CURRENT IMAGING TECHNOLOGIES
Currently, there are three intraoral digital sensors available in the market including a charge-coupled device with a direct digital receiver, complementary metal oxide semiconductor, and photostimulable phosphor plate with an indirect digital image receiver. The digital intraoral receptors may cause problems for the patient and the operator during radiographic procedures. Patients may feel uncomfortable and may not tolerate the detector in the mouth during imaging procedures. Thus, positioning errors may occur, which influences the quality of obtained images and negatively affects diagnostic accuracy[1,2].
Periapical radiographic imaging
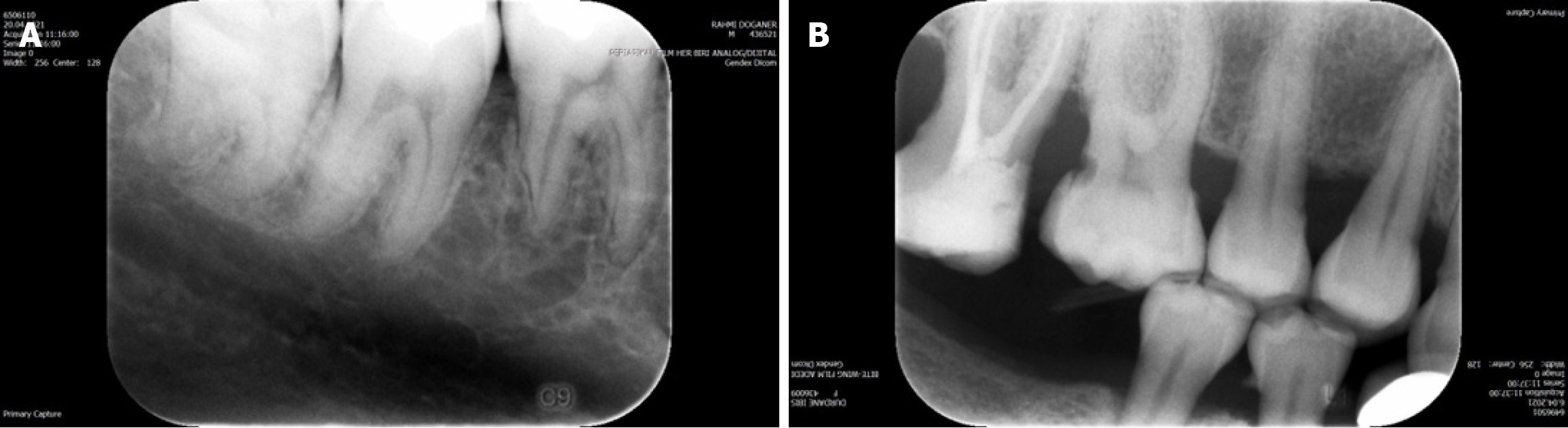
Periapical radiographic examination using a paralleling technique is an adjunct to the clinical examination and provides important information regarding periapical tissues. It has the advantage of showing the entire crown and periapical region of the teeth, which provides crucial information to aid in the diagnosis of the most common dental diseases such as periodontal and periapical pathology. Patient and tooth-related factors, basic principles of aiming techniques, and projection geometry are all important factors to provide accurate information[1,2]. Figure 1A shows a periapical image taken from a patient with replacement external root resorption visible on the distal root surface of the right mandibular first molar tooth. Detailed root and bone structures are discernable but limited to the two-dimensional (2D) view.
Figure 1 Periapical radiographic examination.
A: Periapical image taken from a patient with replacement external root resorption visible on the distal root surface of right mandibular first molar tooth. As can be seen, detailed root and bone structures were discernable but limited to a two-dimensional view; B: Bitewing image taken from a patient with alveolar bone destruction between the right maxillary first and second molar teeth along with a proximal caries on the distal surface of the first maxillary right molar.
Bite-wing radiographic imaging
Bite-wing radiographs are utilized to image interproximal surfaces of teeth and restorations to diagnose caries, periodontal disease, and inaccurate contours of various restorations[3]. Figure 1B shows a bitewing image taken from a patient with alveolar bone destruction between the right maxillary first and second molar teeth along with a proximal caries on the distal surface of the first maxillary right molar.
Panoramic radiographic imaging
In addition to intraoral radiographic imaging techniques, panoramic radiographic systems are frequently utilized in daily dental clinical practice. By panoramic radiography, images are formed by the simultaneous rotation of the detector and X-ray source around the stationary patient. Panoramic images have some drawbacks such as unequal magnification, superimposition of structures, and geometric distortion. Therefore, clinicians should use caution when evaluating linear measurements conducted on panoramic radiographic images. The magnification ratio on panoramic radiographs is influenced by several factors such as variations in technical equipment, head positioning, and the patient. In order to decrease image distortion and magnification for better diagnostic quality without ghost images, correct preparation and positioning of patients are essential.
Extensive general coverage of both mandible and maxilla and teeth is obtained but with less anatomical detail discernable in the images obtained by intraoral periapical radiography[4]. Figure 2A shows a patient with fixation screws and no visible alveolar bone defect in the mandibular anterior region on cropped panoramic radiography. Significant bone loss is evident around the right mandibular lateral incisor on cropped periapical radiography. Figure 2B shows a 35-year-old male patient with a vague radiopacity in the maxillary anterior region on cropped panoramic radiography. A clearly depicted inverted mesiodens tooth is evident between maxillary incisors on cropped periapical radiography. Figure 2C shows a cropped panoramic image of a 55-year-old male patient with aggressive periodontitis and two horizontally impacted canine teeth visible on the mandibular anterior region. Also, a well-defined round Stafne bone cavity can be seen on the right mandibular region extending under the mandibular canal.
Figure 2 Panoramic images.
A: Patient with fixation screws and no visible alveolar bone defect in the mandibular anterior region on cropped panoramic radiography. Significant bone loss was evident around the right mandibular lateral incisor on cropped periapical radiography; B: A 35-year-old male patient with a vague radiopacity in the maxillary anterior region on cropped panoramic radiography. A clearly depicted inverted mesiodens tooth was evident between the maxillary incisors on cropped periapical radiography; C: Cropped panoramic image of a 55-year-old male patient with aggressive periodontitis and two horizontally impacted canine teeth visible on the mandibular anterior region. Also, a well-defined round Stafne bone cavity can be seen on the right mandibular region extending under the mandibular canal.
Cone beam CT
New technologies have been introduced and have evolved in recent years since periapical and panoramic radiographs are limited to 2D visualization and therefore cannot display complex three-dimensional (3D) anatomical structures and related pathologies. Cone beam CT (CBCT) specifically offers 3D images of the dentomaxillofacial region and is considered an important and useful diagnostic tool for clinical dentistry. A very compact CT machine specially designed for dental applications was introduced by Arai et al[5] in 1999. It was first named “Ortho-CT” and was a CBCT device for dental applications. The equipment allows lower radiation doses than medical CT with fast scanning options while being cost effective and user-friendly. In addition, image distortion is minimal, and data are compatible with many software applications used for dentistry-related applications and software[5-13].
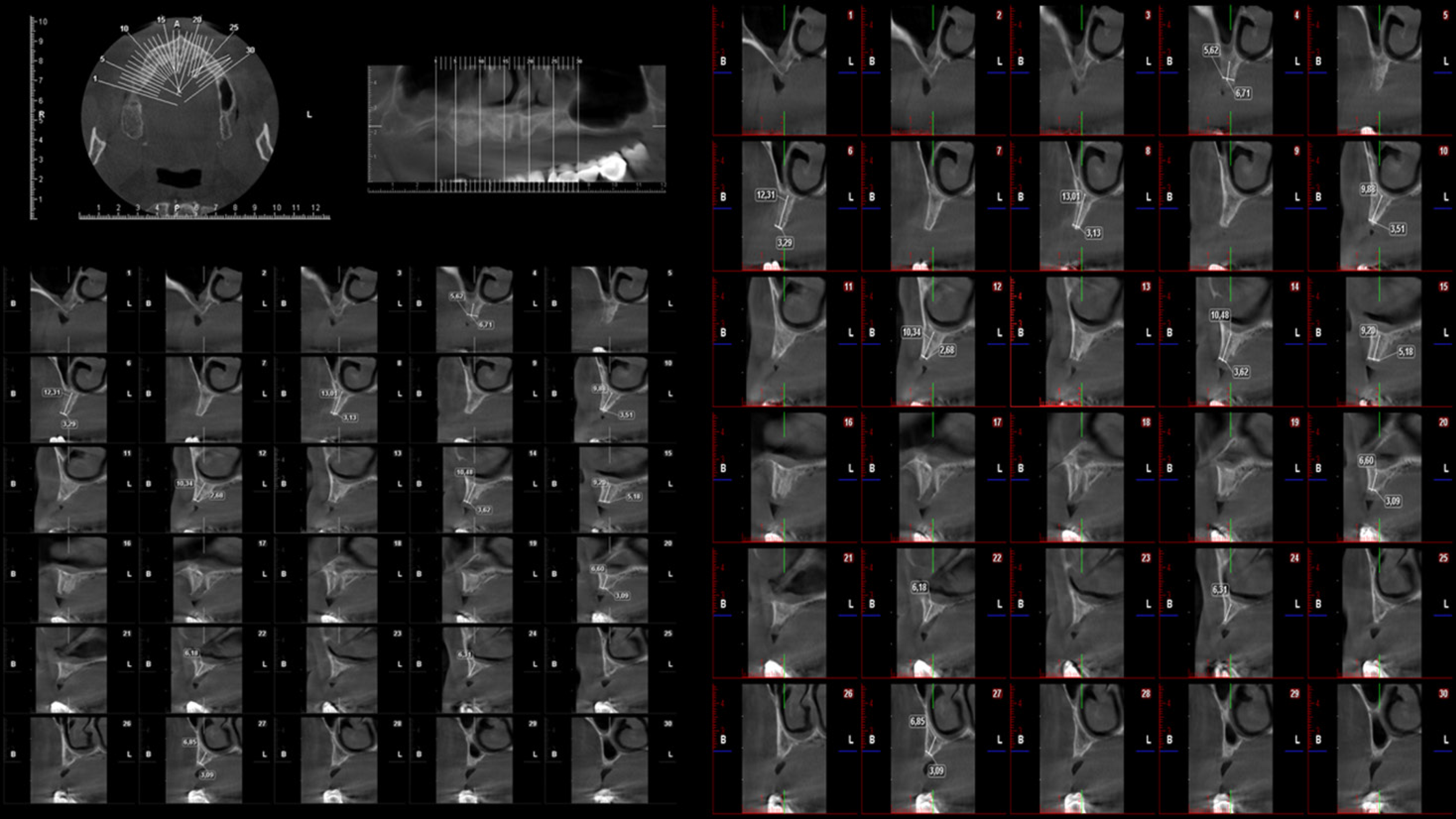
Introduction of this cutting-edge innovative technology caused a paradigm shift in oral and maxillofacial radiology because it outperformed 2D imaging and medical CT. Therefore, CBCT is now the method of choice in oral and maxillofacial implantology, endodontics, maxillofacial surgery, periodontics, degenerative temporomandibular joint (TMJ) disease, orthodontics, airway studies, sleep disorders, and forensic dentistry. The main drawbacks of CBCT systems are low soft tissue contrast and low correlation with Hounsfield units[5-13]. Figure 3 shows multiplanar reformatted reconstruction images of a 60-year-old male patient requiring implant treatment referred for CBCT imaging. Reformatted axial, panoramic, and cross-sectional images obtained at implant planning indicated severe maxillary bone resorption.
Figure 3 Multiplanar reformatted reconstruction images of a 60-year-old male patient requiring implant treatment referred for cone beam CT imaging.
Reformatted axial, panoramic, and cross-sectional images obtained at implant planning mode indicated severe maxillary bone resorption.
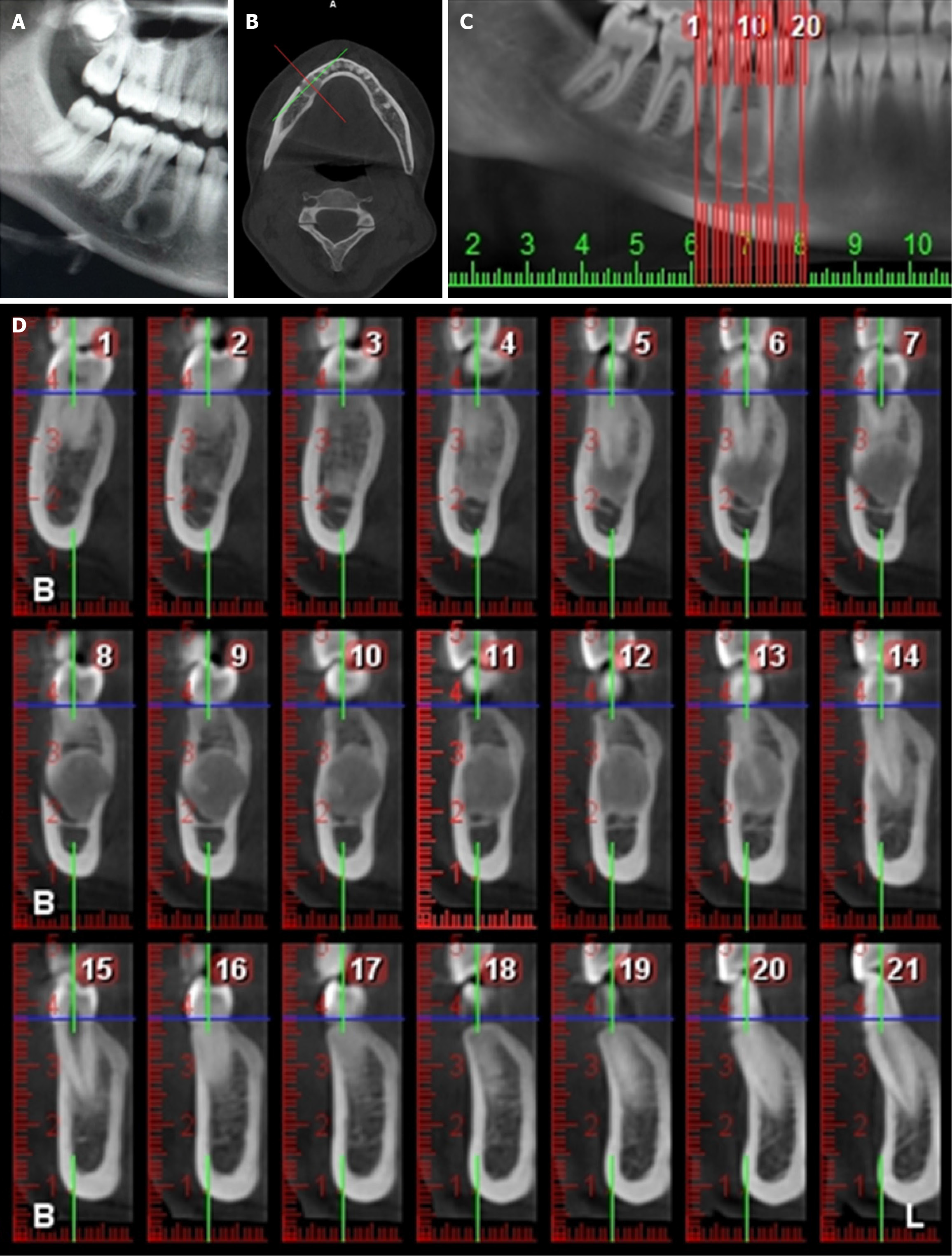
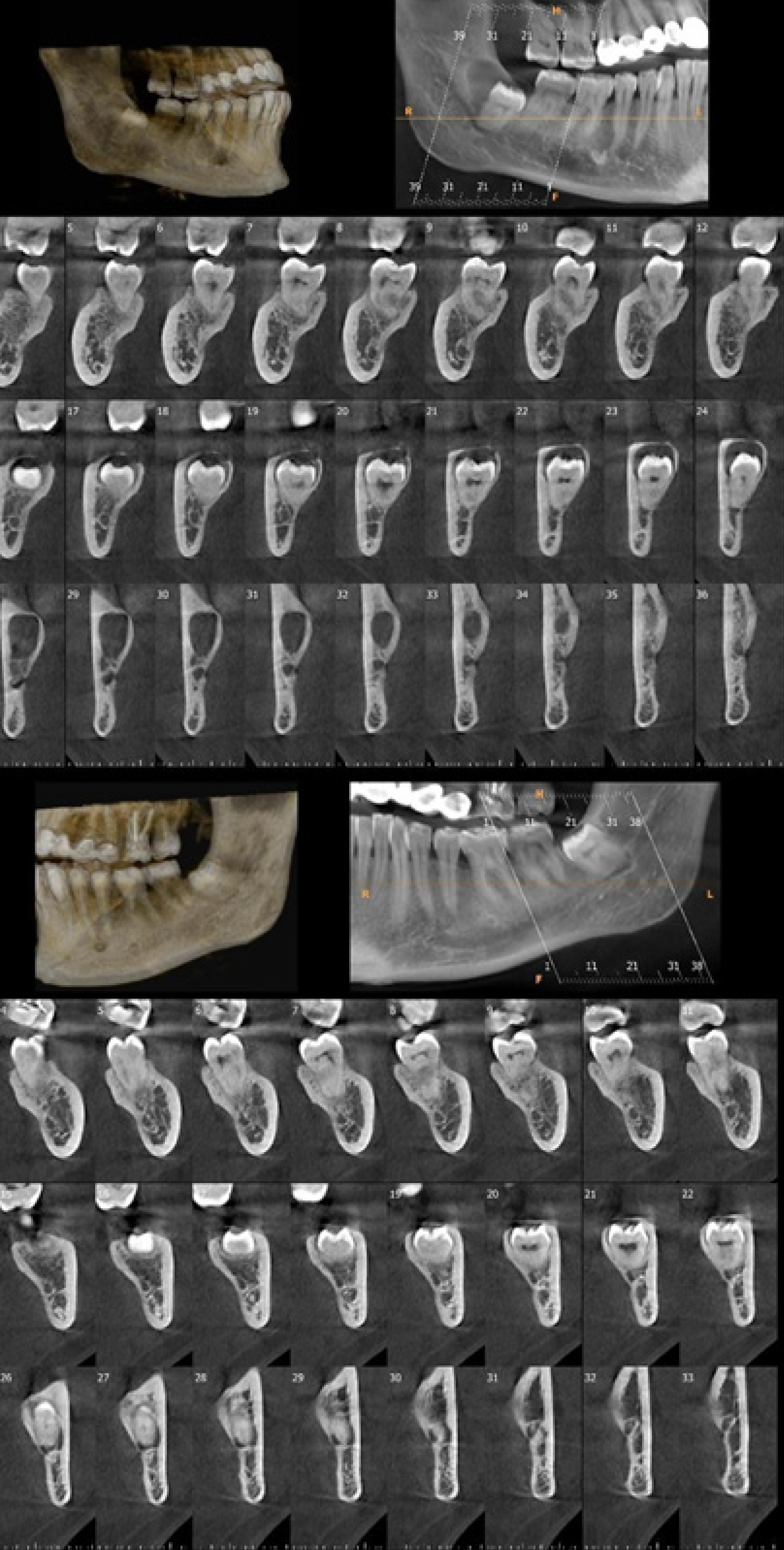
Diagnostic X-ray images of a 16-year-old female patient with histopathologically confirmed cemento-ossifying fibroma between the mandibular right premolar teeth. A well-defined lesion was visible on 2D panoramic X-ray image (Figure 4A), reformatted axial CBCT image (Figure 4B), reformatted panoramic CBCT image (Figure 4C), and reformatted cross-sectional CBCT images (Figure 4D). The mixed radiopacity degree of the inner structures of the lesion was observed in different CBCT sections and were not detectable on 2D panoramic radiography. Figure 5 shows CBCT images of mandibular right (upper image) and left (lower image) 3rd molar teeth of a 25-year-old female patient referred for persistent pain on both retromolar sides. A dentigerous cyst related to the mandibular right third molar tooth and direct contact of the mandibular left third molar tooth root with mandibular canal were visible on the 3D bone model and panoramic and cross-sectional images.
Figure 4 Diagnostic X-ray images of a 16-year-old female patient with histopathologically confirmed cemento-ossifying fibroma between the mandibular right premolar teeth.
A-D: Two-dimensional panoramic X-ray image (A), reformatted axial cone beam CT (CBCT) image (B), reformatted panoramic CBCT image (C), and reformatted cross-sectional CBCT images (D) showed a well-defined lesion. The mixed radiopacity degree of the inner structures of the lesion observed in different CBCT sections was not detectable on two-dimensional panoramic radiography.
Figure 5 Cone beam CT images of mandibular right (upper image) and left (lower image) third molar teeth of a 25-year-old female patient referred for persistent pain on both retromolar sides.
Three-dimensional bone model, panoramic, and cross-sectional images showed a dentigerous cyst related to the mandibular right third molar tooth and direct contact of mandibular left third molar tooth root with mandibular canal.
Micro-CT
Another innovative laboratory research tool that offers 3D detailed high-resolution images of in vitro teeth and neighboring structures with submicrometric accuracy is micro-CT. Micro-CT offers highly accurate tooth, periodontal tissue, and bone structure images in 3D view. Also, unlike histological examination, specimens are not sectioned for visualization. Therefore, this technique is considered a noninvasive and nondestructive method. Today, micro-CT is used in several in vitro conditions and is accepted as the gold standard technique for trabecular and cortical bone assessment, evaluation of implant osseointegration and microstructure, dental caries and root canal treatment assessment, evaluation of the development of the skull bones, and tissue engineering. However, its routine clinical usage is not possible yet due to extremely high effective radiation doses, extra-long scanning and reconstruction times, and high costs[14-16].
Ultrasonography
Considering stochastic and deterministic effects of X-ray radiation in living organisms, there has always been an attempt to search for alternative techniques that do not use ionizing radiation. There has always been a need for a method that could provide on-site and real time images by using a cost-effective, rapid, user-friendly, and portable technique without ionizing radiation, and therefore some authors proposed ultrasound (US) imaging as an alternative to X-ray imaging techniques. A frequency range of 2-20 MHz is generally utilized in diagnostic settings. In US, transducer sound waves with high frequency are transmitted into the patient and echoes from the tissue interface are assessed and displayed on a monitor. The emission of sound waves is achieved via piezoelectric crystals located in the US transducer[17-27].
Use of US is popular in the examination of the dentomaxillofacial region. There are several indications of US in the head and neck region as follows: Assessment of major salivary gland lesions (specifically salivary stones not visible on X-ray images); examination of bone and superficial soft tissue; evaluation of temporomandibular joint and disorders; assessment of some fractures and vascular lesions; lymph node examination; visualization of vessels of the neck; and muscle thickness measurement. It can also be used in the determination of the origin of periapical lesions and follow-up of periapical lesion treatment. Moreover, the detection of periodontal defects and their measurement and gingival thickness measurement before dental implant placement can be conducted.
US is a reliable method for the assessment of the depth of invasion and lymph node metastases, which are important prognostic parameters for tongue cancer. Doppler US is a useful tool to examine congenital vascular lesions of the maxillofacial region. Doppler US could be used to characterize the flow of head and neck vascular anomalies and to differentiate hemangiomas from other vascular lesions. The main drawback of US is that its only effective in the evaluation of superficial tissues and is unable to propagate in bone[17-27].
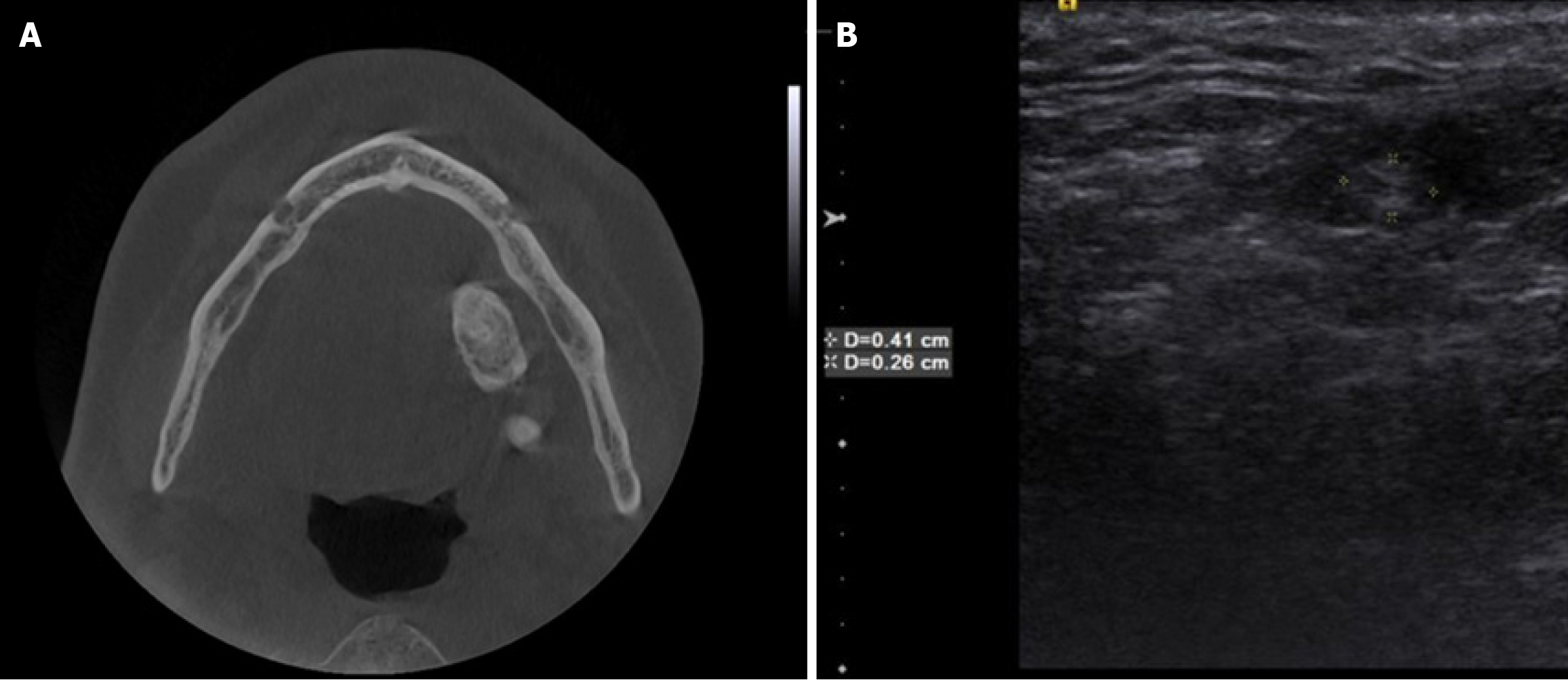
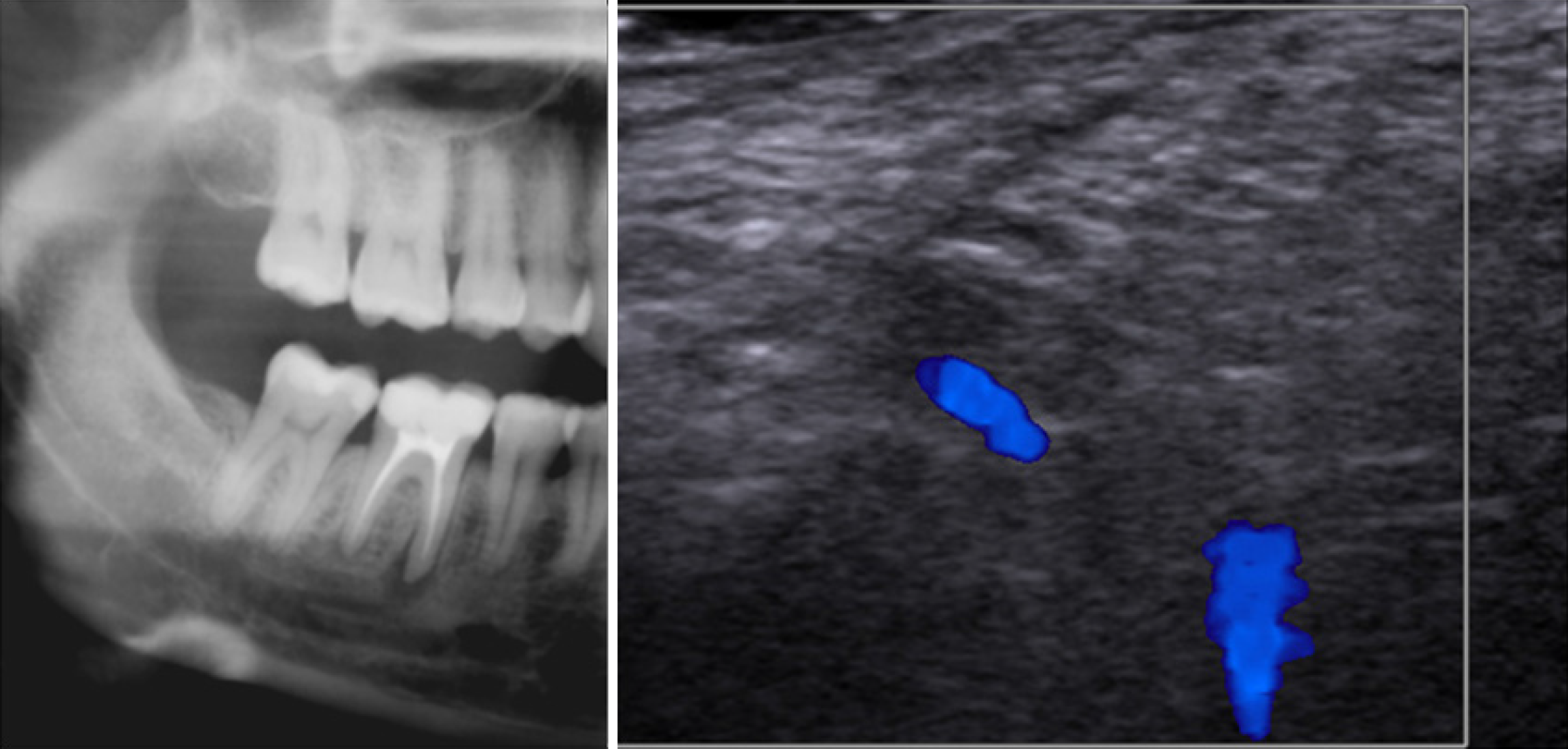
Figure 6 shows axial CBCT (Figure 6A) and US (Figure 6B) images of a 25-year-old female patient referred to our clinic with the complaints of pain and swelling of the cheek after meals. The radiopaque lesion on CBCT and hyperechoic lesion on US in the submandibular region are suggestive of a submandibular sialolithiasis. Figure 7 shows cropped panoramic radiography (left) and laser Doppler US of a 30-year-old female patient referred for slight percussion sensitivity in the right mandibular first molar region. On panoramic radiography a well-defined radiolucent lesion on the mesial root of the first mandibular right molar was visible. Laser Doppler US evaluation revealed that there was blood flow in the region suggestive of a granuloma, which was confirmed by histopathological examination.
Figure 6 Axial cone beam CT and ultrasonographic measurement images.
A and B: Axial cone beam CT (A) and ultrasonographic measurement (B) images of a 25-year-old female patient referred to our clinic with the complaints of pain and swelling of the cheek after meals. The radiopaque lesion on cone beam CT and hyperechoic lesion on ultrasound images in the submandibular region were suggestive of a submandibular sialolithiasis.
Figure 7 Cropped panoramic radiography (left) and laser doppler ultrasonographic image of a 30-year-old female patient referred for slight percussion sensitivity in the right mandibular first molar region.
On panoramic radiography, a well-defined radiolucent lesion on the mesial root of the first mandibular right molar was observed. Laser Doppler ultrasonographic evaluation revealed that there was blood flow in the region suggestive of a granuloma, which was proved by histopathological examination.
Magnetic resonance imaging
Poor soft tissue visualization by using common dental radiological techniques is a critical problem. Recently, 3D magnetic resonance imaging (MRI) assessment of dentomaxillofacial structures has become popular due to high-contrast sensitivity of MRI to tissue differences without ionizing radiation. In MRI, radio waves and the magnetic field are used interactively to obtain accurate and detailed images of tissues and structures within the body. Large tube-shaped magnets are used to interact with the water molecules in the body. Aligned water molecules create signals with the stimulation of radio waves, and cross-sectional MRIs are obtained.
MRI can be used for the examination of oral and maxillofacial lesions particularly those involving soft tissues and intracranial and extracranial lesions[28-32]. MRI is the method of choice and gold standard for imaging TMJ anatomy and abnormalities. All TMJ related structures such as the disk, fibrous tissue, and muscle as well as effusion in the joint can be assessed without ionizing radiation. Bone cortex, bone marrow, and cartilage can also be assessed[22,32]. Recently, dental dedicated MRI with appropriate software, hardware, sequences, and field of view tailored to fit dentomaxillofacial anatomy was introduced. This specific dental MRI has the strong potential to be used for TMJ assessment, orthodontic planning, and evaluation of bone loss and inflammation that occur during endodontic and periodontal diseases and third molar extraction planning[33,34]. Figure 8 shows open mouth sagittal T1 MRI of a 65-year-old female patient with pain and limitation during chewing suggesting anterior disc displacement without reduction.
Figure 8
Open mouth sagittal T1 magnetic resonance image of a 65-year-old female patient with pain and limitation during chewing suggested anterior disc displacement without reduction.
3D printing technology
Lately, 3D printing technologies and their applications in dentistry has attracted attention. 3D printing is a process in which a material is added one by one in consecutive layers to form a 3D object. There are three steps in clinical dentistry: (1) Obtaining digital data using a scanner and/or CBCT; (2) Processing of and design by using a specific software application; and (3) Manufacturing of the object by 3D printing. CBCT offers highly accurate dental and cross-sectional images that are critical for producing precise printed guides. Specific printing machines producing only dental applications are currently sparse. Precision and reproducibility of additive technologies should be improved for certain dental applications.
Further research is being conducted to evaluate their versatility for different dentistry-related tasks. Increased accuracy should not be at the cost of the speed of production. With technological advancements, the use of 3D printing technology in dentistry will become more popular and usable. Currently, equipment prices have decreased, and there are several companies that produce accurate machines at reasonable prices. The availability of economical bench-top printers, self-motivated and educated staff, and financial support will encourage the use of 3D printing in routine dental applications. 3D printing may decrease operation time, eliminate clinician bias, and procedural errors. Current dental research regarding 3D printing should focus on reducing the cost and production time, increasing surface quality, and improving the process reproducibility of innovative printing materials[35-39].
Today, use of 3D printed surgical guides has been strongly recommended in implantology. The accuracy of surgical guides produced using stereolithography showed an angular deviation of 2° and linear deviation of 1.1 mm at the hex and 2 mm at the apex[36]. 3D printing can also guide calcified root canal treatment, periapical surgery, and autotransplantation[37,38]. We anticipate that the use of 3D printers in endodontics, periapical surgery, and maxillofacial surgery will become more specific and sophisticated in the future.
A reproducible, reliable, and useful clinical technique to create accurate models for obturator prostheses fabrication without using conventional impression techniques was developed[39]. In addition, in combination with arthrocentesis, application of occlusal splints produced by 3D printed occlusal splints were more effective than conventionally produced ones[40].
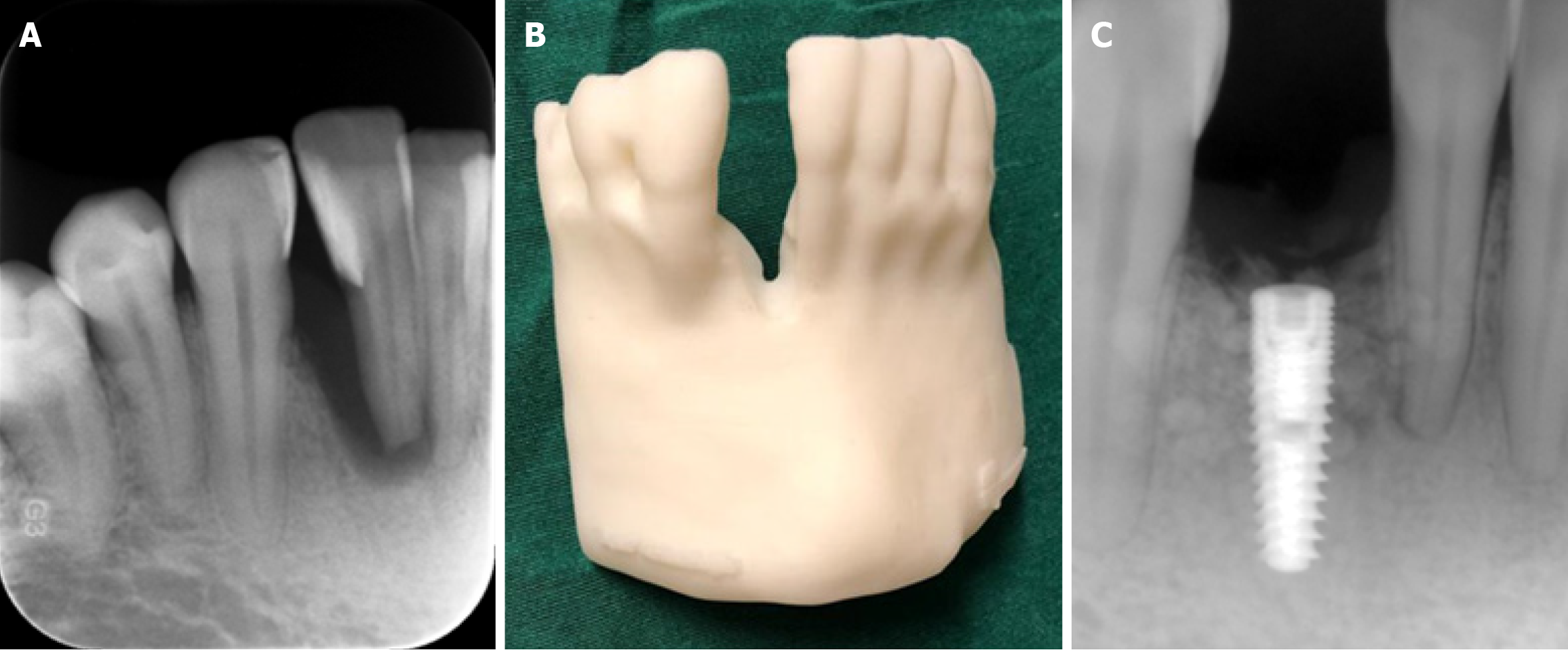
Oral and maxillofacial radiology specialists (OMFRs) will play a significant role in providing, assessing, and reporting diagnostic images to be used for dental 3D printing. OMFRs will actively participate in planning, designing, and printing of clinically useful guides. As information, techniques, and materials advance, OMFR postgraduate programs should implement 3D dental printing as part of their curriculum. Active, self-motivated, and young OMFRs should be encouraged to improve the knowledge and practice regarding 3D dental printing. Research regarding parameters for obtaining optimum quality CBCT images required for 3D dental printing are essential[35-40]. Advancements in technology, decreased costs, and increased expertise will allow OMFRs to make informed decisions regarding employment in clinical practice[35-40]. Figure 9 shows an intraoral periapical image (Figure 9A) and 3D printed bone model (Figure 9B) of a patient from CBCT data obtained in order to assess a right mandibular anterior lateral tooth for implant placement. According to diagnostic images and a 3D bone model an implant was successfully placed in the anterior lateral incisor region as can be seen from the postoperative periapical image (Figure 9C).
Figure 9 Cone beam CT images.
A-C: Intraoral periapical image (A) and three-dimensional printed bone model (B) of a patient from cone beam CT data obtained in order to assess right mandibular anterior lateral tooth for implant placement; C: According to diagnostic images and the three-dimensional bone model, an implant was successfully placed in the anterior lateral incisor region of the patient as can be seen from the postoperative periapical image.
ARTIFICIAL INTELLIGENCE
Another hot topic regarding dentomaxillofacial radiology is artificial intelligence (AI), which is a field related to computer science dedicated to developing systems or machines that can perform tasks traditionally associated with human intelligence. In dentomaxillofacial radiology studies, this technology became very popular due to its compatibility with diagnostic imaging methods. Currently some studies conducted on radiological images are as follows: Early detection of dental diseases; classification and segmentation of teeth; automatic identification of anatomical structures and cephalometric analysis; gingival and periodontal diseases; and evaluation of risk groups[41-44]. With the use of AI algorithms, it is possible to critically analyze dental periapical radiographs, panoramic images, and CBCT scans, patient data, medical history, and intraoral scans to assist in treatment planning. AI algorithms can also analyze patient data to predict oral health outcomes and identify individuals at higher risk of developing certain dental conditions[41-44].
AI has the potential to revolutionize dentistry, and this approach proved to be accurate, time and cost effective, and consistent for creating a maxillofacial diagnostic analytic informative data. Today, researchers are becoming increasingly enthusiastic about conducting AI research. Initial costs are high, and diagnoses made by various algorithms may not be analogous to real clinical scenarios. Dental and maxillofacial radiology-related AI studies revealed moderately successful results in consideration to complex patient and disease physiology. AI can only be accepted as a supplementary method, but it cannot be considered a substitute for human knowledge, experience, capabilities, and decision-making abilities. It is essential to validate the consistency and versatility of various deep learning algorithms by using representative images from different sources in comparison to real “gold standards” before implementing these techniques to real clinical situations. Therefore, further research in the field of AI is essential and has the strong potential to make great contributions to dental and maxillofacial radiology[41-44].
CONCLUSION
More than a century has passed since the introduction of X-rays to dental diagnostic field. During that time period researchers have been able to increase dental image quality with decreased effective radiation doses to patients and healthcare workers. Considering current literature and defacto clinical settings, intraoral periapical and bitewing imaging are the first method of choice for the assessment of one to four teeth with high detail but without the third dimensional assessment available. Panoramic radiography is also used for the routine evaluation of both jaws in 2D without the detail provided by intraoral imaging. Therefore, in the current clinical settings panoramic radiography should be used to evaluate the general bone and tooth structures of both jaws. This technique should be supported by bitewing and periapical imaging for the evaluation of periapical pathology, caries, fracture, and resorption, etc, and pathologies related to teeth assessment when needed[1-4].
Moreover, where 3D periapical, inner structure and bone assessment of the dentomaxillofacial region are necessary CBCT appropriately limited to an accurate field of view should be taken. Clinicians should use caution when prescribing CBCT images as applying radiation to a patient is always a risk, and indications should be selected on a case-by-case basis depending on the expertise. Currently, CBCT can be used for the diagnosis, treatment planning, and follow-up of selected cases in periapical lesions, dental anomalies, root canal treatment, dentomaxillofacial trauma, third molar surgery, implant planning, periodontal furcal lesions, several maxillofacial surgery cases, and jaw lesions[5-13].
Marketing of dental MRI is on the way and will be in use in the near future. MRI is currently the method of choice for the evaluation of TMJ. Also, MRI and medical CT can be used for the differentiation of some bone and soft tissue pathologies related to detomaxillofacial region[28-32]. US is now utilized in dentistry for the evaluation of salivary glands but it is also used for the examination of different superficial soft tissue, bone tissue, and periapical pathologies and fractures. However, specific US equipment with an innovative dental probe is necessary to implement US technology totally into routine dental clinical practice[17-27].
3D printed models have been successfully used in implant dentistry. Due to expired patents and available economical printers and biocompatible materials, the use of 3D models has extended to many fields like endodontics, periapical surgery, maxillofacial and orthognatic surgery, occlusal splint production, and maxillofacial prosthodontics[35-40]. Currently, AI studies in dentistry are conducted by some groups but they are in the research phase. Some key AI and deep learning algorithms are now available for caries and pathology recognition. Also, there are some good examples of algorithms used for dental education. The main drawback of published studies related to AI are the lack of prominent sound data and gold standard findings[41-44].
It is obvious that further investigation and research in the field of dentomaxillofacial radiology will make great contributions to diagnostic imaging for various dental specialties. It is expected that contemporary imaging techniques along with the use of deep learning algorithms will help to reduce the daily working hours of dental professionals and false diagnosis in dental practice. It should be noted that diagnostic images obtained from the dentomaxillofacial region may also show some parts or the entire nasal fossa, paranasal sinuses, airway, cervical vertebrae, and temporal bone. Incidental findings may require follow-up, and different treatment options may be identified in conjunction with clinical findings, including referral to a medical specialist in certain cases.