Published online Mar 28, 2012. doi: 10.4329/wjr.v4.i3.102
Revised: February 28, 2012
Accepted: March 7, 2012
Published online: March 28, 2012
AIM: To determine the influence of anthropomorphic parameters on the relationship between patient centering, mean computed tomography (CT) numbers and quantitative image noise in abdominal CT.
METHODS: Our Institutional Review Board approved study included 395 patients (age range 21-108, years; male:female = 195:200) who underwent contrast-enhanced abdominal CT on a 16-section multi-detector row scanner (GE LightSpeed 16). Patient centering in the gantry isocenter was measured from the lateral localizer radiograph (off center S = patient off centered superior to isocenter; off center I = patient off centered inferior to isocenter). Mean CT numbers (Hounsfield Units: HU) and noise (standard deviation of CT numbers: SD) were measured in the anterior (aHU, aSD) and posterior (pHU, pSD) abdominal wall subcutaneous fat and liver parenchyma (LivHU, LivSD) at the level of the porta hepatis. Patients’ age, gender, weight, body mass index and maximal anteroposterior diameter were recorded. The data were analyzed using linear regression analysis.
RESULTS: Most patients (81%; 320/395) were not correctly centered in the gantry isocenter for abdominal CT scanning. Mean CT numbers in the abdominal wall increased significantly with an increase in the off-centering distance, regardless of the direction of the off-center (P < 0.05). There was a substantial increase in pSD (P = 0.01) and LivSD (P = 0.017) with off-centering. Change in mean CT numbers and image noise along the off-center distance was influenced by the patient size (P < 0.01).
CONCLUSION: Inappropriate patient centering for CT scanning adversely affects the reliability of mean CT numbers and image noise.
- Citation: Kim MS, Singh S, Halpern E, Saini S, Kalra MK. Ablation margin assessment of liver tumors with intravenous contrast-enhanced C-arm computed tomography. World J Radiol 2012; 4(3): 102-108
- URL: https://www.wjgnet.com/1949-8470/full/v4/i3/102.htm
- DOI: https://dx.doi.org/10.4329/wjr.v4.i3.102
Increasing use of computed tomography (CT) has raised concerns about potential risk of radiation-induced carcinogenesis. Clinical and technical strategies have been suggested to reduce radiation dose without compromising diagnostic information[1-6]. For radiation dose reduction, current multi-detector row computed tomography (MDCT) scanners are armed with several technologies such as X-ray intensity shaping bow-tie filters and automatic exposure control (AEC) techniques.
Bow-tie or beam shaping filters configure the X-ray beam to the cross-sectional geometry of the body region being scanned, so that the thinner peripheral portion of the body receives a lower radiation dose compared to the thicker central portion of the cross section[7]. These filters affect the incident X-ray beam characteristics which in turn affect their attenuation from the patient. Errors in centering of patients in the CT gantry isocenter can result in overestimation or underestimation of regional X-ray attenuation, which in turn can lead to erroneous estimation of tube current with the AEC techniques[3]. Thus, both bow-tie filters and AEC techniques require optimum patient centering within the gantry isocenter to reduce radiation dose while maintaining diagnostic image quality[8].
Previous studies have shown that inappropriate patient centering on the gantry affects image quality and radiation dose obtained with AEC techniques[9,10]. However, the effect of patient off-centering on mean CT numbers and image noise has not been assessed with respect to patient size. Therefore, the purpose of our study is to determine the influence of anthropomorphic parameters on the relationship between patient centering, mean CT numbers and quantitative image noise in abdominal CT.
This retrospective study was approved by the Human Research Committee of the Institutional Review Board of Massachusetts General Hospital.
The requirement for informed consent was waived. The study protocol was in compliance with the Health Insurance Portability and Accountability Act.
The study comprised 395 consecutive patients who underwent routine abdominal CT (mean age, 57 years; age range, 21-108 years) at a single tertiary health care hospital in October 2009. There were 195 male patients (49%, 195/395 patients; mean age, 57 years; age range, 21-108 years) and 200 female patients (51%, 200/395 patients; mean age, 57 years; age range, 20-94 years).
Patient body weight and body mass index [(BMI = weight in kg/(height in meters)2] were recorded. Maximal anteroposterior (AP) diameter of the abdomen was measured from the lateral localizer radiograph. Lateral localizer radiographs were preferred over transverse CT images, as often in large patients transverse CT images do not have skin to skin field of view, whereas lateral radiographs have skin to skin coverage in all patients from use of a large field of view of 50 cm.
The outcome variables of our study included CT numbers [Hounsfield units (HU)], and quantitative image noise [standard deviation of the CT numbers (SD)] measured in the subcutaneous fat of the anterior and posterior abdominal wall as well as in liver parenchyma.
Routine contrast-enhanced abdominal CT was performed on a 16-section multi-detector row scanner (GE LightSpeed 16; GE Healthcare, Waukesha, WI, United States) in all patients included in our study. In our institution, we acquired two localizer radiographs for each patient in lateral and AP projections at 80 kVp and 20 mA.
Transverse CT images were acquired from the top of the diaphragm to the pubic symphysis in all patients in single helical acquisition following administration of non-ionic contrast medium (Iopamidol 370 mg%, Bracco Diagnostics, Princeton, NJ, United States) injected at the rate of 2.5-3 cc per second. The scanning parameters comprised of 120 kVp, 0.5 s gantry rotation time, 1.375:1 beam pitch, 27.5 mm table speed per gantry rotation, and 16 × 1.25 mm detector collimation. Images were reconstructed with 5 mm section thickness at 5 mm intervals using a standard soft tissue reconstruction kernel.
A combined automatic exposure control technique (Auto mA 3D, GE Healthcare) was used to scan all patients. This technique uses the noise index as a surrogate for image quality, or more precisely, the average noise in the entire image. The Auto mA 3D technique performs tube current modulation at different projections (angular modulation or x-y modulation) with in individual section positions as well as at different section positions along the patient’s long axis or scanning direction (z-modulation). In addition to the noise index, the technique requires users to specify a range of tube current between which such tube current modulation should occur. The latter allows the user to control the extent of tube current modulation. As per our standard department protocols, the noise index is adjusted according to body weight: < 60 kg, 10 noise index; 61-90 kg, 12.5 noise index; > 91 kg, 15 noise index. The minimum and maximum tube current limits were set at 120 and 440 mA.
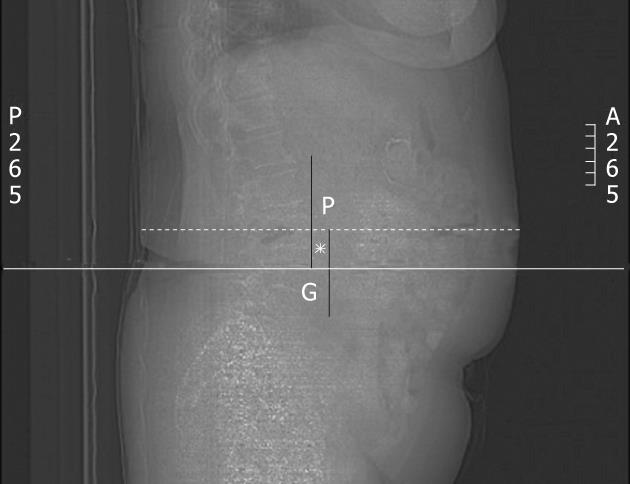
CT images were reviewed on a clinical web-based PACS within the firewalls of our hospital (Radamicas, Merge Healthcare, Hartland, WI, United States). Patient off-center distance from the gantry isocenter was measured from lateral localizer radiographs (Figure 1) by one of the authors (Kim MS with 10 years of experience). Off-centering of patients was estimated from the images by first determining the gantry isocenter as the midpoint of the entire image or the scan field of view. Next, the maximal anterior-posterior diameter of the patient was measured. Lastly, distance between the midpoints of maximal patient diameter and the gantry isocenter was measured to obtain the off-centering distance.
Once the lateral projection localizer radiograph is acquired, technologists plan the acquisition of transverse images. For reconstruction of transverse images, the planning field of view (FOV) defaults to the center of the localizer radiograph. In the case of appropriate patient centering, technologists only have to adjust the size of display FOV. However, with patient off-centering, in our experience the technologists change the position of display FOV without actually re-centering the patient in the gantry isocenter. This re-centering of display FOV rather than re-centering of the patient, leads to patient off-centering. Therefore, for the purpose of our study, we used localizer radiographs instead of transverse CT images to estimate patient off-centering. In addition, previously described automatic centering techniques have also used lateral localizer radiographs to estimate the extent of patient off-centering[7].
The off-center distance was arbitrarily divided into 5 groups based on the distance between the patient AP center on the lateral projection radiograph and the gantry isocenter; 0-5 mm (considered ideal centering), 6-10 mm, 11-20 mm, 21-30 mm and greater than 30 mm from the gantry isocenter. The direction of off-centering (superior and inferior) compared to gantry isocenter was also evaluated.
After measuring the distance and direction of off-centering, the mean CT numbers and their image noise (standard deviation of HU) were measured from the 5 mm contrast-enhanced transverse abdominal CT image in liver parenchyma at the level of the porta hepatis using a circular 30-50 mm2 region of interest (ROI). Mean CT numbers and image noise were measured in the anterior and posterior abdominal wall subcutaneous fat using circular 10-30 mm2 regions of interest.
CT dose index volume (CTDIvol in mGy) from the dose information page of each CT examination included in our study was recorded.
Data were tabulated in a spreadsheet program (Microsoft Excel; Microsoft, Inc., Princeton, NJ, United States). Statistical analysis was performed using a statistical analysis package (SAS/STAT 9.2; SAS Institute, Cary, NC, United States). Linear regression analysis was performed to evaluate the relationship between off-centering, mean CT numbers and image noise. In addition, the same analysis was used to evaluate the influence of patient age, gender, body weight, BMI and maximal AP diameter of abdomen on the variability of mean CT numbers, SD and CTDIvol with off-centering. A P value less than 0.05 was considered to indicate a statistically significant difference.
Only 19% of patients (75/395 patients; male:female, 41:34) were centered correctly in the gantry isocenter. Most patients (81%, 320/395 patients; male:female, 154:166; mean age, 57 years) were off-centered with respect to the gantry isocenter. In terms of magnitude of off-centering, most patients were off-centered by 11-20 mm (39%, 125/320 patients) followed by 21-30 mm off-centering (26%, 85/320 patients) and greater than 31 mm off-centering (17%, 63/320 patients) (Table 1).
| Distance (#patients) | Direction (#patients) | BMI (kg) | Weight (mGy) | AP diameter (cm) | CTDIvol | aHU | pHU | LivHU | aSD | pSD | LivSD |
| 0-5 mm (n = 75) | Ideal centering | 27 (18-59) | 77 (31-181) | 28 (17-52) | 13.4 (5.2-48.3) | -97.5 ± 27.2 (-117~-45) | -92.8 ± 14.9 (-121~-34) | 117.0 ± 43.4 (63~153) | 9.9 ± 4.9 (5~45) | 11.8 ± 4.3 (4~33) | 17.0 ± 3.7 (9~15) |
| 6-10 mm (n = 47) | A (n = 20) | 28 (20-38) | 76 (54-107) | 27 (17-33) | 14.1 (9.0-33.0) | -98.2 ± 9.3 (-115~-78) | -90.9 ± 9.5 (-106~ -71) | 114.0 ± 20.0 (55~153) | 11.0 ± 2.6 (6~18) | 12.3 ± 3.0 (7~16) | 17.8 ± 3.4 (10~30) |
| B (n = 27) | 28 (21-40) | 79 (54-127) | 29 (20-53) | 13 (7.2-23.4) | -95.1 ± 13.1 (-115~-60) | -88.7 ± 19.3 (-109~-59) | 117.6 ± 26.9 (80~167) | 9.7 ± 2.3 (6~15) | 13.4 ± 4.01 (8~23) | 17.4 ± 5.2 (13~23) | |
| 11-20 mm (n = 125) | A (n = 47) | 30 (19-51) | 88 (54-130) | 31 (23-40) | 15.4 (9.2-42.2) | -96.9 ± 13.4 (-116~-45) | -93.3 ± 14.0 (-114~-44) | 109.9 ± 22.5 (63~158) | 11.0 ± 3.6 (5~22) | 12.6 ± 3.7 (7~23) | 18.1 ± 4.9 (11~31) |
| B (n = 78) | 27 (17-49) | 74 (35-136) | 28 (15-44) | 13.2 (5.8-34.5) | -97.1 ± 13.1 (-115~-53) | -92.9 ± 11.8 (-124~63) | 119.3 ± 25.2 (31~175) | 9.5 ± 2.4 (6~18) | 11.9 ± 3.2 (8~21) | 17.9 ± 4.3 (11~29) | |
| 21-30 mm (n = 85) | A (n = 22) | 29 (20-37) | 89 (46-129) | 32 (19-53) | 13.9 (6.2-26.7) | -96.5 ± 10.9 (-112~-74) | -89.0 ± 12.8 (-118~-56) | 107.4 ± 26.31 (40~142) | 12.4 ± 3.31 (7~20) | 13.6 ± 3.91 (9~24) | 18.7 ± 3.81 (6~20) |
| B (n = 63) | 26 (15-35) | 73 (40-109) | 27 (17-38) | 12.7 (5.9-23.5) | -94.6 ± 13.7 (-113~-44) | -85.3 ± 13.01 (-110~-43) | 122.3 ± 25.1 (55~177) | 10.4 ± 2.8 (6~23) | 13.3 ± 3.71 (6~22) | 17.9 ± 4.9 (11~34) | |
| ³31 mm (n = 63) | A (n = 10) | 36 (22-52) | 96 (65-141) | 34 (28-46) | 14.2 (10.1-21.1) | -94.3 ± 7.4 (-103~-80) | -89.1 ± 16.6 (-100~-77) | 116.6 ± 24.8 (81~153) | 16.4 ± 7.01 (9~29) | 14.0 ± 5.0 (8~24) | 26.7 ± 4.01 (21~38) |
| B (n = 53) | 26 (19-38) | 74 (49-118) | 27 (19-36) | 14.1 (6.1-42.6) | -94.1 ± 13.7 (-129~-68) | -87.1 ± 13.5a (-113~-61) | 125.0 ± 24.8a (63~167) | 9.4 ± 2.5 (6~18) | 13.5 ± 4.7a (8~30) | 17.2 ± 4.0 (11~30) |
Amongst the off-centered patients, 99 patients were centered superior to the gantry isocenter (off-center S, 31%, 99/320 patients; male:female, 53:46; mean age, 58 years) and 221 patients were centered inferior to the gantry isocenter (off-center I, 69%, 221/320 patients; male:female, 101:120; mean age, 57 years). Interestingly, most patients with greater than 31 mm off-centering were positioned inferior to the gantry isocenter (84%, 53/63 patients; male: female, 21: 32) (Table 1).
There was no significant difference between patient age in the centered and off-centered groups or in the different off-centering groups (P = 0.15). Although we had almost equitable distribution of male and female patients in our study, more men (n = 40/75 patients, 54%) were centered adequately in the gantry isocenter than women (n = 35/75 patients, 46%).
There was no significant difference between patient weight, AP diameter and BMI of centered (weight = 78.6 ± 27.6 kg, AP diameter, 28.2 ± 5.5 cm, BMI 26.7 ± 6.3 kg/m2) and off-centered (weight = 78.0 ± 19.0 kg, AP diameter, 28.6 ± 5.5 cm, BMI 27.6 ± 6.0 kg/m2) patients (P = 0.41, 0.29 and 0.16, respectively). However, patients off-centered above the gantry isocenter (weight = 89.4 ± 21.3 kg, AP diameter, 32.1 ± 5.8 cm, BMI 30.7 ± 7.1 kg/m2) were significantly larger than patients centered below the gantry isocenter (weight = 73.1 ± 15.8 kg, AP diameter, 27.0 ± 4.5 cm, BMI 26.0 ± 4.9 kg/m2) when the off-centering distance exceeded 10 mm (P < 0.0001). The largest differences in BMI, abdominal AP diameter and weight between off-centering superior and inferior were seen with greater than 30 mm off-centering (P < 0.0001) (Table 1). For subjects with less than 10 mm off-centering, there was no difference between body weight, BMI or AP diameter in the superior (weight = 79.3 ± 15.4 kg, AP diameter, 28.4 ± 4.3 cm, BMI 28.9 ± 6.0 kg/m2) and inferior off-centering directions (weight = 81.1 ± 22.6 kg, AP diameter, 29.8 ± 7.2 cm, BMI 28.8 ± 6.8 kg/m2) (P = 0.36, 0.19 and 0.48, respectively).
The effect of off-centering on CTDIvol is illustrated in Table 1. There was no significant difference between CTDIvol in patients with and without appropriate centering (P = 0.8).
The relationship between distance along the direction of off-center, mean CT numbers and objective image noise is summarized in Table 2. Regardless of the direction of off-centering, the mean CT numbers measured in the abdominal wall were significantly higher in off-centered patients compared to those centered correctly in the gantry isocenter (P = 0.034-0.0009). When the direction of off-centering was taken into account, only the mean CT numbers in the posterior abdominal wall increased significantly for patients centered below the gantry isocenter (P = 0.03). This change in mean CT numbers was less than 10% in absolute numbers (Table 2). When the magnitude of off-centering was taken into account, there was no significant change in mean CT numbers with up to 20 mm off-centering from the gantry isocenter (P = 0.1-0.47).
| Direction | aHU | pHU | LivHU | aSD | pSD | LivSD |
| Ideal centering | -97.5 ± 15.9 | -92.8 ± 15.1 | 117.0 ± 21.5 | 9.9 ± 4.9 | 11.8 ± 4.3 | 17.0 ± 3.7 |
| A | -96.9 ± 11.5 (0.4) | -91.4 ± 12.5 (0.25) | 111.1 ± 24.3 (0.05) | 11.8 ± 4.1 (0.004)a | 12.8 ± 3.8 (0.045)a | 18.8 ± 5.3 (0.003)a |
| B | -95.5 ± 14.4 (0.16) | -89.1 ± 14.5 (0.03)a | 121.0 ± 24.5 (0.1) | 9.8 ± 2.6 (0.33) | 12.8 ± 3.9 (0.03)a | 17.6 ± 4.3 (0.09) |
When data were normalized for patients’ age, gender, weight, BMI and AP diameters, mean CT numbers in all three regions between superior and inferior off-centering varied significantly for patients with different body weights (P < 0.001).
Image noise increased significantly in the posterior abdominal wall and liver parenchyma with an increase in off-centering distance. When the direction of off-centering was taken into account, noise in the anterior abdominal wall (P = 0.004) and liver (P = 0.003) increased significantly only with superior off-centering, whereas noise in the posterior abdominal wall increased significantly with both directions of off-centering (P = 0.03-0.045). There was a significant difference in image noise in the abdominal wall and liver between superior and inferior off-centering after normalizing BMI, body weight and maximal AP diameter of abdomen (P < 0.0001). Although there was a difference in objective image noise between superior and inferior off-centering, subjective image quality was not compromised for all 397 abdominal CT examinations, as reviewed from the radiology reports.
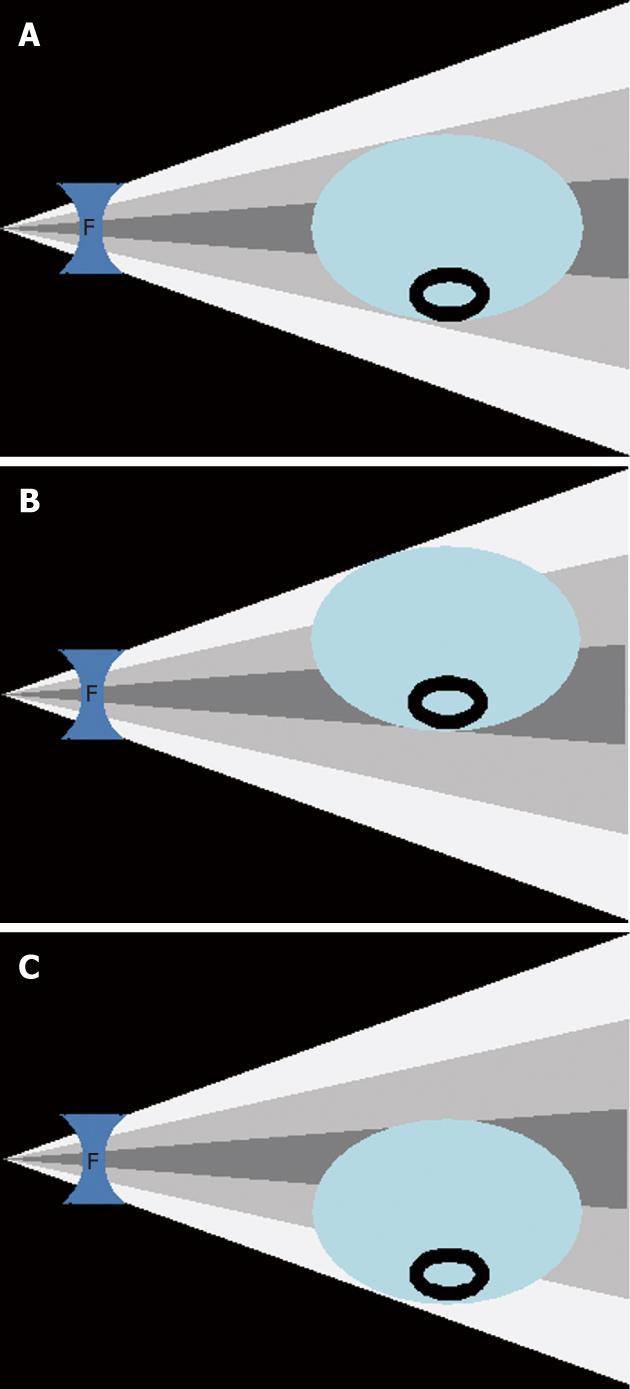
The role of appropriate patient centering has been emphasized for CT scanning, in particular when using AEC techniques and bow-tie filters to reduce radiation dose[8,9]. Optimal patient centering implies matching the patient’s mean center of mass with the center of the bow-tie filter which coincides with the center of the gantry in the CT scanner for optimal use of bow-tie filters. When a patient is not centered optimally, inappropriate compensation of the X-ray beam by bow-tie filters allows more X-ray to the surface of the thinner peripheral portion of the body while the X-ray beam incident upon the thicker central portion is reduced.
Li et al[7] reported that the peripheral and surface radiation dose increases by 12% and 18%, respectively, in images of an elliptical water phantom centered 30 mm below the isocenter, and by 41% and 49% in the same phantom centered 60 mm below the isocenter. These authors reported an overall increase of 6% and 22% in overall image noise at 3 and 6 cm phantom off-centering from the gantry isocenter. Conversely, Matsubara et al[10] reported a much smaller increase in overall image noise (15%) with 5 cm off-centering of a circular water phantom.
Our study highlights the variation in image noise for different anatomic locations in the abdomen. We noted a maximal increase in image noise of 16.5% in the posterior abdominal wall and 10% in the liver with patient off-centering of greater than 3 cm. In contrast, the increase in image noise with the same magnitude of off-centering was only 4% in the anterior abdominal wall. These discrepancies in change of image noise may be explained on the basis of differences in the regional X-ray beam attenuation in anterior and posterior abdominal wall and liver. Compared to the low attenuation from soft tissue of the anterior abdominal wall, the posterior abdominal wall has higher attenuation due to the vertebral column and therefore also has a greater increase in image noise with off-centering compared to the anterior abdominal wall. Since liver has higher attenuation than the anterior abdominal wall but lower than that of the posterior abdominal wall, with off-centering there is an intermediate change in image noise in the liver.
Our study also highlights the influence of directionality of vertical off-centering on image noise. When patients are centered above the gantry isocenter, the center of bow-tie filter corresponds to the posterior abdominal wall and the anterior abdominal wall receives more attenuated X-ray beam (Figure 2). This is likely the reason for a greater increase in image noise in the anterior abdominal wall than in the posterior abdominal wall with superior off-centering. Conversely, when patients are off-centered below the gantry isocenter, there is a greater increase in the posterior abdominal wall noise as it lies in the path of the more attenuated X-ray beam traversing through the peripheral thicker portion of the bow-tie filter.
This selective change in image noise with directionality of off-centering can also be explained on the basis of differences in CTDIvol with off-centering of patients. We noted a slightly higher CTDIvol with off-centering in the superior direction than in the inferior direction, and that may be due to the fact that patients centered above the gantry isocenter were substantially larger than patients centered below the gantry isocenter. It must be emphasized that with use of automatic exposure control, the CTDI vol changes with the size of the patient.
We also found that with off-centering there is some change in the CT numbers in different geometric locations of the images although this change is much less compared to the change in image noise (1%-5% relative to ideal patient centering). This modest change in CT numbers with off-centering may also be a result of differential beam attenuation by bow-tie filters in off-centered patients as relevant to the image noise.
Interestingly, we also noted a substantial influence of patient size on magnitude and direction of off-centering. Patients centered above the isocenter tended to be substantially larger than those centered below the isocenter. This may be explained on the basis of incorrect or underestimation of centering of patients with large body habitus. Unfortunately, we found that despite rising awareness about the risks associated with CT scanning and recent publications emphasizing an increase in radiation dose with patient off-centering, there was a very modest difference between the proportion of off-centered patients in our study (81%) compared to that reported in two prior studies (95%-95.5%) conducted at different institutions[7,11]. In our institution, technologists are reminded about the importance of patient centering from time to time, although there is no fixed routine or interval for completing such notification. The fact that off-centering continues to occur in the vast majority of our patients perhaps suggests that manual off-centering by the CT technologists is either not properly performed or cannot be performed with a great deal of accuracy. Regardless of the reasons for off-centering, there is an urgent need for an automatic assisted patient centering technique on CT equipments which are otherwise being armed with sophisticated dose reduction techniques such as automatic exposure control and bow-tie filters. In this direction, it is important to note that some vendors have introduced a feature to allow CT users to change table position for better patient centering directly from the CT scanner (Siemens Definition Flash, Siemens Medical Solutions, Forchheim, Germany) user interface after checking the localizer radiograph. This ability helps technologists to “fine tune” or “correct” patient centering without the need to go into the CT gantry suite.
There are clinical implications resulting from our study. There needs to be greater education and training of the CT technologists for patient centering. The method of centering patients with large body habitus needs specific attention. Differential distribution of image noise is influenced by both magnitude and direction of off-centering and hence off-centering should be avoided in order to maintain a uniform image quality. Radiologists should bear in mind that there is a slight but statistically insignificant change in mean CT numbers in the liver with off-centering.
There are limitations in our study. Although we included a large number of patients in our study, we did not perform a power analysis to determine the actual sample size required to test our hypothesis. In particular, there were fewer patients in the off-centering groups with more than 30 mm off-centering distance from the gantry isocenter. Another limitation was that the size and location of the ROIs being measured were not homogeneous for each patient. The size of ROIs in abdominal subcutaneous fat ranged from 10 to 30 mm2 according to the amount of subcutaneous fat. Likewise, the liver ROIs ranged from 30 to 50 mm2 to include just the liver parenchyma and avoid inclusion of large blood vessels within the ROI. Although we did not perform a formal detailed subjective image quality assessment, we carried out a retrospective analysis of the radiology reports to check image quality of these CT examinations. Study reports are stored in the hospital database along with the images and comments on suboptimal image quality affecting diagnostic confidence. We found that none of the examinations showed suboptimal image quality. Another limitation of our study is that we did not compare the effect of different off-centering distances and directions in the same patient as it was not feasible and practical to scan patients several times with different off-centering. It is possible, although unproven from our study, that greater changes in CT numbers and image noise may have come to light on an individual patient basis. We also did not assess the effect of horizontal off-centering of the patients on image noise and mean CT numbers.
In conclusion, inappropriate patient centering in the gantry isocenter adversely affects the mean CT numbers and image noise along the distance of off-center. Therefore, attention to appropriate patient centering is important for maintaining image quality and optimizing radiation dose during MDCT examination, particularly in large patients.
Computed tomography (CT) radiation dose related risks are one of the major concerns amongst the medical community, media and general public. There are several attempts in the past to optimize radiation dose associated with CT by following the principle of “as low as reasonably achievable”. X-ray beam shaping filters are designed to expose the peripheral thinner portions of the body with lower radiation dose as compared to thicker central portion. This assumption only works when the authors have the patient perfectly centered in the X-ray beam. Any offcentering of patient affects the selected tube current and finally radiation dose associated with CT.
Prior studies have shown that patient offcentering from the CT scanner iso-center does affect the associated radiation dose with tube current modulation techniques. However, the relationship between mean CT numbers or the Hounsfield values and the image noise has not been assessed with respect to patient size.
The study highlights the influence of directionality of vertical off-centering on image noise. When patients are centered above the gantry isocenter, the center of bow-tie filter corresponds to the posterior abdominal wall and the anterior abdominal wall receives more attenuated X-ray beam. The authors also found that with off-centering there is some change in the CT numbers in different geometric locations of the images although this change is much less compared to the change in image noise (1%-5% relative to ideal patient centering). This modest change in CT numbers with off-centering may also be a result of differential beam attenuation by bow-tie filters in off-centered patients as relevant to the image noise.
Clinical implications of this study are the need for greater education and training of the CT technologists for patient centering. The method of centering patients with large body habitus needs specific attention. Differential distribution of image noise is influenced by both magnitude and direction of off-centering and hence off-centering should be avoided in order to maintain a uniform image quality. Radiologists should bear in mind that there is a slight but statistically insignificant change in mean CT numbers in the liver with off-centering.
Bow-tie or beam shaping filters: These filters configure the X-ray beam to the cross-sectional geometry of the body region being scanned, so that the thinner peripheral portion of the body receives a lower radiation dose compared to the thicker central portion of the cross section. Patient Off-centering: Any deviation of patients center from the CT scanner gantry iso-center, which can be either vertically or horizontally.
This is a good descriptive study in which authors analyze the affect of patient offcentering on CT image noise and Hounsfield Units numbers. The results are interesting and show an increase in 16% image noise in posterior abdominal wall and suggest a need for education and training of CT technologist in more accurate patient centering.
Peer reviewers: Tilo Niemann, MD, Department of Radiology, University Hospital Basel, Petersgraben 4, CH-4031 Basel, Switzerland; Hadi Rokni Yazdi, MD, Associate Professor, Department of Radiology, Central Radiology, Imam Khomeini Hospital, Tehran University of Medical Sciences, Keshavarz Blvd, Tehran 1419733141, Iran; Zhonghua Sun, PhD, Discipline of Medical Imaging, Department of Imaging and Applied Physics, Curtin University of Technology, GPO Box U 1987, Perth, Western Australia 6845, Australia
S- Editor Cheng JX L- Editor Webster JR E- Editor Xiong L
| 1. | Donnelly LF, Emery KH, Brody AS, Laor T, Gylys-Morin VM, Anton CG, Thomas SR, Frush DP. Minimizing radiation dose for pediatric body applications of single-detector helical CT: strategies at a large Children's Hospital. AJR Am J Roentgenol. 2001;176:303-306. [PubMed] |
| 2. | Maher MM, Kalra MK, Toth TL, Wittram C, Saini S, Shepard J. Application of rational practice and technical advances for optimizing radiation dose for chest CT. J Thorac Imaging. 2004;19:16-23. [PubMed] |
| 3. | Kalra MK, Maher MM, Toth TL, Hamberg LM, Blake MA, Shepard JA, Saini S. Strategies for CT radiation dose optimization. Radiology. 2004;230:619-628. [PubMed] |
| 4. | Sodickson A, Baeyens PF, Andriole KP, Prevedello LM, Nawfel RD, Hanson R, Khorasani R. Recurrent CT, cumulative radiation exposure, and associated radiation-induced cancer risks from CT of adults. Radiology. 2009;251:175-184. [PubMed] |
| 5. | Griffey RT, Sodickson A. Cumulative radiation exposure and cancer risk estimates in emergency department patients undergoing repeat or multiple CT. AJR Am J Roentgenol. 2009;192:887-892. [PubMed] |
| 6. | Feng ST, Law MW, Huang B, Ng S, Li ZP, Meng QF, Khong PL. Radiation dose and cancer risk from pediatric CT examinations on 64-slice CT: a phantom study. Eur J Radiol. 2010;76:e19-e23. [PubMed] |
| 7. | Li J, Udayasankar UK, Toth TL, Seamans J, Small WC, Kalra MK. Automatic patient centering for MDCT: effect on radiation dose. AJR Am J Roentgenol. 2007;188:547-552. [PubMed] |
| 8. | Avilés Lucas P, Castellano IA, Dance DR, Vañó Carruana E. Analysis of surface dose variation in CT procedures. Br J Radiol. 2001;74:1128-1136. [PubMed] |
| 9. | Kalra MK, Maher MM, Kamath RS, Horiuchi T, Toth TL, Halpern EF, Saini S. Sixteen-detector row CT of abdomen and pelvis: study for optimization of Z-axis modulation technique performed in 153 patients. Radiology. 2004;233:241-249. [PubMed] |
| 10. | Matsubara K, Koshida K, Ichikawa K, Suzuki M, Takata T, Yamamoto T, Matsui O. Misoperation of CT automatic tube current modulation systems with inappropriate patient centering: phantom studies. AJR Am J Roentgenol. 2009;192:862-865. [PubMed] |
| 11. | Li J, Udayasankar UK, Toth TL, Small WC, Kalra MK. Application of automatic vertical positioning software to reduce radiation exposure in multidetector row computed tomography of the chest. Invest Radiol. 2008;43:447-452. [PubMed] |