Revised: July 8, 2011
Accepted: July 15, 2011
Published online: January 28, 2012
AIM: To evaluate the effect of non-linear adaptive filters (NLAF) on abdominal computed tomography (CT) images acquired at different radiation dose levels.
METHODS: Nineteen patients (mean age 61.6 ± 7.9 years, M:F = 8:11) gave informed consent for an Institutional Review Board approved prospective study involving acquisition of 4 additional image series (200, 150, 100, 50 mAs and 120 kVp) on a 64 slice multidetector row CT scanner over an identical 10 cm length in the abdomen. The CT images acquired at 150, 100 and 50 mAs were processed with the NLAF. Two radiologists reviewed unprocessed and processed images for image quality in a blinded randomized manner. CT dose index volume, dose length product, patient weight, transverse diameters, objective noise and CT numbers were recorded. Data were analyzed using Analysis of Variance and Wilcoxon signed rank test.
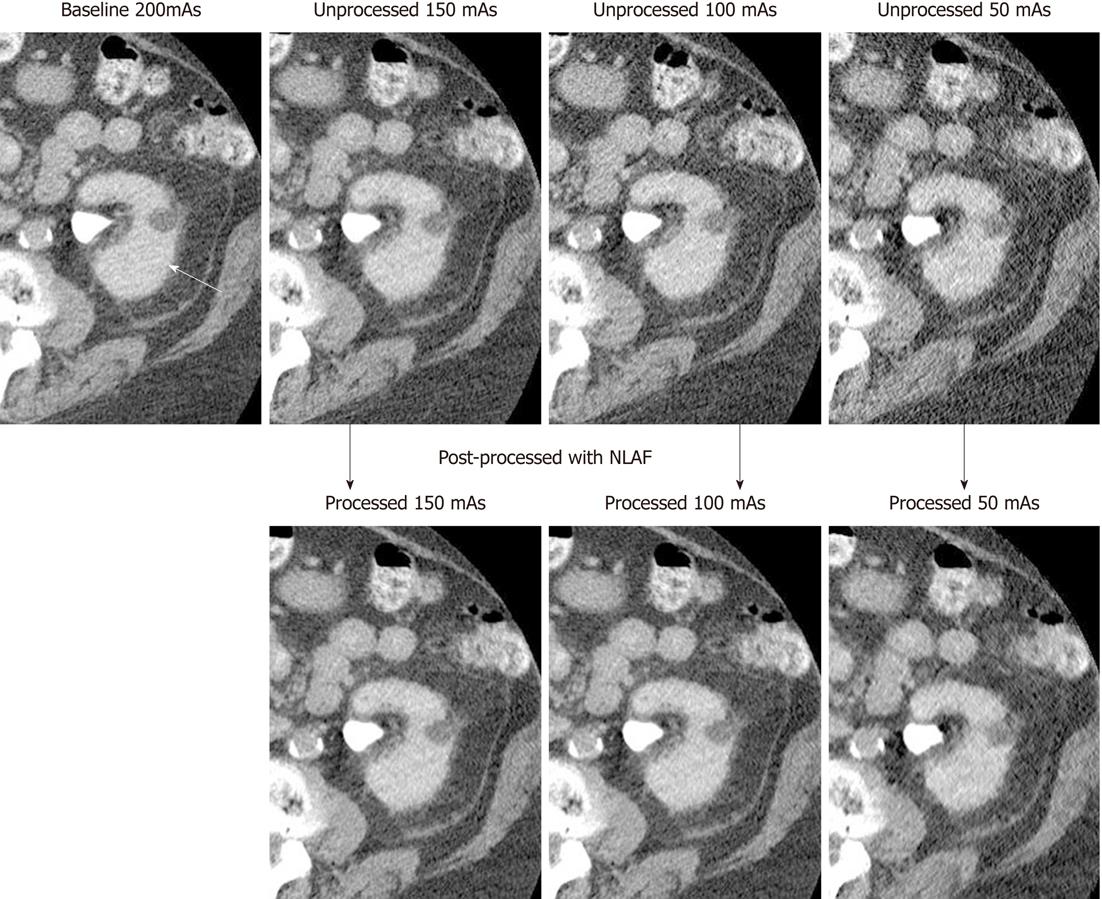
RESULTS: Of the 31 lesions detected in abdominal CT images, 28 lesions were less than 1 cm in size. Subjective image noise was graded as unacceptable in unprocessed images at 50 and 100 mAs, and in NLAF processed images at 50 mAs only. In NLAF processed images, objective image noise was decreased by 21% (14.4 ± 4/18.2 ± 4.9) at 150 mAs, 28.3% (15.7 ± 5.6/21.9 ± 4) at 100 mAs and by 39.4% (18.8 ± 9/30.4 ± 9.2) at 50 mAs compared to unprocessed images acquired at respective radiation dose levels. At 100 mAs the visibility of smaller structures improved from suboptimal in unprocessed images to excellent in NLAF processed images, whereas diagnostic confidence was respectively improved from probably confident to fully confident.
CONCLUSION: NLAF lowers image noise, improves the visibility of small structures and maintains lesion conspicuity at down to 100 mAs for abdominal CT.
- Citation: Singh S, Kalra MK, Sung MK, Back A, Blake MA. Radiation dose reduction with application of non-linear adaptive filters for abdominal CT. World J Radiol 2012; 4(1): 21-28
- URL: https://www.wjgnet.com/1949-8470/full/v4/i1/21.htm
- DOI: https://dx.doi.org/10.4329/wjr.v4.i1.21
As the use of computed tomography (CT) is increasing, with an estimated 62 million scans per year in the United States in the year 2006[1,2], the concerns associated with radiation exposure have also increased in both the news media[3] and the medical literature[4]. The primary concern of radiation dose associated with CT scanning is radiation-induced carcinogenesis. The probability of radiation-induced cancer is directly related to the radiation dose absorbed by tissues and organs and hence the reduction of dose is of paramount importance.
In CT, reduction of dose results in images with larger image noise or mottle and hence raises the possibility of missing lesions or other diagnostic findings. Efforts have been made to reduce radiation dose while maintaining image quality, which have led to several changes in CT hardware and software technologies[5-8]. From the software point of view, image post-processing with linear and non-linear filters have been developed and assessed for lowering image noise and improving or maintaining lesion conspicuity on low dose images[9,10]. Previous clinical studies have reported the use of non-linear image filters for reducing radiation dose for chest and abdominal CT examinations. However, some of these filters lower image noise at the expense of image contrast or visibility of smaller structures[11-13]. New non-linear adaptive filters (NLAF) have been developed and studied using phantom and simulated CT images[14-19].
The purpose of our prospective clinical study was to evaluate the effect of a NLAF on abdominal CT images acquired at different dose levels.
This prospective clinical study was approved by the Human Research Committee of our Institutional Review Board and was conducted in compliance with Health Insurance Portability and Accountability Act guidelines. All 19 patients (mean age 61.6 ± 7.9 years, male:female = 8:11) gave written informed consent for the acquisition of four additional sets of research images for this study, in addition to their standard-of-care, clinically indicated abdominal CT examinations.
The inclusion criteria for the study included: patients scheduled for clinically indicated abdominal CT examinations, older than 50 years, hemodynamic stability (conscious, oriented, regular respiration rate of 12-40 breaths/min, pulse rate of 60-90 bpm without dysrhythmia, systolic blood pressure of 100-140 mmHg), able to provide written informed consent, able to hold breath for a duration of at least 10 s, and able to understand and follow verbal commands for breath-holding and to remain still for the scanning duration.
For all patients included in this study a standard abdominal CT examination was initially performed on a commercially available 64 channel multidetector row CT scanner (Discovery CT750 HD, GE Healthcare, Waukesha, WI.) with administration of an intravenous contrast medium (80-100 mL of Iopamidol 370 mg % Bracco Diagnostics, Princeton, NJ). Subsequently, four additional sets of images were acquired in each patient, through an identical scan length of 10 cm in the abdomen. Selection of the location of the acquisition of these additional image datasets was based on review (by Singh S) of the patient’s prior (available and reviewed in 18/19 patients) and current routine (reviewed in 1/19 patients) abdominal CT images to select the most subtle (first preference) or smallest (second preference) lesion in the abdomen. These research image data sets were thus acquired through the most subtle or smallest abdominal lesion immediately after acquisition of standard-of-care abdominal CT images. The maximum time period between the standard-of-care abdominal CT and the research image acquisition was less than 15-30 s. As all research scan series were planned prior to the acquisition of standard-of-care CT images, the maximum interval between the acquisition of the four different research image series was approximately 10 s.
Abdominal CT images were acquired at four different levels of radiation dose by selecting four different fixed tube current-time products (200, 150, 100 and 50 mAs) for abdominal CT. The acquisition sequence of the four research CT datasets was randomized in order to avoid contrast enhancement bias due to the delay in scanning from start of injection. No additional intravenous contrast medium was administered for acquisition of the research image series since it is not feasible to inject contrast media four times to a patient for acquiring images at identical contrast enhancement phase.
With the exception of tube current, reconstruction kernel and section thickness were held constant and included 120 kVp, 0.984:1 pitch, 39.37 mm table speed per gantry rotation, helical acquisition mode, 64 * 0.625 mm detector configuration and 0.5 s gantry rotation time. All image series were reconstructed at 5 mm section thickness and 5 mm section interval using standard reconstruction kernel as per our routine abdominal CT protocol.
Technical details of the NLAF (ContextVision AB, Linkoping, Sweden) used in our study are described in Appendix 1.
Of the 4 additional research abdominal series (acquired at 200, 150, 100, 50 mAs), three lower dose image series (150, 100 and 50 mAs) were processed with NLAF. For post processing with NLAF, the DICOM image series were de-identified and exported to an external USB storage media. These DICOM image series were processed with NLAF to generate six series (three low dose unprocessed series and three NLAF processed image series). The image processing time with NLAF for image series was less than 2 s. Thus, 7 CT image series were available for evaluation (unprocessed 200, 150, 100, 50 mAs and processed 150, 100, 50 mAs) in each patient. Unprocessed images at 200 mAs were used as standard of reference for lesion detection and image quality assessment.
Each image data set was coded, de-identified and randomized on Microsoft EXCEL 2003 (© Microsoft Corporation, Redmond, WA) by a study co-author (Singh S) to enable double blinded evaluation.
All CT image series were reviewed on a Picture Archiving and Communication System diagnostic workstation (AGFA Impax ES, AGFA Technical Imaging Systems, Ridgefield Park, NJ, USA) for assessment of subjective image quality in a randomized manner. All abdominal CT image series were presented to two experienced abdominal radiologists (MAB with 12 years and MKK with 8 years of experience, respectively) for evaluation of image quality. Both radiologists were trained on two image datasets for the grading of different aspects of subjective image quality as well as lesion assessment in order to understand the evaluation system, in addition to improving inter-observer agreement.
Subjective image quality was assessed in terms of subjective image noise on a five point scale (1 = minimal image noise, 2 = less than average noise, 3 = average image noise, 4 = above average noise, 5 = unacceptable image noise). Visibility of smaller structures for abdominal CT (small blood vessels, adrenal glands, small lymph nodes, ducts and walls of hollow structures) was ranked on a five point scale (1 = excellent visualization, 2 = above average visibility, 3 = acceptable visibility, 4 = suboptimal visibility, and 5 = unacceptable visualization of small structures) using abdominal soft tissue window width 400 HU and window level 40 HU. Artifacts were graded on a four point scale (1 = no artifacts; 2 = minor artifacts not interfering with diagnostic decision making; 3 = major artifacts affecting visualization of major structures, diagnosis still possible; 4 = artifacts affecting diagnostic information), while each type of the following artifacts was assessed (helical or windmill artifacts; streak artifacts due to metals and leads; beam hardening artifacts due to arms by body side; rarely, large body size and truncation due to large body size or off centering, and blotchy pixilated appearance). Lesion size was measured on a four point scale (1 = focal and less than 1 cm, 2 = focal and 1-5 cm, 3 = focal and more than 5 cm, 4 = diffuse lesion), lesion conspicuity was assessed on a five point scale (1 = well-seen lesion with well-visualized margins, 2 = well-seen lesion with poorly visualized margins, 3 = subtle lesions, 4 = probably an artifact mimicking a lesion and 5 = definite artifact mimicking a lesion) and diagnostic confidence (1 = completely confident, 2 = probably confident, 3 = confident only for limited clinical situations such as kidney stones, calcified lesions or a large lesion, and 4 = poor confidence). Image quality attributes assessed in our study have been described in the European Guidelines on Quality Criteria for Computerized Tomography document (EUR 16262 http://www.drs.dk/guidelines/ct/quality/index.htm) and have been used in multiple prior studies in the radiology literature[7,20-22].
Radiologists were first asked to assess the subjective image noise in the seven image sets of each patient (unprocessed and NLAF processed) and then to assess lesion detection starting from the image series with the highest image noise to avoid bias in lesion detection and characterization.
Each subject was weighed on a digital weighing machine just prior to the abdominal CT examination. Circular regions of interest (20-30 mm in diameter) were drawn in the homogenous area of the right lobe of liver. Circular regions of interest (20-30 mm in diameter) were also drawn in the abdominal aorta, without touching the lumen walls, to cover at least two thirds of its lumen. The skin-to-skin maximum transverse diameter of abdomen was measured from localizer radiographs, as transverse images are often reconstructed with a smaller field of view and may not include the skin. Objective image noise (standard deviation) and CT numbers (HU) were measured for all 133 CT image series.
CT radiation dose descriptors such as CT dose index volume (CTDIvol, described in mGy) and dose length product (DLP, described in mGy.cm) were recorded from the dose page following completion of the abdominal CT examination for all image series.
Data were analyzed using analysis of variance (ANOVA) and Wilcoxon signed rank test. Intraobserver variability was not estimated as each radiologist assessed the images only once. Interobserver variability was estimated using both κ statistics as well as percentage agreement between the two radiologists for each of the assessed subjective image quality and lesion assessment parameters.
There was variable interobserver agreement between the two radiologists (κ = 0.2-1) for abdominal CT. However, the percentage agreement between the two radiologists ranged from 68.4% (13/19 scores with agreement for visibility of smaller structures) to 100% (19/19 scores in perfect agreement for criteria such as image noise, lesion conspicuity and diagnostic confidence) for the abdominal CT.
Detailed subjective lesion detection and image quality scores are summarized in Table 1.
| Baseline (200 mAs) | Unpro (150 mAs) | Pro (150 mAs) | Unpro (100 mAs) | Pro (100 mAs) | Unpro (50 mAs) | Pro (50 mAs) | |
| No. of lesions | 31 | 31 | 31 | 31 | 31 | 31 | 31 |
| Lesion size (< 1 cm) | 28 | 28 | 28 | 28 | 28 | 28 | 28 |
| Lesion conspicuity | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Image noise | 2 | 3 | 2 | 4 | 2 | 5 | 4 |
| Visibility of small structures | 3 | 3 | 3 | 4 | 3 | 4 | 4 |
| Image contrast | 3 | 3 | 3 | 3 | 3 | 3 | 3 |
| Diagnostic confidence | 1 | 1 | 1 | 2 | 1 | 4 | 3 |
All 31 abdominal lesions detected in 19 patients were seen on both unprocessed and NLAF processed image series at all tube current-time product levels. Twenty-eight lesions (28/31, 90%) were less than 1 cm in maximum dimension and 2 (2/31, 6%) lesions measured 1-5 cm in maximum dimension. Detected lesions included renal cysts and masses (n = 7 lesions), abdominal lymph nodes (n = 5), adrenal lesions (n = 4), gall bladder stones (n = 3), focal liver lesions (n = 2), peri-renal stranding (n = 2), cholecystectomy (n = 1), minimal ascites (n = 1), surgical clip (n = 1), IVC graft (n = 1), peri IVC soft tissue stranding (n = 1), splenic calcification (n = 1), calcified atherosclerotic plaque (n = 1) and hydronephrosis (n = 1).
Subjective image noise was unacceptable in unprocessed images at 50 and 100 mAs. With NLAF processing, noise was lowered to below average or acceptable at 100 mAs (P < 0.0001) but at 50 mAs was still rated as unacceptable (Figure 1). At 50 mAs, abdominal CT images processed with NLAF were still rated as unacceptable. Visibility of smaller structures, such as small blood vessels, small lymph nodes, ducts or walls of hollow organs, was found to be suboptimal in unprocessed image series at 100 mAs and was improved to acceptable in processed image series. No major artifacts were seen on any of the NLAF processed CT images. Minor beam hardening or photon starvation artifacts were noted in both unprocessed and processed image series in 5 out of 19 image series at 50 and 100 mAs. These artifacts were minor and did not interfere with diagnostic confidence. Diagnostic confidence was suboptimal on unprocessed images at 100 mAs and it improved to fully acceptable in NLAF processed image series at 100 mAs. At 50 mAs both unprocessed and processed images were rated as unacceptable for diagnostic confidence. Weight distribution of subjects with acceptable and unacceptable image noise in both unprocessed and processed images is summarized in Table 2.
| Baseline (200 mAs) | Unpro (150 mAs) | Pro (150 mAs) | Unpro (100 mAs) | Pro (100 mAs) | Unpro (50 mAs) | Pro (50 mAs) | |
| Liver | |||||||
| Objective noise | 15.5 ± 3.9 | 18.2 ± 4.9 | 14.4 ± 4.0 | 21.9 ± 5.6 | 15.7 ± 4.0 | 30.4 ± 9.2 | 18.8 ± 5.0 |
| HU values | 70.9 ± 15.0 | 70.5 ± 16.9 | 70.6 ± 16.0 | 71.2 ± 16.0 | 71.0 ± 16.0 | 70.1 ± 16.0 | 70.1 ± 16.0 |
| Abdominal Aorta | |||||||
| Objective noise | 17.4 ± 4.2 | 20.5 ± 5.4 | 16.0 ± 3.8 | 24.8 ± 6.2 | 18.5 ± 4.2 | 34.3 ± 9.3 | 22.0 ± 6.0 |
| HU values | 80.5 ± 29.0 | 81.6 ± 37.0 | 81.5 ± 31.0 | 82.0 ± 33.7 | 82.1 ± 33.0 | 80.3 ± 31.0 | 80.0 ± 31.0 |
Detailed objective image quality scores for abdominal CT have been summarized in Table 3. Average objective image noise (± standard deviation of the average) in the liver was decreased by 21% (14.4 ± 4/18.2 ± 4.9) at 150 mAs, by 29% (15.7 ± 4/21.9 ± 5.6) at 100 mAs and by 39.4% (18.8 ± 5.7/30.4 ± 9.2) at 50 mAs processed images as compared to unprocessed image series at corresponding mAs levels (P < 0.0001), whereas in the abdominal aorta noise decreased by 22% (16 ± 3.8/20.5 ± 5.4) at 150 mAs, by 26% (18.5 ± 4.2/24.8 ± 6.2) at 100 mAs and by 38% (22 ± 6/34.3 ± 9.3) at 50 mAs processed images (P < 0.0001).
| Unprocessed images | Processed images | |||
| Acceptable noise | Unacceptable noise | Acceptable noise | Unacceptable noise | |
| 150 mAs | 14/19 | 5/19 | 19/19 | 0/19 |
| Weight (kg) | 74.5 ± 14.8 | 95.2 ± 11.1 | 79.9 ± 16.5 | - |
| Transverse diameter (cm) | 34.2 ± 4.3 | 42.9 ± 4.5 | 36.5 ± 5.8 | - |
| 100 mAs | 4/19 | 15/19 | 17/19 | 2/19 |
| Weight (kg) | 77.1 ± 4.0 | 80.7 ± 18.6 | 76.9 ± 14.6 | 106.0 ± 4.3 |
| Transverse diameter (cm) | 32.5 ± 3.5 | 37.6 ± 5.9 | 35.7 ± 5.6 | 43.5 ± 0.7 |
| 50 mAs | 0/19 | 19/19 | 5/19 | 14/19 |
| Weight (kg) | - | 79.9 ± 16.5 | 66.2 ± 13.0 | 91.4 ± 15.1 |
| Transverse diameter (cm) | - | 36.5 ± 5.8 | 33.0 ± 3.4 | 40.6 ± 6.1 |
There was no significant change in the average CT number (for liver and aorta) in unprocessed and processed abdominal CT image series (P > 0.05).
CTDIvol for abdominal CT image series at 200 mAs, 150 mAs, 100 mAs and 50 mAs were 16.8, 12.6, 8.4, 4.2 mGy, respectively. The respective DLP values were 245.6, 141.8, 95.7, and 49.7 mGy-cm.
Since lowering of radiation dose increases the image noise, an approach to reduce radiation dose associated with CT is to post process low dose noisy images in order to lower image noise and enhance diagnostic confidence. In the CT source data domain, users can change the CT image reconstruction technique; for example, filtered back projection with smoother or sharper reconstruction kernel. Use of smoother kernel does entail some loss of spatial resolution or image sharpness, whereas use of sharper kernels increases image noise at the expense of higher spatial resolution and improved image sharpness. Recent studies and commercial release of iterative reconstruction techniques allows scanning at lower radiation dose, as these techniques provide images with less image noise[21-23]. However, presently these iterative reconstruction techniques are somewhat slower in reconstruction time and are only available on the latest high end (64 slices or higher) CT scanners with substantial cost increments for both hardware and software upgrades. On the other hand, image post processing filters have also been developed to lower image noise[12-14]. These filters work in the DICOM image space domain and are less computationally intense compared to the iterative reconstruction techniques. Unlike the iterative reconstruction techniques, which are applied to the CT scanner user interface, NLAF used in our study is a server-based application that identifies and processes low dose CT images automatically as they transit from CT user interface to the PACS network. To the best of our knowledge, there is no head to head comparison available to date between the iterative reconstruction techniques and the image post-processing filters.
Different types of image post processing filters have been used to reduce image noise in low radiation dose CT images[12-14]. We used a NLAF for the purpose of our study. For abdominal CT images, NLAF post processing of 100 mAs image series changed image noise to acceptable from unacceptable in unprocessed images. However at 50 mAs, both processed and unprocessed images were found to be suboptimal. Lowering of image noise with NLAF did not affect the image contrast or lesion conspicuity in abdominal CT images. This trend was confirmed with objective image noise measurements in abdominal CT images. In addition to lowering of image noise, NLAF enhanced the visibility of smaller structures at 100 mAs. Our results are in contradiction to prior non-linear filters described by Kalra et al[11-13]. Contrary to the loss of visibility of small structures and demeaned lesion conspicuity noted on prior studies, NLAF used in our study was not associated with these disadvantages. Hence, application of NLAF in abdominal CT allows radiation dose reduction while maintaining constant image quality and diagnostic confidence.
Our findings are consistent with those reported in a phantom study performed by Funama et al[14], who found that 80 to 100 mAs images were acceptable following post processing with a different vendor’s NLAF. We believe that the inherently high contrast in the chest from air and fat helped in achieving greater dose reduction with NLAF. In another study, Funama et al[19] found that adaptive filters can improve image noise and diagnostic acceptability of abdominal CT images acquired at 60 to100 mAs based on the size of the patients. We also noted that 5/19 abdominal CT images acquired at 50 mAs in subjects weighing less than 66 kg were acceptable, whereas the subjects with unacceptable image quality at 50 mAs were considerably heavier (weight greater than 91 kg) (P < 0.0001).
Results of our study are also in agreement with Kröpil et al[18], who used the same NLAF as in our study to post process simulated upper abdomen MDCT phantom images and found that 50% radiation dose reduction is possible with post processing. We also found that image noise in 100 mAs abdominal CT images following post processing is similar to image noise in unprocessed 200 mAs images. Our results are also similar to another phantom study from Martinsen et al[15], also using the same NLAF, which showed acceptable lowering of tube current-time product down to only 112 mAs for detection of 2 mm-7 mm simulated liver lesions.
Our study has limitations. Foremost, the small sample size of our study is due to the difficulty in recruiting patients, which could be due to many reasons, such as rising concern of radiation-induced cancer. Another limitation of our study is that we did not use automatic exposure technique to evaluate the effect of NLAF on radiation dose reduction, although automatic exposure control techniques are routinely used for dose modulation in routine clinical practice. We used fixed tube current settings to reduce radiation dose for the following reasons: firstly, to obtain four levels of radiation dose with automatic exposure control, we would have been required to adjust the noise index (desired image noise for adjusting tube current) and minimum and maximum tube current for each dose level as well as for different patient size, as automatic exposure control would have increased radiation dose to larger subjects and decreased the radiation dose for slimmer subjects. To further complicate the matter, change in radiation dose with automatic exposure control is non-linear to the body size in order to avoid inadvertent use of high tube currents in larger subjects and too low tube currents in slimmer subjects.
Also, we did not investigate the effect of NLAF post processing in patients of different sizes due to our small sample size. Although it is very difficult to blind the experienced radiologist between unprocessed and processed images due to differences in image noise, we randomized the image sets acquired at varying dose levels (16.8-4.2 mGy). Another possible limitation of our study is the fact that CT images were acquired in equilibrium phase and not in non-contrast or dynamic phase. An additional consideration with our study is the fact that we used 4 image datasets of each patient at four different radiation dose levels and this repetitive reviewing of images may have biased the radiologists for the lesion conspicuity assessment component of our study. However, in order to minimize this bias in image assessment, each radiologist was asked separately to first assess the lesion conspicuity on the image series with the greatest image noise or those image datasets acquired at lowest dose levels and then assess the other dose levels. Although NLAF works on DICOM images from all vendors, we did not perform side by side comparisons for the role of NLAF on CT images from other vendors. Also, we did not compare NLAF filters with other available commercial CT image filters.
Implications of our study include potential for reducing radiation dose by 50% with the application of NLAF as used in our study. Further studies will however be needed to determine the actual noise reduction effect of NLAF on patients of different sizes, in particular for large patients.
In conclusion, substantial CT radiation dose reduction is feasible for abdominal CT images (down to 100 mAs) following processing with NLAF.
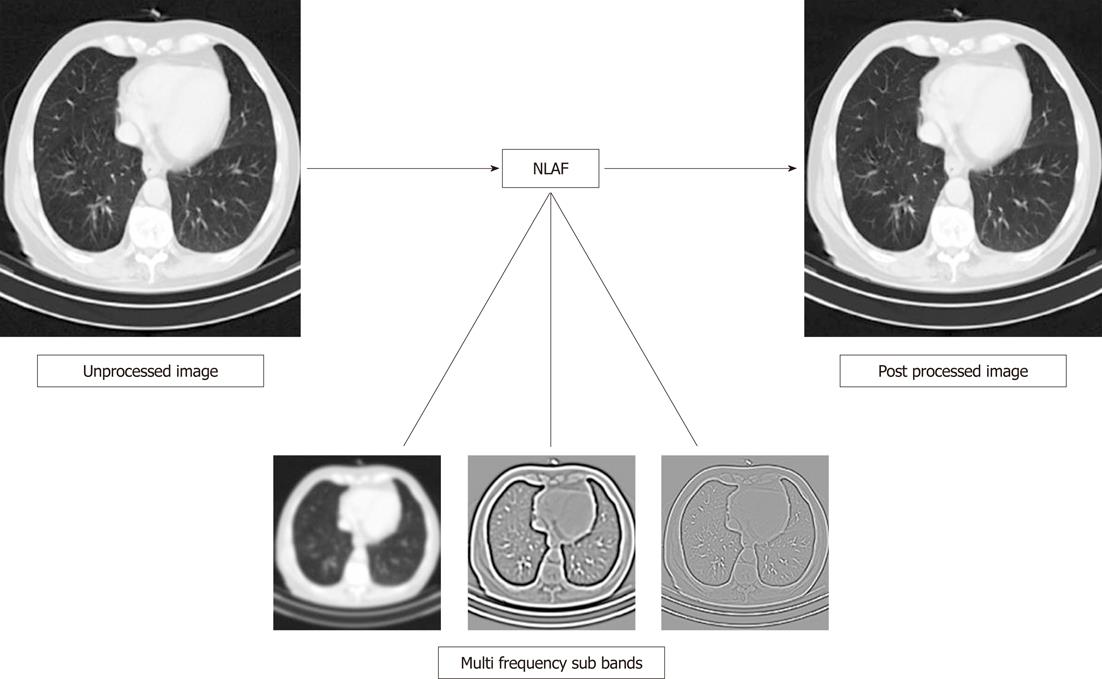
The two dimensional NLAF used in this study are based on the General Operator Processor technology[24]. The algorithm divides the data into several frequency bands that are processed separately and then re-combined. The number of frequency bands varies between cases, depending on the scanner and anatomy of intent (as described in Figure 2, where chest image has been parsed into three frequency bands). Each band usually contains similar size structures, which allows it to process anatomical structures by size. The low-pass band on the left consists mainly of the amplitude of the 2D signal and low frequent variations. The high-pass band contains predominantly small structures and noise. The remaining band cover structures of mid size and low frequency noise. After processing each frequency band, NLAF adaptively combines the enhanced bands to yield a resultant filtered image.
During the filter’s hierarchical process, each pixel is examined in relation to its surroundings. Local features are estimated by using a set of filters in different directions. The filters are designed so that the combined filter response is completely rotational invariant. During the analysis of the filter responses a number of simple, complex and hypercomplex features are estimated. These features can be for example variance, orientation, phase, energy and curvature. When a local NLAF feature has been estimated, the feature is estimated also on a higher abstraction level to get robust results for the neighbourhood. From this information one can decide if the pixel is part of the same structure as its neighbours. Moreover, certainty values on the feature estimations are always generated to further obtain robust results. One example is two crossing lines where there is high signal energy in the crossing point but low certainty on orientation since there is more than one orientation present.
The compiled set of these features forms the contextual information for every location in the image. This contextual information is fused to generate a specific filtering method, which adapts to the image signal in every location and individually optimizes each pixel. The unique nature of NLAF is the possibility of adapting desired behavior to the image content, allowing for simultaneous noise reduction and edge enhancement. For example, edge enhancement in high frequency areas such as lung and bones, and selective noise reduction in other soft tissue regions within a single image. Finally, the parameters may be adjusted for the anatomical region scanned, as for example the abdominal CT images (more noise reduction or smoothing is required) need different parameters than those needed in chest images (where greater edge enhancement with limited smoothing is required). The enhancement is performed in different intensity value ranges, corresponding to tissue-type-specific Hounsfield Units. Also these parameters can be adjusted based on user preference, as some radiologists prefer smooth images while others prefer sharp, crisp images.
As the use of computed tomography (CT) is increasing, with an estimated 62 million scans per year in the United States in the year 2006, the concerns associated with radiation exposure have also increased in both the news media and the medical literature. The primary concern of radiation dose associated with CT scanning is radiation-induced carcinogenesis. The probability of radiation-induced cancer is directly related to the radiation dose absorbed by tissues and organs and hence the reduction of dose is of paramount importance. In CT, reduction of dose results in images with larger image noise or mottle and hence raises the possibility of missing lesions or other diagnostic findings. Efforts have been made to reduce radiation dose while maintaining image quality which have led to several changes in CT hardware and software technologies. From the software point of view, image post processing with linear and non-linear filters have been developed and assessed for lowering image noise and improving or maintaining lesion conspicuity on low dose images. Previous clinical studies have reported the use of non-linear image filters for reducing radiation dose for chest and abdominal CT examinations. However, some of these filters lower image noise at the expense of image contrast or visibility of smaller structures. New non-linear adaptive filters (NLAF) have been developed and studied using phantom and simulated CT images.
Substantial CT radiation dose reduction is feasible for abdominal CT images (down to 100 mAs) following processing with NLAF.
Implications of our study include potential for reducing radiation dose by 50% with the application of NLAF as used in our study. Further studies will however be needed to determine the actual noise reduction effect of NLAF on patients of different sizes, in particular for large patients.
This study presents the results of the application of NLAF software to abdominal CT images and demonstrates the prospect of dose reduction that can be achieved with the use of such filters. Overall, this is a very good paper. It is well designed, well implemented and well analyzed.
Peer reviewers: Ioannis Tsalafoutas, PhD, Medical Physics Department, Anticancer Hospital “Agios Savvas”, 171 Alexandras Avenue, 115 22 Athens, Greece; Wazir Muhammad, PhD, Nuclear Energy Application Laboratory, Department of Physics, Kyungpook National University, Sankuk-dong, Buk-gu, Daegu 702-701, South Korea
S- Editor Cheng JX L- Editor Logan S E- Editor Zheng XM
| 1. | Department of Health and Human Services. What's NEXT?. Nationwide Evaluation of X-ray Trends: 2000 computed tomography. (CRCPD publication no. NEXT_2000CT-T.) Conference of Radiation Control Program Directors 2006; . |
| 2. | Medical Information Division. IMV 2006 CT Market Summary Report. Des Plains, IL: IMV Medical Information Division 2006; . |
| 3. | Guthrie C. How dangerous are CT scans? Time Magazine. New York: Time Inc 2008; Available from: http://www.time.com/time/health/article/0,8599,1818520,00.html on January 17th 2011. |
| 4. | Brenner DJ, Hall EJ. Computed tomography--an increasing source of radiation exposure. N Engl J Med. 2007;357:2277-2284. [PubMed] |
| 5. | Kalra MK, Maher MM, Toth TL, Hamberg LM, Blake MA, Shepard JA, Saini S. Strategies for CT radiation dose optimization. Radiology. 2004;230:619-628. [PubMed] |
| 6. | Rizzo S, Kalra M, Schmidt B, Dalal T, Suess C, Flohr T, Blake M, Saini S. Comparison of angular and combined automatic tube current modulation techniques with constant tube current CT of the abdomen and pelvis. AJR Am J Roentgenol. 2006;186:673-679. [PubMed] |
| 7. | Singh S, Kalra MK, Moore MA, Shailam R, Liu B, Toth TL, Grant E, Westra SJ. Dose reduction and compliance with pediatric CT protocols adapted to patient size, clinical indication, and number of prior studies. Radiology. 2009;252:200-208. [PubMed] |
| 8. | Cohnen M, Fischer H, Hamacher J, Lins E, Kötter R, Mödder U. CT of the head by use of reduced current and kilovoltage: relationship between image quality and dose reduction. AJNR Am J Neuroradiol. 2000;21:1654-1660. [PubMed] |
| 9. | Keselbrener L, Shimoni Y, Akselrod S. Nonlinear filters applied on computerized axial tomography: theory and phantom images. Med Phys. 1992;19:1057-1064. [PubMed] |
| 10. | Alvarez RE, Stonestrom JP. Optimal processing of computed tomography images using experimentally measured noise properties. J Comput Assist Tomogr. 1979;3:77-84. [PubMed] |
| 11. | Kalra MK, Maher MM, Sahani DV, Blake MA, Hahn PF, Avinash GB, Toth TL, Halpern E, Saini S. Low-dose CT of the abdomen: evaluation of image improvement with use of noise reduction filters pilot study. Radiology. 2003;228:251-256. [PubMed] |
| 12. | Rizzo SM, Kalra MK, Schmidt B, Raupach R, Maher MM, Blake MA, Saini S. CT images of abdomen and pelvis: effect of nonlinear three-dimensional optimized reconstruction algorithm on image quality and lesion characteristics. Radiology. 2005;237:309-315. [PubMed] |
| 13. | Kalra MK, Maher MM, Blake MA, Lucey BC, Karau K, Toth TL, Avinash G, Halpern EF, Saini S. Detection and characterization of lesions on low-radiation-dose abdominal CT images postprocessed with noise reduction filters. Radiology. 2004;232:791-797. [PubMed] |
| 14. | Funama Y, Awai K, Miyazaki O, Nakayama Y, Goto T, Omi Y, Shimonobo T, Liu D, Yamashita Y, Hori S. Improvement of low-contrast detectability in low-dose hepatic multidetector computed tomography using a novel adaptive filter: evaluation with a computer-simulated liver including tumors. Invest Radiol. 2006;41:1-7. [PubMed] |
| 15. | Martinsen AC, Saether HK, Olsen DR, Skaane P, Olerud HM. Reduction in dose from CT examinations of liver lesions with a new postprocessing filter: a ROC phantom study. Acta Radiol. 2008;49:303-309. [PubMed] |
| 16. | Okumura M, Ota T, Tsukagoshi S, Katada K. New method of evaluating edge-preserving adaptive filters for computed tomography (CT): digital phantom method. Nihon Hoshasen Gijutsu Gakkai Zasshi. 2006;62:971-978. [PubMed] |
| 17. | Sato K, Goto M, Ishiya H, Oshita R, Mori I, Yanagawa I. [Evaluation of non-linear adaptive smoothing filter by digital phantom]. Nihon Hoshasen Gijutsu Gakkai Zasshi. 2008;64:434-441. [PubMed] |
| 18. | Kröpil P, Lanzman RS, Walther C, Röhlen S, Godehardt E, Mödder U, Cohnen M. [Dose reduction and image quality in MDCT of the upper abdomen: potential of an adaptive post-processing filter]. Rofo. 2010;182:248-253. [PubMed] |
| 19. | Funama Y, Awai K, Miyazaki O, Goto T, Nakayama Y, Shimamura M, Hiraishi K, Hori S, Yamashita Y. Radiation dose reduction in hepatic multidetector computed tomography with a novel adaptive noise reduction filter. Radiat Med. 2008;26:171-177. [PubMed] |
| 20. | EUR 16262. European guidelines on quality criteria for computed tomography. Available from: http://www.drs.dk/guidelines/ct/quality. |
| 21. | Singh S, Kalra MK, Gilman MD, Hsieh J, Pien HH, Digumarthy SR, Shepard JA. Adaptive statistical iterative reconstruction technique for radiation dose reduction in chest CT: a pilot study. Radiology. 2011;259:565-573. [PubMed] |
| 22. | Singh S, Kalra MK, Hsieh J, Licato PE, Do S, Pien HH, Blake MA. Abdominal CT: comparison of adaptive statistical iterative and filtered back projection reconstruction techniques. Radiology. 2010;257:373-383. [PubMed] |
| 23. | Funama Y, Taguchi K, Utsunomiya D, Oda S, Yanaga Y, Yamashita Y, Awai K. Combination of a low-tube-voltage technique with hybrid iterative reconstruction (iDose) algorithm at coronary computed tomographic angiography. J Comput Assist Tomogr. 2011;35:480-485. |
| 24. | Granlund GH. Granlund. In search of a general picture processing operator. Comput Graph Image Process. 1978;8:155-173. |