Published online Sep 28, 2010. doi: 10.4329/wjr.v2.i9.374
Revised: June 20, 2010
Accepted: June 27, 2010
Published online: September 28, 2010
Significant hemobilia due to arterio-biliary fistula is a very rare complication of chemoradiation therapy (CRT) for unresectable intrahepatic cholangiocarcinoma (ICC). Here we report a case of arterio-biliary fistula after CRT for unresectable ICC demonstrated by angiographic examinations. This fistula was successfully treated by endovascular embolization. Hemobilia is a rare complication, but arterio-biliary fistula should be considered after CRT of ICC.
- Citation: Hayano K, Miura F, Amano H, Toyota N, Wada K, Kato K, Takada T, Asano T. Arterio-biliary fistula as rare complication of chemoradiation therapy for intrahepatic cholangiocarcinoma. World J Radiol 2010; 2(9): 374-376
- URL: https://www.wjgnet.com/1949-8470/full/v2/i9/374.htm
- DOI: https://dx.doi.org/10.4329/wjr.v2.i9.374
Arterio-biliary fistula is a rare clinical condition resulting from various causes. Serious clinical symptoms occur due to shunting of high-pressure blood from the hepatic artery into the bile duct. Here, we report a case of arterio-biliary fistula after chemoradiation therapy (CRT) for unresectable intrahepatic cholangiocarcinoma (ICC) demonstrated by angiographic examinations.
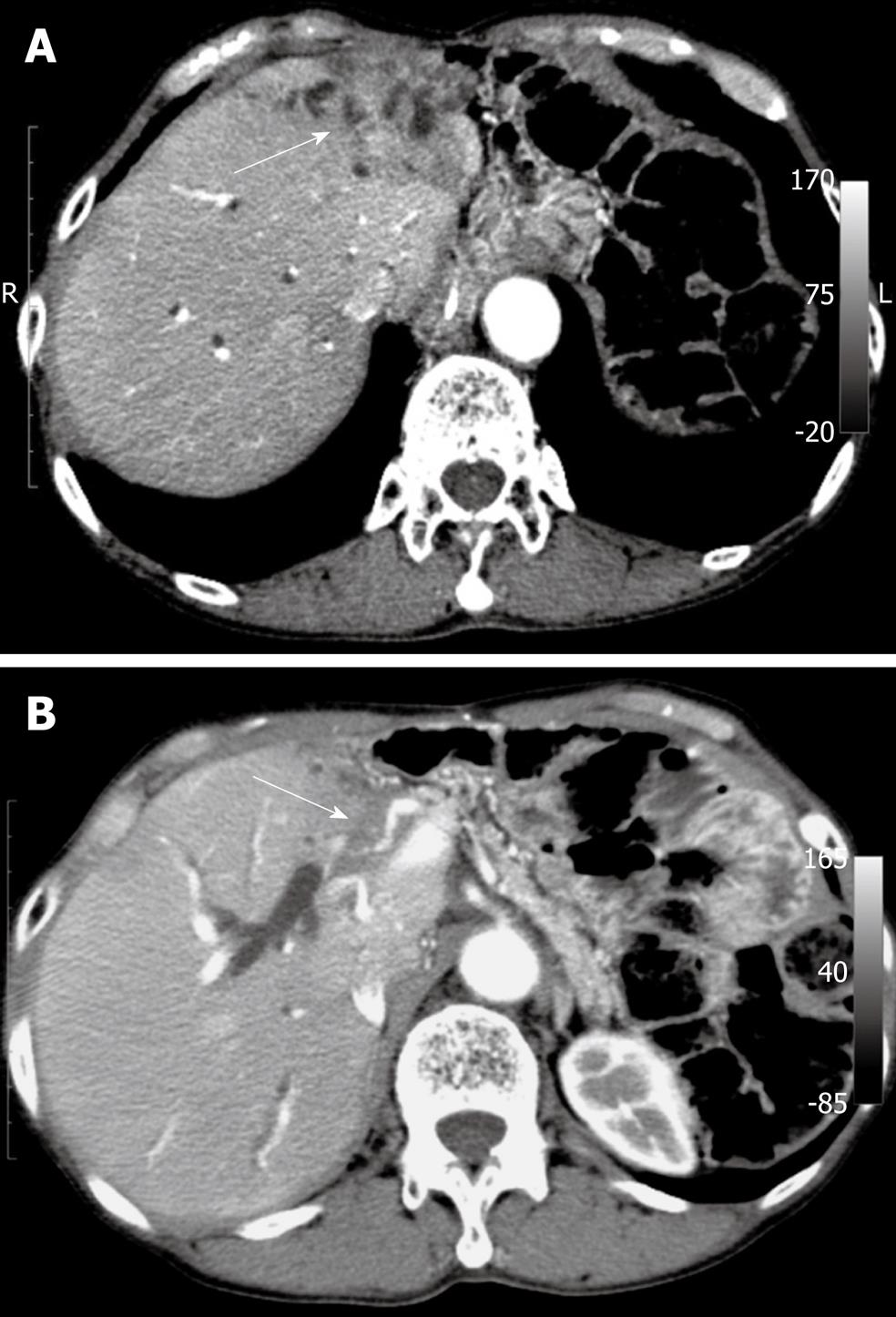
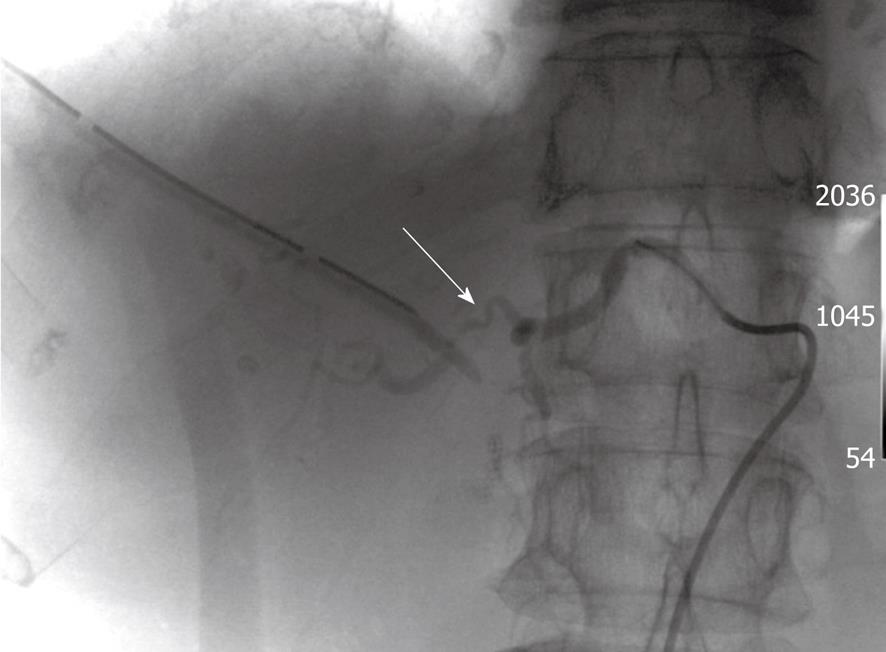
A 78-year-old woman presented with obstructive jaundice. Computed tomography (CT) showed a tumor in the left lobe of the liver, which spread along the bile duct to the right hepatic bile duct. This tumor was diagnosed as cholangiocarcinoma, which had invaded the proper hepatic artery (Figure 1). Thus, we considered that this tumor was unable to be surgically resected, and percutaneous transhepatic biliary drainage (PTBD) was performed. After changing the PTBD tube to an internal-external biliary catheter, gemcitabine-based CRT (external beam radiation therapy; total dose 50 Gy) was administered. Chemotherapy was given in a palliative setting. Six months later, the tumor showed a partial response, but she developed tarry stools and was admitted for evaluation. Upper and lower gastrointestinal endoscopy showed no findings of tarry stool, but hemobilia was observed from the internal-external biliary catheter. Therefore, we performed arterial angiography, which revealed a fistula between the right hepatic artery and the right hepatic bile duct (Figure 2). Transcatheter embolization of the proper hepatic artery using microcoils was successful in stopping the hemobilia. After this event, the patient received chemotherapy, and subsequently showed no hemobilia or sign of recurrence.
Cholangiocarcinoma is a therapeutically challenging malignancy. The prognosis is typically poor. Multiple studies have demonstrated the potential efficacy of radiotherapy, with and without chemosensitization, as palliative therapy[1,2] and neoadjuvant therapy prior to conventional resection[3]. Recently, it was reported that liver transplantation with neoadjuvant CRT is more effective than resection for cholangiocarcinoma[4]. Thus, CRT for cholangiocarcinoma will become a major strategy for the treatment of this malignancy.
On the other hand, significant hemobilia due to arterio-biliary fistula is a very rare complication of CRT for ICC. There have been some reports of arterio-biliary fistula due to iatrogenic injury resulting from PTBD or hepatic biopsy[5,6]. However, arterial bleeding from a PTBD tract is very uncommon as a late complication[7,8], in contrast to the early phase after PTBD placement. In our patient, exchange of the internal-external biliary catheter had been performed prior to CRT with no bleeding, and arterio-biliary fistula occurred 6 mo after PTBD placement. In addition, the arterial angiography showed a region of irregular arterial wall of the right hepatic artery, but the proximal region of irregular arterial wall was some distance from the biliary catheter (Figure 2). Thus, we hypothesize that these facts suggest that transection of the hepatic artery by the biliary catheter was not the cause of the fistula, and we suspect that the tumoricidal depth of CRT beyond the thickness of the tumor resulted in damage of the right hepatic artery and fistula formation between the bile duct and the hepatic artery.
Transarterial embolization is considered the first line of intervention to stop the bleeding, since this interventional radiological procedure is minimally invasive, has a high success rate and a low incidence of complications compared to the more complex and dangerous surgical or laparoscopic options[9].
Arterio-biliary fistula is a very rare complication of CRT for ICC. However, the possibility of arterio-biliary fistula should be considered after CRT of ICC invading the hepatic artery.
Peer reviewer: Misha Luyer, MD, PhD, Department of Surgery, Orbis Medical Centre, Postbus 5500, Sittard, 6130 MB, The Netherlands
S- Editor Cheng JX L- Editor Logan S E- Editor Zheng XM
| 1. | Kamada T, Saitou H, Takamura A, Nojima T, Okushiba SI. The role of radiotherapy in the management of extrahepatic bile duct cancer: an analysis of 145 consecutive patients treated with intraluminal and/or external beam radiotherapy. Int J Radiat Oncol Biol Phys. 1996;34:767-774. |
| 2. | Heron DE, Stein DE, Eschelman DJ, Topham AK, Waterman FM, Rosato EL, Alden M, Anne PR. Cholangiocarcinoma: the impact of tumor location and treatment strategy on outcome. Am J Clin Oncol. 2003;26:422-428. |
| 3. | McMasters KM, Tuttle TM, Leach SD, Rich T, Cleary KR, Evans DB, Curley SA. Neoadjuvant chemoradiation for extrahepatic cholangiocarcinoma. Am J Surg. 1997;174:605-608; discussion 608-609. |
| 4. | Rea DJ, Heimbach JK, Rosen CB, Haddock MG, Alberts SR, Kremers WK, Gores GJ, Nagorney DM. Liver transplantation with neoadjuvant chemoradiation is more effective than resection for hilar cholangiocarcinoma. Ann Surg. 2005;242:451-458; discussion 458-461. |
| 5. | L'Hermine C, Ernst O, Delemazure O, Sergent G. Arterial complications of percutaneous transhepatic biliary drainage. Cardiovasc Intervent Radiol. 1996;19:160-164. |
| 7. | Born P, Rösch T, Triptrap A, Frimberger E, Allescher HD, Ott R, Weigert N, Lorenz R, Classen M. Long-term results of percutaneous transhepatic biliary drainage for benign and malignant bile duct strictures. Scand J Gastroenterol. 1998;33:544-549. |
| 8. | Schumacher B, Othman T, Jansen M, Preiss C, Neuhaus H. Long-term follow-up of percutaneous transhepatic therapy (PTT) in patients with definite benign anastomotic strictures after hepaticojejunostomy. Endoscopy. 2001;33:409-415. |
| 9. | Basile A, Lupattelli T, Giulietti G, Massa Saluzzo C, Mundo E, Carbonatto P, Magnano M, Patti MT. Interventional treatment of iatrogenic lesions and hepatic arteries. Radiol Med. 2005;110:88-96. |