Published online Oct 28, 2011. doi: 10.4329/wjr.v3.i10.246
Revised: July 25, 2011
Accepted: August 1, 2011
Published online: October 28, 2011
Lipomas of the pancreas are very rare. There are fewer than 25 reported cases of lipoma originating from the pancreas. We present a case of pancreatic lipoma in a 61-year-old woman with magnetic resonance imaging findings and confirmatory histological findings. We discuss and highlight the radiological features distinguishing a pancreatic lipoma from other fatty lesions of the pancreas and pancreatic liposarcoma and provide a brief review of the literature.
- Citation: Lee SY, Thng CH, Chow PK. Lipoma of the pancreas, a case report and a review of the literature. World J Radiol 2011; 3(10): 246-248
- URL: https://www.wjgnet.com/1949-8470/full/v3/i10/246.htm
- DOI: https://dx.doi.org/10.4329/wjr.v3.i10.246
Pancreatic tumors arise from cells of mesenchymal or epithelial origin, or from non-ductal structures and fat. Epithelial tumors constitute the largest group including adenocarcinoma which account for 85% of all pancreatic tumors. Non-ductal tumors account for 5%-15%, and mesenchymal tumors account for about 1%[1]. Among these, fat-originating tumors such as lipoma and liposarcomas are the rarest.
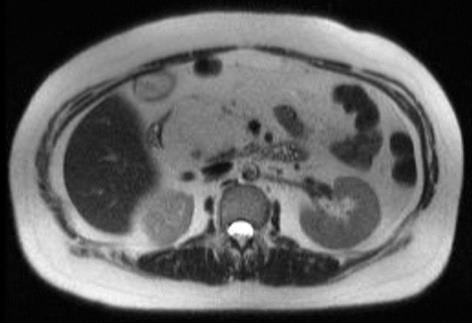
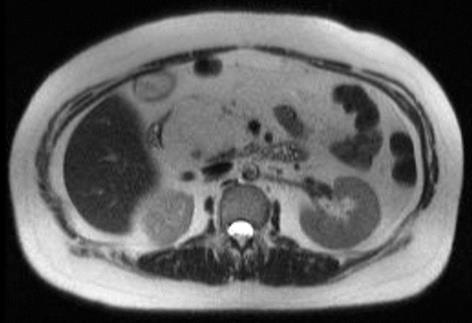
A 61-year-old woman with a past medical history of dyslipidemia and cholelithiaisis was admitted to our institution for right hypochondrium pain and epigastric discomfort and vomiting of 2 wk duration. Her liver function tests revealed mild transaminitis with alanine transaminase 246 U/L, aspartate transaminase 308 U/L, raised alkaline phosphatase (ALP) 188 U/L and γ-glutamyl transferase (GGT) 408 U/L. The tumor marker carbohydrate antigen 19-9 was slightly raised, 52.2 U/mL (reference range 3-50 U/mL). Physical examination was normal. Ultrasonography revealed multiple subcentimetre gallstones; the pancreas was noted not to be well visualized due to overlying bowel gas. She was treated symptomatically for biliary colic and was discharged well with a view for an elective laparoscopic cholecystectomy. In view of her persistent raised ALP and GGT, a magnetic resonance cholangiopancreaticography was performed during follow-up. It revealed a 6.8 cm × 4.4 cm fat containing lesion arising from the pancreatic head, scalloping the pancreatic head and displacing the duodenum (Figures 1 and 2).
Because of its size, liposarcoma could not be excluded. A Whipple’s procedure was performed and the final histology of the lesion was a pancreatic lipoma. Post-operative recovery was uneventful and she was discharged in a healthy condition.
Lipomas are made up of mature adipose cells within a thin collagen capsule. They can be found almost anywhere in the body where there is adipose tissue. When found intra-abdominally, they frequently arise from the gastrointestinal tract, although they can be found in other rare locations such as the pancreas. In the literature there are less than 25 cases of pancreatic lipoma[2] and 4 cases of pancreatic liposarcoma reported to date. The first reported case was described by Bigard et al[3] in 1989 as a hypoechoic mass in the head of the pancreas and this was histologically confirmed as a lipoma. Several imaging modalities were used in the reported cases for diagnosis. Katz et al[4] presented 4 cases of pancreatic lipoma diagnosed on computed tomography (CT), showing a homogenous lesion composing of fat. Legmann et al[5] defined the CT findings of a pancreatic lipoma. CT findings for a pancreatic lipoma include homogenous distribution of fat density with no central or peripheral contrast enhancement, Housefield units of -80 to -120 and a sharp demarcation with no evidence of intra- and extra-pancreatic adjacent structures infiltration. Some of these characteristics were used as a definition by Ozelm et al[2]. Ultrasonography was used in a series by Itai et al[6]. Elliott et al[7] reported a case of pancreatic liposarcoma with plain abdominal X-rays. Di Matteo et al[8] reported a case of pancreatic lipoma that was diagnosed on endoscopic ultrasonography.
Besides lipoma of the pancreas, fatty lesions in the pancreas include focal fatty infiltration of the pancreas, teratoma and liposarcoma. Liposarcoma is itself a heterogeneous group. Classification of liposarcoma into subtypes is based on morphologic features and cytogenetic aberrations; namely, the 5 subtypes are well-differentiated, de-differentiated, myxoid, round cell and pleomorphic[9]. Magnetic resonance imaging (MRI) has been used to characterize the different groups of liposarcomas in the retroperitoneum. Well-differentiated liposarcoma presents as high signal intensity on T1-weighted (T1W) images, intermediate signal intensity on T2-weighted (T2W) images and drop-out signal intensity on fat-suppressed MR images. De-differentiated liposarcoma has clear demarcations between fat and non-adipose solid tissues and reveals small amounts of fatty components. Myxoid liposarcoma has a low signal intensity on T1W image and high signal intensity on T2W image. Round-cell liposarcoma and pleomorphic liposarcoma have soft tissue tumor signal intensity without the characteristic fat signal. This suggests MRI as the ideal imaging modality for retroperitoneal liposarcomas as it can demonstrate its margins and internal components[9]. In a review and meta-analysis of the role of 18F-fluorodeoxyglucose positron emission tomography (FDG-PET) in soft tissue sarcomas, the results indicate that FDG-PET can discriminate between sarcomas and benign tumors and low and high grade sarcomas based on the mean standard uptake value[10].
It has been suggested that both focal fatty infiltrations and lipomas can be managed conservatively in asymptomatic and incidental cases. A presumptive diagnosis of lipoma can be made if the lesion is purely fat containing no solid areas and is small (< 3 cm) in size. In the literature, there are no definite diagnostic criteria based on size for distinguishing a lipoma from a liposarcoma in the retroperitoneum. In fact, the tumor burden (the sum of the maximum diameter of the primary tumors) has been reported in a series to be as small as 5 cm. For liposarcomas, a large (> 10 cm) size, arising from a retroperitoneal site, as well as an involved resection margin, are reported as adverse prognostic factors[11].
Most investigators believe that histology is not absolutely necessary to confirm the diagnosis of pancreatic lipoma because radiologic features are almost diagnostic. However, a well-differentiated lipogenic liposarcoma may mimic a benign lesion because of homogeneity of fat and its sharply defined margins on imaging.
Retroperitoneal liposarcomas are rare and pancreatic liposarcomas are even more uncommon with eventual metastases reported in 30%-60% of cases[12]. Only 4 cases of pancreatic liposarcoma have been reported, with minimal radiologic data[1,3]. The reported pancreatic liposarcomas range from 9 to 16 cm in largest diameter and diagnosis is retrospective in nature and is not achieved based on imaging alone[13,14]. A retrospective review of our departmental records identified 21 patients with primary retroperitoneal liposarcoma treated between July 1990 and June 2005. There have been no liposarcomas related to the pancreas in our institution to date[14].
In our case, the lesion is large and it is difficult to rule out the possibility of liposarcoma. The patient also has pain associated with symptoms of gastric outlet obstruction from compression of the duodenum and has a persistently abnormal liver function test. Hence a decision was made to perform a Whipple’s procedure to excise the tumor.
In summary, lipomas of the pancreas are very rare. The exact radiological diagnosis to differentiate it from other fat-containing lesions can be difficult. Several radiological modalities have been used, of which MRI proves to be the most useful[15]. An asymptomatic or incidental lesion can be managed conservatively and monitored with serial imaging. However, if it is compressing on vital structures e.g. ampulla of vater or duodenum, causing symptoms or if there are any suggestions of malignant change e.g. large size, rapid growth or radiologically heterogeneous, surgery can be offered as an option for treatment and histopathological confirmation.
Peer reviewer: Kenneth Coenegrachts, MD, PhD, Department of Radiology, AZ St.-Jan AV, Ruddershove 10, B-8000 Bruges, Belgium
S- Editor Cheng JX L- Editor O’Neill M E- Editor Zheng XM
| 1. | Raut CP, Fernandez-del Castillo C. Giant lipoma of the pancreas: case report and review of lipomatous lesions of the pancreas. Pancreas. 2003;26:97-99. [PubMed] |
| 2. | Barutcu O, Cihangiroglu M, Yildirim T, Kayaselcuk F, Noyan T. Fat containing unusual tumor of the pancreas. Eur Radiol. 2002;12:770-773. [PubMed] |
| 3. | Bigard MA, Boissel P, Regent D, Froment N. Intrapancreatic lipoma. First case in the literature. Gastroenterol Clin Biol. 1989;13:505-507. [PubMed] |
| 4. | Katz DS, Nardi PM, Hines J, Barckhausen R, Math KR, Fruauff AA, Lane MJ. Lipomas of the pancreas. AJR Am J Roentgenol. 1998;170:1485-1487. [PubMed] |
| 5. | Legmann P, Vignaux O, Dousset B, Grellet J. Rare and secondary tumors of the pancreas. Radiology of the pancreas. 2nd ed. New York: Springer, Berlin Heidelberg 1999; 295-310. |
| 6. | Itai Y, Saida Y, Kurosaki Y, Kurosaki A, Fujimoto T. Focal fatty masses of the pancreas. Acta Radiol. 1995;36:178-181. [PubMed] |
| 7. | Elliott TE, Albertazzi VJ, Danto LA. Pancreatic liposarcoma: case report with review of retroperitoneal liposarcomas. Cancer. 1980;45:1720-1723. [PubMed] |
| 8. | Di Matteo FM, Shimpi L, Pandolfi M, Rabitti C, Fabio C, Gabbrielli A, Costamagna G. EUS diagnosis of pancreatic lipoma: a case report. Gastrointest Endosc. 2006;64:146-148. [PubMed] |
| 9. | Song T, Shen J, Liang BL, Mai WW, Li Y, Guo HC. Retroperitoneal liposarcoma: MR characteristics and pathological correlative analysis. Abdom Imaging. 2004;32:668-674. [PubMed] |
| 10. | Bastiaannet E, Groen H, Jager PL, Cobben DC, van der Graaf WT, Vaalburg W, Hoekstra HJ. The value of FDG-PET in the detection, grading and response to therapy of soft tissue and bone sarcomas; a systematic review and meta-analysis. Cancer Treat Rev. 2004;30:83-101. [PubMed] |
| 11. | Linehan DC, Lewis JJ, Leung D, Brennan MF. Influence of biologic factors and anatomic site in completely resected liposarcoma. J Clin Oncol. 2000;18:1637-1643. [PubMed] |
| 12. | Dei Tos AP. Liposarcoma: new entities and evolving concepts. Ann Diagn Pathol. 2000;4:252-266. [PubMed] |
| 13. | Di Maggio EM, Solcia M, Dore R, Preda L, La Fianza A, Rodino C, Campani R. Intrapancreatic lipoma: first case diagnosed with CT. AJR Am J Roentgenol. 1996;167:56-57. [PubMed] |
| 14. | Lee SY, Goh BK, Teo MC, Chew MH, Chow PK, Wong WK, Ooi LL, Soo KC. Retroperitoneal liposarcomas: the experience of a tertiary Asian center. World J Surg Oncol. 2011;9:12. [PubMed] |
| 15. | Secil M, Igci E, Goktay AY, Dicle O. Lipoma of the pancreas: MRI findings. Comput Med Imaging Graph. 2001;25:507-509. [PubMed] |