Published online Mar 28, 2010. doi: 10.4329/wjr.v2.i3.109
Revised: March 8, 2010
Accepted: March 16, 2010
Published online: March 28, 2010
AIM: To evaluate the effects of percutaneous ozone injection via the posterior-lateral route and inner margin of the facet joint in the treatment of large lumbar disc herniation.
METHODS: Fifty-eight patients with large lumbar disc herniation were treated with percutaneous injection of ozone via the posterior-lateral route and inner margin of the facet joint under digital subtraction angiography. Second injections were performed 5 d after the initial injection. All patients were followed up for 6-18 mo. A modified Macnab method was used for assessing clinical outcomes after oxygen-ozone therapy.
RESULTS: Successful puncture was obtained in all patients. The overall efficacy was 91.4%; the outcome was the excellent in 37 cases (63.8%), good in 16 cases (27.6%) and fair/poor in 5 cases (8.6%) according to the Macnab criteria. No severe complications were found throughout this study.
CONCLUSION: Percutaneous intradiscal ozone injection via the posterior-lateral route and inner margin of the facet joint is effective and safe for treatment of large lumbar disc herniation.
-
Citation: Lu W, Li YH, He XF. Treatment of large lumbar disc herniation with percutaneous ozone injection
via the posterior-lateral route and inner margin of the facet joint. World J Radiol 2010; 2(3): 109-112 - URL: https://www.wjgnet.com/1949-8470/full/v2/i3/109.htm
- DOI: https://dx.doi.org/10.4329/wjr.v2.i3.109
In 2000, the Interventional Department of Nanfang Hospital, Southern Medical University, China was the first in our country to perform ozone therapy for lumbar disc herniation, and obtained good efficacy[1,2]. Because there is little pain, few complications and broad indications as well as being a minimally invasive method, ozone therapy has been widely used clinically before now[3,4]. At present, intradiscal and paravertebral injections through the posterior-lateral route are conventionally used in the treatment of lumbar disc herniation. For patients with minimal or inclusive disc herniation, the efficacy of ozone treatment is very significant, but for patients with large lumbar disc herniation, the efficacy is poor[5]. Since 2005, we have injected ozone via a route through both the posterior-lateral pathway and inner margin of the facet joint in the treatment of 58 patients with large lumbar disc herniation, and we obtained good efficacy.
From January 2005 to December 2007, 58 patients with large lumbar disc herniation were enrolled in this study. A large lumbar disc hernia was where the greatest distance between the edges of the herniated material and the edges of the base of disc were more than 5 cm. Inclusion criteria were as follows: (1) diagnosis of a herniated disc by clinical symptoms, and physical signs matched with computed tomography (CT) and/or magnetic resonance imaging; (2) sciatic pain of 5 or more on a visual analogue scale; and (3) pain radiating to an area appropriate to a herniated disc. There were 43 and 15 females, aged from 22 to 78 years (mean, 40 years). Fifty-eight patients had 69 disc herniations. The positions of the herniated disc levels were L4-L5 (n = 31), L5-S1 (n = 16) and L4-L5 combined with L5-S1 (n = 11). The disease duration ranged from 1 mo to 12 years. The disc herniation portions ranged from 5 to 8 mm, with a mean of 5.87 ± 1.72 mm.
Four patients had disc protrusion and the protruding nucleus pulposus tilted to the lower extremity; the herniated discs of 3 patients were significantly calcified, with combined bony spinal canal stenosis at the same level as the herniated discs. Patients with the following were excluded: bony spinal canal stenosis, ligamentum flavum hypertrophy, and facet joint syndrome. The main clinical manifestations were radiating pain and numbness of the unilateral or bilateral hip and lower extremity, sometimes accompanied by low back pain and sacral pain. Only one case showed interruption of urinary and fecal excretion. As for physical signs, the straight leg raising test and/or strength test were positive in 51 cases, but both were negative in 7 cases. Thirteen cases showed muscular atrophy of the unilateral limb. Ten cases showed a reduction in the flexor muscle strength of the hallux combined with hyporeflexia of the knee and/or Achilles tendon. No beneficial effect had been achieved in any patient during at least 8 wk’ conservative treatment.
Ten milligrams diazepam was intramuscularly injected 30 min before the procedure. The patients lay in the lateral position on a digital subtraction angiography (DSA) operating table, with the affected side upwards. The operation was performed under sterile conditions. In general, the puncture site was 6-10 cm (mean, 8 cm) away from the vertebral line and 5 mL of 2% lidocaine (Xian Changcheng Pharmaceutical Factory, Xi’an, China) was used for local anesthesia of the puncture site, with attention paid to avoidance of damage to the nerve roots. The 21G needle (conical needlepoint and containing 3 side-holes) was used to puncture the center of the disc under DSA, with an angle of 30-40°, with insertion along the ‘security triangle’ through the posterior-lateral pathway. Once the position of the needle tip was confirmed in the center of the disc by both posterior-anterior and lateral fluoroscopy images, 5-10 mL of 30-40 μg/mL ozone was injected. The ozone generator used in our study was made by Humazon ProMedic, Germany. While the needle tip was withdrawn to near the intervertebral foramen, paravertebral injection of 10 mL ozone and 3-4 mL of an anti-inflammatory and analgesic solution (a mixture of diprospan (Schering_Plough, Shanghai, China), vitamin B12 (Hezhong Biochemistry Co. Ltd, Wuhan, China) and lidocaine) was performed. When the puncture site was at the level of L5-S1, a pillow was placed under the healthy hip and the lumbosacral angle was increased to shift the puncture point upwards, then the needle set at an angle of 150-160° to increase the success rate of puncture and injection of ozone along the margin of the disc.
The patients lay in a prone position, and the angle of the plate of the DSA was adjusted so that its plane was perpendicular to the disc punctured, in order to show that the intervertebral space was clear, with the spinal process in the center. The puncture site was 2 cm away from the diseased spinal process in the intervertebral space and 5 mL of 2% lidocaine was injected for local infiltration anesthesia. Then a 20G needle was advanced stepwise into the hernia through the skin, subcutaneous tissue, and the space between the medial border of the articular process and the lateral border of the dural sac after the erector spinae. On meeting an obstacle, the angle of the needle was adjusted under lateral fluoroscopy to avoid the posterior margin of the vertebrae for entering the hernia, the ideal position of the needle tip being inside the herniated portion of the disc. When no blood or cerebrospinal fluid were drawn through the needle, ozone gas (5-6 mL of 30-40 μg/mL) was then injected slowly.
After ozone injection, patients were required to lie on the bed for 48 h. Later, limited activity was allowed but the duration of sitting or standing was not more than 15 min. The patients were administrated with mannitol and neurotropin for 3 d. Five days later, the treatment above was repeated. All patients were followed up by returning to the hospital to have physical examination or answering the questions by telephone. The efficacy was assessed by modified Macnab criteria[6,7]: excellent referred to return to work, but with occasional low back pain or leg pain, no need for painkillers and no physical signs of nerve root injury, and good physical fitness; good/fair referred to general ability to work, with intermittent slight low back pain or radiating pain, no need for painkillers and no physical signs of nerve root injury, and good physical fitness; poor referred to inability to work, with constant pain, requirement for painkillers, and limited physical activity, with physical signs of nerve root injury. The effective rate of the ozone therapy was assessed. The χ2 test was used to evaluate the significant difference in efficacy among the 3 sub-groups (L4-L5 group, L5-S1 group and L4-L5 combined with L5-S1 group).
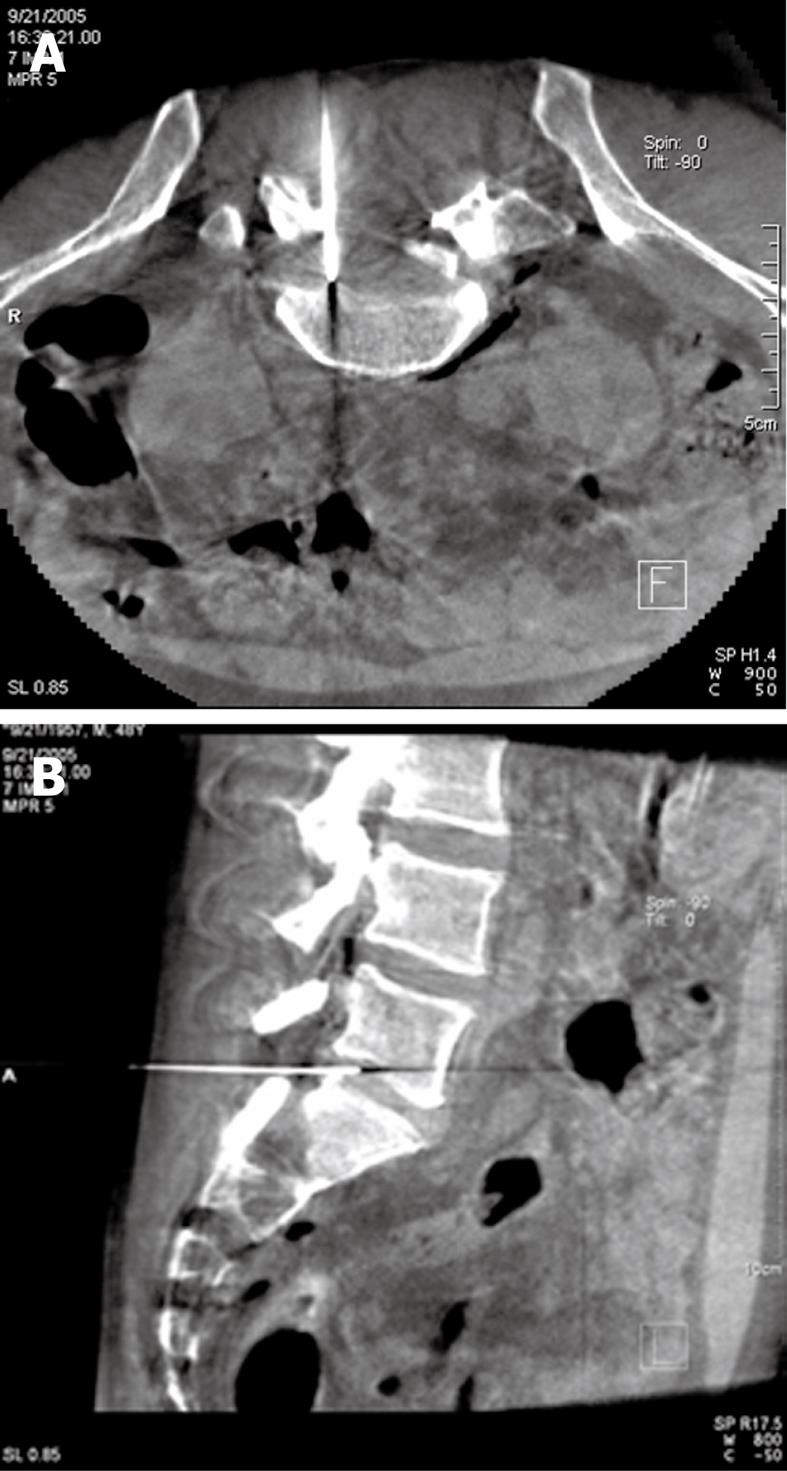
All 58 patients with 69 hernias had successful puncture via the 2 paths, a success rate of 100%. The placement of the needle tip could be measured accurately by Dyna-CT reconstruction under rotary DSA (Figure 1A and B). After injection, all patients were followed up for 6 to 18 mo (mean, 10.5 ± 4.3 mo). According to the modified Macnab criteria, the therapeutic outcomes (Table 1) were: excellent efficacy in 37 cases (63.8%), good/fair in 16 (27.6%) and poor in 5 (8.6%), and the total effective rate (excellent and good/fair) was 91.4%. The total effective rate was 96.8% for L4-L5, 87.5% for L5-S1, and 81.8% for L4-L5 combined with L5-S1. According to statistical analysis, there was no significant difference among the 3 groups of patients with disc herniation at different levels (χ2 = 4.407, P = 0.354). In this study, there were no complications such as disc infection, nerve or vascular injury, and so on.
| Herniated disc (case) | Macnab evaluation | ||
| Excellent | Good | Poor | |
| L4-L5 (n = 31) | 23 (74.2) | 7 (22.6) | 1 (3.2) |
| L5-S1 (n = 16) | 9 (56.3) | 5 (31.3) | 2 (12.5) |
| L4-L5 and L5-S1 (n = 11) | 5 (45.5) | 4 (36.4) | 2 (18.2) |
| Total | 37 (63.8) | 16 (27.6) | 5 (8.6) |
The treatment of lumbar disc herniation with ozone has been widely applied in our country, and at present, the main mechanism of action may be considered as follows[8,9]: (1) Immediate oxidation: ozone is a strong oxidizer, by which proteoglycan in the nucleus pulposus could be oxidized immediately, the osmotic pressure reduced and water lost. Then, the nucleus pulposus would denaturize, necrotize and atrophy, and the volume decrease. At the time of osmotic pressure reduction, the local blood circulation would also be changed. Increasing the oxygen supply could improve the symptoms; (2) Anti-inflammatory effect: as the nerve root and the vein and lymphoid tissue were compressed by the herniated nucleus pulposus and annulus fibrosus, the venous and lymphatic backflow was obstructed, accompanied by nerve edema and exudation. Then antigenic substances, such as glycoprotein and β-lipoprotein, could be released to induce an immune response, resulting in aseptic inflammation, adhesion, etc. All these factors could lead to the pain of disc herniation. Ozone could have an anti-inflammatory effect by releasing antagonistic immune factors; and (3) Analgesic effect: the reason that the disc herniation caused pain was that some inflammatory mediators and enzyme-products (substance P, phospholipase A2, etc.) stimulated the nerve endings on the disc surface and near ligament, the facet articular process and lumbar muscle. The strong oxidative activity of ozone could inactivate the above inflammatory mediators for pain relief.
For small- or medium-sized disc herniations and contained disc herniations, which showed that the annulus fibrosus and posterior longitudinal ligament had not has not been completely ruptured, ozone injected into the center of disc through the conventional posterior-lateral route had good efficacy. In 2003, Andreula reported a multicenter study of a large group of patients (300 cases), with excellent and good outcomes of 78.3%[10]. However, for large disc herniation, ozone could not directly remove the hernia compressing the nerve root so that the symptoms could not be eliminated quickly and the efficacy of reduced compression was limited[11]. In another aspect, because the annulus fibrosus was partially or completely ruptured, the ozone injected could diffuse through the tear into the tissues surrounding the spinal or vertebral disc, such that the nucleus pulposus and hernia could not be fully oxidized[12]. Ozone injected through the inner margin of the facet joint by directly placing the needle into the herniated disc could directly oxidize the hernia, thus the efficacy was increased. At the same time, ozone diffusing between the dura mater and hernia could relieve nerve root pain.
This study showed that the treatment of large lumbar disc herniation with percutaneous ozone injection via the posterior-lateral and inner margin of facet joint was very effective. Also, the efficacy was not significantly different among the 3 levels of herniation including L4-L5, L5-S1, and both L4-L5 and L5-S1. It was proven that the dual approach treatment had a reliable outcome. If the herniation was on the L5-S1 level, it might be difficult to puncture because of an excessively high iliac crest and hypertrophic transverse process. Thus, the needle path of the inner margin of the facet joint could be used to prevent puncture failure as a result of poor needle placement. In this way, the needle was advanced into the hernia through the gap between the lateral nerve root and the inner margin of the facet joint. However, for central herniation, the needle could be advanced through the gap between the lateral position of the nerve root and the dural sac. Because the needle was very thin and the ozone was minimally invasive for nerve root treatment, the inner margin of the facet joint approach has been a common path for minimally invasive treatment of disc herniation. Zhao[12] had performed this treatment with ozone and collagenase, with an effective rate of 94.4%. Because puncture through the inner margin of the facet joint had a straight path, a short distance, was an easy operation, and could allow ‘target’ injection, the efficacy was always good, especially for those patients with large disc herniation or prolapse. Ozone injection into or around the hernias not only improved the local ablation, but also eliminated local aseptic inflammation. The author had reported an excellent and good rate of 91.4%, which was higher than that of the route of the posterior-lateral approach only as reported by Yu et al[13], and that of the inner margin of the facet joint only as reported by Zhao[12]. Thus, the treatment of large lumbar disc herniation with percutaneous ozone injection via the posterior-lateral and inner margin of facet joint was a safe and effective method, which is worthy further promotion.
To ensure efficacy, the concentration of ozone should be adequate and the rupture of the annulus fibrosus by extremely high intradiscal pressure should be avoided. At present, there is pulse injection, low-pressure repeated injection and rapid injection with a large dose of ozone. The authors believed that, for large disc herniation, low-pressure repeat injections of ozone were preferable. By pushing and pulling the syringe repeatedly, the ozone could completely contact and oxidize the nucleus pulposus. Then the residual ozone was abandoned, and new ozone was injected repeatedly to avoid rupture of the annulus fibrosus. At the same time, the injection pressure should also be monitored by a pressure monitoring device to avoid the rupture of the annulus fibrosus.
Oxygen-ozone therapy is a minimally invasive treatment for lumbar disc herniation that exploits the biochemical properties of a gas mixture of oxygen and ozone. Oxygen-ozone therapy is a useful treatment for lumbar disc herniation that has failed to respond to conservative management.
Although intradiscal and paravertebral ozone injections through the posterior-lateral route are effective in the treatment of lumbar disc herniation, the efficacy is poor for patients with large lumbar disc herniation. We report injection of ozone via both the posterior-lateral route and the inner margin of the facet joint to successfully treat large lumbar disc herniation.
This study showed that the treatment of large lumbar disc herniation with percutaneous ozone injection via the posterior-lateral route and inner margin of the facet joint was very effective. Ozone injected via the inner margin of the facet joint, by direct placement of the needle into the herniated disc, could directly oxidize the hernia. Because of its high penetration, the efficacy was increased. The efficacy was similar for the 3 levels of herniation including L4-L5, L5-S1, and both L4-L5 and L5-S1. It was proved that the dual approach to treatment had a reliable effect.
Large lumbar disc herniation had a poor response to ozone injection via the posterior-lateral route. Ozone injected through the inner margin of the facet joint could improve the efficacy. In our study, the overall efficacy was 91.4%, excellent in 37 cases (63.8%) and good in 16 cases (27.6%). The indication for ozone therapy has expanded to include large lumbar disc herniation.
A zygapophysial joint (zygapophyseal, or facet joint) is a synovial joint between the superior articular process of one vertebra and the inferior articular process of the vertebra directly above it. There are 2 facet joints in each spinal motion segment. Large lumbar disc herniation is where the greatest distance between the edges of the herniated material and the edges of the base of disc are more than 5 cm. Dyna-CT is an innovative system for 3-dimensional reconstruction of anatomical structures.
The manuscript is generally acceptable. However, some points must be reconsidered.
Peer reviewers: Jin-Suck Suh, MD, PhD, Professor, & Chairman, Department of Radiology & Research Institute of Radiological Science, Division Head of Yonsei Nanomedical National Core Research Center, Severance Hospital, College of Medicine, Yonsei University, 134 Shinchon-dong, Seodaemun-gu, Seoul 120-752, South Korea; Wessam Bou-Assaly, MD, Department of Radiology, University of Michigan, Ann Arbor VA Health System-2215 Fuller Road, Ann Arbor, MI 48105, United States
S- Editor Cheng JX L- Editor Cant MR E- Editor Zheng XM
| 1. | He XF, Yu ZJ, Teng GJ, Li YH, Zeng QL, Chen Y, Lu W, Kong WD, Xu XL, Li L. Treatment of lumbar disc herniation by using percutaneous intradiscal and paraspinal space injection of O2-O3 mixture. Zhonghua Fangshexue Zazhi. 2003;37:827-830. |
| 2. | Yu ZJ, He XF, Chen Y, Zeng QL, Liu ZH, Zhao ZQ, Lu Y, Li YH. Percutaneous intradiscal ozone (O3)-injection: an experimental study in canines. Zhonghua Fangshexue Zazhi. 2002;36:366-369. |
| 3. | Hua SY, Xu RL, Qi B. Clinical evaluation of lumbar disc heniation treated by percutaneous lumbar discectomy associated with O3 injection. Jieru Fangshexue Zazhi. 2005;14:281-283. |
| 4. | Xiao YY, Meng XD, Li JL, Chen C. CT guided O3 injection for the treatment of lumbar disc herniation. Zhongguo Jieru Yingxiang Yu Zhiliaoxue. 2005;2:245-248. |
| 5. | He XF, Li YH, Chen HW, Lu W, Chen Y, Zeng QL, Zhao JB, Xu XL, Peng J, Shen P. Intradiscal injection of O2-O3 to treat lumbar disc herniations: clinical therapeutic effect analysis with 600 cases. Zhongguo Jieru Yingxiang Yu Zhiliaoxue. 2005;2:338-341. |
| 6. | Nerubay J, Caspi I, Levinkopf M. Percutaneous carbon dioxide laser nucleolysis with 2- to 5-year followup. Clin Orthop Relat Res. 1997;45-48. |
| 7. | Macnab I. Negative disc exploration. An analysis of the causes of nerve-root involvement in sixty-eight patients. J Bone Joint Surg Am. 1971;53:891-903. |
| 8. | Muto M, Andreula C, Leonardi M. Treatment of herniated lumbar disc by intradiscal and intraforaminal oxygen-ozone (O2-O3) injection. J Neuroradiol. 2004;31:183-189. |
| 9. | Arena M, Savoca G, Papa R. Paravertebral percutaneous O2-O3 injection integrated treatments in the management of lunbar herniated disc and disc-joint compression. Ital J Ozono Ther. 2003;2:39-44. |
| 10. | Andreula CF, Simonetti L, De Santis F, Agati R, Ricci R, Leonardi M. Minimally invasive oxygen-ozone therapy for lumbar disk herniation. AJNR Am J Neuroradiol. 2003;24:996-1000. |
| 11. | Wang DJ, Zhang L, Wang XM, Xiao YY. Treatment of huge lumbar intervertebral disc herniation with ozone and collagenase through the route of inner margin of facet joint. Shiyong Tengtongxue Zazhi. 2007;3:22-27. |
| 13. | Yu ZJ, He XF, Li YH. Treatment of lumbar disc herniation with medical ozone. Zhongguo Yixue Yingxiang Jishu. 2004;20:598-600. |