Published online Jan 28, 2022. doi: 10.4329/wjr.v14.i1.19
Peer-review started: October 12, 2021
First decision: December 9, 2021
Revised: December 21, 2021
Accepted: January 11, 2022
Article in press: January 11, 2022
Published online: January 28, 2022
Processing time: 101 Days and 12.4 Hours
The American College of Radiology Thyroid Imaging Reporting and Data System (ACR TI-RADS) was introduced to standardize the ultrasound characterization of thyroid nodules. Studies have shown that ACR-TIRADS reduces unnecessary biopsies and improves consistency of imaging recommendations. Despite its widespread adoption, there are few studies to date assessing the inter-reader agreement amongst radiology trainees with limited ultrasound experience. We hypothesize that in PGY-4 radiology residents with no prior exposure to ACR TI-RADS, a statistically significant improvement in inter-reader reliability can be achieved with a one hour training session.
To evaluate the inter-reader agreement of radiology residents in using ACR TI-RADS before and after training.
A single center retrospective cohort study evaluating 50 thyroid nodules in 40 patients of varying TI-RADS levels was performed. Reference standard TI-RADS scores were established through a consensus panel of three fellowship-trained staff radiologists with between 1 and 14 years of clinical experience each. Three PGY-4 radiology residents (trainees) were selected as blinded readers for this study. Each trainee had between 4 to 5 mo of designated ultrasound training. No trainee had received specialized TI-RADS training prior to this study. Each of the readers independently reviewed the 50 testing cases and assigned a TI-RADS score to each case before and after TI-RADS training performed 6 wk apart. Fleiss kappa was used to measure the pooled inter-reader agreement. The relative diagnostic performance of readers, pre- and post-training, when compared against the reference standard.
There were 33 females and 7 males with a mean age of 56.6 ± 13.6 years. The mean nodule size was 19 ± 14 mm (range from 5 to 63 mm). A statistically significant superior inter-reader agreement was found on the post-training assessment compared to the pre-training assessment for the following variables: 1. “Shape” (k of 0.09 [slight] pre-training vs 0.67 [substantial] post-training, P < 0.001), 2. “Echogenic foci” (k of 0.28 [fair] pre-training vs 0.45 [moderate] post-training, P = 0.004), 3. ‘TI-RADS level’ (k of 0.14 [slight] pre-training vs 0.36 [fair] post-training, P < 0.001) and 4. ‘Recommendations’ (k of 0.36 [fair] pre-training vs 0.50 [moderate] post-training, P = 0.02). No significant differences between the pre- and post-training assessments were found for the variables 'composition', 'echogenicity' and 'margins'. There was a general trend towards improved pooled sensitivity with TI-RADS levels 1 to 4 for the post-training assessment while the pooled specificity was relatively high (76.6%-96.8%) for all TI-RADS level.
Statistically significant improvement in inter-reader agreement in the assigning TI-RADS level and recommendations after training is observed. Our study supports the use of dedicated ACR TI-RADS training in radiology residents.
Core Tip: There is a statistically significant improvement in inter-reader agreement among radiology trainees with limited ultrasound experience using the American College of Radiology Thyroid Imaging Reporting and Data System (TI-RADS) after training for TI-RADS grading and recommendations. This study demonstrates the learnability of TI-RADS in radiology trainees.
- Citation: Du Y, Bara M, Katlariwala P, Croutze R, Resch K, Porter J, Sam M, Wilson MP, Low G. Effect of training on resident inter-reader agreement with American College of Radiology Thyroid Imaging Reporting and Data System. World J Radiol 2022; 14(1): 19-29
- URL: https://www.wjgnet.com/1949-8470/full/v14/i1/19.htm
- DOI: https://dx.doi.org/10.4329/wjr.v14.i1.19
Thyroid nodules are detected in more than 50% of healthy individuals with approximately 95% representing asymptomatic incidental nodules[1-3]. Moreover, an increasing number of thyroid nodules are being detected in recent years on account of improved quality and increased frequency of medical imaging[4]. Although most thyroid nodules are benign and do not require treatment, adequate characterization is necessary in order to identify potentially malignant nodules[1-3]. The American College of Radiology Thyroid Imaging Reporting and Data System (ACR TI-RADS) was therefore introduced to standardize the ultrasound characterization of thyroid nodules based on 5 morphologic categories (composition, echogenicity, shape, margins, and echogenic foci). A TI-RADS score is obtained to represent the level of suspicion for cancer and further direct the need for follow-up and/or tissue sampling[5]. First published in 2017, ACR TI-RADS has been widely adopted by many centers worldwide. Studies have shown that ACR-TIRADS reduces unnecessary biopsies and improves consistency of imaging recommendations[6,7].
Despite its widespread adoption, there are few studies available to date assessing the inter-reader reliability of TI-RADS amongst radiology trainees with limited ultrasound experience. A single-institutional study performed in China by Teng et al [8] evaluated three trainees with less than three months of ultrasound experience, demonstrating fair to almost perfect agreement amongst readers for TI-RADS categorization, with improved agreement and diagnostic accuracy after training. To our knowledge, no similar inter-reader agreement studies have been performed in North American trainees. The purpose of this study is to evaluate the inter-reader reliability amongst radiology trainees before and after designated TI-RADS training in a North American institution.
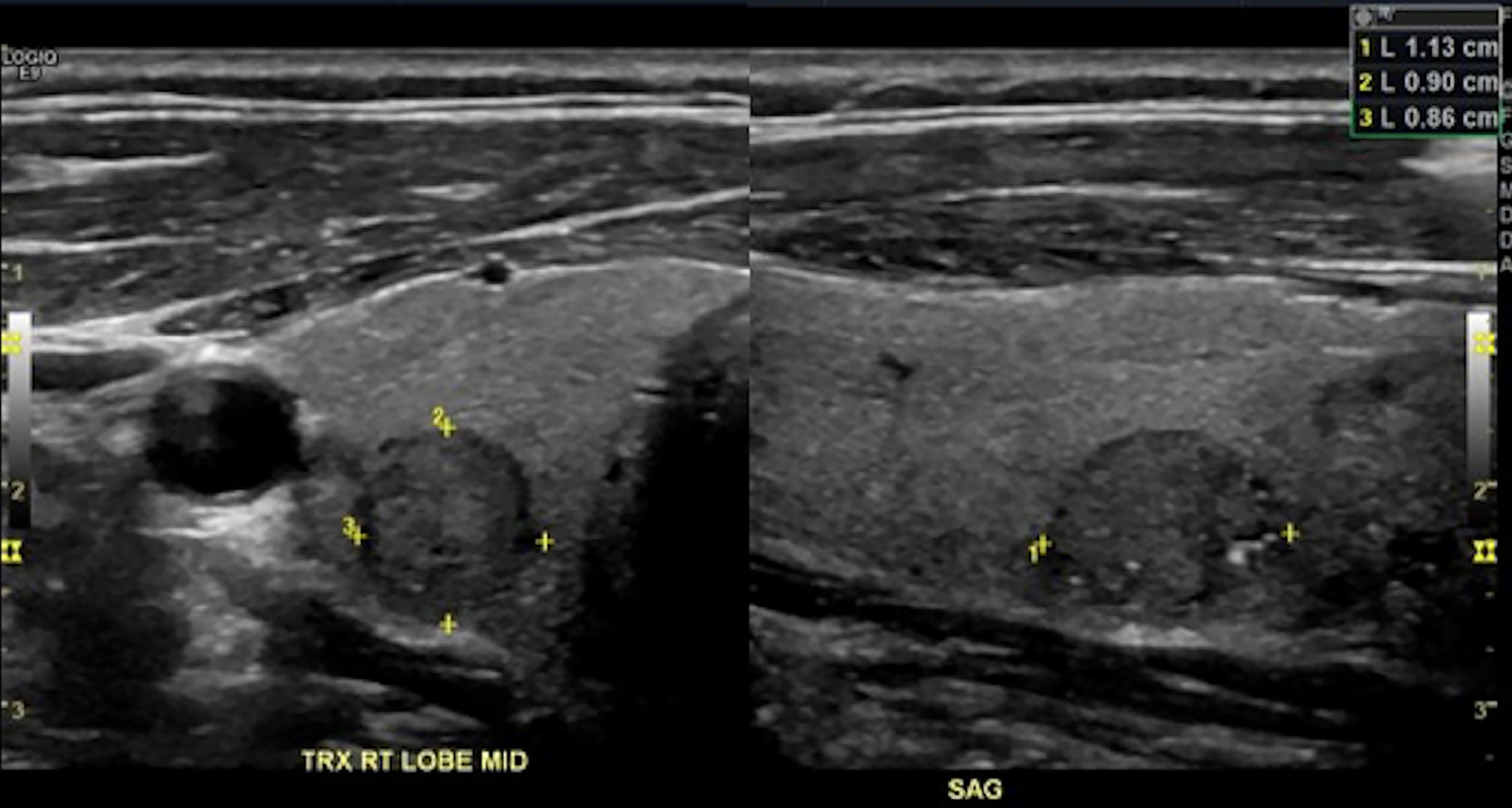
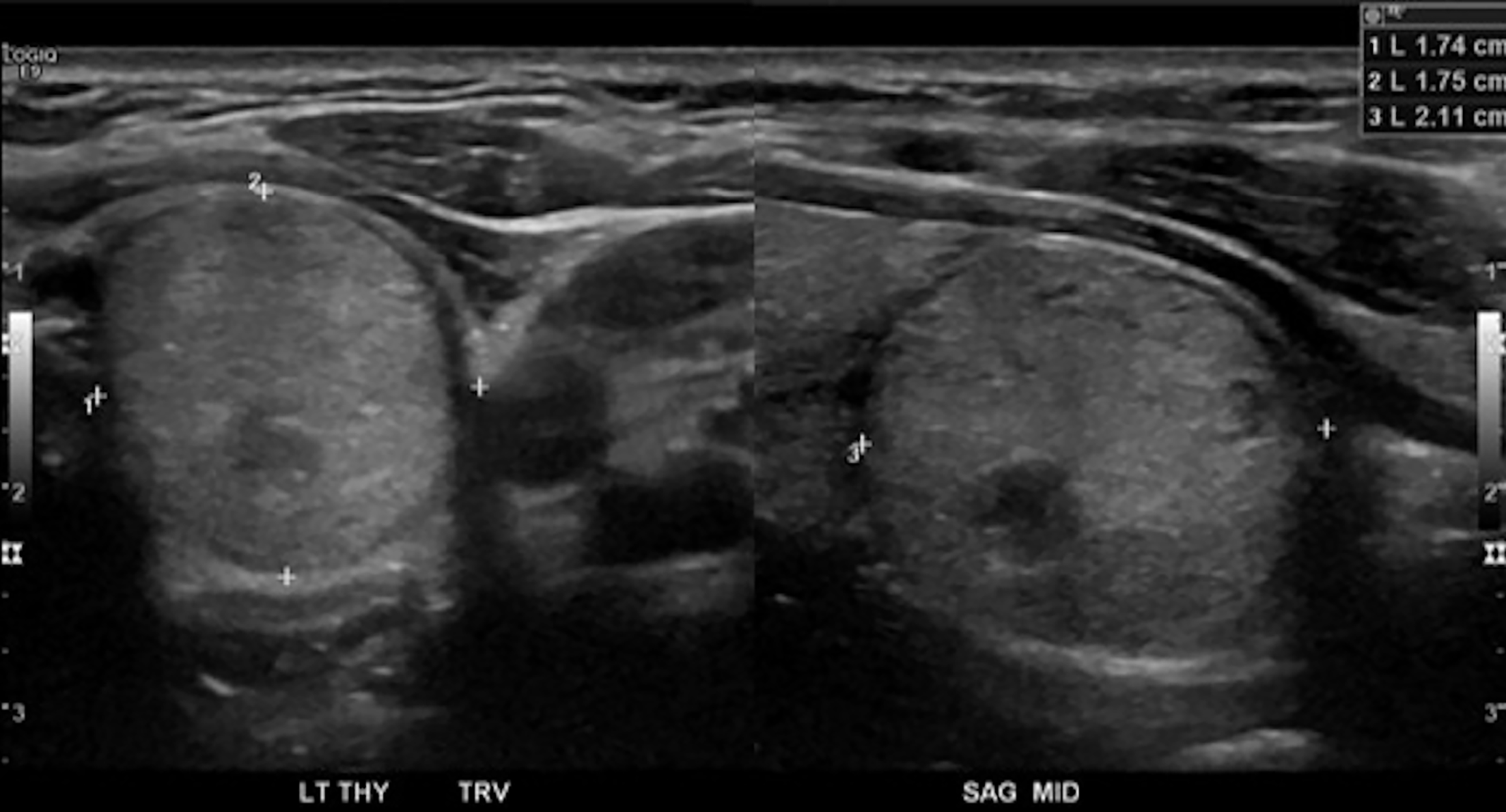
This retrospective, single-institution observational study was approved by the institutional Health Research Ethics Board (Pro 00104708). This study was exempted from obtaining informed consent. A retrospective review of the local Picture Archiving and Communication System (PACS) was performed to identify thyroid ultrasound studies containing thyroid nodules between July 1, 2019 to July 31, 2020. Included cases required at least 1 thyroid nodule (minimal dimension of 5 mm) with both transverse and sagittal still images and cine video recording in at least 1 plane. Nodules with non-diagnostic image quality, incomplete nodule visualization, and absence of a cine clip covering the entirety of the nodule were excluded. The type of ultrasound make, model, or platform were not considered in the selection process.
Eighty consecutive thyroid nodules meeting eligibility criteria were selected by 2 authors (YD, 6 years clinical experience; MB, 3 years clinical experience) from the eligible ultrasound examinations. A single case could include more than one nodule if sufficient imaging was available to meet inclusion criteria for multiple nodules. Still images of each nodule in both transverse and sagittal planes as well as at least 1 cine video clip of the nodule were saved in a teaching file hosted on our institutional Picture Archiving and Communication System. Each nodule and its representative images/cine clips were saved separately. If a single patient had two nodules, the relevant images and cine clips for each nodule were saved as separate case numbers. Of these, 50 cases were allocated into the “testing” group and 30 cases into the “training” group. Non-random group selection was performed to allow an approximately even distribution of TI-RADS categories within each group and to prevent under-representation of any category. A steering committee consisting of 2 authors including the principal investigator (YD, MB) attempted to evenly divide cases of differentiating difficulty equally between “testing” and “training” groups. This variable approach was selected over a pathological gold standard in an attempt to reduce referral bias in the “testing” group, a situation likely encountered by Teng et al [8] where 61% (245/400) of included nodules were pathologically malignant. The trainees were blinded to the distribution approach of the “testing” group.
All patient identifiers were removed apart from age and gender. All cases were evaluated by a consensus review of 3 independent fellowship-trained board-certified staff radiologists with between 1 and 14 years of clinical experience each (GL, MW, MS). Any disagreement on the scoring of nodules for the ACR TI-RADS level was resolved by re-review and consensus discussion. Findings on the consensus review were recorded and set as the standard of reference. This approach has been used in other recent inter-reader reliability studies assessing ACR Reporting and Data Systems[9].
Three PGY-4 radiology residents (trainees) were selected as blinded readers for this study. Each trainee had between 4 to 5 mo of designated ultrasound training, in addition to non-designated ultrasound training on other rotations throughout their training. No trainee had received specialized TI-RADS training prior to this study. Each of the readers independently reviewed the 50 testing cases and assigned TI-RADS score to each case. The readers were provided with a summary chart detailing the ACR TI-RADS classification as described in the ACR TI-RADS White Paper and had access to an online TI-RADS calculator (https://tiradscalculator.com) at the time of independent review[5]. The readers were instructed to assign TI-RADS points for each category including composition, echogenicity, shape, margins, echogenic foci, and to determine the TI-RADS level and ACR TI-RADS recommendations. The pre-training responses were entered into an online survey generated via Google Forms. Four weeks after the readers had completed the pre-training assessment; a one hour-long teaching session including a Microsoft PowerPoint presentation illustrating important features of ACR TI-RADS was provided to the readers along with a Microsoft Word document summarizing common areas of disagreement in nodule characterization[5]. The teaching session provided a step-by-step review of the 5 main sonographic features used for nodule scoring in ACR TI-RADS: (1) Composition; (2) Echogenicity; (3) Shape; (4) Margin; and (5) Echogenic foci. Each feature’s description and interpretation was discussed and illustrated by examples. The readers were given ample opportunity to ask questions, and the consensus panel provided focused clarification to readers in areas of reader uncertainty. Additionally, the trainees were instructed to review the training file that contained the 30 training cases on PACS and corresponding answers were provided for each case. Two weeks after the training session (six weeks after the pre-training assessment), the 50 anonymized cases from the ‘’testing’’ group were re-sent to the readers for independent review. Readers were instructed to re-score the 50 cases and the post-training responses were entered into an online survey generated via Google Forms.
Categorical variables were expressed as values and percentages. Continuous variables were expressed as the mean ± SD. The following statistical tests were used:
Fleiss kappa (overall agreement) was used to calculate the pooled inter-reader agreement. The kappa (K) value interpretation as suggested by Cohen was used: ≤ 0.20 (slight agreement), 0.21–0.40 (fair agreement), 0.41–0.60 (moderate agreement), 0.61–0.80 (substantial agreement), and 0.81–1.00 (almost perfect agreement)[10].
Paired t-test was used to evaluate for significant difference between agreement coefficients[11].
Using the consensus panel as the reference standard, the relative diagnostic parameters (sensitivity, specificity, positive predictive value and negative predictive value) per TI-RADS level were calculated for individual readers and on a pooled basis.
The testing cases comprised of 50 nodules in 40 patients. There were 33 (82.5%) females and 7 males. The mean patient age was 56.6 ± 13.6 years with an age range from 29 to 80 years. Of the 50 nodules, 31 (62%) were located in the right lobe, 18 (36%) in the left lobe and 1 (2%) in the isthmus. The mean nodule size was 19 ± 14 mm with a range from 5 to 63 mm. According to the reference standard that consisted of a consensus panel of 3 fellowship trained staff radiologists, there were 11 (22%) TI-RADS level 1 nodules, 9 (18%) TI-RADS level 2 nodules, 9 (18%) TI-RADS level 3 nodules, 13 (26%) TI-RADS level 3 nodules, and 8 (16%) TI-RADS level 5 nodules.
The pooled inter-reader agreement with the reference standard, pre- and post-training, is listed in Table 1. A statistically significant improvement in reader agree
| Pre-training, k | Post-training, k | P value of the difference | |
| Composition | 0.46 (95%CI: 0.37 to 0.54), moderate | 0.52 (95%CI: 0.44 to 0.61), moderate | 0.32 |
| Echogenicity | 0.36 (95%CI: 0.29 to 0.44), fair | 0.44 (95%CI: 0.37 to 0.52), moderate | 0.30 |
| Shape | 0.09 (95%CI: 0.02 to 0.21), slight | 0.67 (95%CI: 0.56 to 0.78), substantial | < 0.001 |
| Margins | 0.03 (95%CI: -0.14 to 0.08), slight | 0.05 (95%CI: -0.05 to 0.15), slight | 0.71 |
| Echogenic Foci | 0.28 (95%CI: 0.19 to 0.37), fair | 0.45 (95%CI: 0.36 to 0.53), moderate | 0.004 |
| TI-RADS Level | 0.14 (95%CI: 0.08 to 0.20), slight | 0.36 (95%CI: 0.30 to 0.42), fair | < 0.001 |
| Recommendations | 0.36 (95%CI: 0.27 to 0.45), fair | 0.50 (95%CI: 0.41 to 0.59), moderate | 0.02 |
| Sonographic feature | RS | R1 pre | R1 post | R2 pre | R2 post | R3 pre | R3 post |
| Composition | n | n (%) | |||||
| Spongiform | 4 | 0 (0) | 1 (25) | 1 (25) | 1 (25) | 3 (75) | 4 (100) |
| Cystic or almost completely cystic | 11 | 3 (27.3) | 5 (45.5) | 7 (63.6) | 8 (72.7) | 10(90.9) | 10(90.9) |
| Mixed cystic and solid | 12 | 9 (75) | 6 (50) | 5 (41.7) | 7 (58.3) | 5 (58.3) | 6 (50) |
| Solid | 27 | 26 (96.3) | 26 (96.3) | 25 (92.6) | 26 (96.3) | 18 (66.7) | 19 (70.4) |
| Echogenicity | |||||||
| Anechoic | 11 | 3 (27.3) | 5 (45.5) | 5 (45.5) | 5 (45.5) | 9 (81.8) | 8 (72.7) |
| Hyperechoic or isoechoic | 27 | 23 (85.2) | 23 (85.2) | 19 (70.4) | 21 (77.8) | 19 (70.4) | 20 (74.1) |
| Hypoechoic | 12 | 2 (16.7) | 4 (33.3) | 9 (75) | 8 (66.7) | 4 (33.3) | 4 (33.3) |
| Shape | |||||||
| Wilder than tall | 42 | 38 (90.5) | 39 (92.9) | 7 (16.7) | 39 (92.9) | 41 (97.6) | 40 (95.2) |
| Taller than wide | 8 | 7 (87.5) | 7 (87.5) | 7 (87.5) | 7 (87.5) | 6 (75) | 4 (50) |
| Margins | |||||||
| Smooth or ill defined | 47 | 36 (76.6) | 35 (74.5) | 35 (74.5) | 33 (70.2) | 43 (91.5) | 45 (95.7) |
| Lobulated or irregular | 3 | 1 (33.3) | 2 (66.7) | 1 (33.3) | 2 (66.7) | 0 (0) | 0 (0) |
| Echogenic foci | |||||||
| None or large comet tail artifact | 41 | 20 (48.8) | 36 (87.8) | 29 (70.7) | 39 (95.1) | 29 (70.7) | 29 (70.7) |
| Macrocalcification | 3 | 1 (33.3) | 1 (33.3) | 0 (0) | 2 (66.7) | 2 (66.7) | 2 (66.7) |
| Punctate echogenic foci | 6 | 5 (83.3) | 4 (66.7) | 2 (33.3) | 5 (83.3) | 3 (50) | 3 (50) |
| ACR TI-RADS level | RS, n | R1 pre, n (%) | R1 post, n (%) | R2 pre, n (%) | R2 post, n (%) | R3 pre, n (%) | R3 post, n (%) |
| 1 | 11 | 1 (9.1) | 5 (45.5) | 1 (9.1) | 7 (63.6) | 10 (90.9) | 8 (72.7) |
| 2 | 9 | 3 (33.3) | 4 (44.4) | 0 (0) | 4 (44.4) | 3 (33.3) | 3 (33.3) |
| 3 | 9 | 4 (44.4) | 5 (55.5) | 1 (11.1) | 6 (66.7) | 4 (44.4) | 6 (66.7) |
| 4 | 13 | 4 (30.8) | 5 (38.5) | 5 (38.5) | 9 (69.2) | 5 (38.5) | 5 (38.5) |
| 5 | 8 | 7 (87.5) | 4 (50) | 6 (75) | 5 (62.5) | 3 (37.5) | 3 (37.5) |
| Recommendations | RS, n | R1 pre, n (%) | R1 post, n (%) | R2 pre, n (%) | R2 post, n (%) | R3 pre, n (%) | R3 post, n (%) |
| No follow up | 25 | 13 (52) | 17 (68) | 10 (40) | 19 (76) | 21 (84) | 22 (88) |
| Follow up | 5 | 3 (60) | 1 (20) | 1 (20) | 3 (60) | 3 (60) | 3 (60) |
| FNA | 20 | 17 (85) | 15 (75) | 18 (90) | 17 (85) | 11 (55) | 13 (65) |
Finally, the relative diagnostic performance of readers, pre- and post-training, when compared against the reference standard is included in Table 5 and Table 6, respectively. Pre-training pooled sensitivities ranged from 22.3%-66.7% and pooled specificity ranged from 72.2%-95.1%, dependent on TI-RADS category. Post-training pooled sensitivities ranged from 40.7%-63% and pooled specificity ranged from 76.6%-96.8%, dependent on TI-RADS category.
| Pre-training, Statistics | TI-RADS 1, % | TI-RADS 2, % | TI-RADS 3, % | TI-RADS 4, % | TI-RADS 5, % |
| Sensitivity | |||||
| R1 | 9.1 (0.2-41.3) | 33.3 (7.5-70.1) | 44.4 (13.7-78.8) | 30.8 (9.1-61.4) | 87.5 (47.4-99.7) |
| R2 | 9.1 (0.2-41.3) | 0 (0-33.6) | 11.1 (0.3-48.3) | 38.5 (13.9-68.4) | 75 (34.9-96.8) |
| R3 | 90.9 (58.7-99.8) | 33.3 (7.5-70.1) | 44.4 (13.7-78.8) | 38.5 (13.9-68.4) | 37.5 (8.5-75.5) |
| Pooled | 36.4 (20.4-54.9) | 22.2 (8.6-42.3) | 33.3 (16.5-54) | 35.9 (21.2-52.8) | 66.7 (44.7-84.4) |
| Specificity | |||||
| R1 | 100 (91.0-100) | 90.2 (76.9-97.3) | 92.7 (80.1-98.5) | 62.2 (44.8-77.5) | 76.2 (60.6-88) |
| R2 | 100 (91-100) | 97.6 (87.1-99.9) | 80.5 (65.1-91.2) | 81.1 (64.8-92) | 50 (34.2-65.8) |
| R3 | 66.7 (49.8-80.9) | 97.6 (87.1-99.9) | 95.1 (83.5-99.4) | 89.2 (74.6-97) | 90.5 (77.4-97.3) |
| Pooled | 88.9 (81.8-94) | 95.1 (89.7-98.2) | 89.4 (82.6-94.3) | 76.6 (67.6-84.1) | 72.2 (63.5-79.8) |
| Positive predictive value | |||||
| R1 | 100 | 42.9 (16.8-73.6) | 57.1 (26.4-83.2) | 22.2 (10.3-41.6) | 41.2 (27.7-56.1) |
| R2 | 100 | 0 | 11.1 (1.8-46.8) | 41.7 (21.5-65.1) | 22.2 (14.8-32.1) |
| R3 | 43.5 (32.2-55.5) | 75 (26-96.2) | 66.7 (30.1-90.3) | 55.6 (28.3-79.8) | 42.9 (17.1-73.2) |
| Pooled | 48 (31.8-64.6) | 50 (25.9-74.1) | 40.9 (24.8-59.2) | 35 (23.9-48) | 31.4 (23.5-40.5) |
| Negative predictive value | |||||
| R1 | 79.6 (76.4-82.5) | 86.1 (79.4-90.8) | 88.4 (80.8-93.2) | 71.9 (62.2-79.9) | 97 (83.5-99.5) |
| R2 | 79.6 (76.4-82.5) | 81.6 (80.9-82.4) | 80.5 (75.8-84.5) | 79 (70.4-85.6) | 91.3 (75.3-97.3) |
| R3 | 96.3 (79.8-99.4) | 87 (80.7-91.4) | 88.6 (81.2-93.4) | 80.5 (72.6-86.5) | 88.4 (81.5-92.9) |
| Pooled | 83.2 (79.2-86.6) | 84.8 (81.9-87.3) | 85.9 (82.3-88.9) | 77.3 (72.5-81.5) | 91.9 (86.5-95.3) |
| Post-training, Statistics | TI-RADS 1, % | TI-RADS 2, % | TI-RADS 3, % | TI-RADS 4, % | TI-RADS 5, % |
| Sensitivity | |||||
| R1 | 45.5 (16.8-76.6) | 44.4 (13.7-78.8) | 55.6 (21.2-86.3) | 38.5 (13.9-68.4) | 50 (15.7-84.3) |
| R2 | 63.6 (30.8-89.1) | 44.4 (13.7-78.8) | 66.7 (29.9-92.5) | 69.2 (38.6-90.9) | 62.5 (24.5-91.5) |
| R3 | 72.7 (39-94) | 33.3 (7.5-70.1) | 66.7 (29.9-92.5) | 38.5 (13.9-68.4) | 37.5 (8.5-75.5) |
| Pooled | 60.6 (42.1-77.1) | 40.7 (22.4-61.2) | 63 (42.4-80.6) | 48.7 (32.4-65.2) | 50 (29.1-70.9) |
| Specificity | |||||
| R1 | 92.3 (79.1-98.4) | 97.6 (87.1-99.9) | 90.2 (76.9-97.3) | 70.3 (53-84.1) | 81 (65.9-91.4) |
| R2 | 94.9 (82.7-99.4) | 97.6 (87.1-99.9) | 95.1 (83.5-99.4) | 73 (38.6-90.9) | 90.5 (77.4-97.3) |
| R3 | 66.7 (49.8-80.9) | 95.1 (83.5-99.4) | 97.6 (87.1-99.9) | 86.5 (71.2-95.5) | 90.5 (77.4-97.3) |
| Pooled | 84.6 (76.8-90.6) | 96.8 (91.9-99.1) | 94.3 (88.6-97.7) | 76.6 (67.6-84.1) | 87.3 (80.2-92.6) |
| Positive predictive value | |||||
| R1 | 62.5 (32-85.5) | 80 (33.6-96.9) | 55.6 (29.4-79) | 31.3 (16.3-51.5) | 33.3 (16.5-56) |
| R2 | 77.8 (45.8-93.6) | 80 (33.6-96.9) | 75 (41.8-92.6) | 47.4 (32.2-63.1) | 55.6 (29.9-78.6) |
| R3 | 38.1 (25.8-52.2) | 60 (22.6-88.5) | 85.7 (45.1-97.8) | 50 (25.6-74.4) | 42.9 (17.1-73.2) |
| Pooled | 52.6 (40.1-64.8) | 73.3 (48.6-88.9) | 70.8 (52.8-84.1) | 42.2 (31.5-53.8) | 42.9 (29-57.9) |
| Negative predictive value | |||||
| R1 | 85.7 (77.6-91.2) | 88.9 (81.7-93.5) | 90.2 (81.6-95.1) | 76.5 (66.8-84) | 89.5 (80.7-94.5) |
| R2 | 90.2 (80.8-95.3) | 88.9 (81.7-93.5) | 92.9 (83.7-97) | 87.1 (74.5-94) | 92.7 (83.7-96.9) |
| R3 | 89.7 (76.3-95.9) | 86.7 (80.3-91.2) | 93 (84.1-97.1) | 80 (71.9-86.2) | 88.4 (81.5-92.9) |
| Pooled | 88.4 (83.2-92.1) | 88.2 (84.5-91.1) | 92.1 (87.6-95) | 81 (75.5-85.4) | 90.2 (85.9-93.2) |
The overall inter-reader agreement for ACR TI-RADS should take into account the inter-reader agreement of its two major outcome variables – 'TI-RADS level' and 'ACR TI-RADS recommendations'. In our study, the inter-reader agreement for ‘TI-RADS level’ showed a significant improvement with training (k = 0.14 (slight) on the pre-training assessment vs k = 0.36 (fair) on the post-training assessment)[12]. Our inter-reader agreement for ‘ACR TI-RADS recommendations’ also showed a significant improvement with training (k = 0.36 (fair) on the pre-training assessment vs k = 0.50 (moderate) on the post-training assessment [P = 0.02]). Our findings suggest that even a single didactic training session can significantly improve the overall inter-reader agreement in radiology residents. Our findings compare favorably with other inter-reader agreement studies involving ACR TI-RADS. A study by Hoang et al[7] involving 8 board certified radiologists (2 from academic centers with subspecialty training in US and 6 from private practice with no subspecialty training in US) found a fair (k = 0.35) inter-reader agreement for ‘TI-RADS level’, and moderate (k = 051) inter-reader agreement for ‘ACR TI-RADS recommendations’[7]. Teng et al[8] assessed the lear
Our study also evaluated the inter-reader agreement of individual sonographic features including composition, echogenicity, shape, margins, and echogenic foci. Our findings showed a significant improvement in inter-reader agreement with training for features such as ‘shape’ (k = 0.09, slight pre-training versus k = 0.67, substantial post-training, P < 0.001) and ‘echogenic foci’ (k = 0.28, fair pre-training versus k = 0.45, moderate post-training, P = 0.004) but not for the others. The features with the strongest inter-reader agreement in our study were ‘shape’ (k = 0.67 post-training, substantial) and ‘composition’ (k = 0.52 post-training, moderate). Hoang et al[7] also found similar findings in their study with ‘shape’ (k = 0.61, substantial) and ‘composition’ (k = 0.58, moderate) having the strongest inter-reader agreement amongst the 5 principal sonographic features. The feature with the poorest inter-reader agreement in our study was margins (k = 0.05 post-training, slight). Similarly, Hoang et al [7] also found that ‘margins’ had the poorest inter-reader agreement (k = 0.25, fair) in their study. The poor inter-reader agreement for ‘margins’ is not surprising as accurate assessment requires a thorough review of the entire cine clip, rather than review of the still images only. Margins may also be harder to interpret through ultrasound artifacts. Finally, two of the available answer options for ‘margins’ in ACR TI-RADS are ‘ill defined’ (TI-RADS + 0 points) and ‘irregular’ (TI-RADS + 2 points). However, both options share innate conceptual similarities in interpretation and can lead to overlap. The poorest and strongest inter-reader agreement were also matched with the same features identified by Hoang’s board-certified radiologists, indicating that the limitation may be inherent to the reporting and data system rather than trainee experience.
We also evaluated the relative sensitivity and specificity of the radiology residents in assigning TI-RADS levels compared to consensus reference standard before and after training. There was a general trend towards improved pooled sensitivity with TI-RADS levels 1 to 4 for the post-training assessment while the pooled specificity was relatively high (76.6-96.8%) for all TI-RADS level. Overall findings suggest that a single didactic training session improves the detection of benign (TI-RADS 1-3) lesions while retaining high specificity in radiology residents. Improved identification of benign lesions is critical in avoiding unnecessary biopsies and interventions, a major aim of the ACR TI-RADS system.
The current study has several limitations. One limitation is the lack of a pathological reference standard. The reference standard was an expert consensus review by 3 board certified radiologists with Body Imaging fellowship and 1-14 years of clinical experience. However, it should be noted that this study is designed primarily to evaluate inter-reader reliability of radiology residents, and not the inherent performance of the ACR TI-RADS itself. As such, an expert consensus panel was deemed a practical reference standard, and one that simulates ‘real world’ clinical practice[9]. Another limitation is the relatively small number of cases used. However, even with this limited number of cases, we were able to show statistically significant improvements in inter-reader agreement for the two major outcome variables (TI-RADS level and ACR TI-RADS recommendations). While there is a relatively even distribution of TI-RADS levels among the test cases via non-random selection, there is uneven distribution of individual ultrasound features within the group. Of the 50 test cases, only 3 nodules demonstrated ‘lobulated or irregular’ margins (TI-RADS points +2), while the remaining 47 are ‘smooth’ or ‘ill-defined’ (TI-RADS points +0). A larger sample size can improve this and lead to more representative analysis of individual ultrasound features. Finally, training retention over time was not evaluated in this study, with the post-training testing performed two weeks after didactic and training case review.
Overall, the current study demonstrates a statistically significant improvement in inter-reader agreement among radiology residents, with no prior ACR TI-RADS experience, in the assignment of TI-RADS level and recommendations after a single didactic teaching session compared to expert consensus. Our study demonstrates the learnability of the ACR TI-RADS system and supports the use of dedicated training in radiology residents. Future studies can also be directed to evaluate the effect of additional training sessions with focus on areas/features demonstrating lower inter-rater agreement such as “margins” and retention of training over time.
Thyroid nodules are common and often incidental. The American College of Radiology Thyroid Imaging Reporting and Data System (ACR TI-RADS) standardizes the use of ultrasound for thyroid nodule risk stratification.
Despite the widespread usage of this system, the learnability of TI-RADS has not been proven in radiology trainees.
To evaluate the inter-reader reliability amongst radiology trainees before and after TI-RADS training.
Three PGY-4 radiology residents were evaluated for inter-reader reliability with a 50 thyroid nodule data set before and after a 1-hour didactic teaching session and review of a training data set, with assessment performed 6 wk apart. Performance was compared to a consensus panel reference standard of three fellowship trained radiologists.
After one session of dedicated TI-RADS training, the radiology residents demonstrated statistically significant improvement in inter-reader agreement in subcategories of "shape", "echogenic foci", "TI-RADS level", and "recommendations" when compared with expert panel consensus. A trend towards higher pooled sensitivity for TI-RADS level 1-4 is also observed.
Resident trainees demonstrated a statistically significant improvement in inter-reader agreement for both TI-RADS level and recommendations after training. This study demonstrates the learnability of the ACR TI-RADS.
A multi-institutional and multi-national assessment of radiology resident diagnostic accuracy and inter-reader reliability of ACR TI-RADS classification and recommendations before and after training would improve the generalizability of these results.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: The Royal College of Physicians and Surgeons of Canada, 2544834.
Specialty type: Radiology, nuclear medicine and medical imaging
Country/Territory of origin: Canada
Peer-review report’s scientific quality classification
Grade A (Excellent): A, A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Beck-Razi N, Lee KS, Naganuma H S-Editor: Wang LL L-Editor: A P-Editor: Wang LL
| 1. | Gharib H, Papini E, Garber JR, Duick DS, Harrell RM, Hegedüs L, Paschke R, Valcavi R, Vitti P; AACE/ACE/AME Task Force on Thyroid Nodules. American association of clinical endocrinologists, american college of endocrinology, and associazione medici endocrinologi medical guidelines for clinical practice for the diagnosis and management of thyroid nodules--2016 update. Endocr Pract. 2016;22:622-639. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 564] [Cited by in RCA: 746] [Article Influence: 82.9] [Reference Citation Analysis (0)] |
| 2. | Grani G, Lamartina L, Cantisani V, Maranghi M, Lucia P, Durante C. Interobserver agreement of various thyroid imaging reporting and data systems. Endocr Connect. 2018;7:1-7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 126] [Cited by in RCA: 149] [Article Influence: 21.3] [Reference Citation Analysis (0)] |
| 3. | Smith-Bindman R, Lebda P, Feldstein VA, Sellami D, Goldstein RB, Brasic N, Jin C, Kornak J. Risk of thyroid cancer based on thyroid ultrasound imaging characteristics: results of a population-based study. JAMA Intern Med. 2013;173:1788-1796. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 179] [Cited by in RCA: 193] [Article Influence: 16.1] [Reference Citation Analysis (0)] |
| 4. | Lim H, Devesa SS, Sosa JA, Check D, Kitahara CM. Trends in Thyroid Cancer Incidence and Mortality in the United States, 1974-2013. JAMA. 2017;317:1338-1348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1080] [Cited by in RCA: 1514] [Article Influence: 189.3] [Reference Citation Analysis (0)] |
| 5. | Tessler FN, Middleton WD, Grant EG, Hoang JK, Berland LL, Teefey SA, Cronan JJ, Beland MD, Desser TS, Frates MC, Hammers LW, Hamper UM, Langer JE, Reading CC, Scoutt LM, Stavros AT. ACR Thyroid Imaging, Reporting and Data System (TI-RADS): White Paper of the ACR TI-RADS Committee. J Am Coll Radiol. 2017;14:587-595. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 900] [Cited by in RCA: 1379] [Article Influence: 172.4] [Reference Citation Analysis (0)] |
| 6. | Ha EJ, Na DG, Baek JH, Sung JY, Kim JH, Kang SY. US Fine-Needle Aspiration Biopsy for Thyroid Malignancy: Diagnostic Performance of Seven Society Guidelines Applied to 2000 Thyroid Nodules. Radiology. 2018;287:893-900. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 114] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 7. | Hoang JK, Middleton WD, Farjat AE, Teefey SA, Abinanti N, Boschini FJ, Bronner AJ, Dahiya N, Hertzberg BS, Newman JR, Scanga D, Vogler RC, Tessler FN. Interobserver Variability of Sonographic Features Used in the American College of Radiology Thyroid Imaging Reporting and Data System. AJR Am J Roentgenol. 2018;211:162-167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 121] [Article Influence: 17.3] [Reference Citation Analysis (0)] |
| 8. | Teng D, Fu P, Li W, Guo F, Wang H. Learnability and reproducibility of ACR Thyroid Imaging, Reporting and Data System (TI-RADS) in postgraduate freshmen. Endocrine. 2020;67:643-650. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 9. | Pi Y, Wilson MP, Katlariwala P, Sam M, Ackerman T, Paskar L, Patel V, Low G. Diagnostic accuracy and inter-observer reliability of the O-RADS scoring system among staff radiologists in a North American academic clinical setting. Abdom Radiol (NY). 2021;46:4967-4973. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 23] [Article Influence: 5.8] [Reference Citation Analysis (1)] |
| 10. | McHugh ML. Interrater reliability: the kappa statistic. Biochem Med (Zagreb). 2012;22:276-282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6526] [Cited by in RCA: 8803] [Article Influence: 677.2] [Reference Citation Analysis (0)] |
| 11. | Gwet KL. Testing the Difference of Correlated Agreement Coefficients for Statistical Significance. Educ Psychol Meas. 2016;76:609-637. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 80] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 12. | Li W, Wang Y, Wen J, Zhang L, Sun Y. Diagnostic Performance of American College of Radiology TI-RADS: A Systematic Review and Meta-Analysis. AJR Am J Roentgenol. 2021;216:38-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 46] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 13. | Chung R, Rosenkrantz AB, Bennett GL, Dane B, Jacobs JE, Slywotzky C, Smereka PN, Tong A, Sheth S. Interreader Concordance of the TI-RADS: Impact of Radiologist Experience. AJR Am J Roentgenol. 2020;214:1152-1157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 14. | Seifert P, Görges R, Zimny M, Kreissl MC, Schenke S. Interobserver agreement and efficacy of consensus reading in Kwak-, EU-, and ACR-thyroid imaging recording and data systems and ATA guidelines for the ultrasound risk stratification of thyroid nodules. Endocrine. 2020;67:143-154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 34] [Article Influence: 6.8] [Reference Citation Analysis (0)] |