which is presently the most accepted classification. The classification of Todani et al[8] describes five types of choledochal cysts, but does not describes choledochal cysts of the cystic duct.
Cystic malformation of the cystic duct is a less known entity. On extensive review of the literature, we could find only 16 such cases and most of them were limited to sporadic case reports[2-5,9-17]. In most of the reported cases a precise diagnosis of choledochal cyst of the cystic duct was made only intraoperatively[16]. Only Yoon et al[17] diagnosed all three cases preoperatively with CT or MRI. Over a span of 2 years, we encountered 10 cases of congenital dilatation of the cystic duct diagnosed preoperatively by imaging. Age range of our patients corresponded to other types of choledochal cysts. No sex predilection was found in our patients.
Presenting features and complications of choledochal cysts of the cystic duct are similar to other types of choledochal cysts. They might be asymptomatic and incidentally detected, or present with varying degrees of abdominal pain, jaundice, cholangitis, calculus disease and malignancy.
Although preoperative diagnosis of cystic malformation of the cystic duct can be challenging, in most cases a correct preoperative diagnosis can be suggested on careful radiological imaging. Endoscopic retrograde cholangiopancreatography can delineate the anatomy definitively, however, it is invasive in nature. Tc99m iminodiaceticacid cholescintigraphy can be used to determine the biliary origin of the cyst[5,15]. Intraoperative cholangiography can be a useful adjunct at surgery[9,10]. Helical CT cholangiography appears to be an ideal modality for accurately diagnosing such abnormalities, being noninvasive and highly informative[12]. MRCP or MDCT can also suggest the diagnosis most of the time. USG would be an initial imaging modality in many cases and it can accurately depict the cystic nature of the abnormality, diagnose any associated complications, and differentiate from a vascular etiology with the help of Doppler ultrasound. We found USG to be extremely helpful in correctly localizing the abnormality to the cystic duct, by tracing its connection to the gallbladder or normal portion of the cystic duct on one end, and tracing its connection to the CBD at the other end. However, USG is operator dependent and may fail to depict the biliary origin of the cyst. Therefore, a second line of investigation would be required in most cases for better delineation of anatomy, enhancing the preoperative diagnostic confidence and providing a road map to the surgeon. In our experience MRCP or MDCT along with carefully focused USG can suggest correct preoperative diagnosis most of the time. Any dilated nonvascular cystic structure near the porta hepatis should be evaluated for its connection with the biliary tract and its relationship with the gallbladder, and the cystic duct and CBD should be clearly delineated.
The normal diameter of the cystic duct varies from 1 to 5 mm[18]. Two distinct patterns of cystic duct dilatation were found in our patients: fusiform dilatation (n = 6) and saccular dilatation (n = 4). Saccular type choledochal cyst of the cystic duct may be confused with type II choledochal cyst (diverticulum of CBD)[11]. Saccular type choledochal cyst of the cystic duct can be distinguished from type II choledochal cyst only if a normal narrow caliber cystic duct can be identified between the choledochal cyst and CBD. If the choledochal cyst of the cystic duct has a wide opening into the CBD, it cannot be distinguished from type II choledochal cyst either radiologically or pathologically.
The exact etiopathology of choledochal cysts is not clear. Two theories are most prevalent. Babbitt has proposed the theory of anomalous pancreaticobiliary junction (APBJ) with a long common channel, resulting in reflux of pancreatic juice into the biliary tract, with resultant inflammation, scarring and biliary dilatation[1]. This can explain type I, III and IV cysts but does not explain type II and V cysts where the CBD is normal. Some believe that these cysts are congenital due to distal aganglionosis and proximal dilatation[19]. The initial case reports of choledochal cysts of the cystic duct do not discuss APBJ. Weiler et al[13] and Noun et al[14] describe an association of choledochal cysts of the cystic duct with APBJ, although no conclusive etiological role has been established. The exact etiology remains debatable, although some authors favor congenital etiology over APBJ as far as choledochal cysts of the cystic duct are concerned[10].
Manickam et al[5] have reported a case of choledochal cyst of the cystic duct, with apparent evolution of the choledochal cyst over a period of 1.5 years. However, it is not clearly evident from their article, and it appears to us that the choledochal cyst was mistaken for Hartmann’s pouch on initial USG. However, the concept of evolution is interesting and needs to be considered. Two of our 10 patients were infants (aged 6 d and 4 mo) and they showed a distinct abnormal dilatation of the cystic duct, but it was not a sizeable cyst and measured > 5 mm but < 10 mm in diameter. Four patients who were in the pediatric age group (3-7 years) had a fusiform cystic duct dilatation of > 10 mm. All four adult patients (23-75 years) had saccular dilatation of the cystic duct. A choledochal cyst may evolve over a period of time due to repeated infection and inflammation. Mild choledochal cysts diagnosed in infancy or childhood, and not treated surgically for whatever reasons, need to be followed up closely to look for apparent evolution and complications.
Treatment for type I, II and IV choledochal cysts is complete excision and subsequent biliary-enteric anastomosis for drainage[1]. Some treat type II cysts by simple excision[9]. There are no uniform guidelines for the treatment of choledochal cysts of the cystic duct. Some treat isolated choledochal cysts of the cystic duct with a narrow opening in the CBD with simple cholecystectomy and cyst excision either by open surgery or laparoscopically[2,5,9,10] and some prefer complete excision with biliary drainage[13,14]. We recommend complete excision with biliary drainage, in view of the increased risk of developing bile duct and gallbladder cancer in the presence of cystic biliary duct anomalies and APBJ.
In conclusion, cystic malformations of the cystic duct share features common to other types of choledochal cysts in Todani’s classification. Although rare, they need to be recognized. We recommend modification of Todani’s classification and inclusion of cystic malformations of the cystic duct as type VI choledochal cysts. It is not clear whether the milder forms of abnormally dilated cystic duct seen in our infantile patients are an arrested form of the symptomatic choledochal cyst or have the potential to grow into symptomatic cysts with age. Such cases require long-term follow-up to determine the exact significance, future course of events and appropriate management.
Choledochal cysts of the cystic duct are considered to be very rare. They are not described in the widely accepted Todani’s classification of choledochal cysts. There is a lack of awareness of this entity, resulting in missing the diagnosis altogether or confusing it with other types of choledochal cysts, and inappropriate treatment.
There is a lack of proper guidelines for diagnosis and management of choledochal cysts of the cystic duct. In this study, the authors highlight preoperative diagnosis and appropriate management of choledochal cysts of the cystic duct.
To date, only a few sporadic case reports have been published in the literature, of which, most cases were diagnosed correctly only during surgery. In the present study, the authors presented a series of cases correctly diagnosed preoperatively. Furthermore, the condition may not be as rare as previously thought, and the authors suggest that choledochal cysts of the cystic duct should be included as a distinct entity in Todani’s classification of choledochal cysts.
Awareness of choledochal cysts of the cystic duct as a distinct type of choledochal cyst would lead to its consideration in the preoperative differential diagnosis, and correct preoperative diagnosis will help with appropriate treatment.
Choledochal cyst is congenital dilatation of the biliary tract. Todani’s classification describes five types of choledochal cysts depending upon the part of the biliary tract involved, but does not describes choledochal cysts of the cystic duct.
The article is well written. The information is interesting, new and important.
Peer reviewers: Francesco Lassandro, MD, Department of Radiology, Monaldi Hospital, Via Leonardo Bianchi, 80129 Napoli, Italy; Vlastimil Valek, MD, MBA, Professor, Department of Radiology, University Hospital Brno-Bohunice and Medical Faculty of Masaryk University, Jihlavska 20, 62800 Brno, Czech Republic
S- Editor Cheng JX L- Editor Kerr C E- Editor Xiong L
| 1. | Memel DS, Balfe DM, Semelka RC. The Biliary Tract. Computed body tomography with MRI correlation. 3rd ed. Philadelphia, NewYork: Lippincott-Raven Publishers 1998; 779-844. |
| 2. | Champetier P, Partensky C, Ponchon T. Cystic malformations of the cystic duct. Surg Radiol Anat. 1987;9:287-291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Serena Serradel AF, Santamaría Linares E, Herrera Goepfert R. Cystic dilatation of the cystic duct: a new type of biliary cyst. Surgery. 1991;109:320-322. [PubMed] |
| 4. | Bode WE, Aust JB. Isolated cystic dilatation of the cystic duct. Am J Surg. 1983;145:828-829. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 34] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Manickam S, Ramadan K, Adams BK. A rare choledochal cyst of the cystic duct with an anomalous pancreaticobiliary union in an adult patient. Clin Rad Extra. 2004;59:68-71. [RCA] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (1)] |
| 6. | Harun SM, Abdullah BJJ, Rajasingam V. What cyst is this? Biomed. Imaging Interv J. 2007;3:e44. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 7. | Alonso-LEJ F, Rever WB, Pessagno DJ. Congenital choledochal cyst, with a report of 2, and an analysis of 94, cases. Int Abstr Surg. 1959;108:1-30. [PubMed] |
| 8. | Todani T, Watanabe Y, Narusue M, Tabuchi K, Okajima K. Congenital bile duct cysts: Classification, operative procedures, and review of thirty-seven cases including cancer arising from choledochal cyst. Am J Surg. 1977;134:263-269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 934] [Cited by in RCA: 835] [Article Influence: 17.4] [Reference Citation Analysis (0)] |
| 9. | Chan ES, Auyang ED, Hungness ES. Laparoscopic management of a cystic duct cyst. JSLS. 2009;13:436-440. [PubMed] |
| 10. | Bresciani C, Gama-Rodrigues J, Santos VR. Video-laparoscopic treatment of a sizeable cyst of the cystic duct: a case report. Surg Laparosc Endosc. 1998;8:376-379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | Loke TK, Lam SH, Chan CS. Choledochal cyst: an unusual type of cystic dilatation of the cystic duct. AJR Am J Roentgenol. 1999;173:619-620. [PubMed] |
| 12. | Baj M, Sengupta S, O’Donnell LJD. Choledochocele of the cystic duct: a case report. Internet J Gastroenterol. 2002;1. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 13. | Weiler H, Grandel A, Frühmorgen P. [Congenital cystic dilatation of the cystic duct associated with an anomalous pancreaticobiliary ductal junction]. Ultraschall Med. 2003;24:197-201. [PubMed] |
| 14. | Noun R, Sayegh R, Tohme-Noun C, Honein K, Smayra T, Aoun N. Extracystic biliary carcinoma associated with anomalous pancreaticobiliary junction and cysts. J Hepatobiliary Pancreat Surg. 2006;13:577-579. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 15. | Conway WC, Telian SH, Wasif N, Gagandeep S. Type VI biliary cyst: report of a case. Surg Today. 2009;39:77-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 16. | De U, Das S, Sarkar S. Type VI choledochal cyst revisited. Singapore Med J. 2011;52:e91-e93. [PubMed] |
| 17. | Yoon JH. Magnetic resonance cholangiopancreatography diagnosis of choledochal cyst involving the cystic duct: report of three cases. Br J Radiol. 2011;84:e18-e22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 18. | Turner MA, Fulcher AS. The cystic duct: normal anatomy and disease processes. Radiographics. 2001;21:3-22; questionnaire 288-294. [PubMed] |
| 19. | Singham J, Schaeffer D, Yoshida E, Scudamore C. Choledochal cysts: analysis of disease pattern and optimal treatment in adult and paediatric patients. HPB (Oxford). 2007;9:383-387. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 58] [Article Influence: 3.2] [Reference Citation Analysis (1)] |