Published online Sep 28, 2011. doi: 10.4329/wjr.v3.i9.224
Revised: July 28, 2011
Accepted: August 4, 2011
Published online: September 28, 2011
The glenohumeral joint is the most commonly dislocated joint of the body and anterior instability is the most common type of shoulder instability. Magnetic resonance (MR) imaging, and more recently, MR arthrography, have become the essential investigation modalities of glenohumeral instability, especially for pre-procedure evaluation before arthroscopic surgery. Injuries associated with glenohumeral instability are variable, and can involve the bones, the labor-ligamentous components, or the rotator cuff. Anterior instability is associated with injuries of the anterior labrum and the anterior band of the inferior glenohumeral ligament, in the form of Bankart lesion and its variants; whereas posterior instability is associated with reverse Bankart and reverse Hill-Sachs lesion. Multidirectional instability often has no labral pathology on imaging but shows specific osseous changes such as increased chondrolabral retroversion. This article reviews the relevant anatomy in brief, the MR imaging technique and the arthrographic technique, and describes the MR findings in each type of instability as well as common imaging pitfalls.
- Citation: Jana M, Gamanagatti S. Magnetic resonance imaging in glenohumeral instability. World J Radiol 2011; 3(9): 224-232
- URL: https://www.wjgnet.com/1949-8470/full/v3/i9/224.htm
- DOI: https://dx.doi.org/10.4329/wjr.v3.i9.224
Shoulder joint is the most mobile and most commonly dislocated joint of the body[1]. Injuries to this joint leading to dislocation, subluxation and fracture are common, especially in young active individuals. Glenohumeral instability can be classified differently (Table 1) based on the etiopathogenesis (traumatic or atraumatic), direction of dislocation (anterior or posterior) or chronicity (acute or chronic). Traumatic anterior instability (often represented by the term TUBS; Traumatic, Unidirectional, Bankart, Surgical) is the most common clinical entity compared to atraumatic multidirectional instability[1]. Anterior dislocation comprises the majority (95%) of all cases; whereas posterior dislocation is less common[1].
| Classification | Types of instability |
| Anatomic | Anterior |
| Posterior | |
| Multidirectional | |
| Etiologic | Traumatic (TUBS) |
| Atraumatic (AMBRI) | |
| Clinical course | Acute |
| Recurrent | |
| Degree of instability | Subluxation |
| Dislocation |
In this article, we will review the anatomy, the magnetic resonance imaging (MRI) techniques and recent advancements in imaging of glenohumeral instability, and commonly encountered abnormalities in glenohumeral instability.
The shoulder girdle is comprised of three joints, the glenohumeral joint, the acromioclavicular joint and the sternoclavicular joint. The glenohumeral joint, a ball- and socket type of joint, is the main component of the shoulder girdle mechanism[1]. The glenoid labrum is a fibrocartilage located at the glenoid rim which increases the depth by 2-4 mm (50%)[2] and increases the articular surface of the socket by 1 cm. Normal glenoid labrum appears as a triangular structure at the glenoid margin, having hypointense signal intensity on all sequences (Figure 1)[1]. Principal stabilizing mechanisms of the shoulder joint are the rotator cuff tendons (dynamic stabilizers) and the glenoid labrum and the ligaments (static stabilizers)[2]. The rotator cuff tendons are comprised of four tendons arranged around the shoulder girdle: the subscapularis, supraspinatus, infraspinatus, and teres minor. Normal tendons appear hypointense on T1-weighted (T1W) as well as T2-weighted (T2W) images[1,2].
Glenohumeral ligaments (superior, middle and inferior) are thickenings of the capsule of the glenohumeral joint. Normal glenohumeral ligaments appear as hypointense linear bands, best documented after joint distension on magnetic resonance (MR) arthrography (Figures 2-4). The inferior glenohumeral ligament (IGHL) is made up of two components, the anterior and the posterior bands[1,2]. The anterior band of the IGHL is of prime importance in the stability of the shoulder joint. The anterior inferior labrum and the anterior band of the IGHL are better visualized on oblique axial scan with the shoulder in abduction and external rotation (ABER)[3,4]. Inferior labral-ligamentous abnormalities have been reported to be most closely correlated with anterior glenohumeral instability[5].
The attachment of the anterior joint capsule and middle glenohumeral ligament (MGHL) shows significant variability. Three types of attachment have been described: type I refers to an attachment of the anterior joint capsule at the anterior labral tip or at the base of the labrum; in type II attachment, the capsule attaches to the glenoid close to the labral base; whereas type III refers to an attachment more medially along the scapular neck (Figure 5)[6].
Rotator cuff interval (RCI) is defined as the discontinuity of the rotator cuff that occurs between the superior border of the subscapularis and the anterior border of the supraspinatus tendon (Figure 6). Structural insufficiency of its components and the overlying capsule caused by trauma can result in instability[7].
The long head of biceps tendon, after its origin from the supraglenoid tubercle, traverses a long intra-articular course through the superior part of the joint and the RCI before coursing through the bicipital groove. In cranial axial sections, it is seen as a linear hypointense structure coursing parallel to the superior glenohumeral ligament (SGHL) (Figure 2).
Routine imaging of the shoulder is done in three planes. The acquisition of images in the oblique coronal plane, which is the single most important imaging plane in the shoulder joint, is done parallel to the supraspinatus tendon. Oblique sagittal images are acquired at a plane perpendicular to the plane of the glenoid face, and best planned on an axial image[1].
Articular cartilage and labrum are best evaluated on a proton density (PD) or gradient echo image on axial and oblique coronal planes. The rotator cuff tendons should be evaluated on oblique coronal and oblique sagittal planes. For evaluation of the signal intensity of the rotator cuff tendons, T2W fat-saturated images are ideal[1,2]. On oblique sagittal images, the entire rotator cuff tendons, muscles and RCI can be assessed. In the setting of trauma, T1W images are less helpful, and can be acquired in oblique coronal plane only[1].
MR arthrography has proven its utility in the evaluation of glenohumeral instability and cartilage abnormalities. MR arthrography can either be direct or indirect (Table 2). Direct MR arthrography procedure can be divided into two parts: injection of the dilute gadolinium contrast agent into the joint and imaging in a MR scanner. Usually fat-saturated T1W images are obtained in all three planes. The labrum and glenohumeral ligaments are well visualized after distension of the joint cavity by the intra-articular injection[8]. The only drawback of this imaging protocol is that it can miss the presence of any intra-substance rotator cuff tear. To avoid this difficulty, additional T2W MRI with fat suppression can be done in the oblique coronal plane. Imaging with the shoulder in ABER position increases the sensitivity and specificity of detection of anteroinferior labral and glenohumeral ligament attachment abnormalities[3].
| Arthrographic technique | Procedure | Advantages | Drawbacks |
| Indirect | Intravenous injection of gadolinium and imaging 10 min after active exercise of the joint | Simple | Joint cavity distension not achieved; ligamentous pathologies not well detected |
| Does not involve intra-articular injection | |||
| Direct arthrography: anterior approach | Dilute gadolinium injected in the joint cavity through an anterior approach (US- or fluoroscopy-guided). Injection made through a point at the junction of the upper two-thirds and lower–third of anterior joint space | Adequate joint distension helps detection of labral and ligamentous pathologies better | Needs expertise |
| May cause injury to the anterior stabilizing structures | |||
| Carries the risk of intra-articular infection (though rare) | |||
| Direct arthrography: posterior approach | Dilute gadolinium injected in the joint cavity through a posterior approach (US- or fluoroscopy-guided) | Adequate joint distension helps detection of labral and ligamentous pathologies better | Needs expertise |
| May be helpful in anterior instability, to avoid injury to anterior structures | May cause injury to posterior structures | ||
| Carries the risk of intra-articular infection (though rare) | |||
| Direct arthrography: anterosuperior approach | Dilute gadolinium injected in the joint cavity through an anterosuperior approach in the RCI (US- or fluoroscopy-guided) | Adequate joint distension helps detection of labral and ligamentous pathologies better | Needs expertise |
| May cause injury to the rotator interval capsule |
The injecting approach in MR arthrography has undergone several alterations since its introduction. Injection can be performed either through anterior, anterosuperior or posterior approach. Anterior approach is the most commonly adopted one. In 1975, Schneider et al[9] described a simplified injection technique, which uses a straight anteroposterior approach with a 3.5 inch (8.8 cm), 22 gauge needle directed vertically at the junction of the middle and lower thirds of the glenohumeral joint under fluoroscopic guidance. After confirmation of needle placement using 1-2 mL iodinated contrast agent, 10-12 mL of a dilute gadolinium solution (1:200 dilution) is injected into the joint cavity. MR imaging is usually performed within 90 min to avoid absorption of the intra-articular contrast.
A posterior approach can also be adopted, especially when there is anterior instability as needle placement through an anterior route may distort the images of healthy anatomic structures[10]. The patient lies prone with ipsilateral shoulder raised off the table with a pad. A 21 gauge spinal needle is advanced vertically through the inferomedial aspect of the humeral head under fluoroscopic guidance.
For a long time, a modified Schneider technique (anterosuperior approach through rotator interval) has been in use, where the patient is kept supine with arm externally rotated and a 1.5 inch (3.8 cm), 20-22 gauge needle is inserted through an area medial to the superior third of the humeral head. The needle tip is advanced in an anteroposterior direction to the humeral head to avoid contact with the glenoid labrum. The utility of this procedure was established by Dépelteau et al[11].
In indirect MR arthrography, gadolinium is injected intravenously and imaging is done after it diffuses into the joint cavity through a highly vascular synovial lining (which takes a few minutes). However, it lacks the effect of joint distension (compared to direct MR arthrogram).
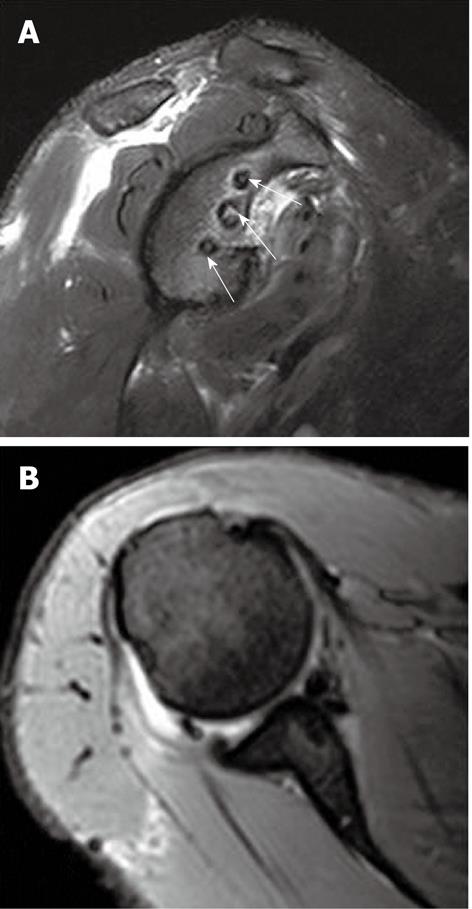
While performing MR arthrography, adequate precautions should be taken to avoid introduction of air in the joint cavity, which can mimic detached and torn labrum on imaging (Figure 7). The gadolinium concentration should also be properly checked, as injection of undiluted gadolinium may lead to diffuse low signal intensity in the joint cavity.
MR imaging in anterior instability can reveal a large number of abnormalities affecting the bone and labroligamentous tissue.
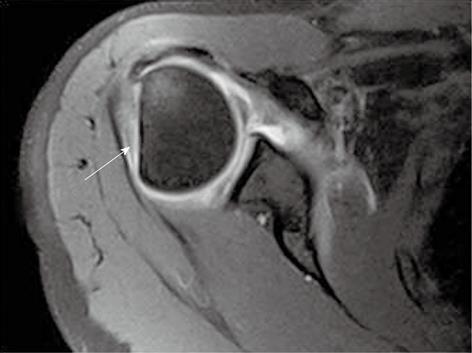
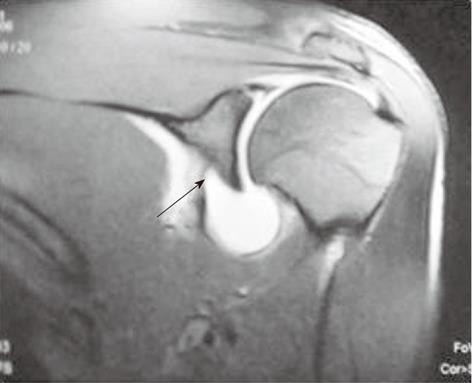
Hill-Sachs lesion (Figure 8) is the most common injury associated with anterior glenohumeral instability. It consists of bony injury of the posterosuperior humeral head manifesting as cortical bony loss, impaction fracture or associated bone marrow edema in acute cases.
Bankart lesion (Figure 9) is the commonest labral injury, manifesting as tear of the anterior inferior labrum with associated periosteal tear[12-14]. It can be purely cartilaginous or may involve the bony glenoid rim (bony Bankart lesion, Figure 10). Bankart lesion is usually accompanied by Hill-Sachs lesion. Several other variants of Bankart lesion have been described, including the Perthes lesion, anterior labroligamentous periosteal sleeve avulsion (ALPSA) lesion, glenolabral articular disruption (GLAD) lesion.
On conventional MR imaging in Bankart lesion, the anteroinferior labrum is seen to be attenuated or absent. The signal intensity on T2* gradient-echo or PD FS FSE MR images may be increased secondary to degeneration of the labrum. On T1 turbo spin echo fat saturation (TSE FS) post-arthrographic MR images, contrast is seen between the labrum and the glenoid margin.
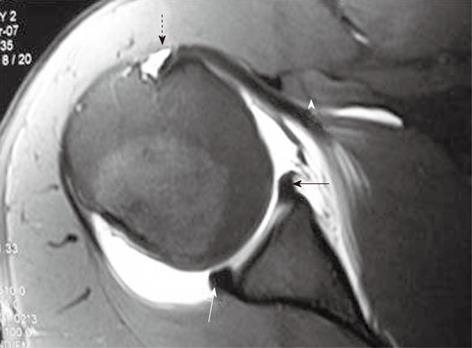
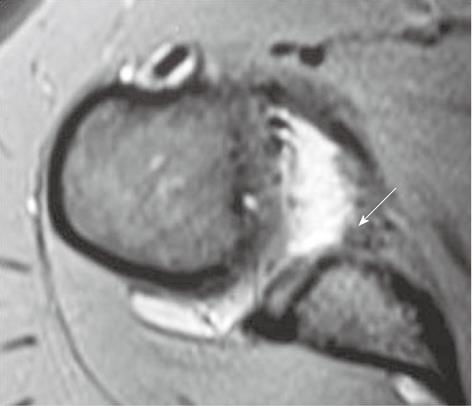
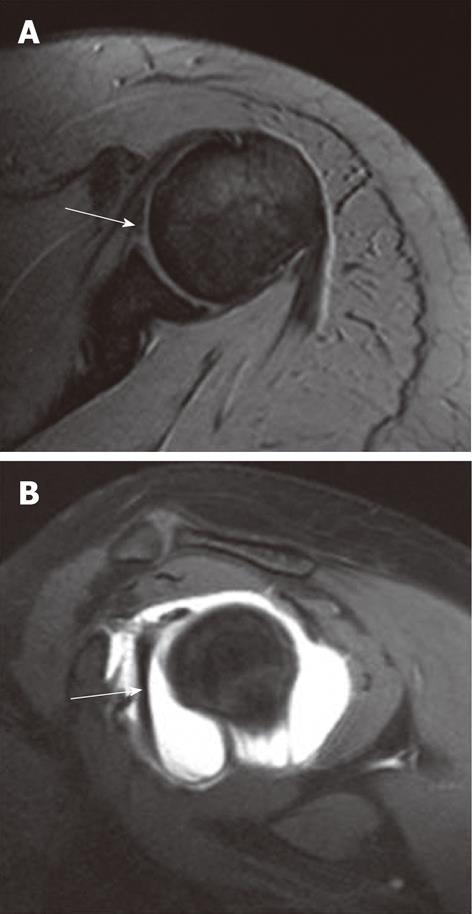
Perthes lesion (Figure 11), described by Perthes in 1905, is defined as a tear of the glenoid labrum with intact scapular periosteum[15]. The torn anterior labrum is often undisplaced and visualized in its normal location on conventional MR imaging. MR arthrography, especially when imaging is performed with the arm in ABER position, improves the detection rate of Perthes lesion, as it puts the anterior band of the IGHL and anteroinferior capsule under stress. This is a difficult lesion to detect, both on conventional MRI and even on arthroscopy[12].
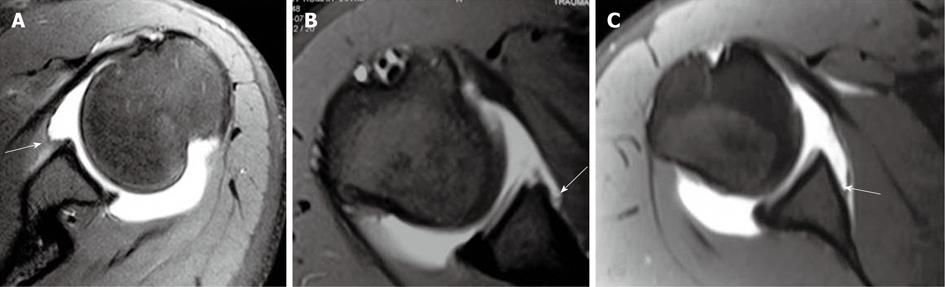
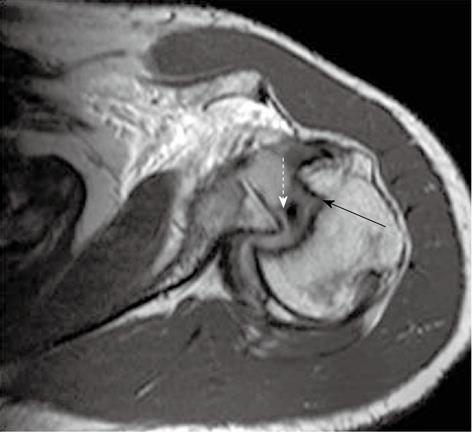
ALPSA lesion (described by Neviaser[16]) is defined as an avulsion and medial rolling of the inferior labroligamentous complex along the scapular neck secondary to a chronic injury (Figure 12). The main differentiating point of ALPSA from a Perthes lesion is the displacement of the torn labroligamentous tissue, which is undisplaced or shows minimal displacement in Perthes lesion. An ALPSA lesion differs from a Bankart lesion in that an ALPSA lesion has an intact anterior scapular periosteum (it is ruptured in Bankart lesion) that allows the labroligamentous structures to displace medially and rotate inferiorly on the scapular neck.
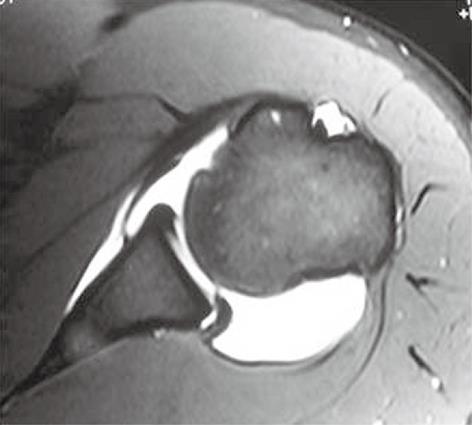
This lesion (also described by Neviaser[17]) consists of a superficial anterior inferior labral tear associated with an anterior inferior articular cartilage injury (Figure 13). The use of intra-articular contrast in MR arthrogram helps to visualize the small tears at the level of the anterior inferior glenoid rim. When a GLAD lesion is seen on MRI, one should look for loose bodies, which can occur from a detached articular cartilage fragment[18].
Superior labrum anterior and posterior (SLAP) lesion, described by Snyder et al[19], is an injury involving the superior aspect of the glenoid labrum that includes the biceps tendon anchor. SLAP tears were initially classified by Snyder et al[19] into 4 distinct but related lesions; Maffet et al[20] added three more types, and currently 10 types or patterns have been recognized. Though SLAP lesions often present with nonspecific symptoms such as pain, locking and snapping, type 5 SLAP lesion (type 2 or 3 SLAP lesion with superior extension of a Bankart lesion) is often associated with anterior shoulder dislocation. Sagittal MRI or MR arthrogram can demonstrate the complete extent of labral tear.
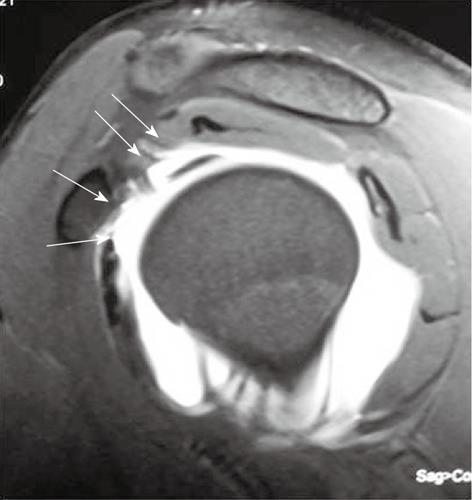
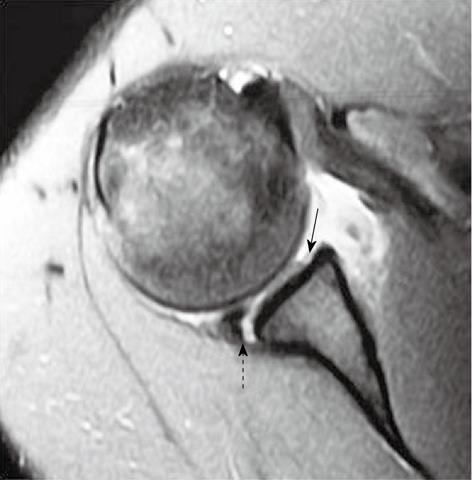
Humeral avulsion of anterior glenohumeral ligament (HAGL) lesion (Figure 14) is a less commonly encountered abnormality (9.3%) in anteroinferior instability[21]. It may coexist with an anterior labral tear in patients with anterior instability. In patients with documented anterior instability without a demonstrable “primary” Bankart lesion, a HAGL lesion should be ruled out[14]. For detection of HAGL, the glenohumeral joint cavity should be well distended, either by contrast agent (direct MR arthrogram) or joint effusion. On coronal MR image, normal distended axillary pouch is seen as a U-shaped structure, which changes into a J-shape in a HAGL lesion as the IGHL drops inferiorly (J sign)[22].
Bony humeral avulsion of glenohumeral ligaments (BHAGL) lesion is less common than HAGL. In BHAGL, there is a small avulsed osseous fragment attached to the torn end of the humeral attachment of the IGHL[23].
This uncommon lesion implies an avulsion of the IGHL from the inferior pole of glenoid without associated disruption of the inferior labrum (Figure 15)[2].
These tears (Figure 16), associated with anterior and inferior glenohumeral dislocation, are commoner in the elderly rather than the younger age group (30% incidence in patients less than 40 years of age and 80% incidence above 60 years of age).
A tear of the RCI typically does not appear as complete disruption of the fibres of its components. Instead it is seen on imaging as thinning, irregularity or focal discontinuity of the rotator interval capsule. Arthroscopy is considered the gold standard in diagnosing RCI lesions. MR arthrography, particularly the T2W sagittal or axial images, may be useful in diagnosing RCI pathologies.
Sublabral foramen is a normal detachment of the anterosuperior labrum (usually at 2 o’clock location) from the glenoid rim that needs to be differentiated from a Bankart lesion[24]. Bankart lesion usually involves the anteroinferior labrum (isolated anterosuperior labral involvement is rare and seen in throwing athletes presenting with pain on overhead abduction). The margins of a labral tear are usually irregular as compared to the sublabral foramen.
Buford complex (Figure 17) is defined as congenital absence of the anterosuperior labrum and thickened cord-like MGHL. The thickened MGHL, when visualized on axial MR images, can mimic detached labrum of a Bankart lesion. However, on oblique sagittal arthrographic images, the superior insertion of a cord-like MGHL is usually visible and misdiagnosis can be avoided[24].
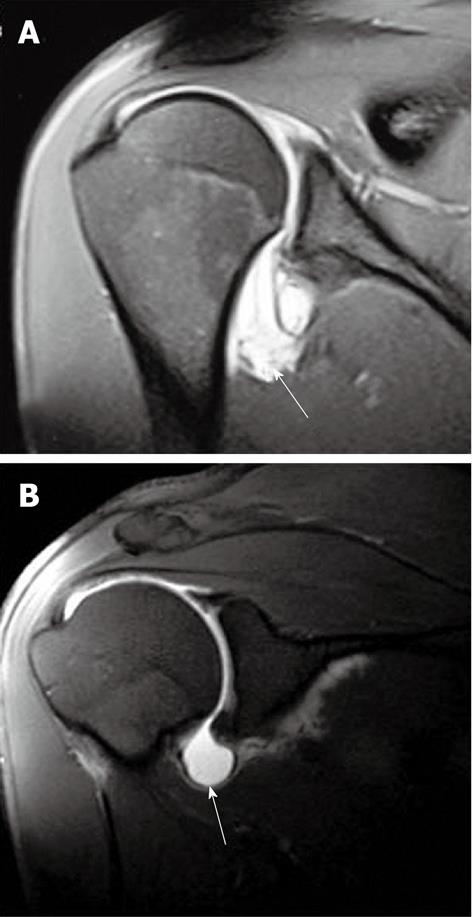
This lesion (Figure 18) consists of an anteromedial superior humeral head impaction fracture which is often associated with a reverse Bankart lesion (posterior glenoid labrum disruption)[25].
In posterior instability, there is sometimes a complete avulsion of the posterior attachment of the shoulder capsule from the posterior humeral neck, associated with tear of the posterior band of the IGHL[4].
This lesion is a newly described entity in posterior glenohumeral instability, which can be seen as focal posterior articular cartilage defect (between 7 and 9 o’clock location)[26].
This is an extra-articular crescentic posterior ossification associated with posterior labral injury and capsular avulsion, sometimes secondary to the posterior subluxation. The ossification is best visualized on CT, and often missed by arthroscopy as it is extra-articular.
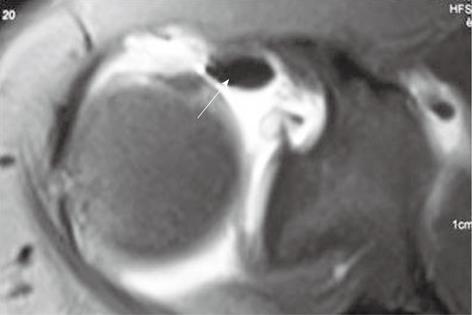
This occurs (Figure 19) as a part of posterior SLAP 2 or posterosuperior to a posterior labral tear in association with a paralabral cyst and may be seen in patients with posterior instability. Posterior superior labral tear may be associated with repetitive microtrauma, as in throwers, and can even be seen in anterior instability[27]. The cysts are almost always associated with labral tears, but the communication with the joint space is often not visualized on MRI.
Anatomic repair of the labrum and capsule using metallic suture anchors is being increasingly employed in glenohumeral instability using an arthroscopic approach[28]. On post-operative MR imaging, susceptibility artifacts
(Figure 20) from the metallic implants may degrade the image quality. A few important points should be kept in mind to overcome this problem: gradient echo sequences should be avoided and replaced by spin echo sequences when possible; fast spin echoes are preferable over standard spin echo sequences; and inversion recovery sequences should be preferred over chemical fat suppression. After an anatomic apposition of the labrum to the articular margin in suture-anchor repair, no hyperintensity should be visible between the two. MR arthrography is more useful in post-operative shoulders as a problem solving tool in suspected recurrent labral tear. Contrast-enhanced T1W sequences should always be acquired in addition if there is a suspicion of septic arthritis[29].
Non-anatomic repairs (Putti-Platt repair, Bristow-Helfet procedure) are usually not preferred for primary instability surgery. Following capsular shift or shrinkage procedures, thickening of the joint capsule can be visualized on imaging.
Complications during arthroscopic repair include inadvertent injury to the axillary nerve (lying in close relation to the inferior joint capsule) and subscapularis muscle injury, hematoma, infection, septic arthritis, heterotopic ossification.
Virtual MR arthroscopy of the shoulder joint has been described in a few reports using 3D gradient echo sequences after intra-articular injection of dilute gadolinium[30]. The technique can act as a useful adjunct tool to MR arthrography in the assessment of labral tears, by providing helpful visual information similar to arthroscopy.
To conclude, MRI and MR arthrography are routinely used investigations in glenohumeral instability and have very high sensitivity in detecting labroligamentous injuries. An MR arthrogram plays a crucial role in the imaging of post-operative shoulder. While diagnosing various labral lesions, anatomic variations should be kept in mind.
Peer reviewers: Sudsriluk Sampatchalit, MD, Lieutenant Colonel, Radiology, Phramongutglao Royal Thai Army Hospital, 315 Ratchawithi Road, Ratchathewi, Bangkok 10400, Thailand; Wenbao Wang, MD, Orthopaedic Department, Columbia University Medical Center, 106 Fort Washington Avenue, Apt 3H, New York, NY 10032, United States
S- Editor Cheng JX L- Editor Logan S E- Editor Zheng XM
| 1. | Tirman PFJ. Glenohumeral instability. Shoulder magnetic resonance imaging. Philadelphia: Lippincott-Raven 1998; 135-167. |
| 2. | Stoller DW, Wolfe EM, Li AE, Nottage WM, Tirman PFJ. The shoulder. Magnetic resonance imaging in orthopedics and sports medicine. 3rd ed. Philadelphia, PA: Lippincott Williams and Wilkins 2007; 1131-1462. |
| 3. | Cvitanic O, Tirman PF, Feller JF, Bost FW, Minter J, Carroll KW. Using abduction and external rotation of the shoulder to increase the sensitivity of MR arthrography in revealing tears of the anterior glenoid labrum. AJR Am J Roentgenol. 1997;169:837-844. [PubMed] |
| 4. | Chung CB, Sorenson S, Dwek JR, Resnick D. Humeral avulsion of the posterior band of the inferior glenohumeral ligament: MR arthrography and clinical correlation in 17 patients. AJR Am J Roentgenol. 2004;183:355-359. [PubMed] |
| 5. | Palmer WE, Caslowitz PL. Anterior shoulder instability: diagnostic criteria determined from prospective analysis of 121 MR arthrograms. Radiology. 1995;197:819-825. [PubMed] |
| 6. | Massengill AD, Seeger LL, Yao L, Gentili A, Shnier RC, Shapiro MS, Gold RH. Labrocapsular ligamentous complex of the shoulder: normal anatomy, anatomic variation, and pitfalls of MR imaging and MR arthrography. Radiographics. 1994;14:1211-1223. [PubMed] |
| 7. | Bigoni BJ, Chung CB. MR imaging of the rotator cuff interval. Magn Reson Imaging Clin N Am. 2004;12:61-73, vi. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Palmer WE, Brown JH, Rosenthal DI. Labral-ligamentous complex of the shoulder: evaluation with MR arthrography. Radiology. 1994;190:645-651. [PubMed] |
| 9. | Schneider R, Ghelman B, Kaye JJ. A simplified injection technique for shoulder arthrography. Radiology. 1975;114:738-739. [PubMed] |
| 10. | Chung CB, Dwek JR, Feng S, Resnick D. MR arthrography of the glenohumeral joint: a tailored approach. AJR Am J Roentgenol. 2001;177:217-219. [PubMed] |
| 11. | Dépelteau H, Bureau NJ, Cardinal E, Aubin B, Brassard P. Arthrography of the shoulder: a simple fluoroscopically guided approach for targeting the rotator cuff interval. AJR Am J Roentgenol. 2004;182:329-332. [PubMed] |
| 12. | Waldt S, Burkart A, Imhoff AB, Bruegel M, Rummeny EJ, Woertler K. Anterior shoulder instability: accuracy of MR arthrography in the classification of anteroinferior labroligamentous injuries. Radiology. 2005;237:578-583. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 135] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 13. | Rowan KR, Keogh C, Andrews G, Cheong Y, Forster BB. Essentials of shoulder MR arthrography: a practical guide for the general radiologist. Clin Radiol. 2004;59:327-334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 14. | Shankman S, Bencardino J, Beltran J. Glenohumeral instability: evaluation using MR arthrography of the shoulder. Skeletal Radiol. 1999;28:365-382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 84] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 15. | Wischer TK, Bredella MA, Genant HK, Stoller DW, Bost FW, Tirman PF. Perthes lesion (a variant of the Bankart lesion): MR imaging and MR arthrographic findings with surgical correlation. AJR Am J Roentgenol. 2002;178:233-237. [PubMed] |
| 16. | Neviaser TJ. The anterior labroligamentous periosteal sleeve avulsion lesion: a cause of anterior instability of the shoulder. Arthroscopy. 1993;9:17-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 267] [Cited by in RCA: 187] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 17. | Neviaser TJ. The GLAD lesion: another cause of anterior shoulder pain. Arthroscopy. 1993;9:22-23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 101] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 18. | McCauley TR. MR imaging of the glenoid labrum. Magn Reson Imaging Clin N Am. 2004;12:97-109, vi-vii. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 19. | Snyder SJ, Karzel RP, Del Pizzo W, Ferkel RD, Friedman MJ. SLAP lesions of the shoulder. Arthroscopy. 1990;6:274-279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1176] [Cited by in RCA: 916] [Article Influence: 26.2] [Reference Citation Analysis (1)] |
| 20. | Maffet MW, Gartsman GM, Moseley B. Superior labrum-biceps tendon complex lesions of the shoulder. Am J Sports Med. 1995;23:93-98. [PubMed] |
| 21. | Wolf EM, Cheng JC, Dickson K. Humeral avulsion of glenohumeral ligaments as a cause of anterior shoulder instability. Arthroscopy. 1995;11:600-607. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 256] [Cited by in RCA: 196] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 22. | Carlson CL. The "J" sign. Radiology. 2004;232:725-726. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 23. | Oberlander MA, Morgan BE, Visotsky JL. The BHAGL lesion: a new variant of anterior shoulder instability. Arthroscopy. 1996;12:627-633. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 47] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 25. | Harish S, Nagar A, Moro J, Pugh D, Rebello R, O’Neill J. Imaging findings in posterior instability of the shoulder. Skeletal Radiol. 2008;37:693-707. |
| 26. | Anderson M, Barr M, Gaskin C, Alford B. Posterior GLAD lesions of the shoulder (scientific Presentation). RSNA 2005. 2005;. |
| 27. | Hottya GA, Tirman PF, Bost FW, Montgomery WH, Wolf EM, Genant HK. Tear of the posterior shoulder stabilizers after posterior dislocation: MR imaging and MR arthrographic findings with arthroscopic correlation. AJR Am J Roentgenol. 1998;171:763-768. [PubMed] |
| 28. | Zlatkin MB. MRI of the postoperative shoulder. Skeletal Radiol. 2002;31:63-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 50] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 29. | Mohana-Borges AV, Chung CB, Resnick D. MR imaging and MR arthrography of the postoperative shoulder: spectrum of normal and abnormal findings. Radiographics. 2004;24:69-85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 74] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 30. | Song HT, Huh YM, Kim S, Kim SJ, Suh JS. The usefulness of virtual MR arthroscopy as an adjunct to conventional MR arthrography in detecting anterior labral lesions of the shoulder. AJR Am J Roentgenol. 2009;192:W149-W155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |