Published online Oct 28, 2012. doi: 10.4329/wjr.v4.i10.439
Revised: October 11, 2011
Accepted: January 4, 2012
Published online: October 28, 2012
Colonic volvulus is a relatively uncommon cause of large bowel obstruction usually involving mobile, intra-peritoneal, colonic segments. Congenital or acquired anatomic variation may be associated with an increased risk of colonic volvulus which can occasionally involve retro-peritoneal segments. We report a case of 54-year-old female who presented to our Institution to perform a plain abdominal film series for acute onset of cramping abdominal pain. Both the upright and supine films showed signs of acute colonic obstruction which was thought to be due to an internal hernia of the transverse colon into the lesser sac. The patient was therefore submitted to a multi-detector contrast-enhanced computed tomography (CT). CT findings were initially thought to be consistent with the presumed diagnosis of internal hernia but further evaluation and coronal reformatting clearly depicted the presence of a colonic volvulus possibly resulting from a retro-gastric colon. At surgery, a volvulus of the ascending colon was found and a right hemi-colectomy had to be performed. However, a non rotated midgut with a right-sided duodeno-jejunal flexure and a left sided colon was also found at laparotomy and overlooked in the pre-operative CT. Retrospective evaluation of CT images was therefore performed and a number of CT signs of intestinal malrotation could be identified.
- Citation: Camera L, Calabrese M, Mainenti PP, Masone S, Vecchio WD, Persico G, Salvatore M. Volvulus of the ascending colon in a non-rotated midgut: Plain film and MDCT findings. World J Radiol 2012; 4(10): 439-442
- URL: https://www.wjgnet.com/1949-8470/full/v4/i10/439.htm
- DOI: https://dx.doi.org/10.4329/wjr.v4.i10.439
Colonic volvulus is a relatively uncommon cause of large bowel obstruction accounting for almost 5% of all cases of intestinal obstruction and 10% of colonic obstruction. It usually involves mobile, intra-peritoneal, colonic segments such as the cecum, transverse colon and sigmoid colon[1].
Congenital (e.g., malrotation) or acquired (e.g., abdominal surgery) anatomical variations may be associated with an increased risk of colonic volvulus. Malrotation, in particular, includes a broad spectrum of fixation anomalies of the small and large bowel occurring when the midgut fails to complete the required 270° counter-clockwise rotation during the embryologic development[2]. This can lead to different degrees of malrotation whereas the term non-rotation indicates the anatomic situation in which the Treitz and the small bowel are right-sided and the entire colon is left-sided[3]. Such is usually an asymptomatic condition which can be occasionally encountered in adult patients[4].
While both the imaging features of intestinal malrotation in adults[5] as well as the diagnostic yield of multi-detector computed tomography (MDCT) in the acute setting of large bowel obstruction have long been recognized[6], the added value of coronal reformatted or reconstructed images in the setting of colonic volvulus has only been recently reported[7].
Herein, we report a case of an acute colonic obstruction which was first thought to be due to an internal hernia of the transverse colon into the lesser sac at the plain abdominal film series, later shown by MDCT to be due to a colonic volvulus possibly resulting from a retrogastric dislocation of the splenic flexure and finally found at surgery to be a volvulus of the ascending colon in a non rotated midgut.
To the best of our knowledge, such a case has never been reported in the radiological literature.
A 54-year-old woman was referred to our institution to undergo an abdominal plain film series for acute onset of crampy abdominal pain, which was only partially relieved by antispastic drugs prescription in the 3 d before hospital admission.
The patient’s past medical history was unremarkable as well as most of lab tests except for mild leukocytosis [white blood cells = 12 × 103/mL 89% neutrophils] and increased levels of both creatine-kinase (220 U/L, n.v. 0-140) and lactate dehydrogenase (500 U/L, n.v. 227-450). She had no previous history of abdominal surgery.
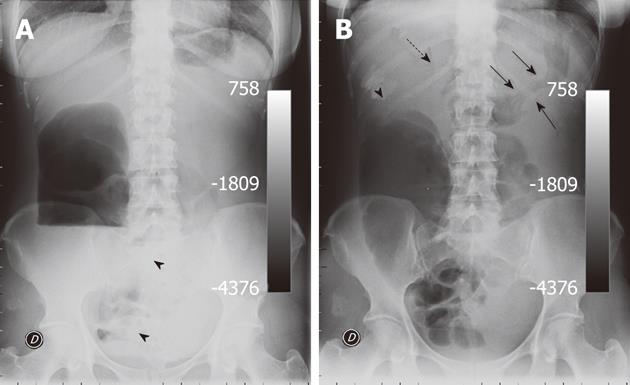
Plain films were performed in both the upright (Figure 1A) and supine position (Figure 1B). The upright film showed a huge air-fluid level in the right flank consistent with obstruction of the ascending colon along with some small bowel air-fluid levels in the lower pelvis and in the mid abdomen (Figure 1A). The supine film showed an abnormally dilated ascending colon with mild distension of some ileal loops in the pelvis whereas both the descending colon and the sigma appeared gasless. Faecal impaction could also be seen at the level of the hepatic flexure along with the associated evidence of an ab-extrinsic printing on the gastric body (Figure 1B). Based on this latter finding, a presumed diagnosis of colonic obstruction due to an internal hernia of the transverse colon into the lesser sac was postulated.
The patient was then submitted to a contrast-enhanced multi-detector abdominal CT (Aquilion 4, Toshiba, Japan) which was performed with a detector configuration of 3 mm × 4 mm, table feed of 9 mm/s, rotation time 0.5 s, beam pitch 1.5, 1.5 mm reconstruction intervals, section thickness of 3 mm, 300 mAs, 120 kVp. A monophasic acquisition was performed 70 s after i.v. bolus (2 cc/s) injection of 150 cc of iodinated non ionic contrast media (Ultravist 370, Bayer Shering Pharma, Berlin, Germany).
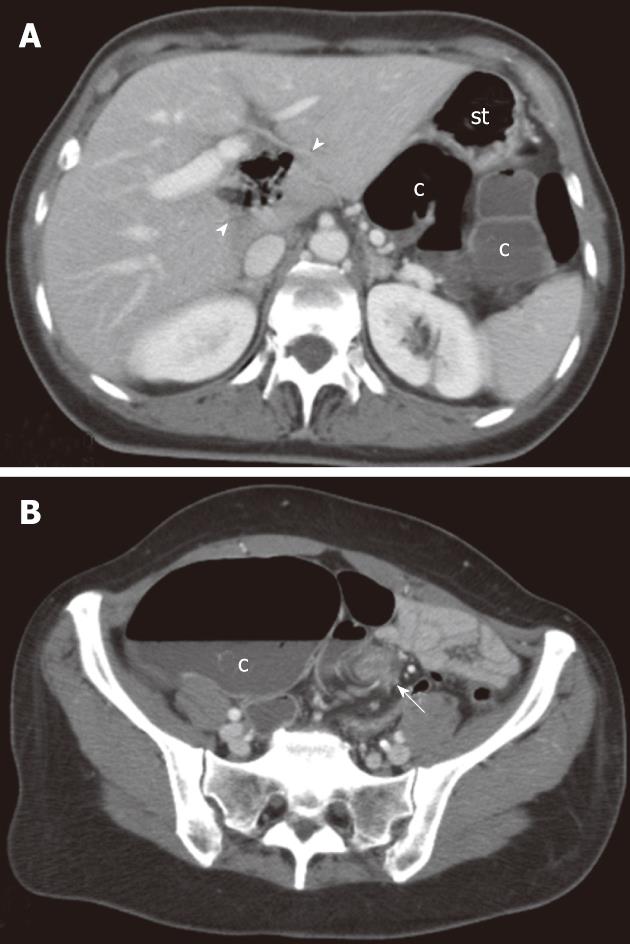
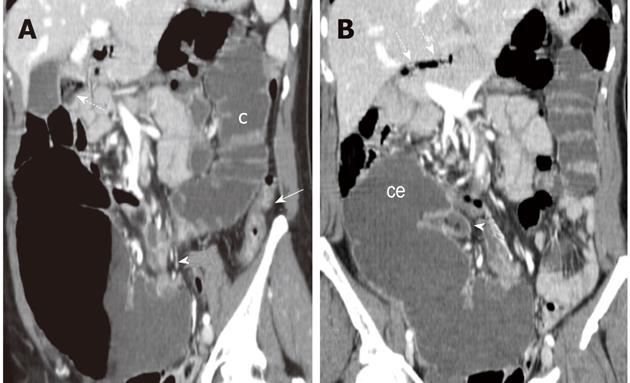
At MDCT, initial evaluation of axial images supported the diagnosis of internal hernia since a gas-containing loop was depicted within the hepatic hilum suggesting a herniation of the transverse colon through the foramen of Winslow (Figure 2A). However, colonic segments proximal to the splenic flexure also appeared distended by fluid and colonic distension could be traced back to the left iliac fossa where torsion of the mesenteric vascular axis (whirl sign) was clearly depicted suggesting a volvulus (Figure 2B). Coronal reformatted images were then obtained (Figure 3).
On the coronal oblique plane, colonic segments distal to the transition zone appeared distended by fluid throughout the splenic flexure whereas the descending colon was collapsed (Figure 3A). On the coronal plane (Figure 3B) the cecum appeared tilted and displaced in the sub-hepatic space.
The patient underwent immediate surgery. At laparotomy, a volvulus of the ascending colon was found and a right hemi-colectomy had to be performed because of ischemia of the involved segments. However, a concomitant malrotation was also found with the ligament of Treitz located in the right upper quadrant (Type 1) and the transverse colon displaced under the root of the mesentery. A derotation had to be performed. The patient had an uneventful recovery and was discharged 13 d later.
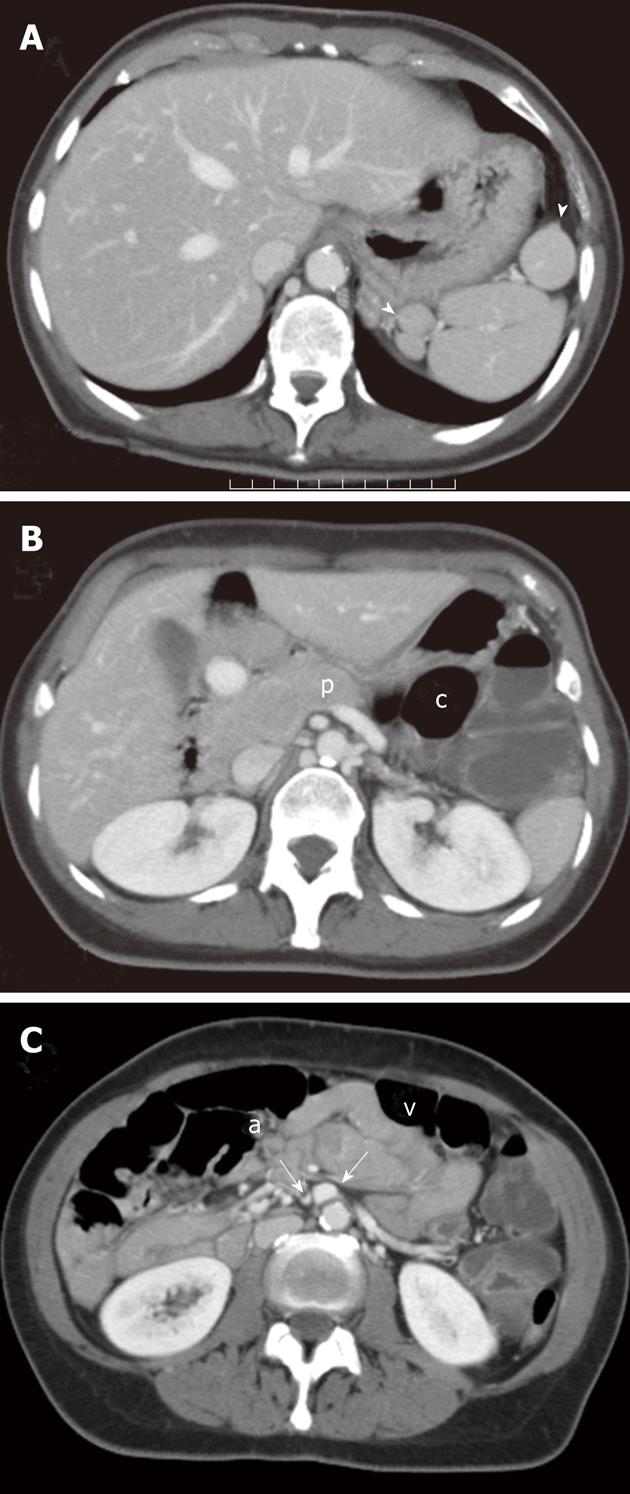
CT scans were then reviewed and a number of CT signs of malrotation were retrospectively found (Figure 4).
Intestinal malrotation is a congenital anomaly resulting in an abnormal position of the small and/or the large bowel within the peritoneal cavity[2]. It includes a broad spectrum of fixation anomalies occurring when the midgut fails to complete the required 270° counter-clockwise rotation during embryologic development. In particular, the term non-rotation indicates the anatomic situation in which the Treitz and the small bowel are right-sided and the entire colon is left-sided[3]. While this is usually an asymptomatic condition[4], it can rarely lead to an acute colonic obstruction due to volvulus of the ascending colon[8].
In our patient, the acute colonic obstruction was initially thought to be due to an internal hernia through the foramen of Winslow. These account for almost 8% of internal hernias defined as protrusion of an abdominal viscus through a natural or a pathologic defect in the peritoneal surface which can either be congenital or acquired following a trauma or a surgical procedure[9].
Almost one third of internal hernias through the foramen of Winslow may involve the large bowel, namely the transverse colon[10]. This was thought to be the case with our patient as the upright film showed a huge isolated air-fluid level in the right flank (Figure 1A) along with a mottled appearance in the sub-hepatic space and an ab-extrinsic printing on the gastric body, the latter most evident in the supine film (Figure1B).
This diagnostic impression was also confirmed by initial evaluation of transverse CT images which revealed intra-luminal gas bubbles at the level of hepatic hilum (Figure 2A). This finding was erroneously thought to be consistent with the diagnosis of internal hernia into the lesser sac. Conversely, CT findings of internal hernias through the foramen of Winslow should include the presence of mesenteric fat in the porto-caval space as well as the evidence of an air-fluid collection in the lesser sac with a beak directed toward the foramen of Winslow[9-11]. In our case, there only was a colonic segment situated behind the stomach (Figure 2A) without definite evidence of herniation.
Ours has, thus, to be considered an interpretative error. Retrospectively, gas bubbles at the level of the hepatic hilum (Figure 2A) could then be traced to either the duodenum, which was found at surgery to be confined to the right between the inferior vena cava and main portal vein and/or the Treitz which was found to be right-sided. Retrospectively, these air bubbles could also be appreciated in the supine film (Figure 1B) whereas the mottled appearance depicted in the sub-hepatic space could be traced to fecal reflux in the distal ileum as shown by the oblique coronal reformatted image (Figure 3A).
The ab-extrinsic printing on the gastric body (Figure 1B) was instead due to the retrogastric dislocation of the colon proximal to the splenic flexure as shown by CT (Figure 2A). As this usually represents a normal anatomic variation occasionally encountered in adults[12], in our patient it possibly represented the cause of the volvulus of the ascending colon which was found at surgery not be attached to the posterior peritoneum because of a congenital non rotation of the midgut. This latter was overlooked in the pre-operative CT but a number of CT findings suggestive of intestinal malrotation could be retrospectively appreciated (Figure 4).
First, a number of nodules isodense to the splenic parenchyma could be found in the left sub-phrenic space (Figure 4A) configuring a poly-splenia syndrome which is a condition correlated with intestinal malrotation either alone[13] or in association with agenesis of the dorsal pancreas[14] which it could also be retrospectively detected in our patient (Figure 4B). Finally, an inverted anatomic relationship of the superior mesenteric artery and vein was noted (Figure 4C). This represents the most accurate finding in intestinal malrotation which was first described in 1983[15].
However, CT clearly depicted the torsion of mesenteric vessels (whirl sign) suggesting the correct diagnosis of volvulus which was confirmed at surgery (Figure 2B). This finding is considered to have a high positive predictive value for the CT diagnosis of volvulus, for both small and large bowel[16]. It represents the twisting and engorgement of the mesenteric vessels around a central point in the peritoneal cavity and it is best appreciated when imaging is perpendicular to the axis of bowel rotation, hence the benefit of multiplanar reformations[6].
We have described a case of a surgically proven volvulus of the ascending colon in a patient with a non rotated midgut and a retrogastric dislocation of the colon proximal to the splenic flexure. To the best of our knowledge, such a case has not been previously reported.
Peer reviewer: Tilo Niemann, MD, Department of Radiology, University Hospital Basel, Petersgraben 4, CH-4031 Basel, Switzerland
S- Editor Cheng JX L- Editor O'Neill M E- Editor Xiong L
| 2. | Balthazar EJ. Congenital positional anomalies of the colon: radiographic diagnosis and clinical implications. I. Abnormalities of rotation. Gastrointest Radiol. 1977;2:41-47. [PubMed] |
| 3. | Jamieson D, Stinger DA. Small bowel. Pediatric gastrointestinal imaging. 2nd ed. Hamilton, Ontario, Canada: Decker 2000; 311-314. |
| 4. | Zissin R, Rathaus V, Oscadchy A, Kots E, Gayer G, Shapiro-Feinberg M. Intestinal malrotation as an incidental finding on CT in adults. Abdom Imaging. 1999;24:550-555. [PubMed] |
| 5. | Pickhardt PJ, Bhalla S. Intestinal malrotation in adolescents and adults: spectrum of clinical and imaging features. AJR Am J Roentgenol. 2002;179:1429-1435. [PubMed] |
| 6. | Sinha R, Verma R. Multidetector row computed tomography in bowel obstruction. Part 2. Large bowel obstruction. Clin Radiol. 2005;60:1068-1075. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 20] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Vandendries C, Jullès MC, Boulay-Coletta I, Loriau J, Zins M. Diagnosis of colonic volvulus: findings on multidetector CT with three-dimensional reconstructions. Br J Radiol. 2010;83:983-990. [PubMed] |
| 8. | Berger RB, Hillemeier AC, Stahl RS, Markowitz RI. Volvulus of the ascending colon: an unusual complication of non-rotation of the midgut. Pediatr Radiol. 1982;12:298-300. [PubMed] |
| 9. | Mathieu D, Luciani A. Internal abdominal herniations. AJR Am J Roentgenol. 2004;183:397-404. [PubMed] |
| 10. | Orseck MJ, Ross JP, Morrow CE. Herniation of the hepatic flexure through the foramen of Winslow: a case report. Am Surg. 2000;66:602-603. [PubMed] |
| 11. | Takeyama N, Gokan T, Ohgiya Y, Satoh S, Hashizume T, Hataya K, Kushiro H, Nakanishi M, Kusano M, Munechika H. CT of internal hernias. Radiographics. 2005;25:997-1015. [PubMed] |
| 12. | Oldfield AL, Wilbur AC. Retrogastric colon: CT demonstration of anatomic variations. Radiology. 1993;186:557-561. [PubMed] |
| 13. | Gayer G, Apter S, Jonas T, Amitai M, Zissin R, Sella T, Weiss P, Hertz M. Polysplenia syndrome detected in adulthood: report of eight cases and review of the literature. Abdom Imaging. 1999;24:178-184. [PubMed] |
| 14. | Soler R, Rodríguez E, Comesaña ML, Pombo F, Marini M. Agenesis of the dorsal pancreas with polysplenia syndrome: CT features. J Comput Assist Tomogr. 1992;16:921-923. [PubMed] |
| 15. | Nichols DM, Li DK. Superior mesenteric vein rotation: a CT sign of midgut malrotation. AJR Am J Roentgenol. 1983;141:707-708. [PubMed] |
| 16. | Lepage-Saucier M, Tang A, Billiard JS, Murphy-Lavallée J, Lepanto L. Small and large bowel volvulus: Clues to early recognition and complications. Eur J Radiol. 2010;74:60-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 28] [Article Influence: 1.8] [Reference Citation Analysis (0)] |