INTRODUCTION
Acute respiratory distress syndrome (ARDS) is a sudden, diffuse, inflammatory lung injury triggered by risk factors such as pneumonia, extrapulmonary infections, trauma, transfusion, burns, shock, or aspiration. This condition leads to increased permeability of the pulmonary vasculature or epithelial barrier, resulting in pulmonary edema and gravity-dependent atelectasis[1]. The clinical features include arterial hypoxemia and diffuse radiographic opacities, accompanied by increased shunting, elevated alveolar dead space, and reduced lung compliance[2]. Diagnosis of ARDS demands a multifaceted approach, incorporating clinical assessment, patient history of toxin exposure, physical examination, and laboratory tests, alongside potential direct airway visualization via procedures such as bronchoscopy[3,4]. The management of ARDS is comprehensive and centers on supportive care to enhance respiratory function by reducing the shunt, improving oxygenation, and preventing lung injury. Lung-protective ventilation is a cornerstone of this strategy that can significantly influence outcomes[5]. A comprehensive approach to ARDS treatment encompasses mechanical ventilation, prone positioning, judicious sedation and medication use, precise fluid management, and pharmacological therapies, all integral to the therapeutic regimen for this complex condition[4,6]. Understanding the pathogenesis and implementing appropriate management strategies are essential for improving patient outcomes in ARDS. Demulsifiers are chemicals widely used to break oil-water emulsions by altering the properties of the oil-water interface, reducing interfacial tension, and facilitating the separation of oil droplets from water[7]. Research has shown that demulsifiers can generate odors that are both pungent and potentially irritating[8]. The precise biological processes responsible for the potential lung toxicity of demulsifiers are still not fully understood. It is hypothesized that these substances could irritate the respiratory system or cause damage, possibly because of the presence of toxic solvents or volatile organic compounds in certain formulations. Inhalation of industrial chemicals can harm the respiratory tract and lung tissue, impairing gas exchange and triggering respiratory distress[9]. This damage may initiate the development of ARDS, a severe condition caused by direct injury to the respiratory system, thereby setting off a cascade of complex pathological events[3,10]. This underscores the urgency for rigorous enforcement of safety protocols and the necessity to equip workers who frequently handle hazardous substances with adequate protective gear. Additionally, conducting operations in well-ventilated settings is crucial for the early identification and intervention of health complications. Current research on the respiratory effects of demulsifiers is limited, with most studies concentrating on their industrial applications rather than the specific impacts and medical management of exposure to these chemicals[11]. In this case report, we present a rare and enlightening documented instance of ARDS induced by a demulsifier and clarify the respiratory symptoms, therapeutic strategies, and prognostic implications associated with this agent. This report not only highlights the potential pulmonary complications arising from demulsifier exposure but also establishes a foundation for future diagnostic and therapeutic protocols in similar cases. Consequently, it seeks to improve clinical management and encourage research within this emerging field.
CASE PRESENTATION
Chief complaints
A 69-year-old male salesperson presented to the emergency department with complaints of shortness of breath and chest tightness lasting approximately 6 hours.
History of present illness
He also reported accompanying symptoms of dyspnea, nausea, abdominal discomfort, and multiple episodes of vomiting.
History of past illness
The patient’s medical history was significant for coronary heart disease, for which he had undergone stent implantation 2 years ago.
Personal and family history
He had no history of alcohol or tobacco use, nor did he have any neurological or psychiatric disorders. There was no reported history of asthma, pneumonia, tuberculosis, infectious diseases, or surgical intervention involving the lungs. The patient had no known genetic disorders. His family members were also reported to be in good health.
Physical examination
Upon admission, the patient was in an agitated state and required high-flow oxygen (8 L/min via mask, bedside blood gas analysis showed a PaO2 of 67.17 mmHg). Vital signs indicated a heart rate of 132 beats/minute, blood pressure of 93/50 mmHg, respiratory rate of 26 breaths/minute, and peripheral oxygen saturation (SpO2) of 78%. The body temperature was 37.4 °C. Chest auscultation revealed bilaterally diminished breath sounds with moist rales. A general physical examination and specific assessments of other body systems revealed no abnormalities.
Laboratory examinations
Routine blood tests showed a total leucocyte count of 23.76 × 109/L, with neutrophile granulocyte count of 22.92 × 109/L (96.4%). The procalcitonin (PCT) level was 2.16 µg/L, and C-reactive protein (CRP) levels were elevated at 71.42 mg/L. Arterial blood gas analysis revealed a pH of 7.242, pO2 of 67.17 mmHg, pCO2 of 71.85 mmHg, HCO3- of 30.30 mmol/L, and a base excess of 0.15 mmol/L. The calculated PaO2/FiO2 ratio was 127. Additional laboratory results included a B-type natriuretic peptide of 37.34 pg/mL, high-sensitivity troponin of 4.4 ng/L, CK of 74 U/L, and CK-MB of 14 U/L.
Imaging examinations
The electrocardiogram findings indicated sinus tachycardia. Transthoracic echocardiogram demonstrated a left ventricular ejection fraction of 71% with a cardiac output of 5 L/min, and no enlargement of the left or right atria or ventricles, with normal pulmonary artery pressure. Lung ultrasound revealed dense B-line consolidations in both lungs. Chest computed tomography (CT) showed pulmonary infiltrates in both lungs without signs of cardiomegaly or pleural effusion (Figure 1A).
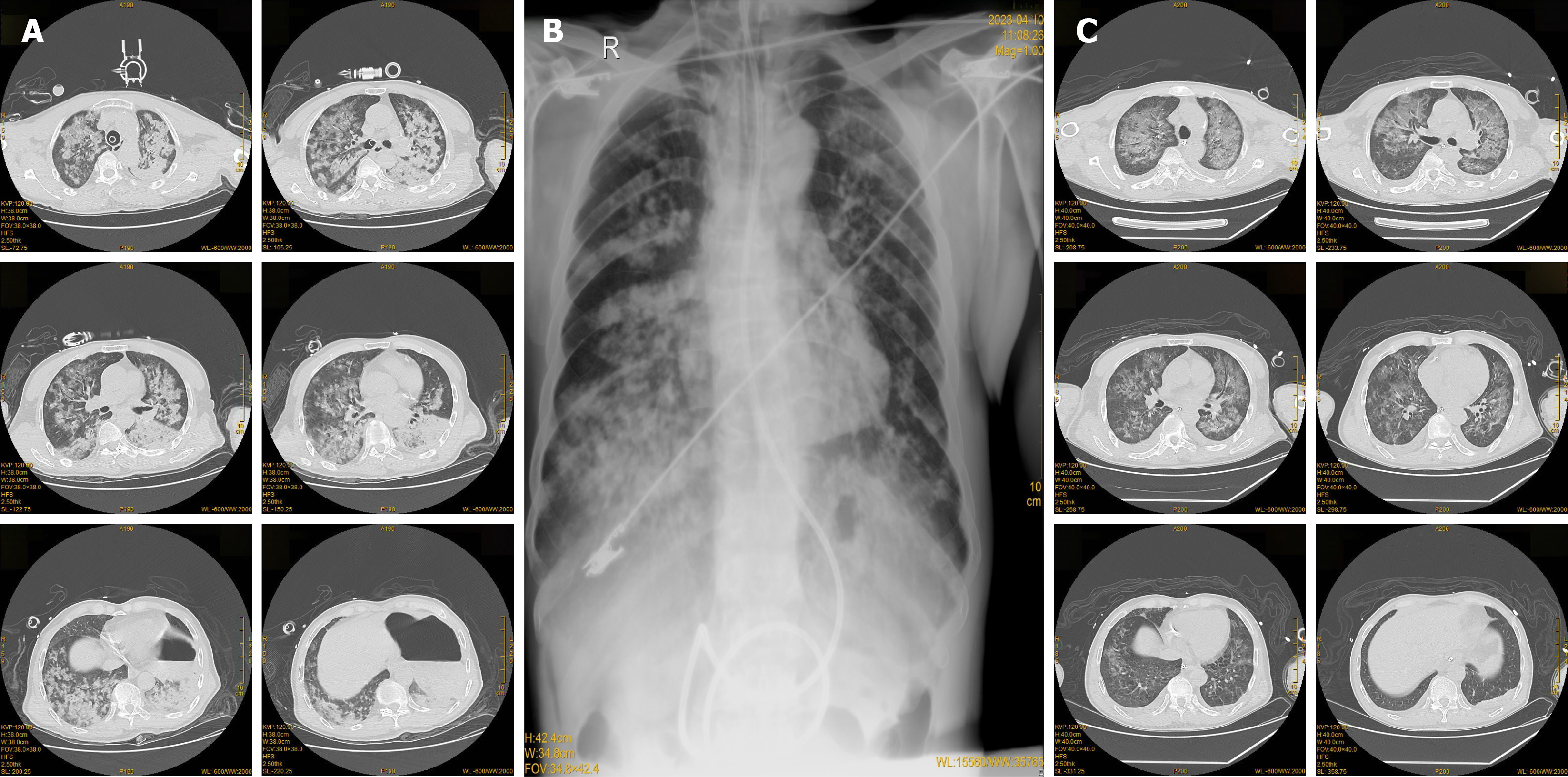
Figure 1 Imaging changes found in the course of acute respiratory distress syndrome management.
Changes on chest computed tomography (CT) before; radiography taken on April 10th; chest CT after treatment on April 13th. A: The chest CT carried out in the emergency room revealed pulmonary infiltrates in both lungs; B: A follow-up chest radiography on April 10th indicated exudative lesions in both lungs; C: After 5 days of treatment, a repeat chest CT examination showed significant resolution of the pulmonary infiltrates.
FINAL DIAGNOSIS
(1) ARDS; (2) Aspiration pneumonitis; (3) Toxic inhalation injury; (4) Hypo-ventilatory respiratory failure; and (5) Post stent placement in coronary arteries.
TREATMENT
After being transferred to the intensive care unit (ICU), a fiberoptic bronchoscopy was immediately performed, along with saline irrigation and suctioning of airway secretions. Piperacillin-tazobactam sodium (450 mg intravenously every 8 hours) and levofloxacin (500 mg intravenously once daily) were given for anti-infection purposes. Other medications included rocuronium, remifentanil, propofol, norepinephrine (16 mg at a rate of 0.5 μg/kg/min), and omeprazole (40 mg, intravenous drip every 12 hours). On day 3, despite the initial treatment, the patient experienced recurrent fever with significantly increased temperature peaks. Dynamic monitoring of infection markers including white blood cell count, PCT, and CRP showed a continuous rise. We conducted a chest X-ray examination for the patient, which revealed exudative lesions in both lungs (Figure 1B). Consequently, the anti-infective regimen was adjusted to include meropenem (1 g intravenously every 12 hours), combined with levofloxacin (0.5 g intravenously once daily) to enhance the anti-infective therapy. The recommendations from evidence-based medicine indicate that glucocorticoid treatment is associated with a reduction in mortality of patients with ARDS[12]. Our patient was treated with Methylprednisolone administered intravenously at a dosage of 40 mg twice daily. After this adjusted treatment, the patient’s temperature gradually decreased, the oxygenation index improved, infection markers decreased, and ventilator support parameters were gradually tapered. Enteral nutrition support (TPF, 500 mL) was initiated. On day 5, a repeat chest CT revealed significant resolution of the pulmonary infiltrates (Figure 1C). The dosage of methylprednisolone was modified from 40 mg twice daily to 40 mg once daily. The volume of enteral nutrition was increased to 1000 mL. By day 7, Methylprednisolone was discontinued after a total of 6 days of administration. On day 10, the patient demonstrated marked improvement in consciousness and respiratory function, with a continuous decline in white blood cell count and PCT levels. Chest radiography indicated visible absorption of bilateral diffuse infiltrative lesions (Figure 2A). On day 11, the antibiotic regimen was changed from meropenem to cefoperazone sulbactam sodium (3 g intravenously every 8 hours). The endotracheal tube was successfully removed, and the patient transitioned to high-flow nasal cannula oxygen therapy. On day 12, high-flow nasal cannula support was switched to a regular nasal cannula, with the patient showing no signs of respiratory distress. On day 13, a follow-up chest CT revealed further absorption of the exudative lesions compared to previous imaging findings (Figure 2B). Finally, on day 14, the patient was deemed eligible for referral to the Department of Pulmonology for further medical evaluation and treatment.
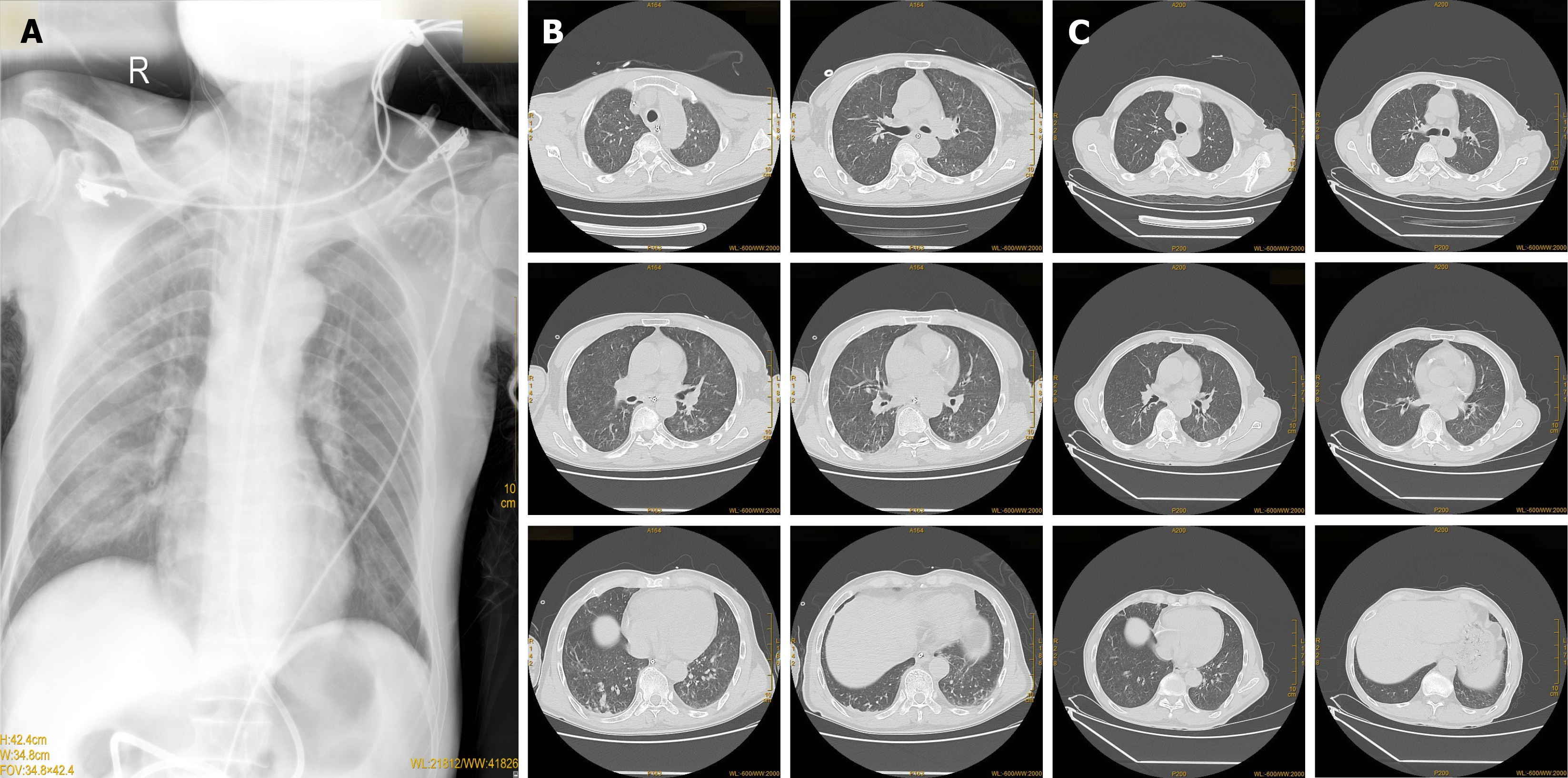
Figure 2 Gradual imaging indications of improvement post-treatment in patients.
Radiography taken on April 16th; Chest computed tomography (CT) after treatment on April 19th; Chest CT after treatment on April 27th. A: Chest radiography taken on April 16th, compared to that on April 9th, indicated a significant reduction in exudative lesions in both lungs; B: The chest CT examination on April 19th showed resolution of the exudative lesion when compared to the previous image; C: After treatment, a follow-up chest CT on April 27th indicated significant improvement in the absorption of exudative lesions in both lungs.
OUTCOME AND FOLLOW-UP
We conducted a follow-up evaluation of the patient. Chest CT examination performed on April 27, 2023, revealed significant improvement in the absorption of diffuse lesions in both lungs, leading to the patient’s discharge the next day (Figure 2C). Following discharge, the patient continued to regularly attend the outpatient clinic for follow-ups. During these active follow-ups, recurrent pneumonia was identified. Further observation and additional data are necessary to determine whether there is a correlation between the recurrent pneumonia and the ARDS that resulted from emulsifier poisoning, as well as to study the long-term prognosis of toxic inhalation.
DISCUSSION
Herein, we reported a case of ARDS caused by acute chemical poisoning in an older male patient. There were no symptoms such as fever, chest tightness, or shortness of breath before disease onset. The patient had a history of exposure to and inhalation of toxic substances, which led to pulmonary edema and subsequently triggered ARDS. Given the rapid progression of the condition, CT also showed evidence of diffuse exudation. A combination of the patient’s history of toxic exposure, progressive difficulty breathing, blood gas analysis (oxygenation index), and chest CT findings indicative of diffuse exudation, provided significant assistance in diagnosis. ARDS was confirmed according to the Berlin criteria[13]. The classification is determined by positive end-expiratory pressure ≥ 5 cm H2O or continuous positive airway pressure ≥ 5 cm H2O. ARDS is categorized as follows: Mild ARDS with 200 mmHg. Chemical pneumonia is a potential cause of acute respiratory distress syndrome (ARDS). The underlying pathophysiological processes may involve direct lung injury from aspiration, along with the activation of pulmonary and systemic inflammatory cascades[14,15].
Demulsifiers are chemical agents broadly utilized in industries such as petroleum refining and wastewater treatment[16]. While the utility of these substances in segregating emulsions into oil and water is well-known, their potential to cause pulmonary toxicity requires further elucidation. To our knowledge, clinical reports of demulsifier poisoning are currently absent, and there is no specific treatment modality for this condition. Research indicates that the management of ARDS caused by chemical exposure primarily involves symptomatic supportive care including oxygen therapy, lung-protective ventilation strategies, and comprehensive supportive care[17,18]. The treatment strategy for ARDS primarily focuses on supportive care, mechanical ventilation, oxygen therapy, and fluid management[4]. In this case, in addition to the above treatment measures, we also administered methylprednisolone and various antibiotics and performed bronchoscopy to clear the airway. Glucocorticoids has been considered a promising treatment for ARDS due to their anti-inflammatory, anti-oxidant, anti-fibrosis, and immunoregulatory effects[19]. The 2024 Society of Critical Care Medicine guidelines recommend the use of corticosteroids in adult patients with severe ARDS, noting that the ideal dosage, timing, and type of corticosteroid should depend on the clinician’s discretion and other considerations[20]. Furthermore, evidence indicates that the use of corticosteroids in patients with ARDS can reduce in-hospital mortality[21,22]. A multicenter retrospective study based on the eICU Collaborative Research Database retrospectively analyzed 2167 patients with ARDS, of whom 254 received glucocorticoid treatment. The results showed that treatment with glucocorticoids was significantly associated with reduced ICU mortality in ARDS patients, demonstrating the potentially protective effects of glucocorticoids therapy[23]. Furthermore, glucocorticoids has been shown to decrease the duration of mechanical ventilation and improve the PaO2/FiO2 ratio in patients[22,24-26]. Given the patient’s history of vomiting and subsequent intubation because of the unconscious state, the index of infection increased significantly, and it became essential to consider the potential occurrence of aspiration pneumonia. Antibiotics play a crucial role in the management of aspiration pneumonia[27]. Based on our patient’s symptoms, biochemical tests, and imaging results, we adjusted the type and dose of antibiotics during treatment. Improvements in patient consciousness and oxygenation index, along with the radiological resolution of bilateral diffuse infiltrative lesions, demonstrated the efficacy of the treatment. The successful transition from mechanical ventilation to a high-flow nasal cannula, followed by conventional oxygen therapy, signifies an effective weaning process and indicates a favorable progression towards recovery. The patient’s delayed presentation to the hospital highlights the poor awareness regarding prevention of exposure to toxins in the working environment. Because of the lack of timely personal protective measures and immediate medical intervention, the patient’s condition had already deteriorated significantly by the time he sought medical attention. Given the rarity of ARDS cases resulting from demulsifier poisoning, the potential for long-term sequelae remains unknown. Therefore, it is essential to maintain long-term follow-up for continued monitoring.
CONCLUSION
This case highlights the importance of recognizing diseases caused by chemical toxicants. In the daily diagnosis and treatment of patients with respiratory symptoms of unknown origin, it is crucial to determine whether exposure to or inhalation of toxicants is a pathogenic factor by a detailed reviewing of the medical history. Standard and effective treatment strategies should be explored. Additionally, preventive measures should be advocated for workers who regularly come into contact with chemical substances to avoid injuries from occupational exposure.
ACKNOWLEDGEMENTS
We would like to extend our sincere appreciation to Dr. Zhi-Xin Cui for his expert advice and critical insights throughout the preparation of this manuscript. We also appreciate the insightful feedback from our colleagues, who contributed significantly to refining our conclusions. Their essential contributions and endorsement of our data have been crucial in the successful completion of this case report.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Radiology, nuclear medicine and medical imaging
Country of origin: China
Peer-review report’s classification
Scientific Quality: Grade A, Grade D
Novelty: Grade B, Grade C
Creativity or Innovation: Grade B, Grade C
Scientific Significance: Grade A, Grade C
P-Reviewer: Liang GD; Zhang W S-Editor: Qu XL L-Editor: A P-Editor: Wang WB