Published online Nov 28, 2024. doi: 10.4329/wjr.v16.i11.629
Revised: October 1, 2024
Accepted: November 8, 2024
Published online: November 28, 2024
Processing time: 257 Days and 2.3 Hours
The appendix vermiformis is a part of the gastrointestinal tract, situated in the lower right quadrant of the abdomen. Acute appendicitis, acute inflammation of the appendix vermiformis, is the most common cause of acute abdomen requiring surgical intervention. Although computed tomography (CT) offers high diagno
To determine the location of the appendix vermiformis on CT using the vertebrae and the right iliac bone as anatomical landmarks.
This retrospective study examined 470 patients presenting with abdominal pain who underwent abdominal CT scans between January 01, 2015 and January 01, 2018. Forty-three patients were excluded due to various reasons. The most supe
The final analysis included 427 adult patients (206 females and 221 males) with a mean age of 42.1 ± 19.5 years. An ascending appendix course was the most common (90.4%). The appendix ranged from the L2 vertebral body level to the coccygeal vertebral level relative to the vertebrae. The appendix ranged between (−) 140.5 mm and (+) 87.4 mm relative to the right iliac bone. A negative correlation was found between patient age, height, body mass index, and the highest and lowest points of the appendix in regard to the vertebrae.
The study’s findings unveiled the locations of the appendix in the population in relation to the bony anatomical landmarks. These data can be used as the basis for future research aimed at reducing patient exposure to ionizing radiation.
Core Tip: It is important to determine the location of the appendix vermiformis in the population using anatomical reference points. Therefore, when there is a suspicion of acute appendicitis and computed tomography is required, the field of view can be adjusted accordingly, potentially reducing the radiation dose given to the patient. Utilizing bony structures as refe
- Citation: Ozturk MO, Resorlu M, Aydin S, Memis KB. Use of the vertebrae and iliac bone as references for localizing the appendix vermiformis in computed tomography. World J Radiol 2024; 16(11): 629-637
- URL: https://www.wjgnet.com/1949-8470/full/v16/i11/629.htm
- DOI: https://dx.doi.org/10.4329/wjr.v16.i11.629
The appendix vermiformis is a part of the gastrointestinal tract and is located in the lower right quadrant of the abdomen. It has a worm-like appearance and originates from the posteromedial wall of the cecum in embryological life, around 2 cm below the terminal ileum[1,2]. The length of the appendix varies between 2 and 20 cm, with an average of 9 cm[1-3].
Atypical positions of the cecum and appendix may be encountered[4]. The relationship between the base of the appendix and the cecum is consistent in terms of location. However, the distal end of the appendix can be found in various locations, such as retrocecal, subcecal, pelvic, preileal, retroileal, right paracolic, promontoric, or subhepatic areas. These variations play an important role in the pain localization of acute appendicitis[5,6]. In Wakeley’s postmortem study of 10000 cases, the frequencies of appendix localization were as follows: Retrocecal 65.3%, pelvic 31%, subcecal 2.3%, and preileal 1%[7]. However, other studies have found the most common position of the appendix to be pelvic[5,8].
Acute appendicitis, the acute inflammation of the appendix vermiformis, is the most common cause of acute abdomen requiring surgical treatment[9,10]. It is most commonly observed in adolescents and young adults and peaks in the second and third decades of life[11]. It usually starts with mild periumbilical visceral pain, which shifts to the right lower quadrant approximately 8 hours after onset. Atypical pain progression and localization can sometimes occur. Radio
The radiological imaging methods used in the diagnosis of acute appendicitis are ultrasonography (US), computed tomography (CT), and, rarely, magnetic resonance imaging[13]. US is usually the first modality used and may be useful in diagnosis; however, it has disadvantages, as its accuracy is highly dependent on patient, device, and operator-related factors[13,14]. In contrast, CT is independent of these factors and maintains diagnostic efficacy in patients with variable appendix positions. Furthermore, severe pain is not a limiting factor for CT scans, allowing for the evaluation of other pathologies in the differential diagnosis of acute appendicitis. The main disadvantages of CT are exposure to ionizing radiation and nephrotoxic and allergic effects associated with contrast media[15].
Obtaining diagnostically adequate images with minimal radiation exposure forms the basis of the “As Low as Reasonably Achievable (ALARA)” principle[16]. Dose modulation, kilovoltage peak adjustments, and reduction of the imaging area are some of the methods that can help reduce radiation exposure during CT scans[17]. Several studies have investigated the effectiveness of low-dose CT for diagnosing acute appendicitis by reducing exposure factors. In the study by Keyzer et al[18], which compared low-dose and standard-dose CT for diagnosing acute appendicitis, no difference was observed in appendix visibility or diagnostic accuracy. Similarly, Fefferman et al[19] found no significant difference between standard-dose and low-dose CT techniques. In another study, Sippola et al[20] found that a low-dose protocol showed no significant difference in diagnostic accuracy compared to the standard protocol, with a significant reduction in the mean effective radiation dose between the two techniques. These studies highlight the unnecessary dose burden associated with CT scans performed to avoid unnecessary appendectomies. In the aforementioned studies, radiation doses were lowered by adjusting exposure parameters, and the results were compared with standard-dose images[18-20]. To further minimize radiation exposure, we recommend narrowing the field of view (FOV) to prevent unnecessary radiation exposure to the patient. This can only be accomplished by using metric markers to accurately locate the appendix in the population. Our study aimed to define the location of the appendix vermiformis using these metric markers.
Patients who presented to the emergency department with abdominal pain and underwent non-contrast or contrast-enhanced abdominal CT between January 01, 2015 and January 01, 2018, were included in this retrospective study. This study was approved by the institutional ethics committee (No. 2011-KAEK-27/2019-E.1900162336) and carried out in compliance with the principles outlined in the Declaration of Helsinki. The requirement for informed consent was waived by the ethics committee, as all patient identification information was removed after data were collected and analyzed.
Clinical data and images of 470 randomly chosen patients who presented to the emergency department with abdo
All abdominal CT studies were conducted using a 64-detector multidetector CT scanner. The CT acquisition para
To objectively determine the location of the appendix in the population included in the study, we used the vertebrae and the highest point of the right iliac bone as anatomical landmarks. The superior and inferior points of the appendix were identified separately relative to the vertebrae for population-based localization. In addition, the superior point, inferior point, and origin of the appendix were measured separately in relation to the right iliac bone. In this context, the superior point of the appendix is labeled as “ApA,” the inferior point is labeled “ApB,” and the appendiceal origin is labeled “Ap0.” For measurements using the vertebrae and the right iliac bone as references, the population was divided into two groups: Normal appendix and acute appendicitis.
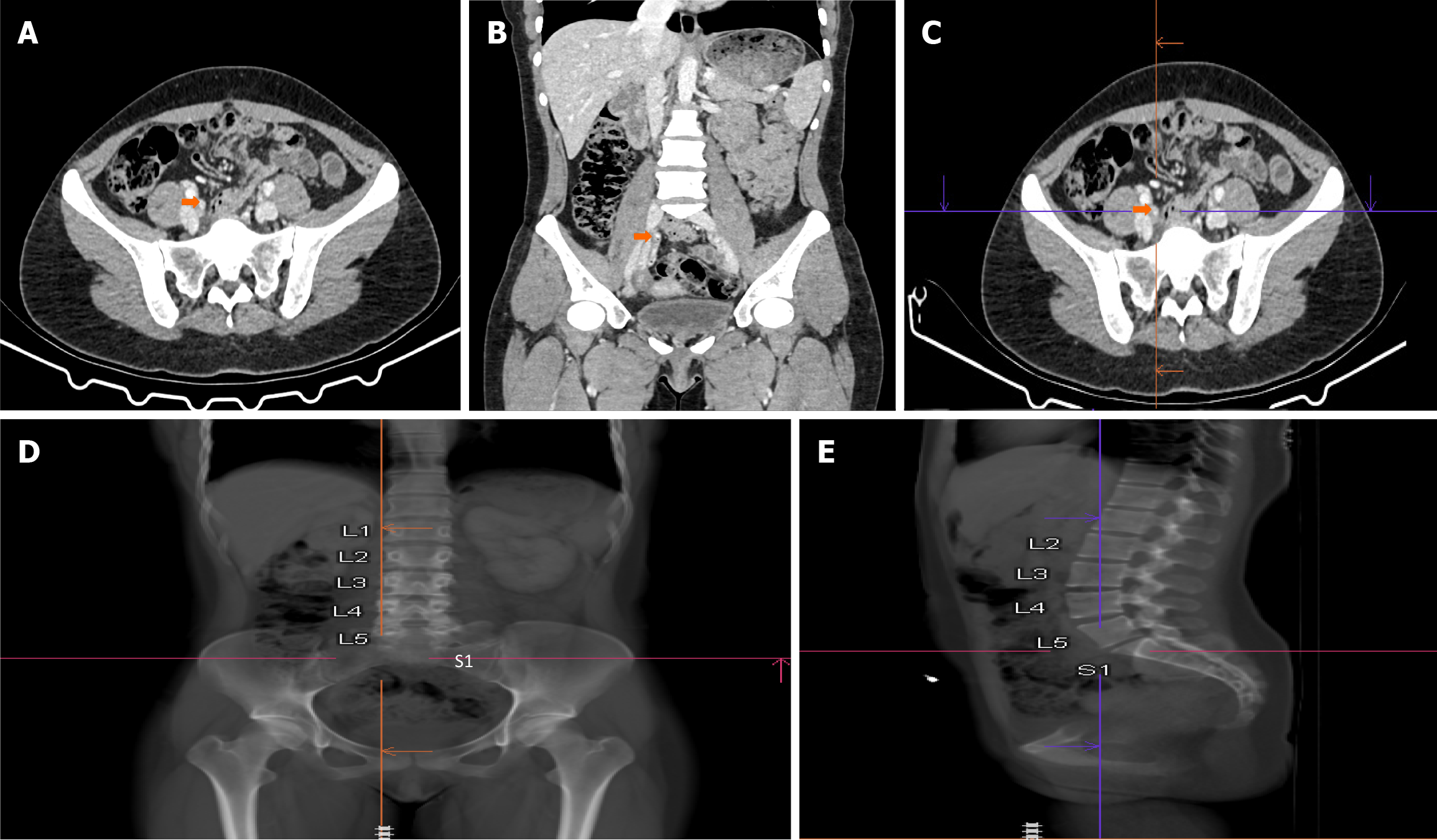
To determine the location of the appendix using the vertebrae as reference points, initially, the locations of the appendix’s superior and inferior points along its course were found and marked on axial CT images. Then, these points were located on thick coronal and sagittal multiplanar reformatted images to determine their respective vertebral levels. We grouped the vertebral levels for appendix localization as follows: L1 & L1-L2 intervertebral joint; L2 & L2-L3 intervertebral joint; L3 & L3-L4 intervertebral joint; L4 & L4-L5 intervertebral joint; L5 & L5-S1 intervertebral joint; and S1, S2, S3, S4, S5, and coccygeal vertebrae. The technique for determining appendix location using vertebral references is illustrated in Figure 1.
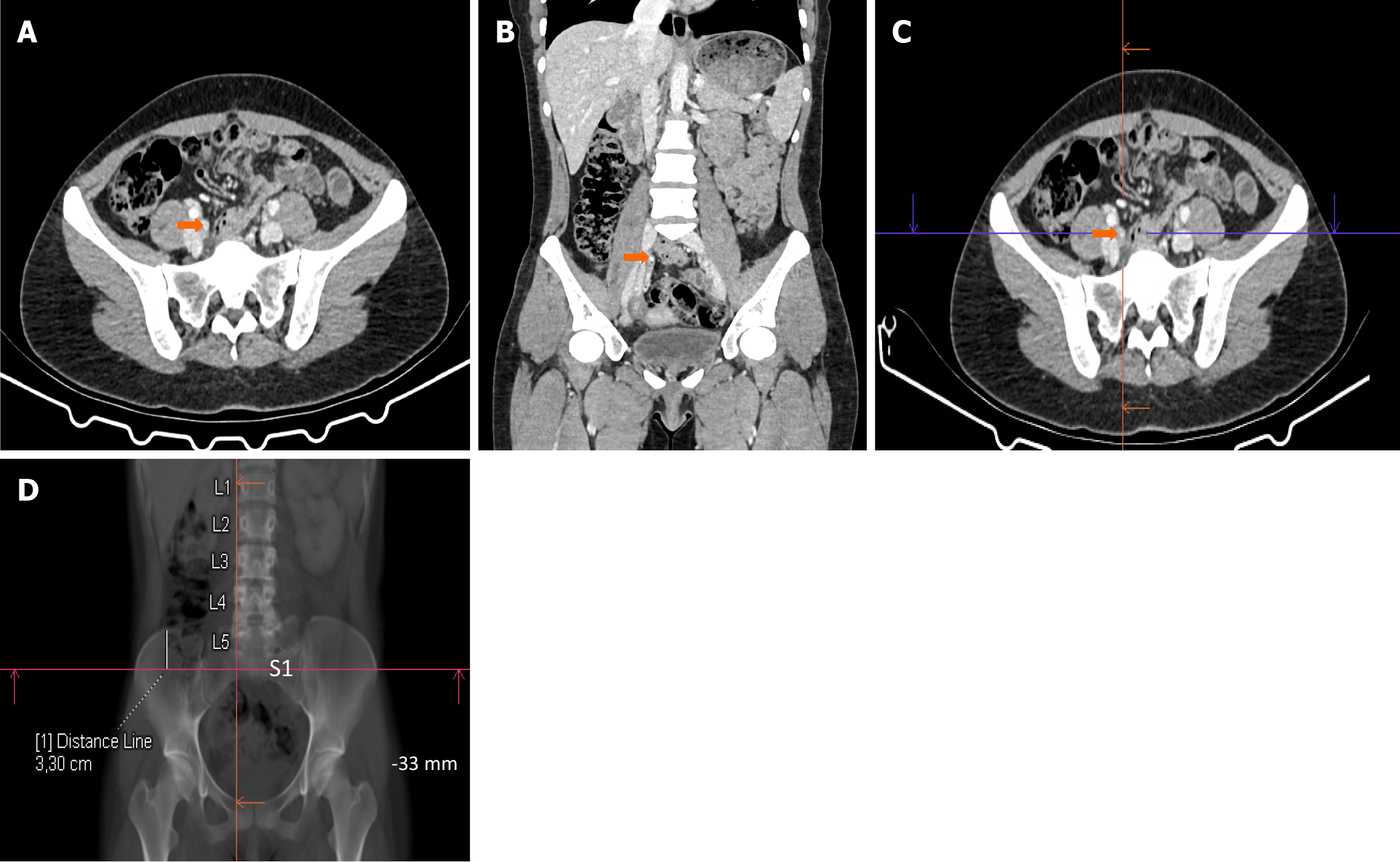
We also used the iliac bone as a reference to determine the location of the appendix with a more quantitative method. For this purpose, we found and marked the lowest, and highest points, and origin of the appendix on axial CT images. We then measured the distance in millimeters between these marked appendix points on coronal reformatted images and the highest point of the right iliac bone using maximum-intensity projection images. If the marked appendix points were superior to the highest point of the right iliac bone, the measurement was expressed as a positive (+) value, and if more inferior, the measurement was expressed as a negative (−) value in millimeters. Figure 2 illustrates how the appendix was localized in reference to the right iliac bone.
The course of the appendix was also investigated in the study population. Appendix vermiformis was classified as “ascending” when it ended up higher than its point of origin and “descending” when it ended up lower than its point of origin. The relationship between appendix location and some anthropometric parameters like height, weight, and body mass index (BMI) was also investigated; BMI was calculated using the formula: Weight/height² (kg/m²). Age and sex data were also collected.
Data were analyzed using SPSS version 20.0 (IBM Corp., Armonk, NY, United States). The distribution of the data was examined for normality using the Kolmogorov-Smirnov test. Numerical data following a normal distribution were presented as mean ± standard deviation, while categorical data were shown as numbers and percentages [n (%)]. The χ2 test was used to compare percentages between the acute appendicitis and normal appendix groups. The mean values of Ap0, ApA, and ApB were compared between male and female patients, as well as between the acute appendicitis and normal appendix groups, using Student’s t-test. Pearson correlation analysis was used to examine potential correlations between ApA and ApB values and anthropometric characteristics (weight, height, and BMI) and age. A P value less than 0.05 was considered statistically significant.
The final analysis comprised 427 patients, of which 206 (48.2%) were female and 221 (51.8%) were male. The mean patient age was 42.1 ± 19.5 (range: 18-90) years. Of the 427 CT scans, 200 (46.8%) were performed with intravenous contrast media administration, and 227 (53.2%) were performed without contrast media. The mean BMI was 25.6 kg/m² ± 6.4 (range: 16.8-40.5) kg/m².
Acute appendicitis was diagnosed on CT in 68 (15.9%) patients, and the diagnosis was subsequently confirmed in surgical specimens. In 359 (84.1%) patients, the appendix appeared normal on CT, and clinical follow-up confirmed the absence of acute appendicitis. In the overwhelming majority of patients (n = 325) who were clinically confirmed not to have acute appendicitis, abdominal pain resolved spontaneously or with simple analgesics. In the remaining patients (n = 34), a combination of clinical and CT findings led to alternative diagnoses of omental infarction (n = 2), sigmoid diver
The appendix had an ascending course in the majority of patients, both with and without acute appendicitis (89.7% and 90.5%, respectively). There was no statistically significant difference in the course of the appendix between the normal appendix and acute appendicitis groups (P = 0.41). The numbers and percentages of ascending and descending appendix courses for the overall population, the appendicitis group, and the normal appendix group are displayed in Table 1.
| Groups | Ascending | Descending | Total |
| Acute appendicitis | 61 (89.7) | 7 (10.3) | 68 (15.9) |
| Normal appendix | 325 (90.5) | 34 (9.5) | 359 (84.1) |
| Total | 386 (90.4) | 41 (9.6) | 427 (100) |
Measurements of the appendiceal origin (Ap0), the highest point of the appendix (ApA), and the lowest point of the appendix (ApB) were made in relation to the highest point of the right iliac bone in the normal appendix group, acute appendicitis group, and the overall population (n = 427). The mean ± SD, minimum, and maximum values for these measurements in each group are shown in Table 2. No statistically significant difference was found between the acute appendicitis and normal appendix groups in the ApB location relative to the right iliac bone (P = 0.19). However, a significant difference was found between these groups in the Ap0 and ApA locations relative to the right iliac bone (P = 0.04 and P = 0.04; respectively).
| Groups | Ap0 (origin) | ApA (highest point of the appendix) | ApB (lowest point of the appendix) |
| Acute appendicitis group (n = 68) | (−) 34.1 ± 29.1; (−) 100.8 − (+) 44.2 | (−) 17.1 ± 27.8; (−) 84.8 − (+) 48.3 | (−) 60.9 ± 27.9; (−) 121.6 − (+) 39.1 |
| Normal appendix group (n = 359) | (−) 42.3 ± 31.5; (−) 126.0 − (+) 40.1 | (−) 24.2 ± 34.1; (−) 126.0 − (+) 87.4 | (−) 59.8 ± 30.2; (−) 140.5 − (+) 44.1 |
| Total (n = 427) | (−) 41.0 ± 32.7; (−) 126.0 − (+) 44.2 | (−) 23.0 ± 30.8; (−) 126.0 − (+) 87.4 | (−) 60.0 ± 30.2; (−) 140.5 − (+) 44.1 |
No significant statistical difference was found between male and female patients in the measurements of ApA and ApB in relation to the right iliac bone (P = 0.08 and P = 0.21, respectively). However, a significant difference was found between male and female patients in the measurements of Ap0 in relation to the right iliac bone (P = 0.03). The mean values of Ap0, ApA, and ApB relative to the right iliac bone for male and female patients are shown in Table 3.
| Sex | Ap0 (mean ± SD) | ApA (mean ± SD) | ApB (mean ± SD) |
| Female (n = 206) | (−) 48.1 ± 30.0 | (−) 26.2 ± 30.4 | (−) 60.4 ± 31.1 |
| Male (n = 221) | (−) 34.3 ± 29.7 | (−) 20.0 ± 29.8 | (−) 59.6 ± 30.8 |
| Total (n = 427) | (−) 41.0 ± 32.7 | (−) 23.0 ± 30.8 | (−) 60.0 ± 30.2 |
In the normal appendix population, ApA ranged from the L2 vertebral body to the coccygeal vertebrae, while in the acute appendicitis population, ApA ranged from the L2 vertebra to the S3-S4 intervertebral joint. In the normal appendix population, ApB ranged from the L2 vertebral body to the coccygeal vertebrae, and in the acute appendicitis population, ApB ranged from the L4 vertebral body to the coccygeal vertebrae. ApA was most commonly found at the L5 and L5-S1 intervertebral joint level (34.4%), while ApB was most commonly found at the S1 vertebral body level (22.5%). No significant difference was found between the acute appendicitis group and the normal appendix group in the localization of ApA and ApB relative to the vertebrae (P = 0.19). ApA was located at or below the level of the L3 vertebra in all pa
The numbers and percentages of ApA and ApB localizations in relation to the vertebrae are shown in Table 4.
| Vertebral levels | ApA | ApB |
| L1& L1-L2 intervertebral joint distance | 0 (0) | 0 (0) |
| L2& L2-L3 intervertebral joint distance | 8 (1.9) | 1 (0.2) |
| L3& L3-L4 intervertebral joint distance | 29 (6.8) | 2 (0.5) |
| L4 & L4-L5 intervertebral joint distance | 88 (20.6) | 20 (4.7) |
| L5 & L5-S1 intervertebral joint distance | 147 (34.4) | 81 (19.0) |
| S1 vertebra | 95 (22.2) | 96 (22.5) |
| S2 vertebra | 34 (8.0) | 81 (19.0) |
| S3 vertebra | 19 (4.4) | 66 (15.5) |
| S4 vertebra | 4 (0.9) | 56 (13.1) |
| S5 vertebra & coccygeal vertebrae | 3 (0.7) | 24 (5.6) |
A weak negative correlation was found between patient age, height, BMI, and the vertebral levels of ApA and ApB. No correlation was found between patient age, height, BMI, and the position of ApA and ApB relative to the right iliac bone. The P and R values are shown in Table 5.
| Appendix locations | Age | Height | BMI | |
| Relative to the vertebrae | ApA | P = 0.007/R = −0.13 | P = 0.006/R = −0.13 | P = 0.044/R = −0.09 |
| ApB | P = 0.028/R = −0.10 | P = 0.007/R = −0.13 | P = 0.01/R = −0.12 | |
| Relative to the right iliac bone | ApA | P = 0.33/R = −0.12 | P = 0.19/R = −0.10 | P = 0.12/R = −0.08 |
| ApB | P = 0.47/R = −0.09 | P = 0.53/R = −0.13 | P = 0.23/R = −0.14 |
Our aim in the study was to define the location of the appendix vermiformis using metric markers. In order to determine the appendix’s location, we used the vertebrae and the right iliac bone as references. By using these references, we examined the frequency and variability of appendix locations, examining associations with anthropometric parameters and the presence of acute appendicitis. We found a weak negative correlation between anthropometric parameters and the location of the uppermost (ApA) and lowermost (ApB) points of the appendix relative to the vertebrae; however, no correlation was found between anthropometric parameters and the location of the uppermost (ApA) and lowermost (ApB) points of the appendix relative to the right iliac bone. No significant difference was found between male and female patients in the localization of ApA and ApB in relation to the right iliac bone.
The need for medical imaging is growing faster than in the majority of other healthcare-related fields[21]. Today's clinicians have become increasingly dependent on imaging to confirm their clinical judgments before planning the management of acute abdominal conditions, including acute appendicitis. CT scan usage has risen sharply in the last two decades because of its reported higher accuracy compared to US for diagnosing acute appendicitis. As a result, many institutions now prefer CT as the primary imaging modality in suspected cases of acute appendicitis[22].
A consensus known as ALARA has been established in radiological practice to restrict the amount of radiation that patients are exposed to, with broad and well-founded support[23]. Reducing the FOV is one approach to decreasing radiation exposure. Therefore, it is important to know the radiological location of the appendix in the population[24].
The scientific literature contains studies that investigate the visibility rates of appendix vermiformis[25,26], various positions of the appendiceal tip (such as retrocecal or pelvic)[25,26], and uncommon locations of the appendix ver
In our study, the appendix was found to have an ascending course most frequently in the acute appendicitis group, the normal appendix group, and the overall population (89.7%, 90.5%, and 90.4%, respectively). To the best of our knowledge, this is the first study to use radiological techniques to assess whether the appendix is ascending or descending in its course. Also, this is the first publication to examine the impact of acute appendicitis on the course of the appendix, with no significant difference found between the acute appendicitis and normal appendix groups. Understanding whether the appendix is positioned in an upward (ascending) or downward (descending) direction in the majority of the population can provide valuable guidance for surgical procedures.
To our knowledge, no previous study has determined the location of the appendix relative to the iliac bone in the population. In our study, the appendix was observed between (−) 140.5 mm and (+) 87.4 mm relative to the highest point of the right iliac bone. A significant difference was found between the acute appendicitis and normal appendix groups in the Ap0 and ApA locations relative to the right iliac bone, and the appendix was located more superiorly in the acute appendicitis group compared to the normal appendix group. This finding suggests that the appendix tends to be in a more upright position when inflamed. We also investigated the relationship between appendix localization and anthropometric parameters and found that measurements based on the right iliac bone did not vary with these parameters, thus supporting the iliac bone as a reliable reference point.
We were the first to use vertebrae as a reference for locating the appendix in the adult population. Davis et al[28] localized the highest point in the course of the appendix (expressed as ApA in our study) in the pediatric population, also using the vertebrae as a reference. Although their study was conducted in the pediatric population, they found ApA most frequently in the L5 vertebral level, as in our study. We found that ApA was located at or below the L3 vertebra in all patients with appendicitis, aligning with the findings of Davis et al[28]. In our study, the location of the appendix relative to the spine was inversely correlated with patient height, age, and BMI.
We localized the appendix relative to both the vertebrae and the right iliac bone in the population, creating a controlled trial within itself because it involves two distinct anatomical measurements. While there was variability in localization of the appendix relative to the vertebrae with age, height, and BMI, no variability was detected with these parameters according to the right iliac bone. This shows that the right iliac bone may be a more reliable reference point in de
Our study has some limitations. As with all retrospective and cross-sectional studies, an increase in sample size could alter the results. We conducted a single-center study, and all measurements were conducted by a single radiologist in a single session; therefore, intra- and interobserver variability could not be evaluated. Moreover, since the pediatric population was not included, we were unable to compare findings between adult and pediatric groups. Another limitation was the lack of intraoperative measurements to validate our results, as all measurements relied solely on CT images.
The highest point of the appendix was most frequently located at the L5 & L5-S1 intervertebral joint (34.4%), while the lowest point was most frequently found at the S1 vertebra level (22.5%). Relative to the right iliac bone, the origin, highest point, and lowest point of the appendix measured (−) 41.0 ± 32.7 mm, (−) 23.0 ± 30.8 mm, and (−) 60.0 ± 30.2 mm; respectively. While localization analyses based on vertebrae varied according to anthropometric variables, those based on the right iliac bone showed no variability. These findings provide a basis for future studies aimed at reducing ionizing radiation exposure.
| 1. | Deshmukh S, Verde F, Johnson PT, Fishman EK, Macura KJ. Anatomical variants and pathologies of the vermix. Emerg Radiol. 2014;21:543-552. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 26] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 2. | Schumpelick V, Steinau G, Schlüper I, Prescher A. Surgical embryology and anatomy of the diaphragm with surgical applications. Surg Clin North Am. 2000;80:213-239, xi. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 93] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 3. | Hodge BD, Kashyap S, Khorasani-Zadeh A. Anatomy, Abdomen and Pelvis: Appendix. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing, 2024. [PubMed] |
| 4. | Aminova GG. [Structure and cytoarchitectonic of the lymphoid tissue of the Appendix of man in elderly and senile ages]. Adv Gerontol. 2018;31:273-279. [PubMed] |
| 5. | Ghorbani A, Forouzesh M, Kazemifar AM. Variation in Anatomical Position of Vermiform Appendix among Iranian Population: An Old Issue Which Has Not Lost Its Importance. Anat Res Int. 2014;2014:313575. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 6. | de Souza SC, da Costa SRMR, de Souza IGS. Vermiform appendix: positions and length – a study of 377 cases and literature review. J Coloproctology. 2015;35:212-216. [RCA] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 19] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 7. | Wakeley CP. The Position of the Vermiform Appendix as Ascertained by an Analysis of 10,000 Cases. J Anat. 1933;67:277-283. [PubMed] |
| 8. | Denjalić A, Delić J, Delić-Custendil S, Muminagić S. [Variations in position and place of formation of appendix vermiformis found in the course of open appendectomy]. Med Arh. 2009;63:100-101. [PubMed] |
| 9. | Constantin M, Petrescu L, Mătanie C, Vrancianu CO, Niculescu AG, Andronic O, Bolocan A. The Vermiform Appendix and Its Pathologies. Cancers (Basel). 2023;15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 10. | Bhangu A, Søreide K, Di Saverio S, Assarsson JH, Drake FT. Acute appendicitis: modern understanding of pathogenesis, diagnosis, and management. Lancet. 2015;386:1278-1287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 535] [Cited by in RCA: 685] [Article Influence: 68.5] [Reference Citation Analysis (0)] |
| 11. | Hardin DM Jr. Acute appendicitis: review and update. Am Fam Physician. 1999;60:2027-2034. [PubMed] |
| 12. | Hwang ME. Sonography and Computed Tomography in Diagnosing Acute Appendicitis. Radiol Technol. 2018;89:224-237. [PubMed] |
| 13. | Di Saverio S, Podda M, De Simone B, Ceresoli M, Augustin G, Gori A, Boermeester M, Sartelli M, Coccolini F, Tarasconi A, De' Angelis N, Weber DG, Tolonen M, Birindelli A, Biffl W, Moore EE, Kelly M, Soreide K, Kashuk J, Ten Broek R, Gomes CA, Sugrue M, Davies RJ, Damaskos D, Leppäniemi A, Kirkpatrick A, Peitzman AB, Fraga GP, Maier RV, Coimbra R, Chiarugi M, Sganga G, Pisanu A, De' Angelis GL, Tan E, Van Goor H, Pata F, Di Carlo I, Chiara O, Litvin A, Campanile FC, Sakakushev B, Tomadze G, Demetrashvili Z, Latifi R, Abu-Zidan F, Romeo O, Segovia-Lohse H, Baiocchi G, Costa D, Rizoli S, Balogh ZJ, Bendinelli C, Scalea T, Ivatury R, Velmahos G, Andersson R, Kluger Y, Ansaloni L, Catena F. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020;15:27. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 697] [Cited by in RCA: 601] [Article Influence: 120.2] [Reference Citation Analysis (109)] |
| 14. | Love BE, Camelo M, Nouri S, Kriger D, Ludi D, Nguyen H. Ultrasound Accuracy in Diagnosing Appendicitis in Obese Pediatric Patients. Am Surg. 2017;83:1063-1067. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 15. | Bahrami M, Mirgaloyebayat H, Mohajeri Z, Mohammadi H, Afshari SA, Fazeli P, Masaeli D, Nourian SMA. The diagnostic value of the computed tomography scan and ultrasonography in acute appendicitis. Am J Nucl Med Mol Imaging. 2023;13:11-17. [PubMed] |
| 16. | Frane N, Bitterman A. Radiation Safety and Protection. 2023 May 22. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. [PubMed] |
| 17. | Dixon MT, Loader RJ, Stevens GC, Rowles NP. An evaluation of organ dose modulation on a GE optima CT660-computed tomography scanner. J Appl Clin Med Phys. 2016;17:380-391. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 24] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 18. | Keyzer C, Tack D, de Maertelaer V, Bohy P, Gevenois PA, Van Gansbeke D. Acute appendicitis: comparison of low-dose and standard-dose unenhanced multi-detector row CT. Radiology. 2004;232:164-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 80] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 19. | Fefferman NR, Bomsztyk E, Yim AM, Rivera R, Amodio JB, Pinkney LP, Strubel NA, Noz ME, Rusinek H. Appendicitis in children: low-dose CT with a phantom-based simulation technique--initial observations. Radiology. 2005;237:641-646. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 30] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 20. | Sippola S, Virtanen J, Tammilehto V, Grönroos J, Hurme S, Niiniviita H, Lietzen E, Salminen P. The Accuracy of Low-dose Computed Tomography Protocol in Patients With Suspected Acute Appendicitis: The OPTICAP Study. Ann Surg. 2020;271:332-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 40] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 21. | Bercovich E, Javitt MC. Medical Imaging: From Roentgen to the Digital Revolution, and Beyond. Rambam Maimonides Med J. 2018;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 53] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 22. | Debnath J, George RA, Ravikumar R. Imaging in acute appendicitis: What, when, and why? Med J Armed Forces India. 2017;73:74-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 26] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 23. | Winder M, Owczarek AJ, Chudek J, Pilch-Kowalczyk J, Baron J. Are We Overdoing It? Changes in Diagnostic Imaging Workload during the Years 2010-2020 including the Impact of the SARS-CoV-2 Pandemic. Healthcare (Basel). 2021;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 49] [Cited by in RCA: 32] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 24. | Vogiatzi T, Menz R, Verna C, Bornstein MM, Dagassan-Berndt D. Effect of field of view (FOV) positioning and shielding on radiation dose in pediatric CBCT. Dentomaxillofac Radiol. 2022;51:20210316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 25. | Altunkas A, Aktas F, Ozmen Z, Albayrak E, Demir O. The Normal Vermiform Appendixin Adults. J Anat Soc India. 2022;71:225-233. [RCA] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 26. | Turkoglu H, Onur MR, Poyraz AK, Kocakoc E. Evaluation of normal appendix vermiformis in adults with multidetector computed tomography. Clin Imaging. 2012;36:758-762. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 27. | Zacharzewska-Gondek A, Szczurowska A, Guziński M, Sąsiadek M, Bladowska J. A pictorial essay of the most atypical variants of the vermiform appendix position in computed tomography with their possible clinical implications. Pol J Radiol. 2019;84:e1-e8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 28. | Davis J, Roh AT, Petterson MB, Kopelman TR, Matz SL, Gridley DG, Connell MJ. Computed tomography localization of the appendix in the pediatric population relative to the lumbar spine. Pediatr Radiol. 2017;47:301-305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |