Published online Aug 28, 2024. doi: 10.4329/wjr.v16.i8.317
Revised: July 15, 2024
Accepted: July 23, 2024
Published online: August 28, 2024
Processing time: 132 Days and 23.4 Hours
Minimally invasive surgery (MIS) and craniotomy (CI) are the current treatments for spontaneous supratentorial cerebral haemorrhage (SSTICH).
To compare the efficacy and safety of MIS and CI for the treatment of SSTICH.
Clinical and imaging data of 557 consecutive patients with SSTICH who underwent MIS or CI between January 2017 and December 2022 were retro
In both conventional statistical and binary logistic regression analyses, the MIS group had a better outcome. The outcome of propensity score matching was unexpected (odds ratio: 0.582; 95%CI: 0.281–1.204; P = 0.144), which indicated that, after excluding the interference of each confounder, different surgical modalities were more effective, and there was no significant difference in their prognosis.
Deciding between MIS and CI should be made based on the individual patient, considering the hematoma size, degree of midline shift, cerebral swelling, and preoperative Glasgow Coma Scale score.
Core Tip: We compared the efficacy and safety of minimally invasive surgery (MIS) and craniotomy (CI) for spontaneous supratentorial cerebral haemorrhage in 557 patients. The prognostic outcome, based on the modified Rankin Scale (mRS) score at 3 months, was evaluated, an mRS score of 0–2 was considered favourable. Before propensity score matching, those who received MIS had a better outcome; however, after accounting for confounding variables, the prognosis was comparable to patients who underwent CI. Deciding between MIS and CI depends on the individual patient, considering the hematoma size, degree of midline shift, cerebral swelling, and preoperative Glasgow Coma Scale score.
- Citation: Xiao ZK, Duan YH, Mao XY, Liang RC, Zhou M, Yang YM. Traditional craniotomy versus current minimally invasive surgery for spontaneous supratentorial intracerebral haemorrhage: A propensity-matched analysis. World J Radiol 2024; 16(8): 317-328
- URL: https://www.wjgnet.com/1949-8470/full/v16/i8/317.htm
- DOI: https://dx.doi.org/10.4329/wjr.v16.i8.317
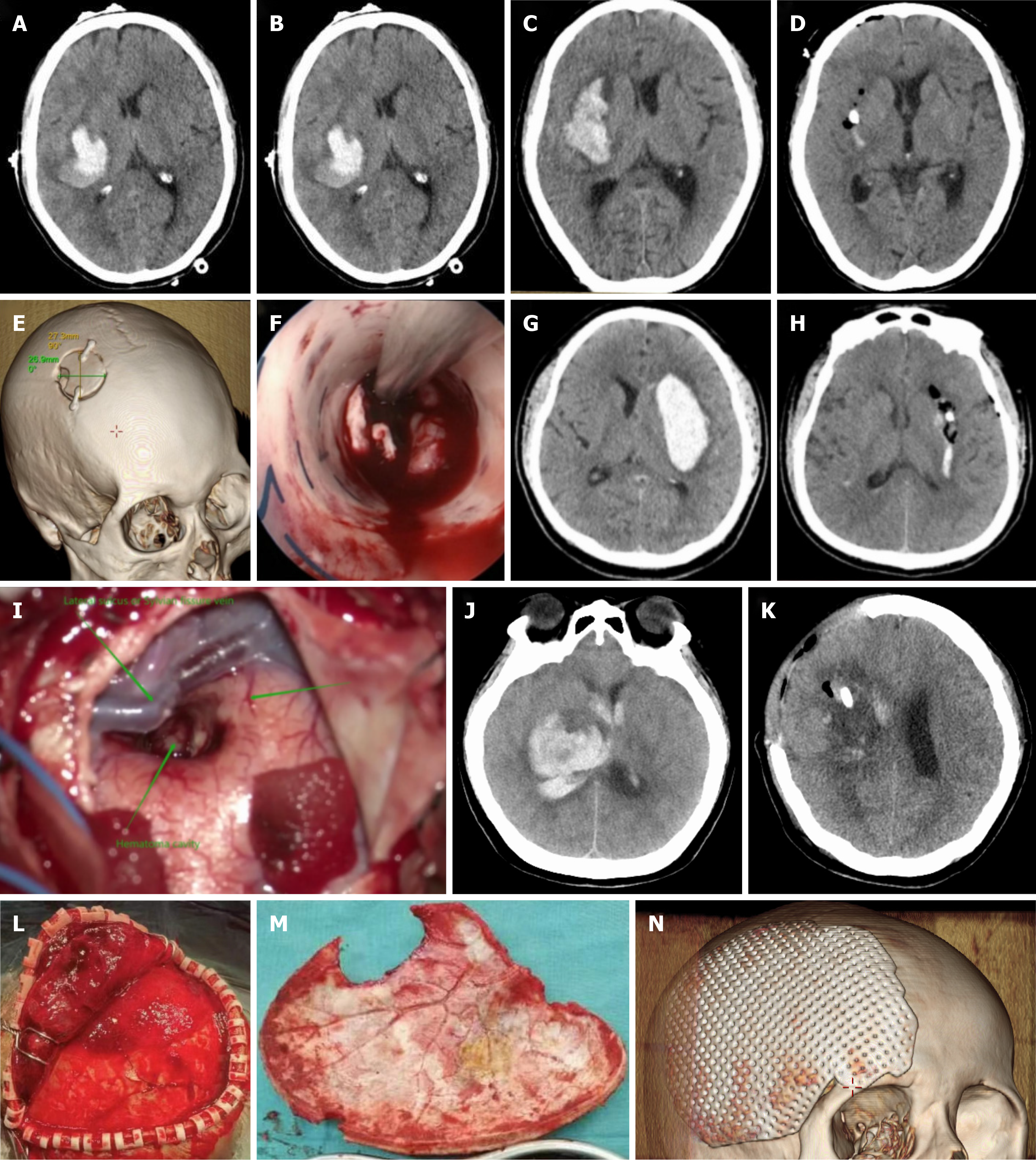
Spontaneous cerebral haemorrhage (SICH) is defined as the spontaneous, non-traumatic rupture of a cerebral blood vessel. Non-traumatic cerebral haemorrhage accounts for 10%–15% of all strokes and is characterised by high morbidity, mortality, and disability[1-3]. If patients with SICH lack prompt and effective pharmacological or surgical treatment, they frequently deteriorate rapidly, which can lead to death, a vegetative state, or loss of function. There are well-established pathophysiological benefits to hemostasis and clot removal in SICH[4-6]. Currently, the surgical treatment for SICH consists of two main procedures: Minimally invasive surgery (MIS) (Figure 1A–F), which includes endoscopic and stereotactic puncture and drainage, and craniotomy (CI), which includes standard CI (Figure 1G–N) and decompressive craniectomy (DC) with hematoma evacuation[4-8]. CI can quickly and effectively remove intracranial hematoma and reduce the mass effect and cytotoxicity of blood substances, thus reducing intracranial pressure (ICP) and preventing brain herniation, which is an important means of saving the lives of patients; however, it results in extensive trauma to brain tissues. Additionally, a series of complications may occur after decompression, which may require further se
Some studies have indicated that MIS is safer and more effective than CI[9,17]. To investigate the safety and efficacy of MIS and CI in the treatment of spontaneous supratentorial cerebral haemorrhage (SSTICH), we retrospectively analysed the clinical and computed tomography (CT) data of these patients and compared the outcomes between patients who underwent MIS with those who underwent CI using a propensity-matched analysis.
All data were obtained from patients with SSTICH who were admitted between January 2017 and December 2022 at The Second Affiliated Hospital of the University of South China. The inclusion criteria for this study were: (1) Episodic cerebral haemorrhage, including basal ganglia haemorrhage and lobar haemorrhage; (2) First-time presentation of cerebral haemorrhage; (3) Age ≥ 18 years; (4) Follow-up time ≥ 12 months; and (5) Patients who underwent MIS or CI in our hospital. The exclusion criteria were as follows: (1) Cerebral haemorrhage due to intracranial tumours, aneurysms, arteriovenous malformations, trauma, cerebral infarction, or other intracranial pathologies; (2) Multiple intracranial haemorrhages; (3) Coagulation disorders or history of anticoagulant medication use; (4) History of severe stroke, cardiac, renal, hepatic, or pulmonary dysfunction; (5) Bilateral pupil dilatation at the time of admission; (6) Subcranial cerebral haemorrhage, including cerebellar haemorrhage and brain stem haemorrhage; (7) Incomplete or missing follow-up information; and (8) Patients who did not undergo surgical treatment. Ethical approval was obtained from the Clinical Research Ethics Committee, The Second Affiliated Hospital of University of South China. The requirement for informed consent was waived due to the retrospective nature of the study.
All patients with SSTICH were treated according to the latest Guidelines for the Treatment of Spontaneous ICH deve
Postoperatively, patients were managed according to the standard United States guidelines for SICH[18]. All patients were admitted to the intensive care unit (ICU) for custodial treatment, and head and chest CT scans were performed within 24 hours to assess hematoma clearance, the presence of recurrent cerebral haemorrhage, and pulmonary conditions. Head CT was performed periodically to monitor cerebral oedema and rebleeding.
We retrospectively collected demographic and clinical data on 22 parameters, including age, sex, smoking, alcohol consumption, diabetes mellitus, coronary atherosclerosis, hypertension, hyperlipidemia, admission systolic blood pressure, admission Glasgow Coma Scale (GCS) score, postoperative complications (pulmonary infection, lower extremity venous thrombosis, pulmonary embolism, intracranial infection, and postoperative cerebral infarction), d-dimer levels, hematoma volume, pneumatic compression therapy of the lower extremities, anticoagulant medication (heparin analogues and rivaroxaban), and modified Rankin Scale (mRS) scores. The Coniglobus formula (A × B × C/2) was used to calculate haematoma volume.
A retrospective blinded independent analysis was performed by two neurosurgical specialists and one radiological imaging specialist to ensure the quality of haematoma volume assessment. In cases of disagreement, the final judgement was made by the chief radiologist. Blood was drawn from patients with SSTICH at different time points: Immediately before surgery after admission, in the ICU within 24 hours after surgery, and every 2 days thereafter. To ensure the reliability of the data analysis, samples collected by a specialist or nurse were left in the ICU or general ward, kept sterile, and tested within 2 hours of collection. D-dimer concentrations were analysed using standard techniques (CA-7000 Sysmex, Dade Behring). D-dimer was considered a dichotomous variable and a value of ≥ 0.55 mg/L fibrinogen equivalent units was considered elevated.
The main outcome was the patients’ health status, determined by telephone and outpatient follow-up. After the occurrence of SSTICH, the patients were advised to visit the hospital for repeat head CT scans every 3 months and 6 months; those who came to the hospital for review were followed-up on an outpatient basis, and those who were unable to participate in the outpatient follow-up completed it by telephone. Patients were followed-up until 12 months after discharge from the hospital, and the time of death of the deceased patients was determined using the household registration inquiry system of the Hunan Provincial Public Security Bureau. Follow-up results were categorised according to mRS scores. Patients with an mRS score of 0–2 were considered to have a good prognosis, whereas those with an mRS score of 3–5 were considered to have a poor prognosis.
Categorical data were analysed using χ² test or other non-parametric tests. Normally distributed data are expressed as the mean ± SD and were analysed using independent samples t test. For non-normally distributed data, values are expressed as the median and interquartile range and were analysed using the Mann–Whitney U test. Subsequently, a logistic regression model was constructed to verify the effect of different surgical methods on prognosis and survival, and the relationship between different surgical procedures and confounding variables. Propensity score matching [phenol-soluble modulin (PSM); 1:1 matching, caliper 0.03] was used to minimise selection bias that may have occurred due to the retrospective nature of the study. The propensity score was based on the following 11 variables using a nearest neighbour matching algorithm without replacement: Age, preoperative GCS score, hematoma volume, hematoma clearance, deep cerebral haemorrhage, location of the hematoma, pulmonary embolism, lower extremity venous thrombosis, postoperative cerebral infarction, postoperative d-dimer level, and anticoagulant use (heparin analogues and rivaroxaban). To determine whether the results were sensitive to the matching method, a logistic regression model was applied after PSM for further validation. Statistical significance was defined as a two-sided P value < 0.05. All analyses were performed using Statistical Package for the Social Sciences statistical software (version 27.0, IBM Corp., version 4.3.1), and RStudio software.
The results presented in Table 1 show that, compared with the CI group, patients in the MIS group were older (61.78 years ± 10.87 years) and had a significantly higher proportion of deep cerebral haemorrhages (n = 255, 45.8%); a significantly lower incidence of postoperative lower extremity thrombosis (n = 45, 8.1%), pulmonary embolism (9 cases, 1.6%), and cerebral infarction (14 cases, 2.5%); a significantly higher hematoma clearance rate [92 (90, 94)]; significantly lower postoperative d-dimer levels; and significantly smaller rates of postoperative heparin analogue use. Most importantly, the proportion of patients with a favourable prognosis was significantly higher in the MIS group [227/327 (69.4%)] than in the CI group [126/230 (54.8%)] (P < 0.001), and the 1-year survival rate was also significantly higher in the MIS group [236/327 (72.2%); P < 0.001].
| Characteristic | Surgical procedures | P value | χ²/Z/t value | |
| Minimally invasive | Craniotomy | |||
| Mean age (years) | 61.78 ± 10.87 | 56.27 ± 11.58 | 0.604 | 5.735 |
| Age (years) | ||||
| < 59.5 | 124 (22.3) | 130 (23.3) | < 0.001 | 18.834 |
| > 59.5 | 203 (36.4) | 100 (18.0) | ||
| Sex | ||||
| Female | 131 (23.5) | 82 (14.7) | 0.292 | 1.111 |
| Male | 196 (35.2) | 148 (26.6) | ||
| Admission Glasgow Coma Scale score | ||||
| ≤ 8 | 102 (18.3) | 144 (25.9) | < 0.001 | 54.043 |
| > 8 | 225 (40.4) | 86 (15.4) | ||
| Left/right side | ||||
| Left | 158 (28.4) | 108 (19.4) | 0.751 | 0.100 |
| Right | 169 (30.3) | 122 (21.9) | ||
| Deep cerebral hemorrhage | 255 (45.8) | 155 (27.8) | 0.005 | 7.796 |
| Systolic blood pressure on admission (mm Hg) | 172.86 ± 26.40 | 175.73 ± 31.06 | 0.062 | 1.175 |
| Smoking | 112 (20.1) | 91 (16.3) | 0.199 | 1.646 |
| Alcohol abuse | 72 (12.9) | 65 (11.7) | 0.092 | 2.837 |
| Hypertension | 224 (40.2) | 156 (28.0) | 0.866 | 0.028 |
| Coronary atherosclerosis | 40 (7.2) | 19 (3.4) | 0.134 | 2.249 |
| Diabetes | 28 (5.0) | 29 (5.2) | 0.121 | 2.406 |
| High blood fat disease | 2 (0.4) | 3 (0.5) | 0.394 | 0.853 |
| Lower extremity vein thrombosis | 45 (8.1) | 59 (10.6) | < 0.001 | 12.572 |
| Lung infection | 285 (51.2) | 208 (37.3) | 0.232 | 1.427 |
| Pulmonary embolism | 9 (1.6) | 16 (2.9) | 0.018 | 5.567 |
| Intracranial infection | 7 (1.3) | 5 (0.9) | 0.979 | 0.001 |
| Postoperative cerebral infarction | 14 (2.5) | 33 (5.9) | < 0.001 | 17.71 |
| Lower extremity pneumatic compression therapy | 316 (56.7) | 216 (38.8) | 0.126 | 2.336 |
| Heparin-like drug | 22 (3.9) | 52 (9.3) | < 0.001 | 29.56 |
| Rivaroxaban | 13 (2.3) | 19 (3.4) | 0.032 | 4.579 |
| Hematoma volume (mL) | ||||
| First quartile (< 28) | 120 (21.5) | 13 (2.3) | < 0.001 | 104.237 |
| Quarter 2 (28-42) | 87 (15.6) | 50 (9.0) | ||
| Quarter 3 (42-64) | 77 (13.8) | 69 (12.4) | ||
| Quarter 4 (≥ 64) | 43 (7.7) | 98 (17.6) | ||
| Hematoma clearance rate | 92 (90, 94) | 87 (84, 89) | < 0.001 | 10.151 |
| Admission d-dimer levels (mg/L) | 1.30 (0.74, 2.74) | 1.19 (0.53, 2.93) | 0.072 | 14.252 |
| Postoperative d-dimer mean levels, mg/L | 3.17 (1.58, 6.78) | 2.73 (1.39, 5.58) | 0.009 | 2.601 |
| Outcome | ||||
| Favorable outcome | 69.4 (227/327) | 54.8 (126/230) | < 0.001 | 12.462 |
| Unfavorable outcome | 100 (18.0) | 104 (18.7) | ||
| Survival within 1 year | ||||
| Live | 236 (42.4) | 132 (23.7) | < 0.001 | 13.157 |
| Dead | 91 (16.3) | 98 (17.6) | ||
To validate the results in Table 1, we constructed a binary logistic regression model by combining the significant variables (those with P < 0.05). The results of the clinical characteristics are shown in Table 2, and the outcomes regarding prognosis and 1-year survival are shown in Table 3. In multifactorial analyses, age, deep cerebral haemorrhage, post
| Characteristic | Crude OR | 95%CI | P value | Adjusted OR | 95%CI | P value |
| Age (years) | 2.128 | 1.510-3.000 | < 0.001 | 4.183 | 2.366-7.395 | < 0.001 |
| Deep cerebral hemorrhage | 0.584 | 0.399-0.853 | 0.005 | 2.926 | 1.615-5.300 | < 0.001 |
| Lower extremity vein thrombosis | 0.462 | 0.300-0.712 | < 0.001 | 0.803 | 0.330-1.951 | 0.628 |
| Pulmonary embolism | 2.642 | 1.146-6.088 | 0.023 | 0.266 | 0.053-1.331 | 0.107 |
| Postoperative cerebral infarction | 3.745 | 1.955-7.174 | < 0.001 | 0.343 | 0.137-0.858 | 0.022 |
| Admission Glasgow Coma Scale score | 0.833 | 0.793-0.874 | < 0.001 | 0.811 | 0.748-0.880 | < 0.001 |
| Hematoma volume, mL | 1.024 | 1.018-1.030 | < 0.001 | 1.016 | 1.009-1.024 | < 0.001 |
| Hematoma clearance rate | 0.687 | 0.643-0.735 | < 0.001 | 0.667 | 0.614-0.724 | < 0.001 |
| Postoperative d-dimer mean levels (mg/L) | 0.918 | 0.864-0.975 | 0.005 | 0.829 | 0.746-0.921 | 0.001 |
| Heparin-like drug | 0.247 | 0.145-0.420 | < 0.001 | 0.351 | 0.134-0.920 | 0.033 |
| Rivaroxaban | 0.46 | 0.222-0.951 | 0.036 | 2.236 | 0.665-7.521 | 0.193 |
| Analysis | Outcome | P value | Survival within 1 year | P value |
| Crude1 OR | 0.534 | < 0.001 | 0.519 | < 0.001 |
| Crude1 95%CI | 0.376-0.758 | 0.364-0.742 | ||
| Adjusted2 OR | 1.071 | 0.913 | 0.454 | 0.221 |
| Adjusted2 95%CI | 0.312-3.685 | 0.128-1.609 | ||
| Crude3 PSM OR | 0.582 | 0.144 | 0.573 | 0.139 |
| Crude3 PSM 95%CI | 0.281-1.204 | 0.274-1.199 | ||
| Adjusted4 PSM OR | 2.235 | 0.092 | 2.450 | 0.070 |
| Adjusted4 PSM 95%CI | 0.877-5.695 | 0.931-6.451 |
In terms of patients' prognosis and survival within 1 year, the results reported in Tables 1 and 3 were opposing; hence, to verify the reliability of the results shown in Table 3, we included the 11 variables with significant between-group differences (shown in Table 1) to construct the propensity score (PS) matched model and obtained 68 matched pairs of data. The data of these 136 patients were re-analysed to verify whether the PS matched model was constructed suc
| Characteristic | Surgical procedures | P value | χ²/Z/t value | |
| Minimally invasive | Craniotomy | |||
| Mean age (years) | 58.81 ± 10.848 | 59.01 ± 10.044 | 0.909 | 0.115 |
| Age (years) | ||||
| < 59.5 | 37 (27.2) | 34 (25.0) | 0.607 | 0.265 |
| > 59.5 | 31 (22.8) | 34 (25.0) | ||
| Sex | ||||
| Female | 35 (25.7) | 30 (22.1) | 0.391 | 0.737 |
| Male | 33 (24.3) | 38 (27.9) | ||
| Admission Glasgow Coma Scale score | ||||
| ≤ 8 | 29 (21.3) | 28 (20.6) | 0.862 | 0.03 |
| > 8 | 39 (28.7) | 40 (29.4) | ||
| Left/Right side | ||||
| Left | 28 (20.6) | 28 (20.6) | > 0.999 | 0 |
| Right | 40 (29.4) | 40 (29.4) | ||
| Deep cerebral hemorrhage | 45 (33.1) | 43 (31.6) | 0.720 | 0.129 |
| Systolic blood pressure on admission (mm Hg) | 172.9 ± 27.98 | 171.16 ± 35.59 | 0.750 | 0.319 |
| Smoking | 23 (16.9) | 19 (14.0) | 0.458 | 0.551 |
| Alcohol abuse | 14 (10.3) | 14 (10.3) | > 0.999 | 0 |
| Hypertension | 45 (33.1) | 46 (33.8) | 0.855 | 0.033 |
| Coronary atherosclerosis | 8 (5.9) | 8 (5.9) | > 0.999 | 0 |
| Diabetes | 9 (6.6) | 7 (5.1) | 0.595 | 0.283 |
| High blood fat disease | 0 (0.0) | 0 (0.0) | > 0.999 | 0 |
| Lower extremity vein thrombosis | 12 (8.8) | 15 (11.0) | 0.519 | 0.416 |
| Lung infection | 60 (44.1) | 58 (42.6) | 0.613 | 0.256 |
| Pulmonary embolism | 1 (0.7) | 1 (0.7) | > 0.999 | 0 |
| Intracranial infection | 1 (0.7) | 0 (0.0) | 0.317 | 1 |
| Postoperative cerebral infarction | 6 (4.4) | 8 (5.9) | 0.573 | 0.319 |
| Lower extremity pneumatic compression therapy | 66 (48.5) | 64 (47.1) | 0.405 | 0.832 |
| Heparin-like drug | 9 (6.6) | 9 (6.6) | > 0.999 | 0 |
| Rivaroxaban | 5 (3.7) | 5 (3.7) | > 0.999 | 0 |
| Hematoma volume, mL | ||||
| First quartile (< 28) | 17 (12.5) | 6 (4.4) | 0.095 | 6.376 |
| Quarter 2 (28-42) | 19 (14.0) | 24 (17.6) | ||
| Quarter 3 (42-64) | 18 (13.2) | 22 (16.2) | ||
| Quarter 4 (≥ 64) | 14 (10.3) | 16 (11.8) | ||
| Hematoma clearance rate | 89 (88, 92) | 89 (87, 91) | 0.519 | 0.645 |
| Admission D-dimer levels (mg/L) | 1.2 (0.65, 2.52) | 1.02 (0.48, 2.76) | 0.318 | 0.999 |
| Postoperative D-dimer mean levels (mg/L) | 2.57 (1.33, 5.68) | 2.48 (1.38, 5.03) | 0.606 | 0.516 |
| Outcome | ||||
| Favorable outcome | 50 (36.8) | 42 (30.9) | 0.143 | 2.15 |
| Unfavorable outcome | 18 (13.2) | 26 (19.1) | ||
| Survival within 1 year | ||||
| Live | 51 (37.5) | 43 (31.6) | 0.138 | 2.205 |
| Dead | 17 (12.5) | 25 (18.4) | ||
We included all the data from the 68 matched pairs obtained from PSM to construct a new binary logistic regression model to verify whether the surgical method was significantly different from the patients' prognosis and survival within 1 year, and the results are shown in Table 3. After PSM was performed, the prognosis (OR: 2.235; 95%CI: 0.877–5.695; P = 0.092) and 1-year survival (OR: 2.450; 95%CI: 0.931–6.451; P = 0.070) were not significantly associated with the surgical approach.
This study aimed to understand the effects of MIS and CI in patients with SSTICH and to determine whether different surgical approaches increase the risk of poor prognosis. Our results showed that different surgical approaches did not increase the risk of poor postoperative prognosis or increase the 1-year mortality rate in patients with SSTICH. However, compared to those in the CI group, patients in the MIS group had a significantly lower incidence of postoperative cerebral infarction, higher rate of hematoma clearance, and lower percentage of postoperative anticoagulant use; patients undergoing MIS were older with a significantly higher percentage of patients aged > 59.5 years and had significantly higher GCS scores on hospital admission. These results may facilitate the development of individualised clinical treatment plans for patients with SSTICH.
Haemorrhagic stroke remains the leading cause of death and disability worldwide. Although it is accepted that patients with subtentorial cerebellar haemorrhage can certainly benefit from surgical treatment, whether patients with SSTICH also can benefit from surgical treatment remains controversial[19-21]. The mechanisms underlying poor prognosis caused by cerebral haemorrhage are the hematoma itself and perihematomal oedema (PHE)-induced occupancy leading to elevated ICP; the process of hematoma degradation, caused by the rupture of cerebral blood vessels, induces a series of pro-inflammatory responses that ultimately lead to apoptosis, degradation, self-phagocytosis, disruption of the blood-brain barrier, and ischaemic and hypoxic apoptosis of brain tissues[22-24]. Therefore, it has been theorised that surgical hematoma removal helps reduce the mass effect, cytotoxic response, and PHE. A midline shift caused by hematoma compression can cause neuronal damage in the early stages of cerebral haemorrhage and is associated with a poor prognosis. Previous studies support the theory that early removal of the cerebral haemorrhagic mass and aggressive clinical interventions are effective in improving patient prognosis[25].
Currently, there are two main types of surgical treatment for SSTICH: MIS and CI. The choice of surgical modality for treating SSTICH has been highly controversial. In several of the MISTIE III trials[19-21], the patients receiving MIS did not demonstrate a clear advantage in terms of therapeutic efficacy compared with patients receiving CI for treating SSTICH[22-24]. Both surgical procedures, however, have their own unique advantages and are commonly performed, with an annual use in more than 600 cases. Direct hematoma removal by CI is still the most commonly used method for high-volume ICH because it can thoroughly expose the hematoma area, the hematoma can be cleaned under the microscope (Figure 1G–N), and bleeding can be stopped by electrocoagulation of the responsible vessel or other small vessels. However, this method also induces a relative degree of brain damage, and the incidence of postoperative complications (such as pulmonary infection, intracranial infection, lower extremity venous thrombosis, pulmonary embolism, and postoperative cerebral infarction) may be higher. Furthermore, patients who undergo DC will require cranial repair at a later stage (Figure 1N). These complications may, therefore, offset the advantages of this method.
Minimally invasive procedures are becoming increasingly popular in ICH, mainly SA and ES, to avoid reducing the congenital damage caused by hematoma removal. Most of the available literature has demonstrated the advantages of such procedures when applied in patients with ICH[26-30]. Before performing MIS, a cranial CT scan should be conducted within 1 hours to precisely localise the haematoma, especially when faced with irregularly shaped haematomas. Surgery should be scheduled immediately after cranial CT if surgical indications are present. Some studies have shown that irregularities in the surface of the haematoma are associated with haematoma enlargement, and delaying surgery after CT may affect the precise positioning of the haematoma because of its enlargement[20-23]. Therefore, it is advisable to schedule a repeat cranial CT examination within 6 hours postoperatively to determine whether the intracranial haematoma has been removed cleanly and whether there is any sign of rebleeding[24-27]. ES can achieve satisfactory hemostasis and rapid relief of the mass effect endoscopically, and many studies have confirmed that ES is superior to CI and conservative treatment in reducing the mortality rate, poor prognosis, and specific complications of medium-volume and large-volume hematomas[14,15,31,32]. Although ES is an effective technique for both hematoma removal and hemostasis, it also has its shortcomings[33]. First, ES is performed in a fibrous tube, and there is a blind zone during the surgical treatment (Figure 1C–F), which is mainly located at the back of the tube; if the angle is adjusted to remove hematoma or hemostasis in the blind zone, this action could excessively pull the brain tissues, potentially leading to unnecessary brain injury. Second, compared with the traditional CI, the field of view and magnification for endoscopic hemostasis are inferior to that of a microscope (Figure 1F). In fact, relative to traditional CI, ES is not as fast in terms of intraoperative rapid hemostasis and release of hematoma compression, or in terms of resolving hematoma compression and removing the hematoma. However, although CI is faster in exerting these effects, the ES surgery time is shorter, mainly due to the longer time it takes to suture the scalp in traditional CI procedures[6,34]. Of these, DC has a natural advantage in that it can be adapted for delayed oedema after hematoma removal, which effectively avoids the possibility of a second surgery in patients with ICH with a large number of hematomas.
Both MIS and CI have their own advantages and disadvantages and, when treating patients with SSTICH, an appropriate surgical plan should be developed according to the individual clinical profile of the patient. In our study, older patients, those with GCS scores > 8 on admission, and those who had small or moderate hematoma volume were more inclined to choose MIS because it is less invasive and has a lower surgical risk. However, for patients with a large hematoma, especially those presenting with brain herniation or multiple intracranial haemorrhages with markedly increased ICP, we believe that CI should be the preferred treatment because it can quickly and efficiently resolve the hematoma and its compression effect; simultaneously, it can be considered for the removal of the cranial bones according to the ICP (Figure 1J–M). After PSM, the surgical approach did not significantly impact the prognosis and survival of patients, which suggests that the physician’s decision regarding the choice of surgical approach is not detrimental to the patient; rather, the surgical approach, decided on the basis of clinical profiles, is more conducive to coping with the complexity of the patient's situation.
The optimal timing for performing surgery to clear cerebral haemorrhages may be a key determinant of clinical management; nonetheless, it remains a controversial topic[35-37]. In theory, early surgical clearance of hematomas may improve prognosis by preventing hematoma enlargement and the attenuation of secondary injuries. However, some authors have highlighted that early surgery may lead to hematoma destabilisation and difficulty in stopping the haemorrhage, leading to an increase in rebleeding or a decrease in efficiency[35,37]. An overview of the preclinical and clinical data in one review strongly suggested that early hematoma removal may be critical for successful surgical access[38]. There was no difference in the time from symptom onset to surgery in any of the patients in this study, which was performed within 24 hours of symptom onset.
In the current study, no significant difference was found between the MIS and CI groups in terms of mortality at the 1-year follow-up. Regarding postoperative complications, we found that the incidence of postoperative lower extremity venous thrombosis, pulmonary embolism, and cerebral infarction was significantly lower in the MIS group than in the CI group; however, there was no significant difference between the two groups in terms of pulmonary and intracranial infections. The patients in the present study all had SSTICH and underwent surgery. These patients had greater intracranial haemorrhage, more severe clinical symptoms, a high incidence of vomiting, prolonged coma, and more frequent use of ventilators; therefore, they were all considered at high risk of pulmonary infection. Regardless of the surgical procedure, foreign bodies enter the cranial cavity, imposing a high infection risk. Some researchers believe that intracranial infections are more likely to occur due to the longer duration of traditional CI surgery and the larger area of exposed brain tissue. However, our results showed that the occurrence of intracranial infections was similar between the two groups; although the percentage was slightly higher in the MIS group, the difference was not statistically significant.
This study provides a reference for neurosurgeons to guide their choice of surgical approach, which should be made with full consideration of the clinical characteristics of the patient, such as age, GCS score on admission, hematoma volume, and hematoma location. However, it should be noted that our study excluded patients with bilateral pupil dilation and cerebral haemorrhage caused by other intracranial lesions (e.g. intracranial aneurysms, intracranial tumours, trauma, and arteriovenous malformations). Patients with dilated pupils generally have extremely high ICP and a very poor prognosis; if the pupil is not dilated for a long period of time, hematoma removal by CI is recommended, and if the pupil is retracted and the ICP is not high in such patients after the operation, DC is recommended. Recently, it has been reported that ES is a minimally invasive, safe, and effective strategy for the treatment of severe thalamic haemorrhage[38].
As this study had a retrospective and single-centre design, it had some limitations. First, we attempted to correct for confounders as much as possible using PSM and constructed a binary logistic regression model; however, the retrospective nature of the study and the presence of unknown confounders may have led to selection bias. Second, the single-centre design may reduce the generalizability of our findings, especially for many locations and clinical populations where surgical hematoma removal is not routinely performed. To determine the effectiveness of different surgical modalities in the treatment of SSTICH, more competent medical centres are needed to conduct multicenter prospective studies.
The current study identified no significant difference in the effect of MIS or CI on the postoperative prognosis of patients with SSTICH; however, MIS was more advantageous in terms of reducing the risk of postoperative complications. The choice of MIS or CI should be decided on an individual basis, considering the size of the hematoma, degree of midline shift, intraoperative brain swelling, location of the haemorrhage (left or right and whether it is a deep cerebral haemorrhage or a specific neurological function area), the GCS score at admission, and the ability of the patient to withstand surgery.
We sincerely thank The Second Affiliated Hospital of the University of South China for supporting the study and the Medical Statistics Department of the University of South China for the review.
| 1. | Caplan LR. Intracerebral haemorrhage. Lancet. 1992;339:656-658. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 112] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 2. | Rincon F, Mayer SA. Intracerebral hemorrhage: getting ready for effective treatments. Curr Opin Neurol. 2010;23:59-64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 43] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 3. | Woo D, Broderick JP. Spontaneous intracerebral hemorrhage: epidemiology and clinical presentation. Neurosurg Clin N Am. 2002;13:265-279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 67] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 4. | de Oliveira Manoel AL. Surgery for spontaneous intracerebral hemorrhage. Crit Care. 2020;24:45. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 76] [Cited by in RCA: 190] [Article Influence: 38.0] [Reference Citation Analysis (0)] |
| 5. | Wang K, Xue Y, Chen X, Cui D, Lou M. Transtentorial herniation in patients with hypertensive putaminal haemorrhage is predictive of elevated intracranial pressure following haematoma removal. J Clin Neurosci. 2012;19:975-979. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |
| 6. | Hayes SB, Benveniste RJ, Morcos JJ, Aziz-Sultan MA, Elhammady MS. Retrospective comparison of craniotomy and decompressive craniectomy for surgical evacuation of nontraumatic, supratentorial intracerebral hemorrhage. Neurosurg Focus. 2013;34:E3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 40] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 7. | Hegde A, Prasad GL, Menon G. Decompressive Craniectomy in Spontaneous Intracerebral Hemorrhage: A Comparison with Standard Craniotomy Using Propensity-Matched Analysis. World Neurosurg. 2020;144:e622-e630. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 8. | Moussa WM, Khedr W. Decompressive craniectomy and expansive duraplasty with evacuation of hypertensive intracerebral hematoma, a randomized controlled trial. Neurosurg Rev. 2017;40:115-127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 28] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 9. | Yao Z, Hu X, You C, He M. Effect and Feasibility of Endoscopic Surgery in Spontaneous Intracerebral Hemorrhage: A Systematic Review and Meta-Analysis. World Neurosurg. 2018;113:348-356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 33] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 10. | Xu X, Chen X, Li F, Zheng X, Wang Q, Sun G, Zhang J, Xu B. Effectiveness of endoscopic surgery for supratentorial hypertensive intracerebral hemorrhage: a comparison with craniotomy. J Neurosurg. 2018;128:553-559. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 80] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 11. | Li Y, Yang R, Li Z, Yang Y, Tian B, Zhang X, Wang B, Lu D, Guo S, Man M, Yang Y, Luo T, Gao G, Li L. Surgical Evacuation of Spontaneous Supratentorial Lobar Intracerebral Hemorrhage: Comparison of Safety and Efficacy of Stereotactic Aspiration, Endoscopic Surgery, and Craniotomy. World Neurosurg. 2017;105:332-340. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 48] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 12. | Feng Y, He J, Liu B, Yang L, Wang Y. Endoscope-Assisted Keyhole Technique for Hypertensive Cerebral Hemorrhage in Elderly Patients: A Randomized Controlled Study in 184 Patients. Turk Neurosurg. 2016;26:84-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 18] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 13. | Angileri FF, Esposito F, Priola SM, Raffa G, Marino D, Abbritti RV, Giusa M, Germanò A, Tomasello F. Fully Endoscopic Freehand Evacuation of Spontaneous Supratentorial Intraparenchymal Hemorrhage. World Neurosurg. 2016;94:268-272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 14. | Yamashiro S, Hitoshi Y, Yoshida A, Kuratsu J. Effectiveness of Endoscopic Surgery for Comatose Patients with Large Supratentorial Intracerebral Hemorrhages. Neurol Med Chir (Tokyo). 2015;55:819-823. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 26] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 15. | Kellner CP, Song R, Pan J, Nistal DA, Scaggiante J, Chartrain AG, Rumsey J, Hom D, Dangayach N, Swarup R, Tuhrim S, Ghatan S, Bederson JB, Mocco J. Long-term functional outcome following minimally invasive endoscopic intracerebral hemorrhage evacuation. J Neurointerv Surg. 2020;12:489-494. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 56] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 16. | Ye Y, Wang Q, Ou W, He J, Zhao Z. Endoscopic Surgery Without Decompressive Craniectomy in Large Putaminal Intracerebral Hemorrhage: Assessment of Efficacy and Safety. Neurocrit Care. 2020;32:392-399. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 17. | Lin K, Cheng Lin Z, Hai Tang Y, Wei D, Gao C, Jiang R. Comparison of endoscopic and open surgery in life-threatening large spontaneous supratentorial intracerebral hemorrhage: A propensity-matched analysis. Int J Stroke. 2023;18:569-577. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 18. | Hemphill JC 3rd, Greenberg SM, Anderson CS, Becker K, Bendok BR, Cushman M, Fung GL, Goldstein JN, Macdonald RL, Mitchell PH, Scott PA, Selim MH, Woo D; American Heart Association Stroke Council; Council on Cardiovascular and Stroke Nursing; Council on Clinical Cardiology. Guidelines for the Management of Spontaneous Intracerebral Hemorrhage: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2015;46:2032-2060. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1852] [Cited by in RCA: 2120] [Article Influence: 212.0] [Reference Citation Analysis (0)] |
| 19. | Hanley DF, Thompson RE, Rosenblum M, Yenokyan G, Lane K, McBee N, Mayo SW, Bistran-Hall AJ, Gandhi D, Mould WA, Ullman N, Ali H, Carhuapoma JR, Kase CS, Lees KR, Dawson J, Wilson A, Betz JF, Sugar EA, Hao Y, Avadhani R, Caron JL, Harrigan MR, Carlson AP, Bulters D, LeDoux D, Huang J, Cobb C, Gupta G, Kitagawa R, Chicoine MR, Patel H, Dodd R, Camarata PJ, Wolfe S, Stadnik A, Money PL, Mitchell P, Sarabia R, Harnof S, Barzo P, Unterberg A, Teitelbaum JS, Wang W, Anderson CS, Mendelow AD, Gregson B, Janis S, Vespa P, Ziai W, Zuccarello M, Awad IA; MISTIE III Investigators. Efficacy and safety of minimally invasive surgery with thrombolysis in intracerebral haemorrhage evacuation (MISTIE III): a randomised, controlled, open-label, blinded endpoint phase 3 trial. Lancet. 2019;393:1021-1032. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 397] [Cited by in RCA: 595] [Article Influence: 99.2] [Reference Citation Analysis (0)] |
| 20. | Mendelow AD, Gregson BA, Rowan EN, Murray GD, Gholkar A, Mitchell PM; STICH II Investigators. Early surgery versus initial conservative treatment in patients with spontaneous supratentorial lobar intracerebral haematomas (STICH II): a randomised trial. Lancet. 2013;382:397-408. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 935] [Cited by in RCA: 912] [Article Influence: 76.0] [Reference Citation Analysis (0)] |
| 21. | Awad IA, Polster SP, Carrión-Penagos J, Thompson RE, Cao Y, Stadnik A, Money PL, Fam MD, Koskimäki J, Girard R, Lane K, McBee N, Ziai W, Hao Y, Dodd R, Carlson AP, Camarata PJ, Caron JL, Harrigan MR, Gregson BA, Mendelow AD, Zuccarello M, Hanley DF; MISTIE III Trial Investigators. Surgical Performance Determines Functional Outcome Benefit in the Minimally Invasive Surgery Plus Recombinant Tissue Plasminogen Activator for Intracerebral Hemorrhage Evacuation (MISTIE) Procedure. Neurosurgery. 2019;84:1157-1168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 95] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 22. | Horowitz ME, Ali M, Chartrain AG, Allen OS, Scaggiante J, Glassberg B, Sakai Y, Turkheimer L, Song R, Martini ML, Zhang X, Mocco J, Kellner CP. Definition and time course of pericavity edema after minimally invasive endoscopic intracerebral hemorrhage evacuation. J Neurointerv Surg. 2022;14:149-154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 23. | Aronowski J, Zhao X. Molecular pathophysiology of cerebral hemorrhage: secondary brain injury. Stroke. 2011;42:1781-1786. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 682] [Cited by in RCA: 648] [Article Influence: 46.3] [Reference Citation Analysis (0)] |
| 24. | Wang J. Preclinical and clinical research on inflammation after intracerebral hemorrhage. Prog Neurobiol. 2010;92:463-477. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 517] [Cited by in RCA: 496] [Article Influence: 33.1] [Reference Citation Analysis (0)] |
| 25. | Jauch EC, Pineda JA, Hemphill JC. Emergency Neurological Life Support: Intracerebral Hemorrhage. Neurocrit Care. 2015;23 Suppl 2:S83-S93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 26. | Auer LM, Deinsberger W, Niederkorn K, Gell G, Kleinert R, Schneider G, Holzer P, Bone G, Mokry M, Körner E. Endoscopic surgery versus medical treatment for spontaneous intracerebral hematoma: a randomized study. J Neurosurg. 1989;70:530-535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 438] [Cited by in RCA: 391] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 27. | Morgan T, Zuccarello M, Narayan R, Keyl P, Lane K, Hanley D. Preliminary findings of the minimally-invasive surgery plus rtPA for intracerebral hemorrhage evacuation (MISTIE) clinical trial. Acta Neurochir Suppl. 2008;105:147-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 200] [Cited by in RCA: 185] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 28. | Newell DW, Shah MM, Wilcox R, Hansmann DR, Melnychuk E, Muschelli J, Hanley DF. Minimally invasive evacuation of spontaneous intracerebral hemorrhage using sonothrombolysis. J Neurosurg. 2011;115:592-601. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 74] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 29. | Schaller C, Rohde V, Meyer B, Hassler W. Stereotactic puncture and lysis of spontaneous intracerebral hemorrhage using recombinant tissue-plasminogen activator. Neurosurgery. 1995;36:328-333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 84] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 30. | Teernstra OP, Evers SM, Lodder J, Leffers P, Franke CL, Blaauw G; Multicenter randomized controlled trial (SICHPA). Stereotactic treatment of intracerebral hematoma by means of a plasminogen activator: a multicenter randomized controlled trial (SICHPA). Stroke. 2003;34:968-974. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 228] [Cited by in RCA: 221] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 31. | Kellner CP, Moore F, Arginteanu MS, Steinberger AA, Yao K, Scaggiante J, Mocco J, Gologorsky Y. Minimally Invasive Evacuation of Spontaneous Cerebellar Intracerebral Hemorrhage. World Neurosurg. 2019;122:e1-e9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 32. | Hersh EH, Gologorsky Y, Chartrain AG, Mocco J, Kellner CP. Minimally Invasive Surgery for Intracerebral Hemorrhage. Curr Neurol Neurosci Rep. 2018;18:34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 46] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 33. | Delcourt C, Sato S, Zhang S, Sandset EC, Zheng D, Chen X, Hackett ML, Arima H, Hata J, Heeley E, Al-Shahi Salman R, Robinson T, Davies L, Lavados PM, Lindley RI, Stapf C, Chalmers J, Anderson CS; INTERACT2 Investigators. Intracerebral hemorrhage location and outcome among INTERACT2 participants. Neurology. 2017;88:1408-1414. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 85] [Cited by in RCA: 103] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 34. | Gregson BA, Mitchell P, Mendelow AD. Surgical Decision Making in Brain Hemorrhage. Stroke. 2019;50:1108-1115. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 46] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 35. | Morgenstern LB, Demchuk AM, Kim DH, Frankowski RF, Grotta JC. Rebleeding leads to poor outcome in ultra-early craniotomy for intracerebral hemorrhage. Neurology. 2001;56:1294-1299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 212] [Cited by in RCA: 213] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 36. | Kellner CP, Schupper AJ, Mocco J. Surgical Evacuation of Intracerebral Hemorrhage: The Potential Importance of Timing. Stroke. 2021;52:3391-3398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 25] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 37. | Polster SP, Carrión-Penagos J, Lyne SB, Gregson BA, Cao Y, Thompson RE, Stadnik A, Girard R, Money PL, Lane K, McBee N, Ziai W, Mould WA, Iqbal A, Metcalfe S, Hao Y, Dodd R, Carlson AP, Camarata PJ, Caron JL, Harrigan MR, Zuccarello M, Mendelow AD, Hanley DF, Awad IA. Intracerebral Hemorrhage Volume Reduction and Timing of Intervention Versus Functional Benefit and Survival in the MISTIE III and STICH Trials. Neurosurgery. 2021;88:961-970. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 39] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 38. | Zhou H, Cha Z, Wang L, Chen M, Zhang Q, Tang J. Clinical efficacy and safety of neuroendoscopic surgery for severe thalamic hemorrhage with ventricle encroachment. Neurosurg Rev. 2022;45:2701-2708. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |