Published online Oct 28, 2012. doi: 10.4329/wjr.v4.i10.431
Revised: September 17, 2012
Accepted: September 24, 2012
Published online: October 28, 2012
AIM: To measure and compare computed tomography (CT) radiation doses delivered to patients in public paediatric hospitals in Australia and Saudi Arabia.
METHODS: Doses were measured for routine CT scans of the head, chest and abdomen/pelvis for children aged 3-6 years in all dedicated public paediatric hospitals in Australia and Saudi Arabia using a CT phantom measurement cylinder.
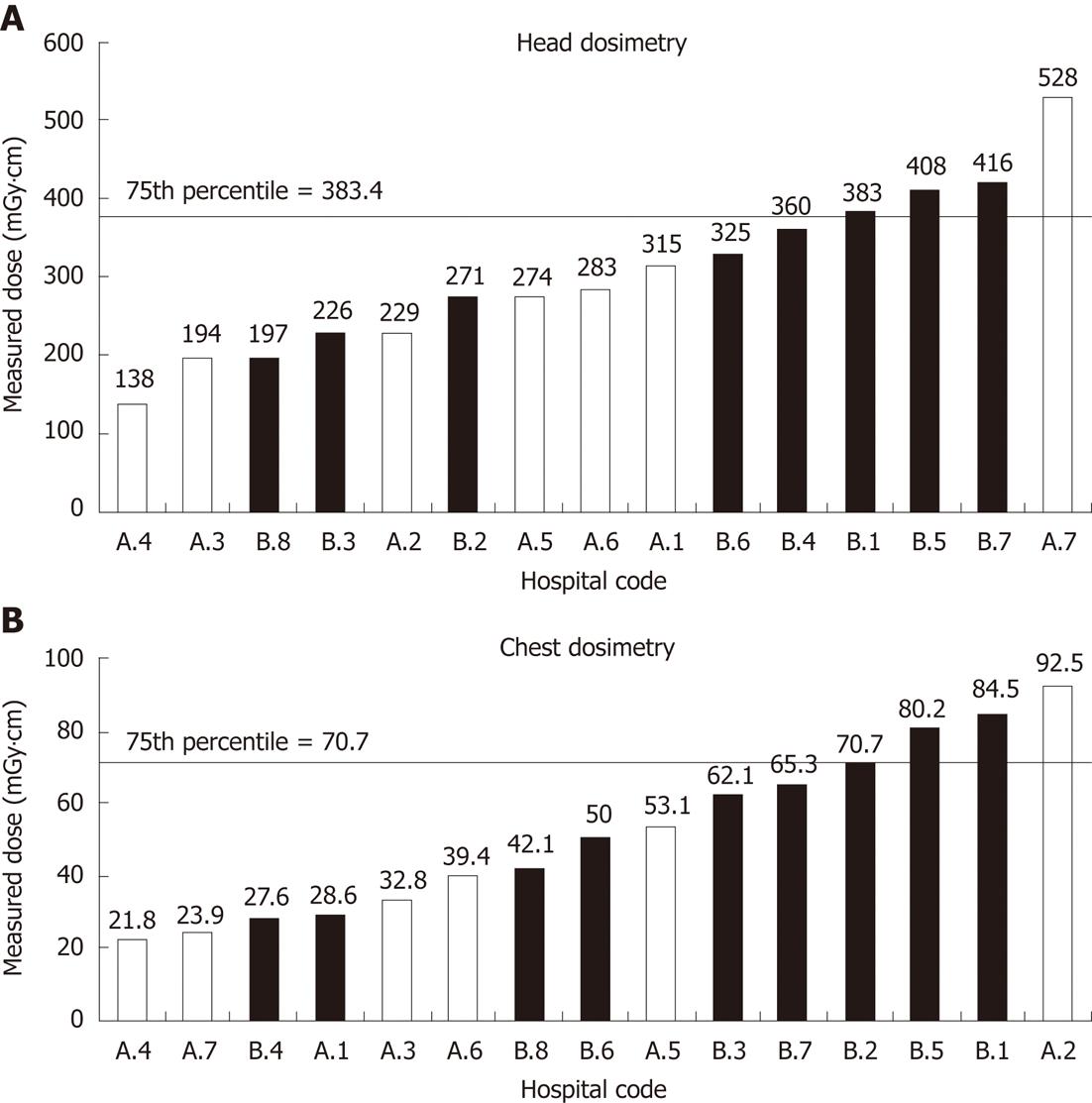
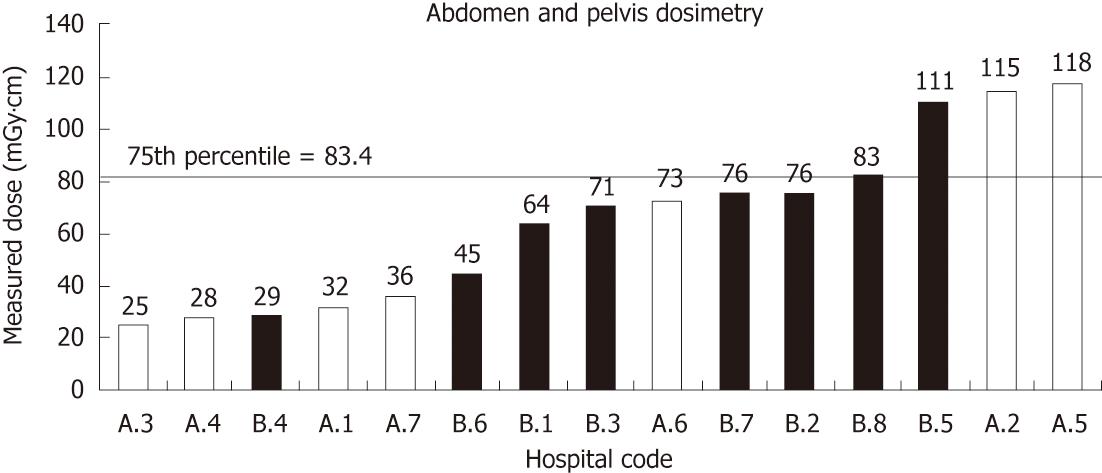
RESULTS: CT doses, using the departments’ protocols for 3-6 year old, varied considerably between hospitals. Measured head doses varied from 137.6 to 528.0 mGy·cm, chest doses from 21.9 to 92.5 mGy·cm, and abdomen/pelvis doses from 24.9 to 118.0 mGy·cm. Mean head and abdomen/pelvis doses delivered in Saudi Arabian paediatric CT departments were significantly higher than those in their Australian equivalents.
CONCLUSION: CT dose varies substantially across Australian and Saudi Arabian paediatric hospitals. Therefore, diagnostic reference levels should be established for major anatomical regions to standardise dose.
- Citation: Mohiy HA, Sim J, Seeram E, Annabell N, Geso M, Mandarano G, Davidson R. A dose comparison survey in CT departments of dedicated paediatric hospitals in Australia and Saudi Arabia. World J Radiol 2012; 4(10): 431-438
- URL: https://www.wjgnet.com/1949-8470/full/v4/i10/431.htm
- DOI: https://dx.doi.org/10.4329/wjr.v4.i10.431
The use of computed tomography (CT) as a diagnostic tool has dramatically increased[1], and with it, the radiation exposure to the general population, which may be a public health issue in the future[2]. Approximately 62 million CT examinations were performed in the United States in 2006, and the numbers are growing at 10% per annum; 4 million CT scans (approximately 6.5%) were performed on American children[1,3]. In Australia between 1996 and 2010, total CT scan numbers have increased 2.8-fold, and paediatric CT scan examinations have had a 2.4-fold increase[4]. Japan, the United States of America and Australia lead the world in the number of CT scanners, with 64, 26 and 18 scanners per million citizens, respectively[5]. The number of CT scans is reportedly growing at about 9% each year in Australia[6]. It is estimated that CT scanning in Australia accounts for 65% of the population’s medical radiation exposure[7]. In 2006, an estimated 13.5 million radiological procedures were undertaken, and approximately 2.4 million of these procedures were CT scans[4]. Schauer et al[8] suggest that because of this increase in CT referrals, and the relatively heavy dose contribution from CT, the risks to the population from ionising radiation will also increase.
Approximately 33% of all paediatric CT examinations are in children aged ten years old or younger, with 17% in children aged five or younger[9]. At these ages, the organs and tissues are intrinsically more sensitive to oncogenic effects of radiation due to the far higher proportion of cells that are dividing and reproducing[10-12]. The radiation-induced risk is also higher in paediatric patients due to wider and increased cellular distribution of red bone marrow, and their greater post-exposure life expectancy[13,14]. The effective radiation doses received by children are about 50% higher than those received by adults for the same acquisition protocols, due to their smaller body size and related attenuation[15]. It is crucial for radiographers and radiologists to understand how CT dose relates to radiation bio-effects. With the growing popularity of CT, and the associated risks of radiation exposure, the need for national comparative CT dose survey data is clear.
Diagnostic reference levels (DRLs) are used for comparison of CT doses from different hospitals and to encourage CT departments to reduce their patient radiation dose levels[16]. A DRL, as first defined by the International Commission on Radiological Protection (ICRP), is “a form of investigation level, applied to an easily measured quantity, usually the absorbed dose in air, or tissue-equivalent material at the surface of a simple phantom or a representative patient”[17]. The ICRP recommended the establishment of DRLs in order to allow CT departments to compare their dose levels to national or regional standards. Using a specified dose measurement protocol and phantom, the DRL is usually defined as the 75th percentile of the data distribution[18]. This identifies the departments which lie above the DRL as those in which dose reduction would have the greatest impact. Since the DRL will always be breached by 25% of the population, the DRL should be used as an indication rather than a proof of excessive dose[19].
The use of DRLs has reduced the overall dose and the range of doses observed in clinical practice in the United Kingdom, with a 50% decrease in average dose between 1985 and 2000[20,21]. To achieve similar outcomes in Australia, DRL surveys must initially be conducted[19]. This paper describes the conduct and results of the first survey of public paediatric hospitals in Australia and Saudi Arabia.
The objective of this research was to obtain doses from common paediatric CT scan examinations in Australia and Saudi Arabia using a simple dose measurement method. From these data, a simple ranking method, similar to those used in DRL methods, was used so that staff in CT departments undertaking paediatric examinations can use this method to compare their CT scan factors against the dedicated paediatric CT scanners.
An additional objective was to compare measured dose data with the dose information that was displayed on the CT console, which should be a regular part of quality assurance procedures. This comparison would assure paediatric CT staff of their ability to evaluate their doses from console data.
Radiation dose measurements were obtained for CT scan examinations of the head, chest and abdomen/pelvis using existing departmental protocols for children aged 3-6 years from all public paediatric hospitals in Australia (designated A1 to A7) and Saudi Arabia (designated B1 to B8) [see Table 1 for details of CT scanners; note that eight models of CT scanner (1, 6, 16 and 64 slices), manufactured by four different companies, were in use at the 15 participating hospitals]. This age range was selected due to the availability of data for all paediatric hospitals participating in the study, and also because this is a popular age for paediatric injuries resulting from trips and falls. Scans were performed in the departments’ own CT scan units using a CT phantom measurement cylinder of 16 cm diameter[22].
| Country | Hospital code | Manufacture | Model | No. of rows of detectors |
| Australia | A1 | Siemens | Sensation | 16 |
| Australia | A2 | Philips | Brilliance | 64 |
| Australia | A3 | General electric | Light speed VCT | 64 |
| Australia | A4 | Toshiba | Aquilion | 64 |
| Australia | A5 | Philips | Brilliance | 64 |
| Australia | A6 | Siemens | Somatom sensation | 64 |
| Australia | A7 | Toshiba | Aquilion | 16 |
| Saudi Arabia | B1 | Toshiba | Aquilion | 64 |
| Saudi Arabia | B2 | Siemens | Emotion | 1 |
| Saudi Arabia | B3 | General electric | Light speed VCT | 64 |
| Saudi Arabia | B4 | Siemens | Somanta | 6 |
| Saudi Arabia | B5 | General electric | Light speed | 16 |
| Saudi Arabia | B6 | General electric | Hispeed | 4 |
| Saudi Arabia | B7 | Siemens | Emotion | 1 |
| Saudi Arabia | B8 | Siemens | Emotion | 1 |
The phantom was scanned using department protocols for each region and dose was recorded using a DIADOS dosimeter and 100 mm long free-air ionisation chamber (PTW DIADOS, Freiburg, Germany). The recorded charge, in nC, was converted to mGy·cm using an established conversion factor. The phantom was scanned over a range of 100 mm, placing the CT probe only in the central chamber. The purpose of scanning over this volume was to eliminate differences due to slice/beam thickness, number of slices and pitches between each department’s protocols. Each CT scan used the department “routine” protocol for each anatomical region and was repeated for a total of three measurements. For all hospitals and scan regions, the three measurements were found to agree to within 0.5% error. Where provided by the CT manufacturer, volume computed tomography dose index (CTDIvol) and/or dose length products (DLP) were recorded for each scan.
From the dosimetry data, reference levels (RLs) were calculated using the developed RL methodology for each CT anatomical region in each country. The RL methodology is similar to DRL, where dosimetry data is placed in rank order. The 75th percentile was used as a RL threshold, with hospitals above this value being classified as delivering “high” doses[19].
To determine whether there was a statistically significant difference between the Australian and Saudi Arabian hospital CT protocols for each anatomical regions (head, chest, abdomen/pelvis), the measured doses were compared using Student’s t-tests (in MINITAB v16) with the confidence level set at 95%. The definition used for an outlier data point is a point which falls more than 1.5 times the interquartile range above the third quartile, or below the first quartile[23].
Figure 1 shows the mean head dosimetry measurements delivered in the seven Australian and eight Saudi hospitals.
The measured head doses from paediatric CT scan protocols in the Australian hospitals had greater range than the Saudi Arabian scans. Nevertheless, the Australian data include a cluster of six doses in the range 137.6 to 315.1 mGy·cm with an outlier at 528 mGy·cm, being the only dose produced by an Australian CT head scan protocol above the 75th percentile DRL. The RL is exceeded in three of the eight Saudi Arabian hospitals sampled; indicating that the Saudi dose distribution is skewed to the right of the Australian distribution. As can be seen in Figure 1, five of the six highest CT head scan doses are from Saudi Arabian CT departments.
The measured head doses given by standard paediatric CT protocol in the Saudi Arabian hospitals varied from just below 200 mGy·cm to 416.3 mGy·cm. The variation in the range of doses from CT head scan protocols in Saudi Arabian paediatric hospitals is less than that in Australian paediatric hospitals.
With the exception of hospital A7 at 528.0 mGy·cm, measured Australian paediatric CT head scan doses were lower than most Saudi Arabian doses, although the overall variation in Saudi Arabian paediatric CT head scan doses was less than observed in the Australian data. The mean Australian paediatric CT head scan dose was not significantly lower than the mean Saudi Arabian paediatric CT head scan dose by 2-sample Student’s t-test (280.1 mGy·cm vs 323.3 mGy·cm, P = 0.438); however, when the sole Australian outlier was removed, the difference was weakly significant (238.8 mGy·cm vs 323.3 mGy·cm, P < 0.10).
The Australian paediatric CT chest data are similar in distribution to the CT head data, in that there is an overall lower grouping with six hospitals delivering standard doses in a small range between 21.8 mGy·cm and 53.1 mGy·cm. The 75th percentile for the Australian hospitals was at 52.1 mGy·cm.
The CT chest doses given by standard paediatric CT protocol in the Saudi Arabian hospitals varied from below 30 mGy·cm to 84.5 mGy·cm. The 75th percentile for Saudi Arabian hospitals was at 77.8 mGy·cm. As can be seen in Figure 2, five of the six highest doses are from Saudi Arabia.
Generally, the Australian CT chest doses were lower than most Saudi Arabian doses. The mean measured Australian chest CT dose was not significantly lower than the mean Saudi Arabian dose by 2-sample Student’s t-test (41.7 mGy·cm vs 60.3 mGy·cm, P = 0.127).
The distribution of Australian mean abdomen/pelvis radiation doses shown in Figure 2 is different to that shown in Figure 1A (head) and 1B (chest), with four hospitals clustered tightly at the low end of the range (24.9-36.4 mGy·cm), a fifth hospital (A6) in the middle of the range at 72.8 mGy·cm, and two larger values at over 100 mGy·cm each.
Note that the highest values (A2 and A5) were also the hospitals which delivered the highest measured doses for chest scans (Figure 3). The 75th percentile for Australian hospitals was at 113.9 mGy·cm. The CT abdomen/pelvis doses given by standard paediatric CT protocol in the Saudi Arabian hospitals varied from below 30 mGy·cm to 111.1 mGy·cm - an increase by a factor of nearly four. The 75th percentile for Saudi Arabian hospitals was at 81.7 mGy·cm. Unlike the head and chest dose distributions, the Saudi Arabian abdomen/pelvis 75th percentile value is lower than the Australian 75th percentile value.
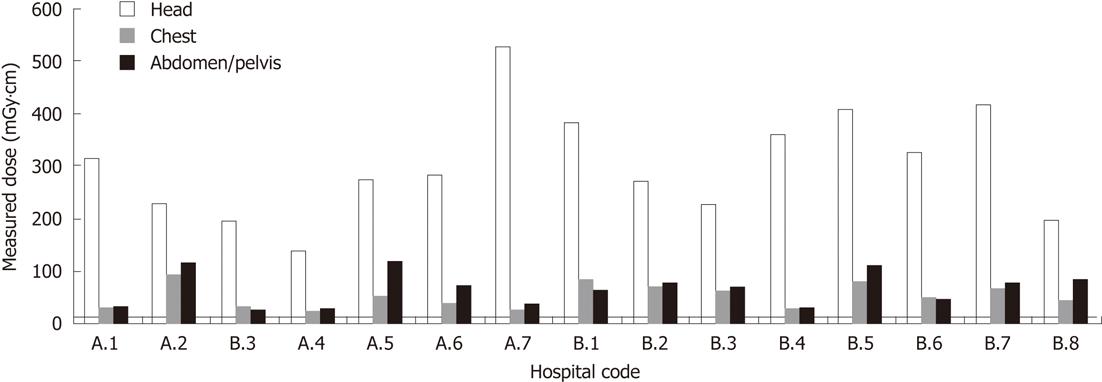
As can be seen in Figure 1B, four of the six highest abdomen/pelvis doses are from Saudi Arabian CT departments, and four of the five lowest doses were from Australian CT departments. Figure 4C shows an unusual distribution of radiation doses, with clusters around 30.0 mGy·cm, 70.0 mGy·cm and 115.0 mGy·cm. Saudi and Australian doses exhibit very similar ranges, although four of seven Australian doses are in the 30 mGy·cm cluster. The mean Australian abdomen/pelvis CT dose was not significantly different from the mean Saudi Arabian abdomen/pelvis dose (61.1 mGy·cm vs 69.4 mGy·cm, P = 0.637). Figure 3A combines the resulting data in Figures 1 and 2. This provides an alternative perspective in tracking each institution’s performance across different protocols. The 75th percentile line is also included for each protocol: head, chest and abdomen/pelvis.
Head, chest and abdomen/pelvis region CT dosimetry readings were analysed to determine whether there was any difference between single-slice and multi-slice CT scanners. Using 2-sample Student’s t-tests, it was found that there was no statistically significant difference between the dose distributions for single-slice and multi-slice CT machines in the head (P = 0.895), chest (P = 0.435) or abdomen/pelvis (P = 0.151) dosimetry data.
Dose data, as provided by the manufacturer in the CT console, were obtained from 10 of the 15 CT scanners. Five of the CT scanners did not have facilities to display DLP and CTDIvol information as these were older CT scanners, and as such, data were not able to be recorded. Figure 4 compare measured dose to the DLP and CTDIvol information from head, chest and abdomen/pelvis region, respectively.
This paper describes the first study of direct measurements of CT radiation doses in multiple dedicated paediatric hospitals conducted in Australia and Saudi Arabia. The authors measured doses delivered in CT departments in seven Australian and eight Saudi Arabian public paediatric hospitals for three common CT examinations (head, chest and abdomen/pelvis).
The methodology chosen to measure the CT doses is not that which is usually used to obtain DRLs. The method used here was chosen in order to simulate clinical examinations and then to compare paediatric CT scanners. In using this method, the dose reading does not just become dependent upon factors such as beam energy (kVp) and tube current (mA) in the departments but also on the CT protocols such as the choice of slice/beam thickness, number of slices within the 100 mm volume used and the pitch factor selected. In choosing this method, it is hoped that this careful approach to measure dose and the subsequent comparison with data provided on the CT console of DLP and CTDIvol will enable others to compare their dose reading to the RL obtained from dedicated paediatric CT scanners. One limitation of the approach used in this study is that at each end of the 100 mm long scan section, full scatter conditions are not present and so this may explain the discrepancy between measured dose and console data.
The results show that there is large variation between hospitals in CT doses delivered from standard protocols for patients aged 3-6 years and that these mean doses (delivered in Australian and Saudi Arabian CT departments) are significantly different (after discarding outlying observations). The fact that such large variation in dose was discovered in paediatric CT scan protocols makes these results particularly important, as children are more susceptible to harm from radiation[15].
Previous research involving estimated doses, based on CT protocols used in the United Kingdom, found that there was substantial variation in the paediatric CT doses delivered by different hospitals[24]. Our confirmation of the results of Shrimpton et al[24] highlights the importance of reducing excessive CT radiation exposure. For example, the head scan from hospital A7 delivered 3.8 times more radiation than that of hospital A4, and the abdomen/pelvis scan from hospital A5 delivered 4.7 times more radiation than that of hospital A3 - both deemed by their respective departments to produce images of adequate quality.
Dose RLs for CT are useful tools for lowering radiation levels[17], but have only recently become a priority in Australia. The Australian Radiation Protection and Nuclear Safety Agency (ARPANSA) was recently tasked with generating representative national DRLs for diagnostic imaging modalities that use ionising radiation[19]. At the time of writing, ARPANSA was in the process of finalising sampling and data collection procedures[25].
The differences between the measured dose delivered in Australian and Saudi Arabian CT departments are likely to be due to different levels of radiographer education, awareness of radiation dose and protocols[26,27]. Other researchers have found that understanding of the factors that affect patient doses in CT has a large impact on delivered dose, and is usually considered as the first step in optimisation strategies[28]. A 1998 study observed a variation of 10%-40% in the typical dose between individual scanners, largely due to imaging technique[29]. Mettler et al[30] pointed out that radiographers’ basic education and training overlooks paediatric CT radiation doses. The International Atomic Energy Agency recommends education and training of radiographers involved in paediatric CT[31].
The level of awareness within the radiography community of potential risks of CT radiation also plays a major role in dose levels. According to a recent survey[26,27], most Australian and Saudi Arabian radiographers lack education about - and awareness of the importance of - radiation dose in paediatric CT. Similarly, a recent survey of health professionals in Northern Ireland regarding awareness of the radiation doses imparted during common diagnostic imaging procedures and their long term impact on patients demonstrated a knowledge gap which could be improved with appropriate training[32]. A 2006 survey in New South Wales (Australia) showed the need for continuing education in paediatric CT examinations[33].
The results also show a variation of RL ranking within hospitals. Hospital A5 achieved a low comparative dose ranking for CT protocols of the head and chest, yet provided the highest recorded dose for the abdomen/pelvis CT examinations. The situation was similar for hospital A7, whose head CT scan doses were the highest, yet they had comparatively low doses for their chest abdomen/pelvis CT examinations. This further highlights the need for vigilance in examining CT doses across the entire range of examinations.
There was good correlation between the measured dose and recorded CTDIvol and DLP for paediatric CT head scans (P = 0.836 and P = 0.727, respectively), but the correlation for chest and abdomen/pelvis scans was poor. Our calculations indicate that the DLP was an average of 30% larger than the measured dose for any given scan. This discrepancy may be due to the size of phantom used in this study compared to the size of patient assumed by the console calculations, which may be a difference of 32 cm. This is supported by the observations of Siegel et al[34] (Figure 3) and Shrimpton et al[24] who found that dose measurements decrease with the increasing size of phantom. Individual facilities might be well advised to confirm agreement between console data and external measurements of their own scanner at commissioning and routine quality assurance. Departments considering reviewing their routine head CT scan doses can, with a high level of confidence, use their own CTDIvol and DLP measurements over 100 mm and determine where they are ranked against dedicated paediatric CT scanners.
To reduce CT radiation dose levels, it is important to regularly review and update CT protocols. A recent survey in Australia showed the need for regular protocol review for paediatric CT examinations[33]. This point was also made following a 2009 survey of Syrian CT departments, which recommended the establishment of national DRLs[35]. CT protocols must acknowledge the fact that manufacturers provide varying protocol guidelines for different technologies, and that these variations can greatly affect dose. Finally, each CT scan should have a clear medical justification to ensure that the overall CT dose delivered to the population is kept as low as practicable[36].
The results presented in this article show that paediatric CT dose variation is substantial across Australian and Saudi Arabian dedicated paediatric hospitals. Also, hospitals can achieve a low comparative DRL ranking for some CT protocols (e.g., chest or abdomen/pelvis), but have a high ranking in others (e.g., head). If such internal and external dose differences can occur in dedicated paediatric CT departments, then it can be assumed that with less specific paediatric CT training and protocol development, a greater range of doses will occur in CT departments that only undertake occasional paediatric CT examinations. DRLs should be established for each major CT scan region and specifically for paediatric patients in order to find and correct such dose delivery variation.
The authors are grateful to the heads of the participating radiology departments in the Australian and Saudi Arabian public paediatric hospitals. We also gratefully acknowledge Professor Patrick Brennan of the University of Sydney for his advice on our manuscript, input from Associate Professor Moshi Geso and Associate Professor Giovanni Mandarano of RMIT’s Department of Medical Radiations and Anthony Wallace of ARPANSA, and statistical assistance from Dr. Adrian Schembri and Dr. Anthony Bedford of RMIT’s School of Mathematics and Geospatial Sciences.
Multi-detector computed tomography (MDCT) has improved the ease, and reduced overall examination time, when imaging paediatric patients. If MDCT is not wisely used, the parameters selected may actually provide a high radiation dose to paediatric patients.
Diagnostic reference levels (DRLs) are used for comparison of computed tomography (CT) doses from different hospitals. These can be used to encourage CT departments to reduce radiation dose levels. In this study, the authors have used a number of calculations [including DRLs and dose length products (DLPs)] to compare radiation doses delivered to paediatric patients at dedicated paediatric centres in Australia and Saudi Arabia.
A CT phantom measurement cylinder was provided to paediatric centres. The data collected allowed the authors to compare radiation doses used in paediatric CT examinations. Overall, dedicated paediatric centres in Australia provided less radiation dose for their paediatric CT examinations than those in Saudi Arabia.
The education and training of Australian radiographers were identified and acknowledged as providing an important contribution to understanding of dose minimisation techniques, while maintaining diagnostic image quality. To minimize variations in radiation dose delivered to paediatric patients, it is recommended that DRLs be established for paediatric body regions commonly scanned with CT.
Further to the definition of CT DRL provided in this text, the definitions and understanding of the following will be of benefit in aiding a radiographer to minimize radiation dose to paediatric patients: computed tomography dose index (CTDI), is a calculation based on the absorbed dose in a cylindrical shaped phantom; CTDI volume is the term used to express the radiation dose to a specific volume slice, on a standard phantom; DLP is the CTDI volume multiplied by the length of the scan.
In this work, the authors present a survey of effective doses between hospitals in Saudi Arabia and Australia with the aim of demonstrating the need for the implementation of dose reference levels and continuous education to the staff of the hospital regarding the minimization of dose according to the ALARA principle. The introduction describes the background and aims adequately and the method’s section gives a concise description of the procedure followed in the study. While it does not produce new insights in the matter of radiation protection, it is a good precursor article for setting the context for decision making bodies to improve radiological practices in the sensitive area of pediatric radiology.
Peer reviewer: Panagiotis Antoniou, PhD, MSc, Medical Physics, Certified Medical Physicist, School of Medicine, Democritus University of Thrace, 31 Irinis Str., 68100 Alexandroupolis, Greece
S- Editor Cheng JX L- Editor Logan S E- Editor Xiong L
| 1. | Available from: http://www.crcpd.org/pubs/nexttrifolds/next2000ct_t.pdf. |
| 2. | Brenner DJ, Hall EJ. Computed tomography--an increasing source of radiation exposure. N Engl J Med. 2007;357:2277-2284. [PubMed] |
| 3. | Goske MJ, Applegate KE, Boylan J, Butler PF, Callahan MJ, Coley BD, Farley S, Frush DP, Hernanz-Schulman M, Jaramillo D. The 'Image Gently' campaign: increasing CT radiation dose awareness through a national education and awareness program. Pediatr Radiol. 2008;38:265-269. [PubMed] |
| 4. | Medicare Australia, Group Statistics Reports 2010, Report No. 2. Available from: http://www.medicareaustralia.gov.au/statistics/mbs_group.shtml. |
| 5. | Sources and effects of ionizing radiation. United Nations Scientific Committee on the Effects of Atomic Radiation UNSCEAR 2000 Report to the General Assembly. United Nations Sales Publication E.00.IX.3 and E.00.IX.4. . |
| 6. | Hayton A, Wallace A, Edmonds K, D . T. Trends in Australian CT Statistics 1994–2008. ) IA, editor. 2009; Available from: http://www.conlog.com.au/epsm-abec2009/program.html. |
| 7. | Wise KN, Thomson JEM. The Changes in CT radiation doses in Australia from 1994 to 2002. Radiographer. 2004;51:81. |
| 8. | Schauer DA, Linton OW. NCRP Report No. 160, Ionizing Radiation Exposure of the Population of the United States, medical exposure--are we doing less with more, and is there a role for health physicists? Health Phys. 2009;97:1-5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 346] [Cited by in RCA: 255] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 9. | Lam WWM. Paediatric CT Radiation Risks: What you should know. Medical Bulletin. 2006;11:5-7. |
| 10. | Frush DP, Donnelly LF, Rosen NS. Computed tomography and radiation risks: what pediatric health care providers should know. Pediatrics. 2003;112:951-957. [PubMed] |
| 12. | One size does not fit all: Reducing risks from pediatric CT. ACR Bulletin. 2001;57:20-23. |
| 13. | Pierce DA, Shimizu Y, Preston DL, Vaeth M, Mabuchi K. Studies of the mortality of atomic bomb survivors. report 12, part I. Cancer: 1950-1990. 1996. Radiat Res. 2012;178:AV61-AV87. [PubMed] |
| 14. | Preston DL, Shimizu Y, Pierce DA, Suyama A, Mabuchi K. Studies of mortality of atomic bomb survivors. Report 13: solid cancer and noncancer disease mortality: 1950-1997. 2003. Radiat Res. 2012;178:AV146-AV172. [PubMed] |
| 15. | Huda W. Effective doses to adult and pediatric patients. Pediatr Radiol. 2002;32:272-279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 36] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 16. | Huda W; CEC. European Guidelines on Quality Criteria For Diagnostic Radiographic Images. Brussels: The European Commission 1996; . |
| 17. | Radiological protection and safety in medicine. A report of the International Commission on Radiological Protection. Ann ICRP. 1996;26:1-47. |
| 18. | Radiological protection and safety in medicine. A report of the International Commission on Radiological Protection. Ann ICRP. 1996;26:1-47. [PubMed] |
| 19. | Matthews K, Brennan P. The application of diagnostic reference levels: General principles and an Irish perspective. Radiography. 2009;15:171-178. [RCA] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 20. | Wallace AB. The implementation of diagnostic reference levels to Australian radiology practice. J Med Imaging Radiat Oncol. 2010;54:465-471. [PubMed] |
| 21. | Shrimpton PC, Wall BF, Hart D. Diagnostic medical exposures in the U.K. Appl Radiat Isot. 1999;50:261-269. [PubMed] |
| 22. | User Manual DIADOS PTW Diagnostic Dosemeter T11003. Freiburg, Germany: PTW, 2008. . |
| 23. | Wolfram Mathworld. Outlier. Available from: http: //mathworld.wolfram.com/Outlier.html. |
| 24. | Shrimpton PC, Hillier MC, Lewis MA, Dunn M. National survey of doses from CT in the UK: 2003. Br J Radiol. 2006;79:968-980. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 404] [Cited by in RCA: 422] [Article Influence: 23.4] [Reference Citation Analysis (0)] |
| 25. | Shrimpton PC; ARPANSA. Quarterly Report of the Chief Executive Officer for the period 1 October 2010 to 31 December 2010. Available from: http://www.arpansa.gov.au/pubs/qrpt/qrp_dec10.pdf. |
| 26. | Almohiy H, Sim J, Euclid S, Davidson R. Understanding Pediatric CT Radiation Dose from Radiographers Perception. 16th ISRRT World Congress; Gold Coast, Australia; 9-12 September; Gold Coast Australia: Australian Institute of Radiography 2010; 61. |
| 27. | Almohiy H, Sim J, Euclid S, Davidson R. Knowledge of paediatric CT radiation among Saudi Arabia radiographers. 16th ISRRT World Congress, Gold Coast, Australia; Gold Coast Australia: AIR; 2010; . |
| 28. | Muhogora WE, Nyanda AM, Ngoye WM, Shao D. Radiation doses to patients during selected CT procedures at four hospitals in Tanzania. Eur J Radiol. 2006;57:461-467. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 29. | Shrimpton PC, Edyvean S. CT scanner dosimetry. Br J Radiol. 1998;71:1-3. [PubMed] |
| 30. | Mettler Jr FA. Training Users of Medical Radiation. Available from: http://irpa11.irpa.net/pdfs/KL-4a.pdf. |
| 31. | Mettler Jr FA; IAEA. International Action Plan for the Radiological Protection of Patients. Available from: http://www-ns.iaea.org/downloads/rw/radiation-safety/PatientProtActionPlangov2002-36gc46-12.pdf. |
| 32. | Soye JA, Paterson A. A survey of awareness of radiation dose among health professionals in Northern Ireland. Br J Radiol. 2008;81:725-729. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 102] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 33. | Moss M, McLean D. Paediatric and adult computed tomography practice and patient dose in Australia. Australas Radiol. 2006;50:33-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 31] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 34. | Siegel MJ, Schmidt B, Bradley D, Suess C, Hildebolt C. Radiation dose and image quality in pediatric CT: effect of technical factors and phantom size and shape. Radiology. 2004;233:515-522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 238] [Cited by in RCA: 210] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 35. | Kharita MH, Khazzam S. Survey of patient dose in computed tomography in Syria 2009. Radiat Prot Dosimetry. 2010;141:149-161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 36. | Brix G, Nagel HD, Stamm G, Veit R, Lechel U, Griebel J, Galanski M. Radiation exposure in multi-slice versus single-slice spiral CT: results of a nationwide survey. Eur Radiol. 2003;13:1979-1991. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 125] [Article Influence: 5.7] [Reference Citation Analysis (0)] |