Published online Jul 28, 2022. doi: 10.4329/wjr.v14.i7.238
Peer-review started: February 14, 2022
First decision: April 8, 2022
Revised: May 6, 2022
Accepted: July 5, 2022
Article in press: July 5, 2022
Published online: July 28, 2022
Processing time: 162 Days and 12.4 Hours
Renal sympathetic denervation (RSD) provides a minimally invasive interventional treatment modality for patients with resistant hypertension. However, the post-operative outcomes remain a key area of investigation since its earliest clinical trials.
To evaluate patient outcomes after RSD intervention among peer-reviewed patient cases.
A systematic review of literature on MEDLINE, Google Scholar, and the Cochrane Database of Systematic Reviews for RSD case studies to assess post-operative hypertension readings and medical management.
Among 51 RSD cases, the post-operative RSD patients report an apparent reduction with a mean number of 3.1 antihypertensive medications. The mean systolic arterial blood pressure 1 year following RSD was 136.0 mmHg (95%CI: 118.7-153.3).
The apparent improvements in office systolic blood pressure after 12 month post-operative RSD can support the therapeutic potential of this intervention for blood pressure reduction. Additional studies which utilized a uniform methodology for blood pressure measurement can further support the findings of this systematic review.
Core Tip: This is the first systematic review focused on peer-reviewed clinical case reports in the topic area of renal sympathetic denervation in hypertension outcomes. In addition, this study has noted the changes in blood pressure medication regimens for the management of resistant hypertension.
- Citation: Singh SP, Varghese KJ, Qureshi FM, Anderson MC, Foxworth J, Knuepfer MM. Catheter-based renal sympathetic nerve denervation on hypertension management outcomes. World J Radiol 2022; 14(7): 238-248
- URL: https://www.wjgnet.com/1949-8470/full/v14/i7/238.htm
- DOI: https://dx.doi.org/10.4329/wjr.v14.i7.238
Hypertension continues to be a pressing health condition worldwide. Despite widespread use of antihypertensive medications, it is estimated that only 24% of the patients who are prescribed these medications currently have their blood pressures controlled[1,2]. It is estimated that between 10% and 15% of patients with hypertension do not achieve adequate blood pressure control, despite the use of at least three antihypertensive agents[1,2]. Moreover, this group of patients is designated as having resistant hypertension[2]. Let alone, patients with true resistant hypertension bear a greater risk for mortality compared to the general population[3-5]. In fact, rates of cardiovascular events correlate with mean 24-hour ambulatory blood pressures, which further justifies the pressing need to innovate medical management of this condition[5]. Similarly, non-adherence to anti-hypertensive therapy is a significant problem that limits the success of drug therapies[6]. As such, the need for additional intervention beyond medication in patients with resistant hypertension is apparent.
Renal sympathetic denervation (RSD) has been proposed as a potential solution to control arterial pressure. Moreover, RSD is a catheter-based renal denervation which employs transvascular ablation of the renal sympathetic nerves using radiofrequency energy to interrupt both sensory and motor nerves through the renal arterial wall. The earliest clinical studies on RSD demonstrated a significant reduction in arterial pressure in most patients[7-9]. However, the body of evidence has largely been in dispute as to what the true postoperative outcomes are regarding this novel procedure. In fact, the SYMPLICITY HTN-3 clinical trial did not show a benefit for patients treated with the procedure compared to the sham group[10]. This has prompted the numerous additional studies of the effects of RSD. Most of these studies have reported reductions of ambulatory blood pressure, but the extent and location of ablation sites have varied considerably[10-12]. The efficacy of this procedure is difficult to evaluate due to widely varying levels of denervation and often the lack of appropriate control groups[11]. Despite this paucity in evidence, there have been a number of clinical cases reported in peer-reviewed literature which showcase the utilization of catheter-based renal denervation. However, there has not been a systematic review of these cases to consolidate the findings. Therefore, the aim of this study is to assess the efficacy of RSD treatment in attenuating systolic blood pressures and reducing antihypertensive agents among patients with resistant hypertension.
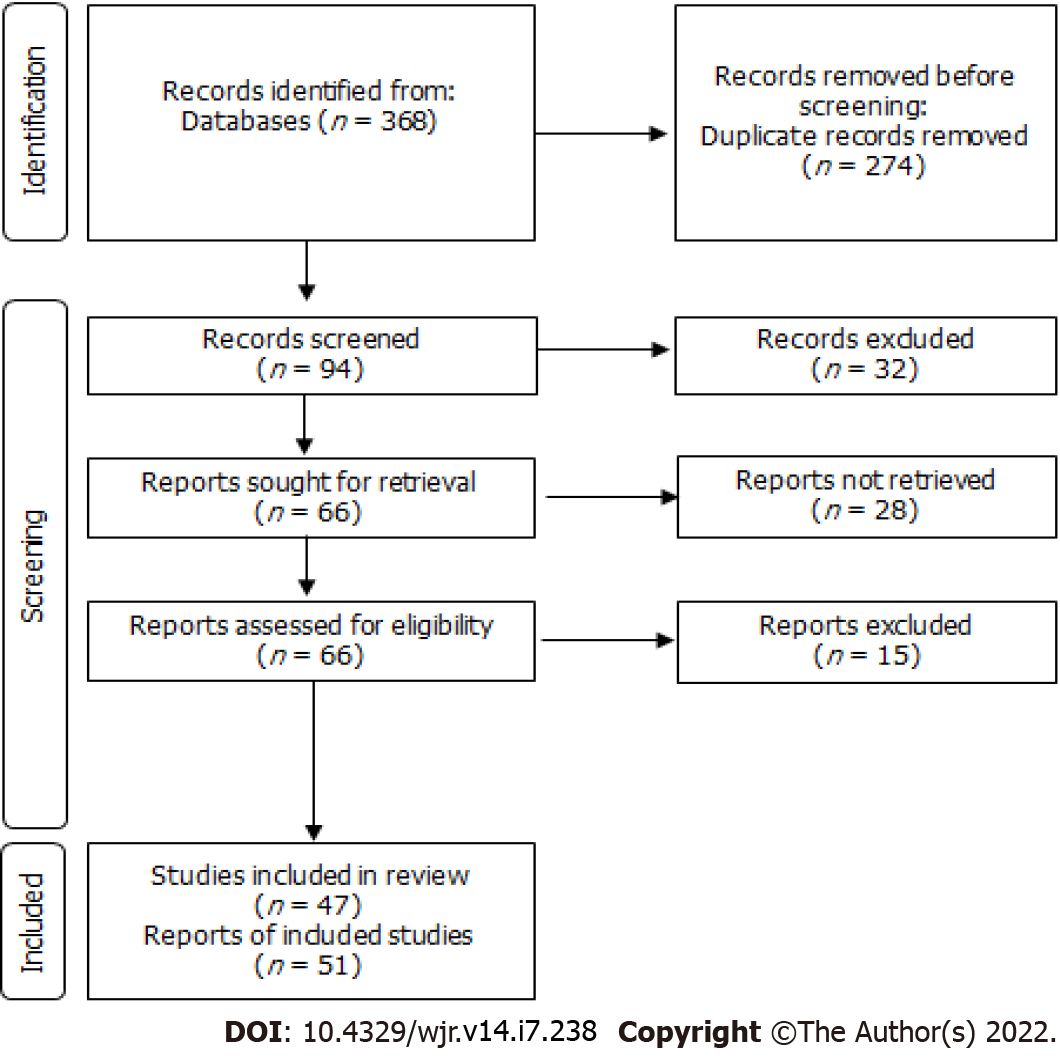
A systematic review of literature was performed on MEDLINE, Google Scholar, and the Cochrane Database of Systematic Reviews for renal denervation case studies. This study methodology was registered by PROSPERO International prospective register of systematic reviews (National Institute for Health Research). The search was performed following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines and checklist.3 Contingent valuation studies within renal denervation procedures were identified using search terminologies that combined the following epidemiological terms: renal sympathetic denervation, renal sympathetic ablation, hypertension renal denervation, renal denervation case studies, renal denervation case reports. Variations of the terms were also used when deemed necessary by the reviewers (e.g., “study” vs “studies”).
The initial search yielded 368 articles. Duplicates were removed, and then each article was reviewed for the following inclusion criteria: English language, case reports, full-text, pertinence to renal denervation procedures, and peer-reviewed (Figure 1). In addition, the reference list of each identified study was also reviewed to further ensure that all appropriate studies were identified. No further articles met the inclusion criteria. This qualitative synthesis yielded 62 articles.
Each study included was independently appraised by three reviewers (Singh SP, Varghese KJ, Qureshi FM) for literature quality and categorical data including: patient age, sex, ethnicity, height, weight, hypertension diagnosis, years hypertensive, blood pressure reading prior to renal denervation, presentation to emergency department, medications prior to renal denervation procedure, previous treatments related to hypertension, past medical/social/family history, renal denervation approach, number of lesions, duration of lesion/ablation, brand name of ablation catheter, bilateral (Y/N), renal artery length/diameter(s), days until discharge, blood pressure readings on follow-up, post-treatment medications, success in attenuating hypertension, and complications post-procedure. If there was any discrepancy between the three reviewers, discussion was conducted, and final determination was made by Singh SP. Meta-analyses were not performed due to a heterogeneity in reporting methodologies.
Statistical analysis was performed using Stata 14 Statistical Package (StataCorp, College Station, TX, United States) for descriptive statistics on the variables of interest including counts, percentages, means and standard deviations where appropriate. ANOVA calculations were performed to determine significance between variable groups of interest. The level of significance was set at P < 0.05.
The systematic review identified 368 records through the search methodology (Figure 1). After duplicates were removed, 94 records remained and 66 of those records were then screened and assessed for eligibility. This left a total of 43 complete studies to be included in the qualitative synthesis. Three of these studies included multiple patients. In total, 51 patient cases involving renal denervation procedures for hypertension were extracted from the 43 studies examined. The articles included in this study were published between 2012 and 2021. The peak year for case study reports was 2015 (n = 12), followed by 2013 (n = 11), 2012 (n = 7), 2014 (n = 6), 2017 and 2018 (n = 4), 2021 (n = 3), 2019 and 2020 (n = 1), respectively.
Among patients treated with RSD, 24 were female, 27 were male. The mean age of the patient population was 49.9 years (95%CI: 44.9-55.0) with the youngest being 6 years and the oldest being 83 years. Among sexes, the mean age of females was 50.1 (95%CI: 41.7-58.5) and for males was 49.5 (95%CI: 43.3-55.8). The mean body mass index (BMI) of the patient population was 31.3 (95%CI: 27.4-35.2). Among sexes, the mean BMI of females was 31.6 (95%CI: 25.3-37.9) and males was 31.0 (95%CI: 24.7-37.3).
The reviewers identified the terminology used for diagnosis of hypertension for each of the 51 patients studied and stratified these to identify 40 patients with resistant hypertension. Additionally, not all studies reported the number of years patients were hypertensive prior to RSD. Among those that did, the total patient population had a mean duration of diagnosed hypertension of 10.1 years (95%CI: 4.5-15.8), with the mean for males being 8.1 years (95%CI: -1.2-17.4) and females being 11.8 years (95%CI: 2.4-21.2). Additionally, of the patients diagnosed with resistant hypertension, the mean decreases to 7.8 years (95%CI: 3.4-12.1).
Two patients underwent RSD treatment following a presentation of hypertensive crisis in the Emergency Department. Six patients reported a history of diabetes (type 1: n = 1; type 2: n = 5). Another 4 patients reported polycystic kidney disease. One patient reported fibromuscular dysplasia. Histories of myocardial infarctions, hypercholesterolemia and hyperlipidemia were not compiled due to variations in reporting these potential contributing factors. No patient underwent RSD before the case report. Prior to RSD treatment, patient histories reported a mean number of 4.7 antihypertensive medications (95%CI: 4.1-5.4) as shown in Table 1.
| Ref. | Patients, n | Age (yr) | Sex | Brand |
| Aksu et al[21] | 1 | 46 | M | MARINER |
| Alegria-Barrero et al[22] | 1 | 53 | M | SYMPLICITY |
| Armaganijan et al[23] | 1 | 29 | F | |
| Atas et al[24] | 1 | 42 | F | SYMPLICTY, ARDIAN |
| Berra et al[25] | 1 | 54 | M | SYMPLICITY |
| Bilge et al[26] | 1,1 | 41, 51 | F, M | . |
| Yap et al[27] | 2 | 44, 69 | M, M | |
| Bonanni et al[28] | 1 | 6 | F | SYMPLICITY |
| Bortolotto et al[29] | 1 | 39 | F | MARINER |
| Celik et al[30] | 1 | 59 | M | SYMPLICITY |
| Chandra et al[31] | 1 | 51 | F | SYMPLICITY |
| Chiarito et al[32] | 1 | 47 | F | ARDIAN |
| Daemen et al[33] | 1 | 55 | M | RADIANCE |
| Ewen et al[34] | 1 | 61 | M | . |
| de Araújo Gonçalves et al[35] | 1 | 67 | F | SYMPLICITY |
| Gziut et al[36] | 1 | 62 | . | ENLIGHTN |
| Heradien et al[37] | 1 | 62 | F | SYMPLICITY |
| Himmel et al[38] | 1 | 83 | F | SYMPLICITY |
| Ho et al[39] | 1 | 58 | M | . |
| Jaguszewski et al[40] | 1 | 72 | F | ENLIGHTN |
| Kelle et al[41] | 1 | 62 | F | SYMPLICITY |
| Kiuchi et al[42] | 1 | 15, 16, 32 | F, F, M | ENLIGHTN |
| Koppelstaetter et al[43] | 1 | 68 | F | SYMPLICITY |
| Kostka-Jeziorny et al[44] | 1 | 52 | F | SYMPLICITY |
| Lee et al[45] | 1 | 31 | F | SYMPLICITY |
| Lee et al[46] | 1 | 16 | M | |
| Luo et al[47] | 1 | 80 | F | |
| Miller et al[48] | 1 | 54 | M | |
| Możeńska et al[49] | 1 | 60 | M | |
| Ott et al[50] | 1 | 29 | F | SYMPLICITY |
| Papademetriou et al[51] | 1 | 59 | F | ENLIGHTN |
| Pietilä-Effati et al[52] | 4 | 24, 55, 56, 72 | M, F, F, M | SYMPLICITY |
| Prejbisz et al[53] | 1 | 26 | M | SYMPLICITY |
| Pucci et al[54] | 1 | 73 | F | SYMPLICITY |
| Raju et al[55] | 1 | 19 | M | STOCKERT |
| Shah et al[56] | 1 | 74 | M | SYMPLICITY |
| Spinelli et al[57] | 1 | 39 | M | SYMPLICITY |
| Sridhar et al[58] | 1 | 67 | F | SYMPLICITY |
| Stefanadis et al[59] | 1 | 74 | M | SYMPLICITY |
| Tsioufis et al[60] | 1 | 58 | M | |
| Versaci et al[61] | 1 | 49 | M | VESSIX |
| Wang et al[62] | 1 | 49 | M | |
| Wu et al[63] | 1 | 62 | M | CORDIS |
The mean standard office blood pressure of patients prior to RSD treatment was assessed. The mean systolic blood pressure was 172.7 mmHg (95%CI: 165.1-180.3) among the entire patient population, and 171.4 mmHg (95%CI: 162.3-180.4) among those with resistant hypertension. Females had a mean systolic blood pressure of 170.2 mmHg (95%CI: 158.2-183.3), and males had a mean of 175.5 mmHg (95%CI: 164.7 – 186.3).
The first-generation SYMPLICITY renal denervation catheter® (Medtronic, Dublin, Ireland) was the most commonly used, being identified in 57.5% of cases (n = 40). This frequency was greater than EnligHTN renal artery ablation catheter® (St. Jude Medical, Inc., Saint Paul Minnesota) at 15%. The remaining cases used other available treatments. The mean number of ablations on the left renal artery was 5.0 (95%CI: 3.2-6.8), and the right renal artery was 5.3 (95%CI: 3.5-7.2). The reported duration of an ablation varied among each study, noting the shortest duration at 10 s, and longest duration at 120 s. Four studies reported discharge from the hospital within 24 h of treatment.
Three studies reported renal artery stenosis in at least 1 artery during follow up appointments. One study noted progression into aortic stenosis. Two studies reported aortic dissection, one occurring during the operation, and the second reported the dissection twenty-two months post-operatively. In both cases, the dissection was deemed unrelated to the RSD procedure. Episodes of hypertensive crises post-treatment were not reported in any of the case studies. In addition, the mean standard office blood pressure (BP) of patients post-RSD treatment was assessed. The mean post-operative systolic blood pressure of reported cases was reported at 24 h, 1 mo, 3 mo, 6 mo and 1 year after surgery (Table 2). The arterial pressure appeared to be significantly reduced although all measurements were not done at all time points in all these studies. After RSD treatment, patient follow-up histories in some reports described an apparent reduction with a mean number of 3.1 antihypertensive medications (95%CI: 2.3-3.9) in all patients (Table 3).
| Mean systolic blood pressure | ||||||
| Prior to RSD | Time post-RSD | |||||
| 24 h | 1 mo | 3 mo | 6 mo | 1 yr | ||
| All subjects | 172.7 mmHg (95%CI: 165.1-180.3) | 146.2 mmHg (95%CI: 131.4-161.1) | 139.2 mmHg (95%CI: 124.8-153.6) | 132.9 mmHg (95%CI: 114.8-151.1) | 133.0 mmHg (95%CI: 120.7-145.31) | 136.0 mmHg (95%CI: 118.7-153.3) |
| Females | 170.2 mmHg (95%CI: 158.2-183.3) | 147.2 mmHg (95%CI: 125.7-168.7) | 137.0 mmHg (95%CI: 102.8-171.2) | 136.7 mmHg (95%CI: 105.3-168.7) | 130.0 mmHg (95%CI: 118.0-142.0) | 134.2 mmHg (95%CI: 107.4-161.0) |
| Males | 175.5 mmHg (95%CI: 164.7– 186.3) | 144.4 mmHg (95%CI: 114.0-174.8) | 137.0 mmHg (95%CI: 102.8-171.2) | 126.3 mmHg (95%CI: 117.2-135.3) | 1160.0 mmHg | 1131.0 mmHg |
| Mean number of antihypertensive medications | ||
| Pre-RSD | Post-RSD | |
| All subjects | 4.7 (95%CI: 4.1-5.4), | 3.1 (95%CI: 2.3-3.9), |
| Females | 4.9 (95%CI: 3.8-6.0) | 3.0 (95%CI: 1.0–5.0) |
| Males | 4.6 (95%CI: 3.7-5.5) | 3.0 (95%CI: 1.96-4.0) |
The aim of this systematic review of case reports was to examine the postoperative efficacy of RSD on blood pressure reduction in patients with resistant hypertension and evaluate the change in antihypertensive medication regimen. Overall, the therapeutic potential that this catheter-based procedure provides in attenuating hypertension merits its exploration. This search for contemporary case studies published in English medical journals yielded 48 patient cases which reviewers utilized to draw conclusions. The focus of this study is to determine the effect of RSD on blood pressure attenuation in hypertensive patients. Based on the most recent European Society of Cardiology (ESC) and the European Society of Hypertension (ESH) guidelines for the management of arterial hypertension, which classifies arterial blood pressures into grades[12], the mean standard office systolic blood pressure of patients prior to RSD treatment was between 160-179, or grade 2 hypertension, and ≥ 180, or grade 3 hypertension, among the patient population as a whole. The mean 24 h post-operative systolic blood pressure of reported cases was in grade 2 hypertension. At 1, 3, 6, and 12 month follow-up, the mean systolic arterial pressure of reported cases remained in grade 1 hypertension (systolic blood pressure between 140-159). For the majority of patients, the severity of hypertension declined from borderline-malignant hypertension to grade I hypertension. The resulting reduction in arterial pressure during these follow up visits are consistent with the results of larger renal denervation trials[7-9,12].
Regarding the current body of literature, the SYMPLICITY HTN-3 clinical trial which was performed in the United States reported the lack of a sustained reduction in arterial pressure after RSD[10]. Despite the observations in other studies showing reductions maintained for at least three years, the consistency of arterial pressure reduction has been controversial. There were similar observations in the case reports reviewed here, but the overall findings note a net reduction in blood pressure at one year follow up. In addition, the intention to evaluate the office systolic blood pressure readings is further supported by contemporary literature as a modality to objectively evaluate blood pressure reduction effects[13].
The most common instrument used in these studies was the first generation, radiofrequency device (Symplicity, Medtronic®). During the initial studies with this instrument, it was recommended that the device be advanced to the first bifurcation of the renal artery allowing for 3-6 RF lesions on each renal artery. Subsequent studies have shown that this has highly variable effects on depletion of renal catecholamines[14]. Additionally, it has been shown that the renal nerves are more closely apposed to the renal artery in the distal segments[15]. This has led to the development of smaller catheters with multiple electrode sites that can be advanced farther into the renal artery and are able to make many more focal lesions[16]. This has likely improved the success of the actual denervation making the second-generation devices more effective in RSD.
Contemporary clinical guidelines encourage a stepwise approach, involving combination therapy, in order to increase the number and doses of medications when treating hypertension. Additionally, this is also with the understanding that every drug has a limited capacity for blood pressure reduction[17,18]. Therefore, patients described in these reports with grade 2 or 3 hypertension were typically on several medications. Since it is known that adherence to antihypertensive drug therapy is poor[6], the permanence of the RSD treatment offers a significant advantage, including reducing drug therapies in some patients and thereby improving compliance. These case reports were encouraging in this regard, as this study reported an average reduction by one-to-two medications from the patient’s regimen. Furthermore, chronic administration of common antihypertensives can lead to adverse effects such as impotence with beta-blockers or angioedema with ACE inhibitors. Therefore, a desirable characteristic of RSD is a corresponding reduction in pharmacotherapy leading to improved compliance and reduced side effects.
Several case studies detailed complications of RSD, particularly associated with renal artery stenosis. While these were not deemed a major risk, the outcome can exacerbate hypertension. Furthermore, renal artery stenosis is a contraindication for medications such as ACE inhibitors or angiotensin receptor blockers. The combination of drug therapy and inhibiting Angiotensin II can significantly reduce renal function, particularly in the context of kidney disease. This study proposes the close monitoring of the renal arteries at the follow-up visits post-RSD treatment to track and quickly counter the occurrence of renal artery stenosis.
While the first United States-based trial (SYMPLICITY HTN-3) reported a reduction in arterial pressure in treated patients that was the same as the reduction observed in control patients[10], RSD has not been approved in the United States. Clinicians in the United States have a wealth of data because practitioners in other countries have been using RSD to treat resistant hypertension for nearly a decade. The International Sympathetic Nervous System Summit evaluated the future of RSD. The author’s conclusions include an expected 10 mmHg decrease in blood pressure and 25% decrease in overall cardiovascular events[19]. Furthermore, a large meta-analysis comparable to this review established similar findings. Warchoł-Celińska et al[7] included 613815 patients from 122 studies to find a reduction of office systolic blood pressure by 10 mmHg, cardiovascular events by 20%, and overall mortality by 13%. Adding our study to the current conversation supports the notion that RSD is an intervention with significant advantages[18,19]. It would be most beneficial to perform additional randomized control trials to acquire definitive evidence of the antihypertensive effects of RSD treatment.
Renal sympathetic denervation is a procedure that can manage resistant hypertension while avoiding the complications of drug adherence. Benefits of the procedure include sustainable attenuation of arterial pressure, reduced dependence on medications leading to fewer side effects, and to a reduction in the inherent diseases associated with hypertension. One limitation encountered in this analysis is that the antihypertensive medications detailed were only evaluated based on the quantity, dose or number that a patient was taking, not based on the class or mechanism of action. Furthermore, as all included articles were case studies, which can affect the validity of these results to translate into clinical reasoning and practice. Moreover, the use of case reports in a systematic review make the structure of this review require further investigation through larger systematic reviews in order to have more rigor in translational reasoning. Another area of development which would benefit future studies is through use of a artificial intelligence-controlled databases which can provide greater accuracy of citation retrieval in a systematic review (e.g., Reference Citation Analysis)[20]. Overall, this study recognizes that there is a need for more randomized control trials to establish the benefits of RSD, duration of effectiveness, incidence of complications, and improvement in all-cause mortality. Finally, findings of irregular attenuation of arterial pressure are likely confounded by improved quality of denervation afforded by newer devices. This procedure offers a viable option to control blood pressure with significant advantages over current treatments that could improve the effectiveness of the treatment of hypertension.
The background behind this literature is the initial collaboration between SPS and MMK who explored the effects of renal afferent denervation from a basic science perspective. Of note, MMK has contributed to a number of early literatures regarding renal sympathetic denervation.
The utilization of thermal radiofrequency ablation in medical practice has grown tremendously over the past decade alone. We are motivated to contribute to the potential direction of bringing this therapeutic modality to greater avenues of evaluation compared to the past. Of note, renal sympathetic denervation (RSD) is not used in the United States yet.
The objective was to utilize current peer-reviewed case report data to gain a current understanding of the climate regarding RSD interventions.
Systematic Review of the literature.
RSD intervention has shown, in these case reports, to mainly lower office systolic blood pressure and lessen the patient burden on medication regimens.
The promising results of RSD can simplify therapeutic regimens in patients with resistant hypertension. There is a significant amount of area which can be explored in clinical trials in the future.
The study team believes this therapeutic intervention needs to be brought under greater attention among the interventional radiology community for it future usage.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Manrai M, India; Prkacin I, Croatia S-Editor: Ma YJ L-Editor: A P-Editor: Ma YJ
| 1. | Elliott WJ. Systemic hypertension. Curr Probl Cardiol. 2007;32:201-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 107] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 2. | Ritchey MD, Gillespie C, Wozniak G, Shay CM, Thompson-Paul AM, Loustalot F, Hong Y. Potential need for expanded pharmacologic treatment and lifestyle modification services under the 2017 ACC/AHA Hypertension Guideline. J Clin Hypertens (Greenwich). 2018;20:1377-1391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 63] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 3. | American Heart Association. Hypertension Guideline Resources. [cited August 3, 2020] Available from: https://www.heart.org/en/health-topics/high-blood-pressure/high-blood-pressure-toolkit-resources. |
| 4. | Oliveras A, de la Sierra A. Resistant hypertension: patient characteristics, risk factors, co-morbidities and outcomes. J Hum Hypertens. 2014;28:213-217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 64] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 5. | Judd E, Calhoun DA. Apparent and true resistant hypertension: definition, prevalence and outcomes. J Hum Hypertens. 2014;28:463-468. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 178] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 6. | Chang TE, Ritchey MD, Park S, Chang A, Odom EC, Durthaler J, Jackson SL, Loustalot F. National Rates of Nonadherence to Antihypertensive Medications Among Insured Adults With Hypertension, 2015. Hypertension. 2019;74:1324-1332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 62] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 7. | Warchoł-Celińska E, Prejbisz A, Florczak E, Kądziela J, Witkowski A, Januszewicz A. Renal denervation - current evidence and perspectives. Postepy Kardiol Interwencyjnej. 2013;9:362-368. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Esler MD, Böhm M, Sievert H, Rump CL, Schmieder RE, Krum H, Mahfoud F, Schlaich MP. Catheter-based renal denervation for treatment of patients with treatment-resistant hypertension: 36 month results from the SYMPLICITY HTN-2 randomized clinical trial. Eur Heart J. 2014;35:1752-1759. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 186] [Cited by in RCA: 195] [Article Influence: 17.7] [Reference Citation Analysis (0)] |
| 9. | Krum H, Schlaich MP, Sobotka PA, Böhm M, Mahfoud F, Rocha-Singh K, Katholi R, Esler MD. Percutaneous renal denervation in patients with treatment-resistant hypertension: final 3-year report of the Symplicity HTN-1 study. Lancet. 2014;383:622-629. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 454] [Cited by in RCA: 467] [Article Influence: 42.5] [Reference Citation Analysis (0)] |
| 10. | Bhatt DL, Kandzari DE, O'Neill WW, D'Agostino R, Flack JM, Katzen BT, Leon MB, Liu M, Mauri L, Negoita M, Cohen SA, Oparil S, Rocha-Singh K, Townsend RR, Bakris GL; SYMPLICITY HTN-3 Investigators. A controlled trial of renal denervation for resistant hypertension. N Engl J Med. 2014;370:1393-1401. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1571] [Cited by in RCA: 1595] [Article Influence: 145.0] [Reference Citation Analysis (0)] |
| 11. | Esler M. Renal denervation for treatment of drug-resistant hypertension. Trends Cardiovasc Med. 2015;25:107-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 39] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 12. | Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, Clement DL, Coca A, de Simone G, Dominiczak A, Kahan T, Mahfoud F, Redon J, Ruilope L, Zanchetti A, Kerins M, Kjeldsen SE, Kreutz R, Laurent S, Lip GYH, McManus R, Narkiewicz K, Ruschitzka F, Schmieder RE, Shlyakhto E, Tsioufis C, Aboyans V, Desormais I; ESC Scientific Document Group. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39:3021-3104. [PubMed] |
| 13. | Liang B, Liang Y, Li R, Gu N. Effect of renal denervation on long-term outcomes in patients with resistant hypertension. Cardiovasc Diabetol. 2021;20:117. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Feyz L, van den Berg S, Zietse R, Kardys I, Versmissen J, Daemen J. Effect of renal denervation on catecholamines and the renin-angiotensin-aldosterone system. J Renin Angiotensin Aldosterone Syst. 2020;21:1470320320943095. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 15. | van Amsterdam WA, Blankestijn PJ, Goldschmeding R, Bleys RL. The morphological substrate for Renal Denervation: Nerve distribution patterns and parasympathetic nerves. A post-mortem histological study. Ann Anat. 2016;204:71-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 43] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 16. | Wolf M, Hubbard B, Sakaoka A, Rousselle S, Tellez A, Jiang X, Kario K, Hohl M, Böhm M, Mahfoud F. Procedural and anatomical predictors of renal denervation efficacy using two radiofrequency renal denervation catheters in a porcine model. J Hypertens. 2018;36:2453-2459. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 17. | Paz MA, de-La-Sierra A, Sáez M, Barceló MA, Rodríguez JJ, Castro S, Lagarón C, Garrido JM, Vera P, Coll-de-Tuero G. Treatment efficacy of anti-hypertensive drugs in monotherapy or combination: ATOM systematic review and meta-analysis of randomized clinical trials according to PRISMA statement. Medicine (Baltimore). 2016;95:e4071. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 75] [Cited by in RCA: 58] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 18. | Guirguis-Blake JM, Evans CV, Webber EM, Coppola EL, Perdue LA, Weyrich MS. Screening for Hypertension in Adults: Updated Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA. 2021;325:1657-1669. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 65] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 19. | Kiuchi MG, Esler MD, Fink GD, Osborn JW, Banek CT, Böhm M, Denton KM, DiBona GF, Everett TH 4th, Grassi G, Katholi RE, Knuepfer MM, Kopp UC, Lefer DJ, Lohmeier TE, May CN, Mahfoud F, Paton JFR, Schmieder RE, Pellegrino PR, Sharabi Y, Schlaich MP. Renal Denervation Update From the International Sympathetic Nervous System Summit: JACC State-of-the-Art Review. J Am Coll Cardiol. 2019;73:3006-3017. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 73] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 20. | Baishideng Publishing Group Inc. Reference Citation Analysis.[cited June 29, 2022] Available from: https://www.referencecitationanalysis.com/. |
| 21. | Aksu T, Güler TE, Özcan KS, Bozyel S, Yalın K. Renal sympathetic denervation assisted treatment of electrical storm due to polymorphic ventricular tachycardia in a patient with cathecolaminergic polymorphic ventricular tachycardia. Turk Kardiyol Dern Ars. 2017;45:441-449. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 22. | Alegria-Barrero E, Teijeiro R, Casares M, Vega M, Blazquez MA, Martos R, De Diego C, Moreno R, Martin MA. Treating Refractory Hypertension: Renal Denervation With High-Resolution 3D-Angiography. Res Cardiovasc Med. 2013;2:106-108. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 23. | Armaganijan L, Staico R, Abizaid A, Moraes A, Moreira D, Amodeo C, Sousa M, Sousa JE. Unilateral renal artery sympathetic denervation may reduce blood pressure in patients with resistant hypertension. J Clin Hypertens (Greenwich). 2013;15:606. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 24. | Atas H, Durmus E, Sunbul M, Mutlu B. Successful accessory renal artery denervation in a patient with resistant hypertension. Heart Views. 2014;15:19-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 25. | Berra E, Rabbia F, Rossato D, Covella M, Totaro S, Chiara F, Di Monaco S, Veglio F. Renal sympathetic denervation in a previously stented renal artery. J Clin Hypertens (Greenwich). 2014;16:238-239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 26. | Bilge M, Tolunay H, Kurmuş O, Köseoğlu C, Alemdar R, Ali S. Percutaneous renal denervation in patients with resistant hypertension-first experiences in Turkey. Anadolu Kardiyol Derg. 2012;12:79-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 27. | Yap LB, Balachandran K. Renal Denervation in the treatment of Resistant Hypertension. Med J Malaysia. 2021;76:893-897. [PubMed] [DOI] [Full Text] |
| 28. | Bonanni A, Pasetti F, Ghiggeri GM, Gandolfo C. Renal denervation for severe hypertension in a small child with Turner syndrome: miniaturisation of the procedure and results. BMJ Case Rep. 2015;2015. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 29. | Bortolotto LA, Midlej-Brito T, Pisani C, Costa-Hong V, Scanavacca M. Renal denervation by ablation with innovative technique in resistant hypertension. Arq Bras Cardiol. 2013;101:e77-e79. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 30. | Celik IE, Acar B, Kurtul A, Murat SN. De novo renal artery stenosis after renal sympathetic denervation. J Clin Hypertens (Greenwich). 2015;17:242-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 31. | Chandra AP, Marron CD, Puckridge P, Spark JI. Severe bilateral renal artery stenosis after transluminal radiofrequency ablation of renal sympathetic nerve plexus. J Vasc Surg. 2015;62:222-225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 32. | Chiarito M, Scotti A, A Pivato C, Cottone G, Ballarotto C, Godino C, Margonato A. A Complicated Case of Resistant Hypertension. Acta Med Iran. 2017;55:525-529. [PubMed] |
| 33. | Daemen J, Van Mieghem N. First-in-man radial access renal denervation with the ReCor Radiance™ catheter. EuroIntervention. 2015;10:1209-1212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 34. | Ewen S, Mahfoud F, Böhm M. First-in-human experience: percutaneous renal denervation through a false lumen fenestration in aortic dissection type B. EuroIntervention. 2013;8:1110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 35. | de Araújo Gonçalves P, Teles RC, Raposo L. Catheter-based renal denervation for resistant hypertension performed by radial access. J Invasive Cardiol. 2013;25:147-149. [PubMed] |
| 36. | Gziut AI, Gil RJ. Denervation of three equivalent right renal arteries in a patient with resistant hypertension after left-sided nephrectomy: five-year follow-up. Postepy Kardiol Interwencyjnej. 2020;16:114-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 37. | Heradien MJ, Augustyn J, Saaiman A, Brink PA. First reported cases: renal denervation with second-generation multi-electrode catheter via brachial and radial access. Cardiovasc J Afr. 2016;27:53-55. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 38. | Himmel F, Bode F, Mortensen K, Reppel M, Franzen K, Schunkert H, Weil J. Successful single-sided renal denervation approach in a patient with stenosis of an accessory renal artery. J Clin Hypertens (Greenwich). 2012;14:187-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 39. | Ho HH, Foo D, Ong PJ. Successful preoperative treatment of a patient with resistant hypertension who had percutaneous renal denervation therapy before bariatric surgery. J Clin Hypertens (Greenwich). 2012;14:569-570. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 40. | Jaguszewski M, Ghadri JR, Lüscher TF, Templin C. Optical coherence tomography to reveal vascular lesions after catheter-based renal nerve ablation with a novel multi-electrode EnligHTN™ system. Kardiol Pol. 2013;71:775. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 41. | Kelle S, Teller DC, Fleck E, Stawowy P. Renal denervation in fibromuscular dysplasia. BMJ Case Rep. 2013;2013. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 42. | Kiuchi MG, Souto HB, Kiuchi T, Chen S. Case Report: Renal Sympathetic Denervation as a Tool for the Treatment of Refractory Inappropriate Sinus Tachycardia. Medicine (Baltimore). 2015;94:e2094. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 43. | Koppelstaetter C, Kerschbaum J, Lenzhofer M, Glodny B, Esterhammer R, Frick M, Alber H, Mayer G. Distal renal artery stenosis after percutaneous renal denervation leading to renal impairment but normotension. J Clin Hypertens (Greenwich). 2015;17:162-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 44. | Kostka-Jeziorny K, Radziemski A, Tykarski A, Niklas A, Grajek S. Effect of unilateral catheter-based renal sympathetic denervation in a patient with resistant hypertension. Kardiol Pol. 2015;73:132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 45. | Lee CJ, Kim BK, Yoon KB, Lee HY, Dominiczak AF, Touyz RM, Jennings GLR, Cho EJ, Hering D, Park S. Case of Refractory Hypertension Controlled by Repeated Renal Denervation and Celiac Plexus Block: A Case of Refractory Sympathetic Overload. Hypertension. 2017;69:978-984. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 46. | Lee SH, Lim DH, Lee JH, Chang K, Koo JM, Park HJ. Long-Term Blood Pressure Control Effect of Celiac Plexus Block with Botulinum Toxin. Toxins (Basel). 2016;8:51. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 47. | Luo G, Zhu JJ, Yao M, Xie KY. Computed tomography-guided chemical renal sympathetic nerve modulation in the treatment of resistant hypertension: A case report. World J Clin Cases. 2021;9:9970-9976. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 1] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 48. | Miller MA, Gangireddy SR, Dukkipati SR, Koruth JS, d'Avila A, Reddy VY. Renal sympathetic denervation using an electroanatomic mapping system. J Am Coll Cardiol. 2014;63:1697. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 49. | Możeńska O, Rosiak M, Gziut A, Gil RJ, Kosior DA. Firstinman experience with renal denervation of multiple renal arteries in a patient with solitary kidney and resistant hypertension. Pol Arch Intern Med. 2017;127:60-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 50. | Ott C, Schmid A, Ditting T, Sobotka PA, Veelken R, Uder M, Schmieder RE. Renal denervation in a hypertensive patient with end-stage renal disease and small arteries: a direction for future research. J Clin Hypertens (Greenwich). 2012;14:799-801. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 32] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 51. | Papademetriou V, Tsioufis C, Stefanadis C. Impressive blood pressure and heart rate response after percutaneous renal denervation in a woman with morbid obesity and severe drug-resistant hypertension. J Clin Hypertens (Greenwich). 2013;15:852-855. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 52. | Pietilä-Effati PM, Salmela AK, Koistinen MJ. Intravascular Renal Denervation in Renal Dialysis Patients with Uncontrolled Hypertension: A Case Series of Four Patients. Am J Case Rep. 2018;19:985-991. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 53. | Prejbisz A, Kądziela J, Lewandowski J, Florczak E, Zylińska E, Kłopotowski M, Witkowski A, Januszewicz A. Effect of percutaneous renal denervation on blood pressure level and sympathetic activity in a patient with polycystic kidney disease. Clin Res Cardiol. 2014;103:251-253. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 54. | Pucci G, Battista F, Lazzari L, Dominici M, Boschetti E, Schillaci G. Progression of renal artery stenosis after renal denervation. Impact on 24-hour blood pressure. Circ J. 2014;78:767-768. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 55. | Raju N, Lloyd V, Yalagudri S, Das B, Ravikishore AG. Renal denervation in a patient with Alport syndrome and rejected renal allograft. Indian Heart J. 2015;67 Suppl 3:S71-S73. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 56. | Shah S, Jimenez MA, Fishel RS. Irrigated radiofrequency ablation catheter and electro-anatomical mapping with computerized tomography integration for renal artery sympathetic denervation. J Invasive Cardiol. 2012;24:E308-E310. [PubMed] |
| 57. | Spinelli A, Da Ros V, Morosetti D, Onofrio SD, Rovella V, Di Daniele N, Simonetti G. Technical aspects of renal denervation in end-stage renal disease patients with challenging anatomy. Diagn Interv Radiol. 2014;20:267-270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 58. | Sridhar GS, Watson T, Han CK, Ahmad WA. Profound sustained hypotension following renal denervation: a dramatic success? Arq Bras Cardiol. 2015;105:202-204. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 59. | Stefanadis C, Toutouzas K, Vlachopoulos C, Tsioufis C, Synetos A, Pietri P, Tousoulis D, Tsiamis E. Chemical denervation of the renal artery with vincristine for the treatment of resistant arterial hypertension: first-in-man application. Hellenic J Cardiol. 2013;54:318-321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 60. | Tsioufis C, Dimitriadis K, Tsiachris D, Thomopoulos C, Kasiakogias A, Kordalis A, Kefala A, Kallikazaros I, Stefanadis C. Catheter-based renal sympathetic denervation for the treatment of resistant hypertension: first experience in Greece with significant ambulatory blood pressure reduction. Hellenic J Cardiol. 2012;53:237-241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 61. | Versaci F, Andò G, Chiocchi M, Romeo F. Long-term benefit of renal denervation on blood pressure control in a patient with hemorrhagic stroke. SAGE Open Med Case Rep. 2019;7:2050313X19870972. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 62. | Wang P, Wan J, Hou J, Liu S, Ran F. Renal denervation in a patient with a highly tortuous renal artery using a guide extension catheter: a case report. BMC Cardiovasc Disord. 2021;21:388. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 63. | Wu Y, Duan S, Qiang X, Ning Z, Xing C, Zhang B. Sympathetic renal denervation in hypertension with chronic kidney disease: a case report and review of literature. Int J Clin Exp Med. 2015;8:16858-16862. [PubMed] [DOI] [Full Text] |