Revised: November 18, 2011
Accepted: November 25, 2011
Published online: February 28, 2012
Lipomatous uterine tumors are uncommon benign neoplasms, with incidence ranging from 0.03% to 0.2%. They can generally be subdivided into two types: pure or mixed lipomas. A third group of malignant neoplasm has been proposed, which is liposarcoma; however, this is very rare. In this article, we report three patients having lipomatous uterine tumors, including one uterine lipoma and two uterine lipoleiomyomas. All our patients are postmenopausal women, which is the typical presenting age group. They did not have any symptoms and the tumors were only found incidentally on imaging. However, in some patients, symptoms may uncommonly occur. If symptoms occur, these are similar to those of leiomyoma. We illustrate the imaging features of the tumors in our patients with ultrasound, computed tomography (CT) scan and magnetic resonance imaging (MRI). The tumor typically appears as a well-defined homogenously hyperechoic lesion on ultrasound. It shows fat density on CT scan and signal intensity of fat on MRI. MRI is the modality of choice because of its multiplanar capability and its ability to demonstrate fat component of the lesion, as illustrated in our cases. We also discuss the importance of differentiating lipomatous uterine tumors from other lesions, especially ovarian teratoma which requires surgical intervention. Despite the rarity and the common asymptomatic nature of the tumors, we believe that this series of three cases demonstrates a review of a rare tumor which provides important knowledge for patient management.
- Citation: Chu CY, Tang YK, Chan TSA, Wan YH, Fung KH. Diagnostic challenge of lipomatous uterine tumors in three patients. World J Radiol 2012; 4(2): 58-62
- URL: https://www.wjgnet.com/1949-8470/full/v4/i2/58.htm
- DOI: https://dx.doi.org/10.4329/wjr.v4.i2.58
Lipomatous uterine tumors are rare benign uterine tumors, with only approximately 180 cases reported in the literature[1]. Although it is rare, correct diagnosis of lipomatous uterine tumor is important. Differentiation from other fat-containing tumors in the female pelvis, such as ovarian teratoma, may save a patient from unnecessary surgery[2,3]. We would like to present a series of three cases of these rare uterine tumors and provide a review of the imaging characteristics.
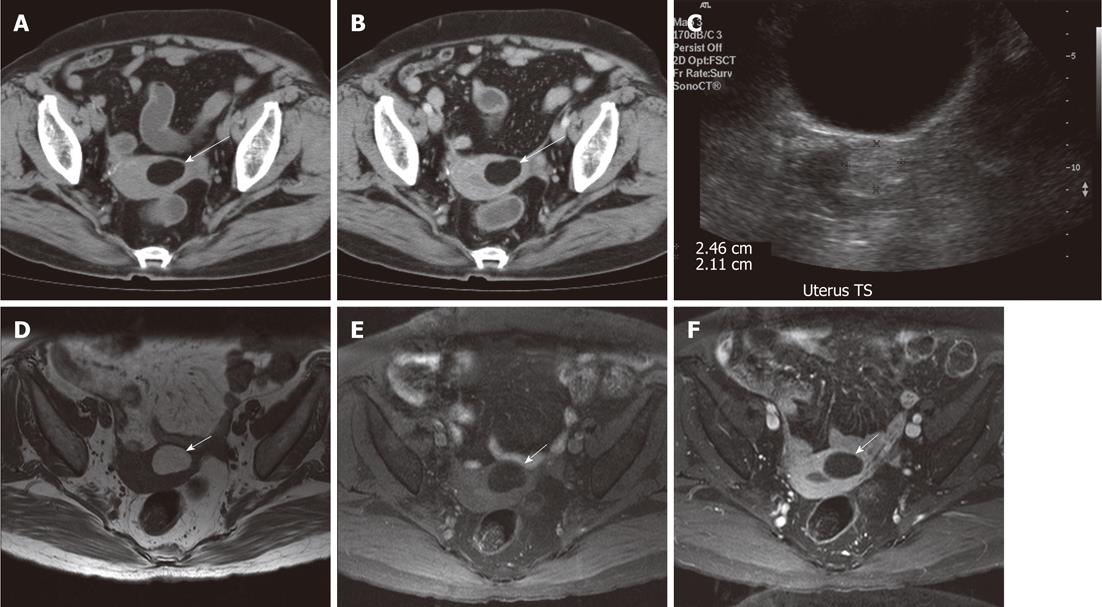
A 79-year-old woman, with past medical history of diabetes mellitus, hypertension, presbyacusis, cholecystectomy and right Warthin’s tumor which was being conservatively treated, complained of “on and off” abdominal pain. Mild splenomegaly was detected on ultrasound of the abdomen. A computed tomography scan was then performed in view of the splenomegaly. On computed tomography (CT) scan, hepatosplenomegaly, colonic polyp and a pancreatic tail tumor were found. Moreover, there was incidentally a well-defined mass of fat density (-82 HU units) arising from the wall of the uterine fundus (Figure 1A and B). The mass lesion showed no significant contrast enhancement. Distortion of the uterine cavity by the mass lesion was also noted. Intrauterine lipoma was the provisional diagnosis based on the CT findings.
Transabdominal sonography of the pelvis was performed and showed a well-defined echogenic lesion in the uterine fundus (Figure 1C). A better characterization of the tumor was noted on magnetic resonance imaging (MRI) (Figure 1D-F). The mass was found to be arising from the anterior wall of uterus. It appeared homogeneously hyperintense on T1- and T2-weighted images, with signal intensity similar to that of peritoneal fat. On fat-saturated images, complete suppression of the hyperintense signal of the lesion was noted. No contrast enhancing component was seen. Compression on the endometrial cavity by the mass lesion was also noted. Based on the imaging features, the final diagnosis was uterine lipoma.
The patient was followed up by a gynecologist for the uterine lipoma. Since the patient was asymptomatic, no surgery or biopsy of the mass lesion was performed. The patient is now being followed up by surgeons in view of CT scan findings of a pancreatic tail tumor and hepatosplenomegaly. The patient is now under conservative management for all her conditions. She has not had any symptoms during her 2 years of follow-up.
A 61-year-old female patient, with past history of cholecystectomy, complained of intermittent abdominal pain for 2 years. Upper endoscopy and colonoscopy both showed no abnormality. A CT scan of the abdomen and pelvis was performed in view of chronic abdominal pain.
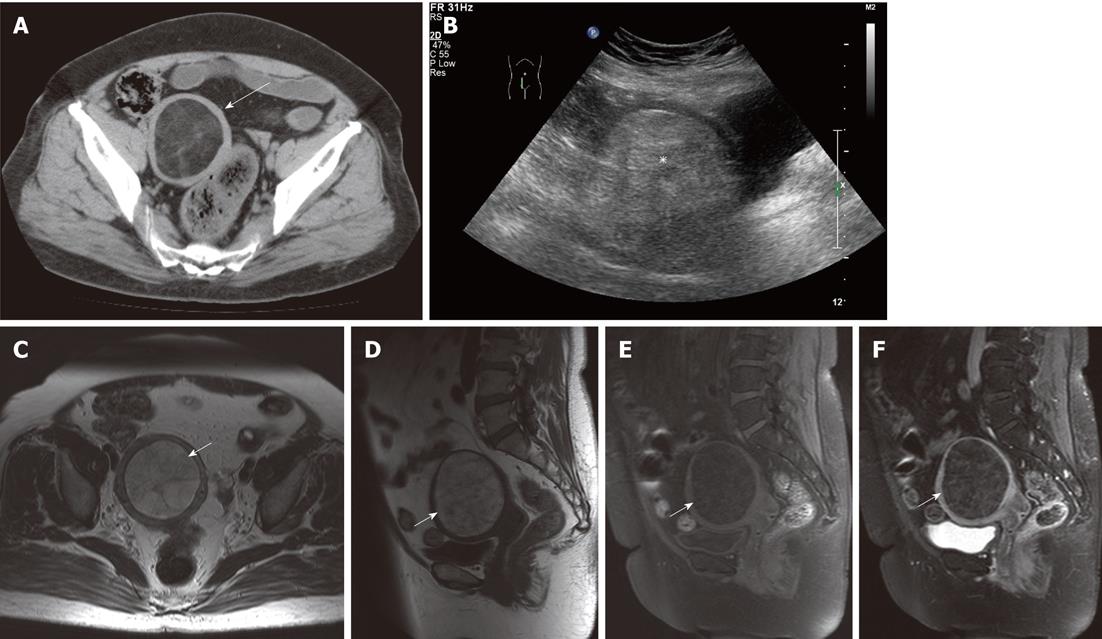
On the CT scan, a well-defined lesion of fat density with intralesional septa was incidentally found in the body of the uterus (Figure 2A). No intralesional calcification was seen. No other abnormality was noted in the rest of the abdomen and pelvis. A transabdominal ultrasound revealed a homogeneously hyperechoic lesion in the uterus. (Figure 2B).
MRI was subsequently performed to further characterize the lesion (Figure 2C-F). A well-defined T1 and T2 hyperintense lesion was seen in the uterine fundus. Intralesional septa were seen, which showed contrast enhancement. No solid component was seen in the lesion. The final diagnosis was uterine lipoleiomyoma.
The patient prefers conservative management and is now under follow up by a gynecologist. She remains asymptomatic 6 mo after the diagnosis.
A 72-year-old female patient, with history of depression, was referred by her general practitioner to a gynecologist because of intermittent abdominal pain. She did not have any other symptoms. An ultrasound scan performed in China showed an unknown tumor in the pelvis. Therefore, a transvaginal ultrasound scan was performed and this showed a highly hyperechoic lesion over the left side of the pelvis. However, the exact nature could not be determined by the ultrasound at that time.
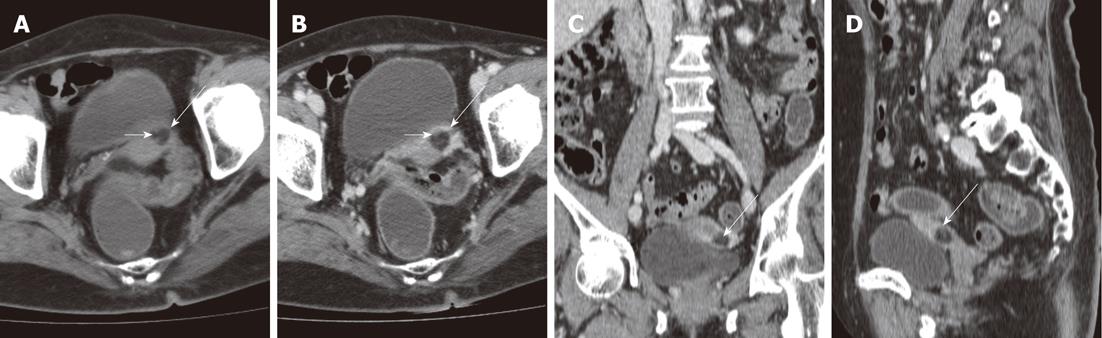
A subsequent contrast CT scan of the abdomen and pelvis was performed. It revealed a roundish lesion of fat density over the left side of the uterine body, with no intralesional calcification (Figure 3). A small amount of soft tissue density was seen inside the lesion (Figure 3). No adnexal mass lesion was detected. The lesion was decided to most likely represent a uterine lipoleiomyoma.
Transvaginal sonography was repeated during follow up and showed no growth of the tumor. The patient is now asymptomatic and, as a result, no resection of the tumor has been needed. She now has been followed up by a gynecologist for 1 year, with no complaints of symptoms. She is now under conservative management for the lipomatous uterine tumor.
Lipomatous uterine tumors are uncommon benign neoplasms, with incidence ranging from 0.03% to 0.2%[1,3-5]. They can generally be subdivided into two types: pure or mixed lipomas[6,7]. The latter consist of lipoleiomyoma, angiomyolipoma, fibrolipoma[1]. A third group of malignant neoplasm has been proposed, which is liposarcoma; however, this is very rare[1]. Mixed lipoma contains variable amounts of fat, fibrous tissue and smooth muscle while pure lipoma is composed of encapsulated adipose tissue with thin septa of fibrous tissue only[6]. Most of the reported cases are of mixed type and lipoleiomyoma is the most common[1,2]. Pure lipoma of the uterus is extremely rare, with only a handful of cases reported[7].
Uterine lipoleiomyoma is typically seen in postmenopausal women, with the majority found in patients between 50-70 years of age[1,8,9]. Most of the patients are asymptomatic. On the other hand, the presentation is similar to that of leiomyoma if there is any symptom[3-5]. For example, the patient may complain of a palpable mass, urinary frequency, constipation, pelvic discomfort, uterine bleeding or hypermenorrhea. These are related to the size and location of the lesion[3-5,9]. Malignant degeneration in uterine lipoleiomyoma is extremely rare, although it has been reported in the literature[3,9].
The most common location is in the uterine corpus. The tumors are usually intramural[3,4,6,7,9]; however, they can be found anywhere in the uterus or cervix and can be subserosal or submucosal[3,4]. Average size of the lesion is usually between 5 and 10 cm[1,2,8,9]. Concomitant uterine leiomyoma is commonly found, although this is not present in all patients, including ours[1-3,6,7,9].
The pathogenesis of the lesion remains unknown[1,3-5,8,9]. Several theories have been proposed, including misplaced embryonic fat cells, perivascular extension of peritoneal or retroperitoneal fat, lipocytic differentiation of primitive connective or mesenchymal tissue, and metaplasia of smooth muscle cells or connective tissue into adipose cells[3,4]. The last theory regarding metaplasia is so far the most widely accepted underlying mechanism of uterine lipoleiomyoma[3,4].
Ultrasound: On ultrasound, the lesion is echogenic and is usually partially encased by a hypoechoic rim[2,3,6,7,9]. The hypoechic rim is thought to represent a layer of myometrium surrounding the fatty component[6,7,9]. However, ultrasound findings are not specific to the diagnosis[6,7]. The sonographics findings of the tumors in our first and second patients were compatible with these characteristics, being homogenously echogenic although the hypoechoic rim was not seen.
CT: CT findings are more specific since CT scan can clearly demonstrate a fat component of the lesion, which appears low in attenuation with Hounsfield units between -40 and -100[5,6,9]. A CT scan may also help differentiate uterine lipoleiomyoma from pure uterine lipoma. On CT scan, uterine lipoleiomyoma is well-circumscribed showing heterogeneous fat density while uterine lipoma demonstrates homogeneous density[8]. Based on this feature, uterine lipoma is the most likely diagnosis in our first patient. Enhancing septa were found in the CT images of our second patient while soft tissue density components were noted in our third patient. Therefore, uterine lipoleiomyomas were the more likely diagnoses in our second and third patients. Although CT is more specific than ultrasound, it has it own disadvantages, including inability to illustrate detailed uterine anatomy and confusion between an adnexal mass and a lesion arising from the uterus, particularly exophytic or pedunculated lesions[5].
MRI: MRI, with its multiplanar capabilities, is the most useful modality in demonstrating the organ of origin[3,5]. MRI is also the best tool for diagnosing a lipomatous tumor[6]. On MRI, the fatty component is high in signal intensity on both T1- and T2-weighted images[4]. Chemical shift artifacts along the frequency-encoding axis may be seen, which further verify the fatty component[9]. The fatty component of the lesion can also be confirmed by fat suppression sequence, which demonstrates decrease in signal intensity in fat components of the lesion[6,7].
MRI enables better tissue characterization than CT[6,7]. Septa inside the mass can be seen on T1-weighted images[6,7]. MRI sometimes shows a peripheral low signal intensity rim which corresponds to a thin fibrous pseudocapsule. This feature is not demonstrated on CT scan[6,7].
MRI can also help differentiate pure lipoma from uterine lipoleiomyoma[5,7]. On MRI, pure lipoma shows absence of nonadipose components, the presence of a homogeneous mass with a large amount of fat and signal decrease in the whole mass on fat-saturated images. On the other hand, lipoleiomyoma demonstrates heterogeneous signal intensity with fat and non-fat soft tissue content, and decrease in signal only in part of the lesion on fat-saturated images[7]. In the MR images of our first patient, only signal intensity of fat was seen, suggestive of pure lipoma in the uterus. Enhancing septa seen in our second patient favor uterine lipoleiomyoma.
The various imaging features of the tumor in different modalities are important to guide the final diagnosis. Knowledge of these is also important to radiologists since most of the tumors are incidental findings on imaging. Although ultrasound and CT scan findings may be non-specific, any presence of the previously mentioned imaging features should raise the suspicion of a lipomatous uterine tumor. MRI is the modality of choice for the final diagnosis. If there is any uncertainty despite the use of MRI, combination of clinical history, physical examination and all imaging features will probably provide the accurate diagnosis in the majority of cases.
There are a number of differential diagnoses for a fat-containing tumor in the female pelvis, such as benign cystic ovarian teratoma, malignant degeneration of a benign cystic ovarian teratoma, non-teratomatous lipomatous ovarian tumor, benign pelvic lipoma, liposarcoma, extra-adrenal myelolipoma in pelvis, lipoblastic lymphadenopathy and retroperitoneal cystic hamartoma. Among the long list of differentials, the most common one is benign cystic ovarian teratoma, which usually requires surgical excision[2]. On the other hand, asymptomatic uterine lipoleiomyoma can be managed conservatively because of its benign nature[2]. Therefore, correct diagnosis of uterine lipoma/lipoleiomyoma and differentiation from other fat-containing pelvic tumors are important in the patient’s management and can prevent unnecessary surgery[2,3].
In conclusion, we report a case series of 3 rare lipomatous uterine tumors. The ultrasound, CT and MRI features of the tumors have been illustrated. MRI with its multiplanar capabilities, better tissue characterization and the ability to demonstrate fat component by fat-saturated sequences is the best modality for diagnosis. With better understanding of the imaging characteristics, we can make a correct pre-operative diagnosis, differentiate the lesion from other fat-containing tumors in the female pelvis and choose the optimal management for patients.
Peer reviewer: Masami Yamamoto, MD, Departamento de Ginecología y Obstetricia, Clínica Alemana de Santiago, Unidad de Medicina Materno Fetal, Facultad de Medicina CAS-UDD, Manquehue norte 1410, Cuarto Piso, Vitacura, Santiago, Chile
S- Editor Cheng JX L- Editor Logan S E- Editor Zheng XM
| 1. | Kitajima K, Kaji Y, Imanaka K, Sugihara R, Sugimura K. MRI findings of uterine lipoleiomyoma correlated with pathologic findings. AJR Am J Roentgenol. 2007;189:W100-W104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 2. | Dodd GD, Budzik RF. Lipomatous uterine tumors: diagnosis by ultrasound, CT, and MR. J Comput Assist Tomogr. 1990;14:629-632. [PubMed] |
| 3. | Chan HHL, Chau MT, Lam CHL, Cheung SCW. Uterine lipoleiomyoma: ultrasound and computed tomography findings. J HK Coll Radiol. 2003;6:30-32. |
| 4. | Loffroy R, Nezzal N, Mejean N, Sagot P, Krausé D. Lipoleiomyoma of the uterus: imaging features. Gynecol Obstet Invest. 2008;66:73-75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 5. | Senior EL, Taylor HL. Uterine leiomyolipoma - incidental finding on screening CT. Eur J Radiol Extra. 2006;59:63-65. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 6. | Coumbaras M, Validire P, Strauss C, Herry M, Dahan H, Palau R. Uterine lipoma: MRI features with pathologic correlation. Abdom Imaging. 2005;30:239-241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Erdem G, Celik O, Karakas HM, Alkan A, Hascalik S. Pure uterine lipoma. Magn Reson Imaging. 2007;25:1232-1236. |
| 8. | Maebayashi T, Imai K, Takekawa Y, Sasaki J, Otsuka H, Katsura Y, Mochizuki T. Radiologic features of uterine lipoleiomyoma. J Comput Assist Tomogr. 2003;27:162-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Lau LU, Thoeni RF. Case report. Uterine lipoma: advantage of MRI over ultrasound. Br J Radiol. 2005;78:72-74. [PubMed] |