Revised: September 7, 2011
Accepted: September 14, 2011
Published online: February 28, 2012
AIM: To compare the reported injuries on initial assessment of the chest X-ray (CXR) in thoracic trauma patients to a second read performed by a dedicated trauma radiologist.
METHODS: By retrospective analysis of a prospective database, 712 patients with an injury to the chest admitted to the University Medical Center Utrecht were studied. All patients with a CXR were included in the study. Every CXR was re-evaluated by a trauma radiologist, who was blinded for the initial results. The findings of the trauma radiologist regarding rib fractures, pneumothoraces, hemothoraces and lung contusions were compared with the initial reports from the trauma team, derived from the original patient files.
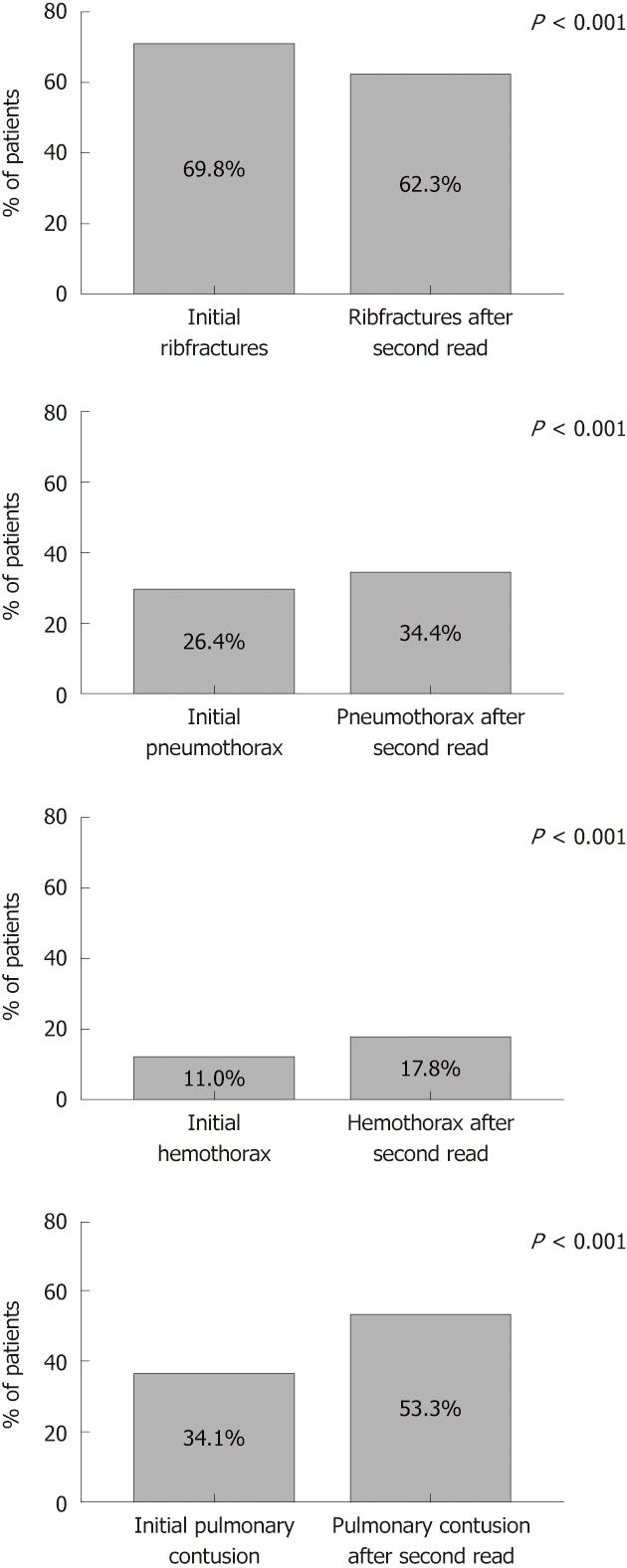
RESULTS: A total of 516 patients with both thorax trauma and an initial CXR were included in the study. After re-evaluation of the initial CXR significantly more lung contusions (53.3% vs 34.1%, P < 0.001), hemothoraces (17.8% vs 11.0%, P < 0.001) and pneumothoraces (34.4% vs 26.4%, P < 0.001) were detected. During initial assessment significantly more rib fractures were reported (69.8% vs 62.3%, P < 0.001).
CONCLUSION: During the initial assessment of a CXR from trauma patients in the emergency department, a significant number of treatment-dictating injuries are missed. More awareness for these specific injuries is needed.
- Citation: Aukema TS, Beenen LF, Hietbrink F, Leenen LP. Initial assessment of chest X-ray in thoracic trauma patients: Awareness of specific injuries. World J Radiol 2012; 4(2): 48-52
- URL: https://www.wjgnet.com/1949-8470/full/v4/i2/48.htm
- DOI: https://dx.doi.org/10.4329/wjr.v4.i2.48
Chest X-ray (CXR) is the main modality in screening for and diagnosing thoracic injuries in trauma patients. It is considered as a primary initial diagnostic test. This modality is part of the advanced trauma life support work up[1] and it is widely available in hospitals. The CXR is used to visualize AO classified rib fractures, lung contusions, pneumothorax, and hemothorax. Apart from these, subcutaneous and mediastinal emphysema, diaphragmatic and aortic injury, fractures of the axial skeleton and malposition of tubes and catheters can also be evaluated. The CXR is a quick modality with a high diagnostic yield which is crucial in the early work up of trauma patients. Radiation exposure for the patient is minimal[2].
In common practice, the CXR undertaken in the emergency department is assessed by the trauma team, frequently by residents on call. Although the trauma team may have adequate interpretive skills, they do not routinely have the luxury of prolonged interpretation times and have to work under difficult conditions. Occult pneumothoraces can be missed in up to 76% of all seriously injured patients when CXRs are interpreted by a trauma team[3]. Potentially, the diagnostic performance of CXR might increase if a dedicated trauma radiologist could detect specific injuries not seen by the trauma team, during a second read.
The aim of the present study was to evaluate the reported injuries on initial assessment of the CXR in thoracic trauma patients by comparing with a double read performed by a dedicated trauma radiologist for rib fractures, pneumothorax, hemothorax and lung contusion.
From the prospective trauma database of the University Medical Center Utrecht, all patients admitted to the Emergency Department of the University Medical Center Utrecht over a period of 5 years were evaluated. We retrospectively searched the database for thoracic trauma patients with a CXR.
The following pathologic entities were assessed on CXR: rib fractures, pneumothorax, hemothorax and lung contusion. The included patients were diagnosed with at least one of the assessed pathologic entities on the initial CXR.
The following factors were retrieved from the database: patients’ age, sex, total hospital stay, intensive care unit (ICU) stay, thorax-related complications and mortality. For every patient, the initial reported findings of the admission CXR by the trauma team were placed in a database. All CXR were retrospectively assessed by a trauma radiologist (LB) blinded for clinical outcome and original report.
Statistical analyses were performed by using SPSS 15 (Version 15, for Windows, SPSS Inc., Chicago, IL, USA). Statistical testing was achieved using the McNemar test for related samples. Statistical significance was defined as P value < 0.05.
Screening CXR was obtained in 516 patients. The study cohort had a median age of 43 years (range 1-92 years). The study population was predominately male: 375 males (73%) and 141 females. The median overall hospital length of stay was 23 d (range 1-257 d). Two hundred and seventy-one patients were admitted to the ICU; the median ICU stay was 8 d (range 1-198 d). Two hundred and thirty-three patients were ventilated; the median mechanical ventilation duration was 7 d (range 1-190 d). Demographic data are presented in Table 1.
| Number of patients | 516 |
| Mean age (yr) | 43 |
| Sex of patient n (%) | |
| Male | 375 (73) |
| Female | 141 (27) |
| Days of hospital stay (median) | 23 |
| Patients in ICU n (%) | 271 (53) |
| Median length of ICU stay (d) | 8 |
| Ventilated patients n (%) | 233 (45) |
| Median duration of ventilation (d) | 7 |
| Mortality n (%) | 52 (10) |
Initial assessment of the CXR showed rib fractures in 69.8% of the patients. After a second read by the trauma radiologist, rib fractures were diagnosed in 62.3% of the patients (Figure 1A, P < 0.001). Initially, 7.4% of the patients were diagnosed with bilateral rib fractures and the range of number of rib fractures was 1-16. After assessment by the trauma radiologist, 7.6% of the patients showed bilateral rib fractures and the range was 1-14 (P = 1.0).
Initial CXR assessment by the trauma team revealed a pneumothorax in 26.4% of the patients. The trauma radiologist diagnosed a pneumothorax in 34.4% of the patients (Figure 1B, P < 0.001). Bilateral pneumothorax was initially seen in 3.5% of the patients; after assessment by the trauma radiologist in 2.8% of the patients (P = 0.13).
Initial assessment of the CXR by the trauma team revealed hemothoraces in 11.0% of the thoracic trauma patients. After a second read by the dedicated trauma radiologist, hemothoraces were diagnosed in 17.8% of the patients (Figure 1C, P < 0.001). Initially, 1.0% of the patients were diagnosed with bilateral hemothoraces; after a second read by the dedicated trauma radiologist bilateral hemothoraces were seen in 0.8% of the patients (P = 1.0).
Initial assessment of the CXR showed a lung contusion in 34.1% of the patients. After evaluation by the dedicated trauma radiologist, a lung contusion was seen in 53.3% of the patients (Figure 1D, P < 0.001).
This study demonstrates that there is a discrepancy between the initial assessment of the CXR in thoracic trauma patients by the trauma team and a second read by a dedicated trauma radiologist. During initial evaluation significantly more patients with rib fractures are diagnosed on CXR and during the second read significantly more pneumothoraces, hemothoraces and pulmonary contusions are seen.
Our results suggest that a second read by a dedicated trauma radiologist increases the diagnostic performance of CXR for these thoracic injuries. The enhanced diagnostic performance subsequently improves treatment of thoracic trauma patients since the injuries can be treated more adequately or can be monitored closely.
The cause of the missing injuries on radiographs during initial assessment by the trauma team, mostly residents, can be diverse. Ball et al[3] suggested that missed injuries were likely based on the difficult conditions in which the trauma team functions. They do not have prolonged interpretation times, a perfectly lit environment and premium digital monitors, which most radiologists benefit from. Other studies have compared the performance of residents in the interpretation of radiographs with that of a radiologist and found their performance suboptimal[4,5]. A combination of both factors could account for the discrepancy between the initial results and those obtained on second read by a trauma radiologist.
In this study, 7.5% more rib fractures were diagnosed during the initial assessment by the trauma team than during the second read by the dedicated trauma radiologist. The clinical value of a single rib fracture can be questioned. Indeed, multiple rib fractures and rib fractures in older patients require adequate patient management[6-10]. However, the prognosis of a patient with a single rib fracture is good if treatment consists of appropriate pain management and pulmonary rehabilitation[11,12].
Missed pneumothoraces on CXR are a known cause of preventable death, for which relatively simple interventions may be life-saving[13]. This study demonstrates that 8% more pneumothoraces can be detected on CXR during a second look by a dedicated trauma radiologist. Although a minor pneumothorax may not be clinically important initially, it can become a dangerous entity when trauma patients require positive-pressure mechanical ventilation or when patients are exposed to decreased atmospheric pressure during air transport. In the case of unawareness of this initially non-life threatening condition, there is an increased risk of adverse outcome during rapid progression to a tension pneumothorax[14,15]. Currently, there is an ongoing debate on observing all the occult pneumothorax without chest tube drainage[16-18] vs the standard treatment of placing thoracic drainage in every ventilated patient[1,19]. Either way, patients with an occult pneumothorax require additional observation, thus identification of this type of injury is essential.
This study demonstrates that 6.8% more hemothoraces can be detected after initial CXR during a second look by a dedicated trauma radiologist. In contrast to the extensive literature on occult pneumothoraces, little is known about the incidence of, and associated management outcomes of, occult hemothorax in thoracic trauma patients. Several studies suggest that small, isolated, occult hemothoraces can be observed without initial placement of a chest tube in the stable patient[20,21]. In our institute every patient with a hemothorax is treated with a chest tube. In both treatment strategies, it is clinically relevant to detect hemothoraces on CXR.
Pulmonary contusion is an independent risk factor for the development of acute respiratory distress syndrome (ARDS)[22,23]. Although fatal outcome of ARDS has declined over the last decade, ARDS still is one of the most serious thorax trauma-related complications with a mortality rate up to 20%-43%[24,25]. This study demonstrates that 19.2% more patients are diagnosed with pulmonary contusion on the initial CXR after a second read by a dedicated trauma radiologist, which is 19% higher than the initial assessment. These additional findings place the patients in a high-risk group for subsequent respiratory failure. These findings also have important implications on resource utilization such as admission to a monitored or intensive care unit bed.
Some limitations of this study should be acknowledged. This study was performed retrospectively which makes the results subject to bias. In an attempt to limit ascertainment bias, a single examiner performed all chart reviews. In addition, the dedicated trauma radiologist was blinded for the initial results from the CXR during the second read. Another potential limitation is the lack of control for interobserver or intraobserver variability in interpretation of the CXR findings. Brar et al[26] demonstrated that the inter- and intraobserver variability to detect occult pneumothoraces is moderate. Szucs-Farkas showed that the kappa agreement was 0.23 for detecting rib fractures on CXRs[27]. However, none of the studies differentiated between conventional reading of the X-ray and reading by a dedicated radiologist.
During the initial assessment of a CXR of thoracic trauma patients by the trauma team a significant number of thoracic injuries are missed. A second read by a trauma radiologist can improve the detection of these injuries. This conclusion translated into clinical practice: CXR in trauma patients - take a second look.
In common practice, the chest X-ray (CXR) of trauma patients in the emergency department is assessed by the trauma team, frequently by residents on call. Although the trauma team may have adequate interpretive skills, they do not routinely have the luxury of unrestricted interpretation times and have to work under difficult conditions.
In the literature, little has been published on the difference in detecting injuries on a CXR by a dedicated radiologist and by a trauma team. This study shows how to focus on the detection of injuries on the routinely used CXR for patients in the emergency room.
There is an ongoing discussion regarding improving the detection of thoracic injuries by using a computed tomography (CT)-scan of the thorax instead of a CXR. However, the CT-scan is more expensive, not every trauma department is equipped with a CT-scanner in the trauma room and a CT-scan significantly increases the radiation dose of the patient. Few studies have focused on how to improve the detection rate of the conventional CXR.
A dedicated radiologist detects more pneumothoraces, hemothoraces and pulmonary contusions on a CXR than a conventional trauma team. One could consider adding a dedicated radiologist to the trauma team.
The paper is well written with a clear hypothesis and study design, appropriate statistics and conclusions.
Peer reviewer: Thomas Deserno, PhD, Professor, Department of Medical Informatics, RWTH Aachen University, Pauwelsstr. 30, 52057 Aachen, Germany
S- Editor Cheng JX L- Editor Logan S E- Editor Zheng XM
| 1. | Kortbeek JB, Al Turki SA, Ali J, Antoine JA, Bouillon B, Brasel K, Brenneman F, Brink PR, Brohi K, Burris D. Advanced trauma life support, 8th edition, the evidence for change. J Trauma. 2008;64:1638-1650. [PubMed] |
| 2. | Berrington de González A, Darby S. Risk of cancer from diagnostic X-rays: estimates for the UK and 14 other countries. Lancet. 2004;363:345-351. [PubMed] |
| 3. | Ball CG, Ranson K, Dente CJ, Feliciano DV, Laupland KB, Dyer D, Inaba K, Trottier V, Datta I, Kirkpatrick AW. Clinical predictors of occult pneumothoraces in severely injured blunt polytrauma patients: A prospective observational study. Injury. 2009;40:44-47. [PubMed] |
| 4. | Benger JR, Lyburn ID. What is the effect of reporting all emergency department radiographs. Emerg Med J. 2003;20:40-43. [PubMed] |
| 5. | Perron AD, Huff JS, Ullrich CG, Heafner MD, Kline JA. A multicenter study to improve emergency medicine residents' recognition of intracranial emergencies on computed tomography. Ann Emerg Med. 1998;32:554-562. [PubMed] |
| 6. | Bansidhar BJ, Lagares-Garcia JA, Miller SL. Clinical rib fractures: are follow-up chest X-rays a waste of resources. Am Surg. 2002;68:449-453. [PubMed] |
| 7. | Holcomb JB, McMullin NR, Kozar RA, Lygas MH, Moore FA. Morbidity from rib fractures increases after age 45. J Am Coll Surg. 2003;196:549-555. [PubMed] |
| 8. | Flagel BT, Luchette FA, Reed RL, Esposito TJ, Davis KA, Santaniello JM, Gamelli RL. Half-a-dozen ribs: the breakpoint for mortality. Surgery. 2005;138:717-23; discussion 723-5. [PubMed] |
| 9. | Bulger EM, Arneson MA, Mock CN, Jurkovich GJ. Rib fractures in the elderly. J Trauma. 2000;48:1040-1046; discussion 1046-1047. [PubMed] |
| 10. | Cameron P, Dziukas L, Hadj A, Clark P, Hooper S. Rib fractures in major trauma. Aust N Z J Surg. 1996;66:530-534. [PubMed] |
| 11. | Gabram SG, Schwartz RJ, Jacobs LM, Lawrence D, Murphy MA, Morrow JS, Hopkins JS, Knauft RF. Clinical management of blunt trauma patients with unilateral rib fractures: a randomized trial. World J Surg. 1995;19:388-393. [PubMed] |
| 12. | Kerr-Valentic MA, Arthur M, Mullins RJ, Pearson TE, Mayberry JC. Rib fracture pain and disability: can we do better. J Trauma. 2003;54:1058-1063; discussion 1058-1063. [PubMed] |
| 13. | Stocchetti N, Pagliarini G, Gennari M, Baldi G, Banchini E, Campari M, Bacchi M, Zuccoli P. Trauma care in Italy: evidence of in-hospital preventable deaths. J Trauma. 1994;36:401-405. [PubMed] |
| 14. | Baumann MH, Sahn SA. Tension pneumothorax: diagnostic and therapeutic pitfalls. Crit Care Med. 1993;21:177-179. [PubMed] |
| 15. | Plewa MC, Ledrick D, Sferra JJ. Delayed tension pneumothorax complicating central venous catheterization and positive pressure ventilation. Am J Emerg Med. 1995;13:532-535. [PubMed] |
| 16. | Barrios C, Tran T, Malinoski D, Lekawa M, Dolich M, Lush S, Hoyt D, Cinat ME. Successful management of occult pneumothorax without tube thoracostomy despite positive pressure ventilation. Am Surg. 2008;74:958-961. [PubMed] |
| 17. | Collins JC, Levine G, Waxman K. Occult traumatic pneumothorax: immediate tube thoracostomy versus expectant management. Am Surg. 1992;58:743-746. [PubMed] |
| 18. | Jenner R, Sen A. Best evidence topic report. Chest drains in traumatic occult pneumothorax. Emerg Med J. 2006;23:138-139. [PubMed] |
| 19. | Enderson BL, Abdalla R, Frame SB, Casey MT, Gould H, Maull KI. Tube thoracostomy for occult pneumothorax: a prospective randomized study of its use. J Trauma. 1993;35:726-729; discussion 726-729. [PubMed] |
| 20. | Bilello JF, Davis JW, Lemaster DM. Occult traumatic hemothorax: when can sleeping dogs lie. Am J Surg. 2005;190:841-844. [PubMed] |
| 21. | Stafford RE, Linn J, Washington L. Incidence and management of occult hemothoraces. Am J Surg. 2006;192:722-726. [PubMed] |
| 22. | Miller PR, Croce MA, Kilgo PD, Scott J, Fabian TC. Acute respiratory distress syndrome in blunt trauma: identification of independent risk factors. Am Surg. 2002;68:845-850; discussion 850-851. [PubMed] |
| 23. | Wu JS, Sheng L, Wang SH, Gu J, Ma YF, Zhang M, Gan JX, Xu SW, Zhou W, Xu SX. The impact of clinical risk factors in the conversion from acute lung injury to acute respiratory distress syndrome in severe multiple trauma patients. J Int Med Res. 2008;36:579-586. [PubMed] |
| 24. | Plurad D, Martin M, Green D, Salim A, Inaba K, Belzberg H, Demetriades D, Rhee P. The decreasing incidence of late posttraumatic acute respiratory distress syndrome: the potential role of lung protective ventilation and conservative transfusion practice. J Trauma. 2007;63:1-7; discussion 8. [PubMed] |
| 25. | Zambon M, Vincent JL. Mortality rates for patients with acute lung injury/ARDS have decreased over time. Chest. 2008;133:1120-1127. [PubMed] |
| 26. | Brar MS, Bains I, Brunet G, Nicolaou S, Ball CG, Kirkpatrick AW. Occult pneumothoraces truly occult or simply missed: redux. J Trauma. 2010;69:1335-1337. [PubMed] |
| 27. | Szucs-Farkas Z, Lautenschlager K, Flach PM, Ott D, Strautz T, Vock P, Ruder TD. Bone images from dual-energy subtraction chest radiography in the detection of rib fractures. Eur J Radiol. 2011;79:e28-e32. [PubMed] |