Published online Jul 28, 2010. doi: 10.4329/wjr.v2.i7.280
Revised: June 8, 2010
Accepted: June 15, 2010
Published online: July 28, 2010
A 70 years old male on ventilatory and circulatory support for sepsis and non ST segment elevation myocardial infarction developed abdominal distension 14 d after placement of a percutaneous endoscopic gastrostomy tube for enteral feeding. Radiography revealed free air in the abdomen and gastrograffin (G) study showed no extravasation into the peritoneum. The G tube was successfully repositioned with mechanical release of air. Imaging showed complete elimination of free air but the patient had a recurrence of pneumoperitoneum. Mechanical release of air with sealing of the abdominal wound was performed. Later, the patient was restarted on tube feeding with no complications. This case demonstrates a late complication of pneumoperitoneum with air leakage from the abdominal wall stoma.
-
Citation: Vijayakrishnan R, Adhikari D, Anand CP. Recurrent tense pneumoperitoneum due to air influx
via abdominal wall stoma of a PEG tube. World J Radiol 2010; 2(7): 280-282 - URL: https://www.wjgnet.com/1949-8470/full/v2/i7/280.htm
- DOI: https://dx.doi.org/10.4329/wjr.v2.i7.280
Percutaneous endoscopic gastrostomy (PEG) is a method of choice for providing enteral access and nutritional support to patients who are unable to take oral feedings. Pneumoperitoneum is a common complication of PEG tube placement and imaging needs to be performed to rule out leakage at the site of the visceral stoma. We report a case of late occurrence of pneumoperitoneum after PEG tube placement occuring due to air leakage from the abdominal wall stoma.
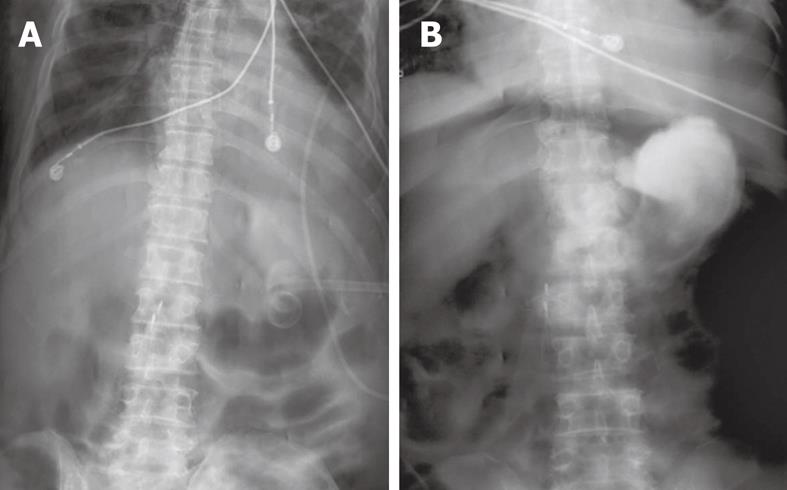
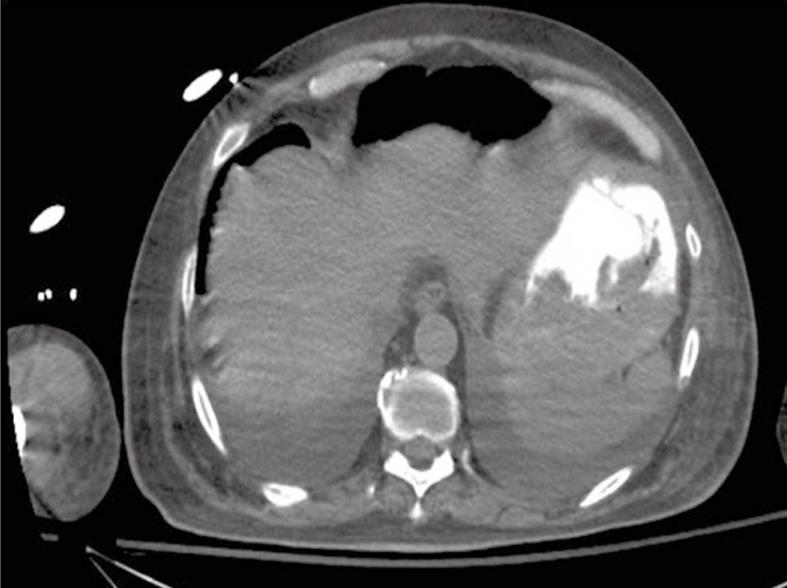
A 70-year-old Asian male with sepsis and non ST segment elevation myocardial infarction (NSTEMI) was admitted to the intensive care unit for ventilatory and circulatory support. As the patient required ventilatory support for a prolonged period due to sepsis, pneumonia and NSTEMI, PEG tube placement was considered for enteral feeding. The placement of the PEG tube was performed without any complications and an X-ray of the abdomen (Figure 1A) revealed no air leak. The patient was feeding well until day 14 of the PEG tube placement, when the patient developed abdominal distension with hemodynamic compromise and ventilatory non-compliance. Tube feeding was stopped immediately and an X-ray of the abdomen was obtained that revealed the gastrograffin (G) tube in place with free air in the abdomen. A G contrast study (Figure 1B) was performed to determine the tube position and revealed normal G tube positioning without any extravasation into the peritoneum. While repositioning the PEG tube mechanically, a gush of free air was noted to leak out of the abdominal wall stoma. Subsequent X-rays of the abdomen and chest revealed no evidence of pneumoperitoneum. PEG tube feeding was commenced after sealing the abdominal stoma with DuoDERM®. The patient continued on tube feeding without any residual effects but again developed abdominal distension. There was no documented fever or leukocytosis to suggest peritonitis. A computed tomography (CT) scan of the abdomen (Figure 2) revealed free air in the abdomen without any evidence of ascitis or inflammation of the small and large bowel. G study revealed no extravasation of contrast into the peritoneum to suggest a visceral stomal leak or bowel perforation. The patient again underwent a tube repositioning during which a gush of free air was noted to leak out of the abdominal stoma. The conclusion was that the patient had an air leak not from the visceral stoma but possibly through the abdominal wall stoma. The patient had the abdominal wall stoma sealed again with DuoDERM® after removal of air by mechanically pushing on the abdominal wall. Serial X-rays were taken during the hospital stay that revealed a progressive decrease in pneumoperitoneum and a correct G tube position. The patient tolerated the tube feeds well and was discharged to a short term rehabiliation centre.
PEG is a commonly used method for providing nutritional support to patients in whom oral feeding is contra-indicated. Various complications such as skin site infection, bleeding, hematoma formation, aspiration, perforation and pneumoperitoneum are common (Table 1)[1]. Pneumoperitoneum was noted in 8.6% of the PEG tube placements in a retrospective analysis[2]. Pneumoperitoneum is usually benign in nature and resolves spontaneously. Air in the abdomen is usually seen within 72 h of PEG tube placement. In nearly all cases reported in the literature, the air leak is from the visceral tube insertion site[3,4]. If there is evidence of free fluid in the peritoneal cavity in addition to free air, some gastroenterologists have recommended explorative laprotomy[3]. If the patient is asymptomatic and hemodynamically stable with only pneumoperitoneum, no further intervention is recommended.
| Major complication | Minor complication |
| Gastric perforation | Pneumoperitoneum |
| Esophageal perforation | Gastroesophageal erosion |
| Gastrocolocutaneous fistula | Temporary ileus |
| Gastric outlet obstruction | Hematoma |
| Necrotizing fascitis | Tube dislodgement |
| Buried bumper syndrome | Hemorrhage |
| Wound infection | |
| Aspiration | |
| Tube clogging |
In our patient, as there was hemodynamic compromise, ventilatory non-compliance and progressively increasing abdominal distension, an attempt was made to reposition the PEG tube. In our case, pneumoperitoneum occurred as a late complication and the leakage site was the abdominal wall stoma. This is rare when compared to an air leak from the visceral stoma, which occurs as an early complication of PEG tube placement.
In a patient with a PEG tube, if pneumoperitoneum is suspected, tube feeding should be withheld immediately. Another differential diagnosis of pneumoperitoneum should be ruled out prior to making a definitive diagnosis of PEG tube leakage. One must also look for clinical signs of peritonitis such as abdominal pain, tenderness, rigidity, nausea, vomiting, progressive distension and fever. In patients who are intubated and sedated, careful observation for signs of sepsis and serial abdominal examinations need to be performed to detect early peritonitis. The other group in which detection of peritonitis can be challenging are patients receiving chemotherapy. Abdominal discomfort, distension and low grade fever should raise suspicion of PEG tube leakage in this group of patients. Radiographic imaging with X-ray and/or CT scan with or without contrast must be undertaken. An increased white blood cell count will also indicate an inflammatory process. These investigations guide the management of the pneumoperitoneum. PEG tube repositioning may be considered as a treatment modality. Serial radiographic imaging is warranted to visualise the resolution of pneumoperitoneum after repositioning. If there is no evidence of contrast leakage into the peritoneum (with G contrast study), PEG tube feeding can be resumed.
Peristomal leakage is a common complication in the elderly population. Spontaneous closure of the leakage occurs in a limited number of patients with improved nutrition, proton pump inhibitors and local wound care. Surgical tract closure and excision have been the traditional treatments for persistent peristomal leakage. Recent advances in endoscopic techniques like electrochemical cauterization and clip closure have shown encouraging preliminary results[5].
This is the first reported case of recurrent tense pneumoperitoneum occurring due to an influx of air through the external stoma of a PEG. After exclusion of intestinal perforation and a visceral tube insertion site leak, an air leak from the abdominal wall stoma should be considered as a cause of pneumoperitoneum in PEG tube patients.
Peer reviewer: Dr. Dinesh Vyas, Department of Minimally and Endosopic Surgery, St John Mercy Hospital, 851 E Fifth Street, Washington, DC 63090, United States
S- Editor Tian L L- Editor Lutze M E- Editor Yang C
| 1. | Wiesen AJ, Sideridis K, Fernandes A, Hines J, Indaram A, Weinstein L, Davidoff S, Bank S. True incidence and clinical significance of pneumoperitoneum after PEG placement: a prospective study. Gastrointest Endosc. 2006;64:886-889. |
| 2. | Stassen WN, McCullough AJ, Marshall JB, Eckhauser ML. Percutaneous endoscopic gastrostomy: another cause of "benign" pneumoperitoneum. Gastrointest Endosc. 1984;30:296-298. |
| 3. | Blum CA, Selander C, Ruddy JM, Leon S. The incidence and clinical significance of pneumoperitoneum after percutaneous endoscopic gastrostomy: a review of 722 cases. Am Surg. 2009;75:39-43. |
| 4. | Alley JB, Corneille MG, Stewart RM, Dent DL. Pneumoperitoneum after percutaneous endoscopic gastrostomy in patients in the intensive care unit. Am Surg. 2007;73:765-767; discussion 768. |
| 5. | Duddempudi S, Ghevariya V, Singh M, Krishnaiah M, Anand S. Treatment of Persistently Leaking Post PEG Tube Gastrocutaneous Fistula in Elderly Patients with Combined Electrochemical Cautery and Endoscopic Clip Placement. South Med J. 2009;102:585-588. |