Published online May 28, 2021. doi: 10.4329/wjr.v13.i5.102
Peer-review started: January 10, 2021
First decision: April 6, 2021
Revised: April 10, 2021
Accepted: May 10, 2021
Article in press: May 10, 2021
Published online: May 28, 2021
Processing time: 138 Days and 2.4 Hours
In coronavirus disease 2019 (COVID-19), medical imaging plays an essential role in the diagnosis, management and disease progression surveillance. Chest radiography and computed tomography are commonly used imaging techniques globally during this pandemic. As the pandemic continues to unfold, many healthcare systems worldwide struggle to balance the heavy strain due to overwhelming demand for healthcare resources. Changes are required across the entire healthcare system and medical imaging departments are no exception. The COVID-19 pandemic had a devastating impact on medical imaging practices. It is now time to pay further attention to the profound challenges of COVID-19 on medical imaging services and develop effective strategies to get ahead of the crisis. Additionally, preparation for operations and survival in the post-pandemic future are necessary considerations. This review aims to comprehensively examine the challenges and optimization of delivering medical imaging services in relation to the current COVID-19 global pandemic, including the role of medical imaging during these challenging times and potential future directions post-COVID-19.
Core Tip: In coronavirus disease 2019 (COVID-19) testing, there is a need for quick and accurate diagnosis of the disease. This has affirmed the significance of medical imaging (chest radiography and computed tomography) in the battle against COVID-19. The pandemic and the consequent mitigation measures have had a significant impact on the practices in medical imaging. Despite the large and dynamic challenge presented, patient safety and care are paramount. Necessary precautions must be instituted to ensure the safety of medical imaging professionals, patients and the public. As the pandemic continues to ravage our globe, medical imaging service providers need to exercise flexibility without compromising on patient safety.
- Citation: Tay YX, Kothan S, Kada S, Cai S, Lai CWK. Challenges and optimization strategies in medical imaging service delivery during COVID-19. World J Radiol 2021; 13(5): 102-121
- URL: https://www.wjgnet.com/1949-8470/full/v13/i5/102.htm
- DOI: https://dx.doi.org/10.4329/wjr.v13.i5.102
A cluster of unknown pneumonia cases was reported in Wuhan, Hubei Province, China on December 31, 2019. There were both similarities and differences in various aspects of this pathogen with the severe acute respiratory syndrome (SARS) that originated in China’s Guangdong Province on November 27, 2002[1]. Despite the difference in epidemiology, like SARS, it presented as a respiratory disease which was officially named and announced by the World Health Organization (WHO) as “COVID-19” (coronavirus disease 2019), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)[2]. Most patients infected with COVID-19 had pneumonia and hence medical imaging became vital in the early diagnosis and assessment of disease course[3]. Moreover, the medical imaging role in an infectious disease outbreak had been well described and was epitomized by the SARS epidemic[4]. While the use of medical imaging techniques—chest radiography and computed tomography (CT) differed across countries, there was no doubt about the significance and importance of medical imaging in this COVID-19 pandemic[3,4]. The aim of this review is to highlight the challenges and optimization strategies in medical imaging service delivery in Singapore and around the world during this COVID-19 pandemic.
Chest radiography played an important role in the diagnosis of SARS during the 2003 outbreak in Hong Kong[5,6]. Despite poor sensitivity, patients with clinical and epidemiologic suspicion of SARS were evaluated by serial chest radiography[7]. A similar practice of serial chest radiography was also adopted in Singapore (together with Hong Kong, one of the 10 countries with the most cumulated numbers of cases)[8,9]. This practice included chest radiography for patients with contact history who had developed respiratory symptoms, even if afebrile, when person-to-person transmission was evident globally[5]. In fact, this was in line with the Centres for Disease Control and Prevention (CDC) recommendation at that time[5].
With the global resurgence of person-to-person transmission in the form of COVID-19, the sense of Déjà vu was vivid. During this pandemic, despite the trajectory use of CT scan in China as a screening tool[10], most radiology societies still do not endorse routine screening CT for COVID-19 pneumonia[11,12]. Although the WHO rapid advice guide for the use of chest imaging in COVID-19[13] highlighted considerations for choice of imaging modalities, it stopped short of recommending specific imaging modalities for different categories of patients. This could be attributed to the different community norms and public health directives[14].
Chest radiography was of greater value in patients with advanced symptoms as compared to those in the early course of their disease[14,15]. For patients who were encouraged to present once symptomatic, as was the case in Wuhan, China, chest radiography had little value as it was insensitive in mild or early COVID-19 infection[14-16]. In a similar vein, Singapore also had the public health directive for citizens to consult a doctor even when they had mild respiratory symptoms[17]. However, in Singapore, chest radiography remains the primary imaging modality of choice in COVID-19 screening, with a CT scan used only as a problem-solving tool[4,18]. On the other hand, some countries such as South Korea uses reverse transcription polymerase chain reaction (RT-PCR) for initial screening instead of relying on diagnostic imaging studies[19]. Nevertheless, chest radiography is a fundamental tool in the diagnosis, management and monitoring of disease[20-22]. Moreover, chest radiography is widely available (less resource intensive), coupled with features of rapid execution, low cost and function of bedside radiography. This enables chest radiography to be an important complement to clinical and epidemiological features in the battle against COVID-19[13,22].
On the other hand, although a CT scan has relatively low specificity, it has a relatively higher sensitivity as compared to chest radiography and RT-PCR[10,13]. This is useful in patients with some pre-existing pulmonary diseases and when results of RT-PCR tests are negative[10,13,14]. While there were differing views on the first assessment medical imaging technique for COVID-19 infection, there was no doubt of the importance of medical imaging services in the battle against COVID-19. Considerations on the choice of medical imaging technique were usually dependent on local practice patterns and resource availability[14].
Nevertheless, as mentioned in the multinational consensus statement from the Fleischner Society[14] — the choice of medical imaging techniques should be based on the clinical judgement of the clinical teams while considering the attributes of the techniques, local resources and expertise. In addition, the involvement of all stakeholders — referring clinician, radiologist and patient, in the decision-making on the choice of medical imaging of COVID-19 was encouraged[13]. Similarly, whenever possible, the patient should be provided with information on the chosen medical imaging techniques and the potential of the multiple imaging requirement highlighted[13].
Maintaining a healthy and adequate workforce is crucial in any infectious disease epidemic. Moreover, with screening, monitoring and evaluation roles undertaken by radiology in this COVID-19 pandemic, managing manpower was even more important. Given that more COVID-19 patients were being admitted and enough manpower would be required to meet the demands of increased workload, ensuring functional staff for continued service should not be undermined[23].
Within a month (January 30, 2020) after the first reported confirmed case of SARS-CoV-2, there were 82 confirmed cases outside of China with the majority of cases reported in Asia[24]. The WHO subsequently released its strategic objectives for the pandemic which included early identification, isolation and care of patients, including providing optimized care for infected patients[25]. Clearly, a substantial number of staff was required in response to this new infectious disease, especially when there was unprecedented numbers of people diagnosed with COVID-19 and seeking treatment.
At the early onset of the battle against COVID-19, Singapore faced the possibility of the healthcare system being overwhelmed. The Singapore Ministry of Health responded to the threat by initiating an island-wide call for former healthcare professionals (HCPs) to support the country’s fight against the coronavirus, including doctors and allied health professionals[26]. A similar picture was seen globally, where retired doctors, nurses and medical students were mobilized to join the fight[26-30].
As the pandemic unfolded, many radiology departments experienced an increase in manpower demand due to many factors which included the increase in workload, and procedure time and the impact of team segregation[4,31,32]. A similar experience was also reported in low resource settings such as Ghana and Iran, although some regions reported a decline in general workload, in line with reports from North America and Europe, which could be attributed to low COVID-19 case intensities in these regions[33,34]. Nonetheless, it was well established that the healthcare workforce was facing high adversity and workload as more countries were impacted by the spread of COVID-19[35].
To respond to the sudden surge and new waves of COVID-19, the radiology workforce had to be redeployed or re-assigned to other imaging modalities[33,36-38]. In tandem with the call for former HCPs, there was a need to reskill and/or upskill the returning workforce to support the current workforce. Clearly, a substantial amount of time had to be invested in creating training opportunities for staff to be prepared to face the pandemic. However, that would result in hours away from the clinical environment. Indeed, it was suggested that tens of thousands of radiographer hours would be invested to develop information to help radiographers worldwide to manage the imaging of COVID-19 patients using mobile chest radiography with appropriate infection control measures[39]. Notwithstanding, there was also the potential of the massive amount of replication of information globally while attempting to address this information deficiency[39]. Moreover, departments had to grapple with understaffing at the peak of the outbreak due to HCPs infections, self-isolation due to contact with positive cases and statutory paid sick leave in many countries globally[40].
In a radiology department, radiographers may be exposed to SARS-CoV-2 during mobile radiography and chest CT procedures. As these procedures were more often performed as part of routine diagnosis, assessment and monitoring of the disease, there was an increased risk of radiographers contracting COVID-19[41]. In addition, procedures with prolonged patient contact such as ultrasound and interventional radiology expose radiology staff to an even higher risk of infection[41-44]. At the same time, radiology services are a crossroad of heterogeneous subjects within hospitals; measures had to be taken to mitigate the risk of the radiology workforce being infected to protect other HCPs, patients and the general public[41,45].
It is well established that the shortage of personal protective equipment (PPE), lack of training in infection control measures, and poor PPE usage increase the risk of patient-HCP transmission of infection[46,47]. Indeed, the provision of adequate PPE is of paramount importance and is a critical component of infection control and prevention during this pandemic. However, globally, many departments were facing a shortage of PPE[48]. In fact, multiple reports of shortages of PPE, medical supplies and COVID-19 test kits had surfaced in various countries ranging from developing countries in Southeast Asia to developed countries like the United States[49,50]. This was worrying as previous lessons from other infectious disease outbreaks had identified PPE as a crucial element in reducing infections and deaths of HCPs[47]. During this pandemic, SARS-CoV-2 infection among HCPs was not unheard-of. China and Italy both reported infections and deaths of HCPs[50,51], while United States[52], Spain[46] and Qatar[53] all reported COVID-19 infection among its HCPs. This could lead to a decline in the healthcare workforce, resulting in unstable healthcare infrastructure, thus reducing the quality and quantity of care available while increasing the workload on remaining staff[47,54].
Although ensuring that HCPs are well protected is crucial in reducing viral transmission and sustaining health system capacity[47], equipment used in the radiology department is also a potential vector for transmission of the virus. Identified equipment include ultrasound units, non-portable modalities, such as CT or magnetic resonance imaging (MRI) and mobile radiography units[31,41,43,55,56]. The immerse challenge for infection control in the CT suite was epitomized in China where CT was often the first-line investigation for COVID-19[15]. The equipment had to be disinfected after exposure according to recommended guidelines by the vendors or institutions. Similarly, accessories such as keyboards, mice, viewing stations and blood pressure cuffs had to be disinfected accurately with appropriate and safe disinfectant[57,58]. Clearly, all potentially contaminated surfaces had to be disinfected to reduce the risk of virus transmission.
Provision of medical imaging services to many patients suspected of having or confirmed to have COVID-19 during the pandemic was a herculean task. The procedure duration was lengthened and complicated by strict infection control measures to mitigate infection risk in the radiology department[14,41,59]. This was highlighted by the American College of Radiology (ACR)[60] where it noted that CT decontamination after scanning COVID-19 patients might disrupt radiologic service availability. Studies sharing recommendations for infection control in the CT suite were widely available. However, it also demonstrated the substantial time and resources needed during, pre- and post-CT scans, which was highlighted by the ACR[57,61,62]. While hospitals with more than one scanner could dedicate one scanner for scanning COVID-19 patients, it could not be instituted in all hospitals[63,64]. Therefore, in this pandemic, in some countries, CT cannot be superseded by chest radiography due to limited scanners[15].
To mitigate the limitation, coupled with long turnaround times for RT-PCR, countries such as Italy and United Kingdom had adopted chest radiography as a first-line triage tool[15]. This could also be attributed to the favourable feature of a mobile unit — portability, where chest radiography could be performed at the bedside instead of transporting the patient to the scanner[14]. This effectively reduced patient transfer and minimized the risk of cross-infection to others[13,55]. Given the obvious benefit of mobile chest radiography, the uptake and demand of chest radiography as a first-line assessment tool would increase over time. This posed a challenge to even a large hospital — where Singapore’s largest acute tertiary referral medical centre had to acquire additional mobile units to meet the increasing clinical demands[55]. A similar challenge was also noted in South-East Queensland, Australia where purchase, rapid acquisition and deployment of additional mobile units were initiated[65].
However, with the urgent delivery and growing orders for mobile units, some vendors could not meet the urgent delivery timeframe[66]. Against this backdrop, many hospitals in England were struggling with equipment shortage and backlog[67]. Many were in urgent need of more staff and imaging equipment — CT, MRI, ultrasound and mobile units, to deal with backlog cases. It was particularly vivid in the United Kingdom where it was reported to have the lowest number of scanners when compared with other Organization for Economic Co-operation and Development countries[67]. This resulted in a significant block capacity gap within the United Kingdom, prompting The Royal College of Radiologists (RCR) to describe the situation as a perfect storm in terms of delivering capacity[67].
Faced with the challenge of limited delivering capacity and mounting wait lists, patient access to medical imaging services was profoundly affected. This was evident in Canada where waiting time for medical imaging is now twice as long when compared with pre-COVID times — significantly beyond the acceptable standards[68]. A similar picture was painted in the UK where statistics had highlighted the knock-on impact of pausing non-emergency imaging during the peak of COVID-19 infection — a substantial increase in waiting time for CT or MRI scans[69]. In particular, the RCR[69] warned of a continuum of such figures if without more sustained investment.
In the battle against COVID-19, the most important and valuable assets were HCPs[70]. However, a recent systematic review[71] highlighted that many HCPs faced aggravated psychological pressure and even mental illness. The intensive work drained the HCPs physically and emotionally[72]. This was especially vivid for the HCPs who had neither infectious disease expertise nor experienced the SARS outbreak[72,73]. They had to adjust to a new working environment in this extraordinarily stressful situation. Low resource countries such as Nepal, had considerable mental health symptoms among HCPs[74]. In fact, Iraqi communities who are already afflicted by the ongoing conflict, political instability and social upheavals now face an even more challenging task to secure the mental well-being of their HCPs[75].
It was reported that frontline HCPs like radiographers, who often had to take on the role of caring directly for patients with COVID-19 were at a higher-level risk of having severe mental health symptoms than those in secondary roles[76]. They had to work with the constant changing protocols with some reported to have inadvertent exposure to COVID-19 positive patients without suitable PPE — a result of poor communication[77]. Moreover, some radiographers experienced burnout as they were subjected to 12-hour shifts in order to meet the service needs and for team segregation[78]. This was in line with the systematic review which identified long working hours as a factor for increased risk of various psychological and mental illness as well as physical and emotional distress[71].
Similarly, radiologists were vulnerable to experiencing burnout with the increased emphasis on reporting speed and studies per day, long working hours, and limited personal interaction[79]. Coupled with the pre-COVID reasons for increased rates of burnout in radiology, all these stressors were being magnified exponentially during this COVID-19 pandemic[80]. As mentioned by Wolfman et al[80], the medical imaging profession is now facing an untenable situation where “COVID had turned a smouldering ember into a blazing fire”.
Undeniably, both radiographers and radiologists were at risk of burnout. In addition, they were also at risk of fatigue[81]. This had concerning implications as it resulted in a negative outcome in terms of patient safety in medical imaging. This could not be emphasized further with burnout and fatigue being highlighted in the joint paper[82] released by the European Society of Radiology and the European Federation of Radiographer Societies on patient safety in medical imaging. Indeed, ensuring the physical and psychological well-being of the professionals is crucial for safe delivery of medical imaging. A summary of the challenges in the provision of medical imaging service during COVID-19 is shown in Table 1.
| Challenge | Experiences of medical imaging departments |
| Coping with limited manpower | Team segregation; Increased workload; Increased responsibility; Increased procedure time due to infection control measures and terminal cleaning of equipment; Self-isolation due to contact with positive cases; Statutory paid sick leave |
| Coping with strict infection control measures | Shortage of PPE; Increased risk of exposure from prolonged patient contact; Resource and labour intensive due to terminal cleaning of equipment |
| Coping with limited resources | Equipment segregation; Inadequate mobile radiography units; Delay in delivery of equipment due to increased orders; overseas shipment of equipment delayed; Poor imaging service delivery due to a lack of imaging equipment |
| Safeguarding of medical imaging professionals’ well-being | Aggravated psychological pressure and mental illness; Physical and emotional distress among medical imaging professionals; Burnout; Fatigue |
During this pandemic, timely decisions need to be made and strategies promptly executed to mitigate the risk of widespread transmission. As the pandemic unfolds, the continuity of an effective medical imaging service for both COVID-19 and non-COVID-19 patients is essential. Notably, radiology departments must now adhere to the strictest infection control practices, different countries’ varying healthcare and lock down policies and continue to value add to patient care amidst this unprecedented challenge.
During this period of COVID-19, strong clinical and compassionate leadership is paramount in improving the provision of quality care[83]. Similarly, Shingler-Nace[84] identified: Staying calm, communication, collaboration, coordination and providing support, as the five elements to successful leadership during this pandemic. Undeniably, this pandemic has caused a global turmoil in many aspects in our way of life and continues to challenge established leadership models[85].
Fortunately, there was a substantial amount of materials to guide radiology leaders as the profession navigates through unchartered waters[86,87]. Moreover, leadership lessons from prior pandemics were invaluable and augmented the available resources in this COVID-19 pandemic[88]. Radiology leaders demonstrated good leadership qualities in the face of adversity[89-91]. Comparably, radiographers had also shown their ability to contribute as highly effective COVID-19 leaders in safely and sustainably reorganizing radiography services[55].
There was no doubt that adaptability, flexibility, teamwork, clear communication, patient and staff safety as well as staff well-being were key principles for managing leadership teams in this pandemic[89-93]. While many would agree upon the key principles emphasized, Dr Gerada[94] highlighted in her presentation delivered at the prestigious Sir Godfrey Hounsfield Lecture, that a successful leader in the COVID-19 is one who offers hope yet bounded by realism. Clearly, one should not forget about instilling hope in times of crisis.
With chest radiography preferred in many countries to screen and monitor the progression of COVID-19, mobile units were in high demand. By using mobile digital radiography (DR) units instead of conventional radiography (CR) units, mobile DR solutions were a key element in turning the tide in COVID-19 management. Mobile DR units had the advantages of delivering high quality DR images in real time and had the feature of wireless data transmission which enabled early reporting and access by clinicians[55,95]. Moreover, some DR mobile units had added features to help reduce contamination, mitigating the risk of cross-infection[96]. The use of the DR mobile unit was supported and endorsed by the ACR task force on COVID-19 where it was highlighted that the surfaces of the unit could be cleaned with ease and therefore well suited for use in ambulatory care facilities[97]. In fact, recognizing the mobile DR units’ advantages, hospitals in Brazil and Namibia have since adopted a retrofit solution to their mobile CR units to meet the increasing demands[98,99].
Reducing contamination was not only a key feature in mobile DR units. CT systems were also embracing such a norm. In China where CT scans were in high demand, artificial intelligence (AI) was empowering automated patient positioning and scanning from the control console room[100]. Such an approach reduces cross infection between the radiographers and patients. Other uses of technology can be appreciated in the form of leveraging medical imaging data — remote diagnosis, data-driven management of COVID-19 operations, mounting imaging backlog and a foundation for ongoing monitoring and research on COVID-19[100,101]. Lastly, the use of AI to provide COVID-19 specific education, screening, triage and home monitoring can also help to reduce unnecessary demand on medical imaging services by supporting and providing guidance to all patients[102].
As the pandemic continues to spread globally, clear communication with radiographers is necessary to ensure infection control[103]. If radiographers are communicated promptly regarding the health of the patient to be scanned, appropriate PPE can be worn in advance — avoiding repetition of miscommunication incidents that led to radiographers in Ireland[77] being exposed to COVID-19 positive patients without donning appropriate PPE. Moreover, such clear communication is crucial in ensuring that radiographers comply and perform self-monitoring for symptoms when exposed to positive cases[101]. This can be in the form of daily routine instructions, newsletters, open forums and one-on-one communications[103,104]. Similarly, other forms of communique such as websites, virtual telecommuting and team-based communication can be utilized to ensure timely updates of current guidance and policies[105].
Clear and frequent communication amongst all members of the healthcare team has been of utmost importance throughout the pandemic[105]. This was especially crucial in the communication of imaging examination findings. In addition, rapid and prompt communication of results is also essential for staff safety and management of the patient[103]. This was highlighted by the radiology experts from Norway and Germany[106] who accentuated the role of structured reporting in communicating clear results to the rest of the team. In fact, the importance of structured reporting could not be emphasized enough with structured reporting templates that were endorsed by the Society of Thoracic Radiology, the ACR and The Radiological Society of North America being made available[107]. Such reporting language and a template for chest radiography have also since surfaced[108,109].
To prepare for any sudden patient surge and to minimize potential staff or patient exposure, many elective/non-urgent imaging procedures were postponed[110]. This was implemented with the consideration of prioritizing urgent and emergency visits while preserving PPE as the COVID-19 pandemic escalated[111]. Both the ACR[111] and RCR[112] released an advisory in the support of postponing non-urgent outpatients’ visits such as elective radiology-related procedures, cancer screenings and mammography. The postponement of breast imaging related screening was also supported by various societies[113,114]. Likewise, many non-high priority nuclear medicine procedures were also rescheduled[115]. In tandem, radiologists were tasked to review and prioritize all scheduled outpatients on the necessity of imaging at that juncture[111]. It was clear that such a decision was made deliberately with the safety of patients and staff as the utmost priority.
Patients who were scheduled for imaging procedures during this period had to be triaged before they could enter the radiology department. In Sichuan, China, a three-level triage was introduced to categorize patients according to the different risk levels[116]. Other triaging approaches were also reported such as an external triage unit in Switzerland[117] and a pre-access telephone triage in Italy[118]. These were supported by evidence from China[119,120] which suggested that the procedure of triaging patients effectively screened patients and identified any high-risk populations. The importance of establishing a triage area was well established with the WHO regional office for Africa releasing a document[121] to provide guidance on how to rapidly establish a triage area at a healthcare facility.
As part of safe/physical distancing, radiology departments in Singapore adopted temporal and physical segregation policies to reduce the risk of cross-infection to staff and other patients and to maintain staff capabilities to meet the demand of medical imaging services[31]. For similar purposes, radiographers were segregated to different teams based on clinical location with the roster pattern fixed and synchronized with the nurses’ and radiologists’ rosters to facilitate contact tracing[55]. A similar approach was also adopted in China with success as institutions in Singapore and China reported no COVID-19 positive cases in their radiographers[55,122].
Like many hospitals globally, at the initial phase of the outbreak, many medical and radiography students were immediately withdrawn from the clinical setting or had their clinical rotations suspended for their protection[122-124]. Other work processes such as isolation mobile radiography workflow[55] and dedicated workflow management processes for modalities that required high staff numbers[125] were modified to adapt and optimize imaging services to meet the current clinical needs. Similarly, technical operations such as the undertaking of mobile radiography through side room windows[126], and the radiologist’s responsibility were also included in the review with the primary aim of optimizing the radiology protocol during the pandemic[116].
The safety of HCP is paramount during a pandemic. Strict cleaning and disinfection procedures were in place to mitigate the risk of infection. Practical alternatives are needed to augment current practices especially when new waves of outbreak surface globally. This includes introduction of an imaging booth (SG SAFE.R) for chest radiography where the patient can have a chest X-ray done without contact with the radiographer—reducing the need for additional manpower while improving safety[127]. A similar booth set up (Radiology Annex) was also reported by Penn State Health which commented that such an X-ray booth offered quick scans to COVID-19 patients while eliminating the time needed to wipe down the equipment and exchange the air[128].
Radiological equipment used for scanning of COVID-19 patients should be reorganized as part of the segregation of patients to reduce the risk of cross-infection and continuum of routine radiology services[122]. Many hospitals in Singapore and China assigned dedicated equipment exclusively for suspected and confirmed cases of COVID-19[4,122]. This practice was advocated by many authors and societies [58,129-131]. In addition, a dedicated transport team, low traffic access routes, lift lobbies, dedicated waiting area and scanners with negative-pressure capability were established and used[4,122,129,132]. Hospitals constrained by the availability of equipment can navigate this challenge by assigning dedicated time for COVID-19 cases[122]. Moreover, such scanning can be scheduled only towards the end of the work-day[4]. This not only reduces the risk of cross-contamination but also increases work efficiency and room utilization considering the substantial time required for cleaning the scan room[4,116]. Most importantly, terminal cleaning needs to be performed by a specialized team[4,132].
With mobile radiography and CT scans in high demand during the COVID-19 pandemic, the radiology department risks being a site of potential spread[132]. Therefore, it is paramount to ensure utmost safety of radiology staff and to reduce staff and patient transmission. Mobile units require to be disinfected according to a fixed cleaning regime which might include the subsequent process of exposing the unit to ultraviolet light for more than 30 min before being used on the next patient[132,133]. Other examples of protocol included having the mobile units and X-ray cassettes covered with layers of polythene sheet sealed with adhesive tapes or leucoplast[134] and wrapping of mobile DR flat detectors with disposable sheets[135]. Such protocols have since been established beyond mobile radiography and CT to include ultrasound, MRI and interventional radiology[132,136-139]. A summary of the strategies to optimize medical imaging service delivery during COVID-19 is shown in Table 2.
| Theme | Strategies |
| The need for strong and compassionate leadership | Staying calm, communication, collaboration, coordination and providing support; Practising adaptability, flexibility, and teamwork; Ensuring the safety of patients and staff; Safeguarding the well-being of staff; Instilling hope in times of crisis |
| Embracing technological usage | Adopting mobile DR units in the department; Adopting AI to reduce contamination of equipment; Harnessing capability of AI in: (1) Remote diagnosis; (2) Data-driven management of COVID-19 operations; (3) Mounting imaging backlog; (4) Ongoing monitoring and research on COVID-19; and (5) Supporting and provision of guidance to patients |
| Clear communication | Communication among staff through: (1) Routine instructions; (2) Newsletters; (3) Open forum; and (4) One-to-one communications. Timely updates and dissemination of current guidance and policies through: (1) Websites; (2) Virtual telecommuting; and (3) Team-based communication. Structured reporting in communicating imaging results |
| Enhancing processes, protocol, and policies | Postponement of elective/non-urgent imaging procedures; Review and prioritisation of outpatient schedules by radiologists; Triaging of patients prior to entering the radiology department; Temporal and physical segregation; Suspension of students’ placement; Dedicated workflow management process; Development of isolation mobile radiography workflow; Involvement of medical imaging professionals in technical operations; Reorganisation of radiological equipment and assigning of dedicated equipment for suspect and confirmed cases; Implementation of dedicated transport team, routes, lift lobbies and waiting area for COVID-19 patients; End of day schedules for COVID-19 patients |
| Innovation | Developing new solutions to minimise patient contact |
In this pandemic, there is no doubt regarding the critical role played by HCPs in the national and local responses. It is crucial to ensure that HCPs are “pandemic ready” as most of the actions required to prepare for the COVID-19 pandemic can be applied or adapted to the management of other emergencies or crises[140]. Such pandemic guidance which included recommendations were released by WHO and various public health agencies globally for more than 15 years[141]. They were likely prompted by 2 major healthcare events—H5N1 avian influenza outbreak in 2002-2005 and SARS in 2003[141]. According to WHO[140], preparedness tasks for HCPs include the development and implementation of training programmes that are based on the staff roles in an emergency, and to develop protocols to provide staff with training in an emergency and provide staff with social and psychological support. Clearly, mechanisms and systems must be in place before the pandemic to ensure that radiology staff are pandemic prepared.
To prepare HCPs for and respond to such events, it is advocated by the WHO to ensure appropriate and quality training and education are in place for all staff. Various authors have responded with remarkable vigour in sharing the approaches to prepare radiology staff for a pandemic. They included curated on-boarding programmes[142], film discussion sessions[143], use of a skill-set inventory[144], and introducing hospital arranged tutorials and video awareness campaigns[145]. It is essential to ensure that radiology staff who were battling the pandemic had the knowledge and skills needed to provide the best care for the patients while maintaining safety. In tandem, resources should be readily available to safeguard the mental health and wellbeing of radiology staff during the pandemic[144,146].
The COVID-19 pandemic had also highlighted the importance of academic institutions in raising the pandemic readiness of students. Rainford et al[147] identified that radiography students might not be fully confident in using PPE and suggested that practical training sessions be conducted before their placement—an approach that a Singapore academic institution adopted[123]. New norms of teaching HCPs have also been suggested by many authors ranging from virtual teaching[148,149], adoption of technology-based platforms[150,151], simulation and virtual reality[152,153]. Similar to qualified HCPs, medical students who are recruited to assist in a pandemic need to undergo specific training programmes. Such student disaster training programmes improve the students’ readiness, knowledge and skills which can play a valuable role in pandemic management[154].
Compared to SARS, COVID-19 has had a significant impact on the way education is being delivered. Lessons from SARS have resulted in academic institutions establishing and increasing their online presence through effective learning management systems, video conference facilities and facilitators’ experience in e-learning[155]. During this COVID-19 pandemic, many academic institutions successfully switched to online learning with just a few days of preparation[155,156]. Clearly, post-SARS, there was an increased digital trajectory in the provision of education. However, this pandemic has demonstrated that online education is still not universally embraced in countries such as Argentina, Zimbabwe and Malaysia[155]. It is now incumbent upon all educators to explore online learning technology’s full potential as this pandemic can be an inflection point for further acceleration. Likewise, educators should also ensure that there is adequate training, bandwidth, and preparation for online education where it is believed to have become an integral component of school education[156].
In parallel, the preparation and practices of many radiology departments during this pandemic have been heavily influenced by the SARS experience. This has included formulation of rigorous protocols and reconfiguration of facilities to prevent in-hospital transmission, improvement of diagnostic capabilities, resourcing, communication and coordinated outbreak response[4,91,157,158]. It is undeniable that the SARS lessons have provided valuable experience for the healthcare community and was crucial in our battle against COVID-19.
Clear differences between SARS and COVID-19 have emerged. A paper published in The Lancet[159] shared the differences between both situations and the outbreak measures. Unlike SARS which was effectively eradicated by implementing top-down measures to stop all human-to human transmission, but due to the nature and extent of spread, mitigation measures must be implemented instead of containment in view of the current situation of COVID-19[159].
It was noted in a paper in Clinical Radiology[160] that the use of infection control advocated procedures might have contributed to the low staff sickness levels during COVID-19—which could be maintained after COVID-19. In addition, the need to embrace information technology was also required to develop a more robust digital platform for patients while minimizing waiting room utilization—a negative outcome of waiting room distancing and increased time for cleaning of rooms in this pandemic. Likewise, remote working and physical distancing have their pros and cons. A thorough reflection after the pandemic is required to facilitate the thought processes on practices to keep, and which to revert to pre-COVID[160]. In tandem, special attention should be paid towards building trust in the radiologist-to-clinician relationship amid the “distance” between these professionals[161]. Indeed, despite the valuable lessons from previous experiences, adaptations to practices and responses will be necessary to prepare the department for the next pandemic.
There is no doubt that effective, safe and high-quality medical imaging is paramount in healthcare. The number of global imaging procedures is increasing considerably. The role of medical imaging in medical decision-making and minimization of unnecessary interventions cannot be emphasized enough[82,162]. As highlighted by the European Society of Radiology and the European Federation of Radiographer Societies in a joint paper[82], radiographers and radiologists are essential in the provision of medical imaging services to patients, while continuously safeguarding patient care and safety. The joint paper distinctly reflects the concern of the medical imaging field where patient safety is key.
To date, a substantial amount of money and resources have been invested in AI for medical imaging[163]. There were profound concerns about medical imaging professionals being replaced or obsolete. Fortunately, they were not destined to become dodos. The American Medical Association (AMA) deliberately adopted the term augmented intelligence in place of the more common term AI and highlighted why AI could not replace medicine’s human component where it was believed that medicine could harness AI in ways that safely and effectively improved patient care[164].
As advocated by the AMA, AI is designed to enhance human intelligence and the patient-physician relationship but not to replace it[165]. Moreover, AI can help improve human effectiveness and efficiency in the form of a decision aid for clinical reasoning and decision making[166]. Similarly, for radiographers, AI can be used as a decision support tool to ensure that the examination performed is correct for a patient with dose optimization to answer the clinical question[167]. Importantly, AI will enable physicians to spend more precious time with their patients, improving the humanistic touch. Indeed, with the adoption of AI, radiologists can be freed up to perform more value-added tasks, while playing a more vital role in integrated clinical teams to improve patient care[168].
Undeniably, COVID-19 has become a catalyst for change in the development of telemedicine and AI in medical imaging services. With the global positive cases skyrocketing and many countries grappling with the sudden surge in waves of coronavirus, telemedicine must be considered and optimized. This is in line with the current guidance from the CDC for healthcare facilities[169]. Of which, the need for physical distancing has acted as a springboard for the rapid adoption of telemedicine solutions globally[170]. Through telemedicine, critical medical care can be provided to patients while reducing transmission of COVID-19 and preserving scarce resources amid the pandemic[171]. According to results of a nationally representative survey published by the AMA in 2018, radiology had the highest use of telemedicine for patient interactions although its scope has been limited[172,173]. While there is variability in the adoption of telemedicine across the world, the evidence is suggesting a positive role in this technology for developed countries in improving health systems’ performance and outcomes[174]. Indeed, COVID-19 has served as a reminder about the need and future potential of telemedicine.
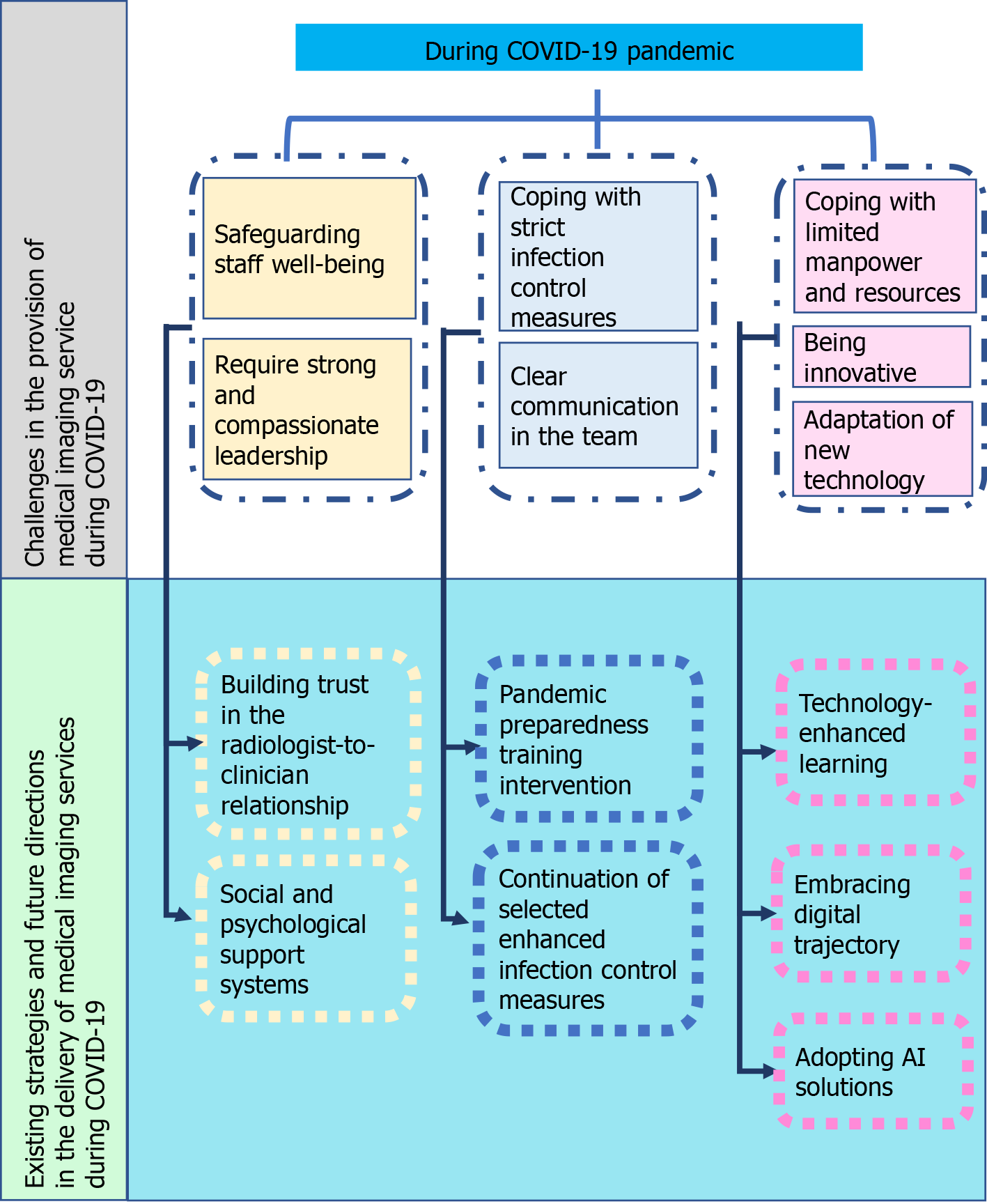
During this pandemic, AI has been harnessed in medical imaging to fight COVID-19. A collaborative network led by the National Institute of Biomedical Imaging and Bioengineering[175] has been formed to develop new tools for physicians in the early detection and optimization of treatment for COVID-19 patients. In addition, the integration of AI with medical imaging has the capability of advancing predictive medicine, preventive medicine and personalized medicine[176]. Other forms of digital transformation in medical imaging services include the use of AI in precision diagnosis, optimization of workflow and productivity[177-179]. Looking ahead, AI will be critical in empowering radiologists and radiographers across the world to address the challenges brought about by COVID-19. It is now time for medical imaging to embrace AI and the opportunities it may present in the post-COVID-19 world to enhance our patient care and patient outcome. The current challenges, strategies, and a path for future directions is described in Figure 1.
In an unprecedented pandemic, there are significant challenges globally in delivering medical imaging services and this crisis has further highlighted how complicated these challenges can be. Amid the crisis, health care is still being delivered and with the integral role of medical imaging services in the ongoing battle against COVID-19, the quality and safety of care become more important. There are dramatic implications associated with sub-optimal radiology practices and service delivery. Implementing strategies to optimize medical imaging service delivery will ensure quality healthcare in the era of COVID-19 and beyond where patient care processes continue to change rapidly. Ultimately, through the collaborative efforts of all radiology staff, we can assure provision of high-quality and safe medical imaging services while safeguarding the health of the public, patients and HCPs.
Manuscript source: Invited manuscript
Specialty type: Radiology, nuclear medicine and medical imaging
Country/Territory of origin: Singapore
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Maurea S S-Editor: Gao CC L-Editor: Webster JR P-Editor: Wang LL
| 1. | Caldaria A, Conforti C, Di Meo N, Dianzani C, Jafferany M, Lotti T, Zalaudek I, Giuffrida R. COVID-19 and SARS: Differences and similarities. Dermatol Ther. 2020;33:e13395. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 2. | World Health Organization. Naming the coronavirus disease (COVID-19) and the virus that cause. [cited 26 December 2020]. In: World Health Organization [Internet]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/naming-the-coronavirus-disease-(covid-2019)-and-the-virus-that-causes-it. |
| 3. | Zu ZY, Jiang MD, Xu PP, Chen W, Ni QQ, Lu GM, Zhang LJ. Coronavirus Disease 2019 (COVID-19): A Perspective from China. Radiology. 2020;296:E15-E25. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1106] [Cited by in RCA: 952] [Article Influence: 190.4] [Reference Citation Analysis (1)] |
| 4. | Tan BP, Lim KC, Goh YG, Kok SSX, Teo SY, Poh ACC, Kaw GJL, Quek ST, Wong SBS, Chan LP, Tan BS. Radiology Preparedness in the Ongoing Battle against COVID-19: Experiences from Large to Small Public Hospitals in Singapore. Radiol Cardiothorac Imaging. 2020;2:e200140. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 5. | Chan SS, Mak PS, Shing KK, Chan PN, Ng WH, Rainer TH. Chest radiograph screening for severe acute respiratory syndrome in the ED. Am J Emerg Med. 2005;23:525-530. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 6. | Antonio GE, Wong KT, Chu WC, Hui DS, Cheng FW, Yuen EH, Chung SS, Fok TF, Sung JJ, Ahuja AT. Imaging in severe acute respiratory syndrome (SARS). Clin Radiol. 2003;58:825-832. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Hsu LY, Lee CC, Green JA, Ang B, Paton NI, Lee L, Villacian JS, Lim PL, Earnest A, Leo YS. Severe acute respiratory syndrome (SARS) in Singapore: clinical features of index patient and initial contacts. Emerg Infect Dis. 2003;9:713-717. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 182] [Cited by in RCA: 191] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 8. | Lam WK, Zhong NS, Tan WC. Overview on SARS in Asia and the world. Respirology. 2003;8 Suppl:S2-S5. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 104] [Cited by in RCA: 86] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 9. | Kaw GJ, Tan DY, Leo YS, Tsou IY, Wansaicheong G, Chee TS. Chest radiographic findings of a case of severe acute respiratory syndrome (SARS) in Singapore. Singapore Med J. 2003;44:201-204. [PubMed] |
| 10. | Fang Y, Zhang H, Xie J, Lin M, Ying L, Pang P, Ji W. Sensitivity of Chest CT for COVID-19: Comparison to RT-PCR. Radiology. 2020;296:E115-E117. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2088] [Cited by in RCA: 1872] [Article Influence: 374.4] [Reference Citation Analysis (2)] |
| 11. | American College of Radiology. ACR Recommendations for the use of Chest Radiography and Computed Tomography (CT) for Suspected COVID-19 Infection. [cited 26 December 2020]. In: American College of Radiology [Internet]. Available from: https://www.acr.org/Advocacy-and-Economics/ACR-Position-Statements/Recommendations-for-Chest-Radiography-and-CT-for-Suspected-COVID19-Infection. |
| 12. | Society of Thoracic Radiology. Society of Thoracic Radiology/American Society of Emergency Radiology COVID-19 Position Statement. [cited 26 December 2020]. In: Society of Thoracic Radiology [Internet]. Available from: https://thoracicrad.org. |
| 13. | World Health Organization. Use of chest imaging in COVID-19. [cited 26 December 2020]. In: World Health Organization [Internet]. Available from: https://www.who.int/publications-detail-redirect/use-of-chest-imaging-in-covid-19. |
| 14. | Rubin GD, Ryerson CJ, Haramati LB, Sverzellati N, Kanne JP, Raoof S, Schluger NW, Volpi A, Yim JJ, Martin IBK, Anderson DJ, Kong C, Altes T, Bush A, Desai SR, Goldin O, Goo JM, Humbert M, Inoue Y, Kauczor HU, Luo F, Mazzone PJ, Prokop M, Remy-Jardin M, Richeldi L, Schaefer-Prokop CM, Tomiyama N, Wells AU, Leung AN. The Role of Chest Imaging in Patient Management during the COVID-19 Pandemic: A Multinational Consensus Statement from the Fleischner Society. Radiology. 2020;296:172-180. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 665] [Cited by in RCA: 605] [Article Influence: 121.0] [Reference Citation Analysis (0)] |
| 15. | Wong HYF, Lam HYS, Fong AH, Leung ST, Chin TW, Lo CSY, Lui MM, Lee JCY, Chiu KW, Chung TW, Lee EYP, Wan EYF, Hung IFN, Lam TPW, Kuo MD, Ng MY. Frequency and Distribution of Chest Radiographic Findings in Patients Positive for COVID-19. Radiology. 2020;296:E72-E78. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 832] [Cited by in RCA: 826] [Article Influence: 165.2] [Reference Citation Analysis (1)] |
| 16. | Cleverley J, Piper J, Jones MM. The role of chest radiography in confirming covid-19 pneumonia. BMJ. 2020;370:m2426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 94] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 17. | Government of Singapore. Steps to take when you’re unwell. [cited 26 December 2020]. In: Government of Singapore [Internet]. Available from: https://www.gov.sg/article/steps-to-take-when-youre-unwell. |
| 18. | Pung R, Chiew CJ, Young BE, Chin S, Chen MI, Clapham HE, Cook AR, Maurer-Stroh S, Toh MPHS, Poh C, Low M, Lum J, Koh VTJ, Mak TM, Cui L, Lin RVTP, Heng D, Leo YS, Lye DC, Lee VJM; Singapore 2019 Novel Coronavirus Outbreak Research Team. Investigation of three clusters of COVID-19 in Singapore: implications for surveillance and response measures. Lancet. 2020;395:1039-1046. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 471] [Cited by in RCA: 437] [Article Influence: 87.4] [Reference Citation Analysis (0)] |
| 19. | Jung JI. Radiologists' Solutions for COVID-19 in Korea. Korean J Radiol. 2020;21:1196-1197. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 20. | Yasin R, Gouda W. Chest X-ray findings monitoring COVID-19 disease course and severity. Egypt J Radiol Nucl Med. 2020;51:193. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 60] [Cited by in RCA: 62] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 21. | Oterino Serrano C, Alonso E, Andrés M, Buitrago NM, Pérez Vigara A, Parrón Pajares M, Cuesta López E, Garzón Moll G, Martin Espin I, Bueno Barriocanal M, De Ceano-Vivas la Calle M, Calvo Rey C, Bret-Zurita M. Pediatric chest x-ray in covid-19 infection. Eur J Radiol. 2020;131:109236. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 34] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 22. | Cellina M, Orsi M, Toluian T, Valenti Pittino C, Oliva G. False negative chest X-Rays in patients affected by COVID-19 pneumonia and corresponding chest CT findings. Radiography (Lond). 2020;26:e189-e194. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 23. | Hwang J, Yong E, Cheong K, Ling ZJ, Goh LH, Lim FS, Loh V, Bagdasarian N, Somani J, Archuleta S, Sng J, Lim SM. Responding to the COVID-19 pandemic: The role of occupational health services in a tertiary hospital in Singapore. J Occup Health. 2020;62:e12172. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 24. | World Health Organization. Novel Coronavirus (2019-nCoV)- Situation Report 10. [cited 26 December 2020]. In: World Health Organization [Internet]. Available from: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200130-sitrep-10-ncov.pdf?sfvrsn=d0b2e480_2. |
| 25. | World Health Organization. Coronavirus disease 2019 (COVID-19)- Situation Report 31. [cited 26 December 2020]. In: World Health Organization [Internet]. Available from: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200220-sitrep-31-covid-19.pdf. |
| 26. | Singapore Healthcare Corps. Join the SG Healthcare Corps. [cited 26 December 2020]. In: Singapore Healthcare Corps [Internet]. Available from: https://healthcarecorps.gov.sg/. |
| 27. | Center for Strategic and International Studies. Strengths and vulnerabilities in Southeast Asia’s response to the Covid-19 pandemic. [cited 26 December 2020]. In: Center for Strategic and International Studies [Internet]. Available from: https://www.csis.org/analysis/strengths-and-vulnerabilities-southeast-asias-response-covid-19-pandemic. |
| 28. | Reuters. Ireland’s call for retired medics to return to work gets huge response. [cited 26 December 2020]. In: Reuters [Internet]. Available from: https://www.reuters.com/article/us-health-coronavirus-ireland/irelands-call-for-retired-medics-to-return-to-work-gets-huge-response-idUSKBN2153JX. |
| 29. | National Health Service. Clinicians considering a return to the NHS. [cited 26 December 2020]. In: National Health Service [Internet]. Available from: https://www.england.nhs.uk/coronavirus/returning-clinicians/. |
| 30. | De Avila J, Chen T. To fight coronavirus, states call on retired medical staff and new graduates. The Wall Street Journal. 31 March 2020. Available from: https://www.wsj.com/articles/to-fight-coronavirus-states-call-on-retired-medical-staff-and-new-graduates-11585647003 Cited 26 December 2020.. |
| 31. | Goh Y, Chua W, Lee JKT, Ang BWL, Liang CR, Tan CA, Choong DAW, Hoon HX, Ong MKL, Quek ST. Operational Strategies to Prevent Coronavirus Disease 2019 (COVID-19) Spread in Radiology: Experience From a Singapore Radiology Department After Severe Acute Respiratory Syndrome. J Am Coll Radiol. 2020;17:717-723. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 42] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 32. | Elshami W, Akudjedu TN, Abuzaid M, David LR, Tekin HO, Cavli B, Issa B. The radiology workforce's response to the COVID-19 pandemic in the Middle East, North Africa and India. Radiography (Lond). 2021;27:360-368. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 50] [Cited by in RCA: 45] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 33. | Akudjedu TN, Botwe BO, Wuni AR, Mishio NA. Impact of the COVID-19 pandemic on clinical radiography practice in low resource settings: The Ghanaian radiographers' perspective. Radiography (Lond). 2021;27:443-452. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 25] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 34. | Shoja E, Aghamohammadi V, Bazyar H, Moghaddam HR, Nasiri K, Dashti M, Choupani A, Garaee M, Aliasgharzadeh S, Asgari A. Covid-19 effects on the workload of Iranian healthcare workers. BMC Public Health. 2020;20:1636. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 86] [Cited by in RCA: 101] [Article Influence: 20.2] [Reference Citation Analysis (0)] |
| 35. | Morgantini LA, Naha U, Wang H, Francavilla S, Acar Ö, Flores JM, Crivellaro S, Moreira D, Abern M, Eklund M, Vigneswaran HT, Weine SM. Factors contributing to healthcare professional burnout during the COVID-19 pandemic: A rapid turnaround global survey. PLoS One. 2020;15:e0238217. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 198] [Cited by in RCA: 323] [Article Influence: 64.6] [Reference Citation Analysis (0)] |
| 36. | Akudjedu TN, Lawal O, Sharma M, Elliott J, Stewart S, Gilleece T, McFadden S, Franklin JM. Impact of the COVID-19 pandemic on radiography practice: findings from a UK radiography workforce survey. BJR Open. 2020;2:20200023. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 37. | Shi J, Giess CS, Martin T, Lemaire KA, Curley PJ, Bay C, Mayo-Smith WW, Boland GW, Khorasani R. Radiology Workload Changes During the COVID-19 Pandemic: Implications for Staff Redeployment. Acad Radiol. 2021;28:1-7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 32] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 38. | Albano D, Bruno A, Bruno F, Calandri M, Caruso D, Clemente A, Coppolino P, Cozzi D, De Robertis R, Gentili F, Grazzini I, Jannone ML, Liguori C, Natella R, Pace G, Posa A, Scalise P, Accarino B, Bibbolino C, Barile A, Grassi R, Messina C; Young SIRM Working Group. Impact of coronavirus disease 2019 (COVID-19) emergency on Italian radiologists: a national survey. Eur Radiol. 2020;30:6635-6644. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 31] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 39. | Hogg P, Holmes K, McNulty J, Newman D, Keene D, Beardmore C. Covid-19: Free resources to support radiographers. Radiography (Lond). 2020;26:189-191. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 40. | Vox. The critical role of paid sick leave in the COVID-19 health and labour market crisis. [cited 26 December 2020]. In: Vox [Internet]. Available from: https://voxeu.org/article/paid-sick-leave-during-covid-19-health-and-labour-market-crisis. |
| 41. | Heng AL, Ooi CC, Wen Eu BJ, San Kiew Y, Wong ASK, Da Zhuang K. The bug stops with me: Prevention of COVID-19 nosocomial transmission during radiographic procedures. J Med Imaging Radiat Sci. 2020;51:540-545. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 42. | Peh WM, Ting Chan SK, Lee YL, Gare PS, Ho VK. Lung ultrasound in a Singapore COVID-19 intensive care unit patient and a review of its potential clinical utility in pandemic. J Ultrason. 2020;20:e154-e158. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 43. | World Federation for Ultrasound in Medicine and Biology Safety Committee (Jacques S. , Abramowicz JS, Basseal JM. World Federation for Ultrasound in Medicine and Biology Position Statement: How to Perform a Safe Ultrasound Examination and Clean Equipment in the Context of COVID-19. Ultrasound Med Biol. 2020;46:1821-1826. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 52] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 44. | Gogna A, Punamiya S, Gopinathan A, Irani F, Toh LHW, Wen Cheong LH, Babu S, Wee B, Goh P, Tan BP, Damodharan K, Venkatanarasimha N, Chan SJM, Chandramohan S, Too CW, Chung R, Ong SJ, Tan A, Tan BS, Tay KH. Preparing IR for COVID-19: The Singapore Experience. J Vasc Interv Radiol. 2020;31:869-875. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 45. | Mossa-Basha M, Meltzer CC, Kim DC, Tuite MJ, Kolli KP, Tan BS. Radiology Department Preparedness for COVID-19: Radiology Scientific Expert Review Panel. Radiology. 2020;296:E106-E112. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 192] [Cited by in RCA: 220] [Article Influence: 44.0] [Reference Citation Analysis (0)] |
| 46. | Suárez-García I, Martínez de Aramayona López MJ, Sáez Vicente A, Lobo Abascal P. SARS-CoV-2 infection among healthcare workers in a hospital in Madrid, Spain. J Hosp Infect. 2020;106:357-363. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 77] [Cited by in RCA: 84] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 47. | Cohen J, Rodgers YVM. Contributing factors to personal protective equipment shortages during the COVID-19 pandemic. Prev Med. 2020;141:106263. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 301] [Cited by in RCA: 267] [Article Influence: 53.4] [Reference Citation Analysis (0)] |
| 48. | Burki T. Global shortage of personal protective equipment. Lancet Infect Dis. 2020;20:785-786. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 104] [Cited by in RCA: 133] [Article Influence: 26.6] [Reference Citation Analysis (0)] |
| 49. | Nortajuddin A. Medical supplies shortage in ASEAN. The ASEAN Post. 25 March 2020. Available from: https://theaseanpost.com/article/medical-supplies-shortage-asean Cited 26 December 2020.. |
| 50. | Ranney ML, Griffeth V, Jha AK. Critical Supply Shortages - The Need for Ventilators and Personal Protective Equipment during the Covid-19 Pandemic. N Engl J Med. 2020;382:e41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1276] [Cited by in RCA: 1186] [Article Influence: 237.2] [Reference Citation Analysis (0)] |
| 51. | Zhan M, Qin Y, Xue X, Zhu S. Death from Covid-19 of 23 Health Care Workers in China. N Engl J Med. 2020;382:2267-2268. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 207] [Cited by in RCA: 194] [Article Influence: 38.8] [Reference Citation Analysis (0)] |
| 52. | Jeremias A, Nguyen J, Levine J, Pollack S, Engellenner W, Thakore A, Lucore C. Prevalence of SARS-CoV-2 Infection Among Health Care Workers in a Tertiary Community Hospital. JAMA Intern Med. 2020;180:1707-1709. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 62] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 53. | Alajmi J, Jeremijenko AM, Abraham JC, Alishaq M, Concepcion EG, Butt AA, Abou-Samra AB. COVID-19 infection among healthcare workers in a national healthcare system: The Qatar experience. Int J Infect Dis. 2020;100:386-389. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 60] [Cited by in RCA: 76] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 54. | Lewis S, Mulla F. Diagnostic radiographers' experience of COVID-19, Gauteng South Africa. Radiography (Lond). 2021;27:346-351. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 32] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 55. | Sim WY, Chen RC, Aw LP, Abu Bakar R, Tan CC, Heng AL, Ooi CC. How to safely and sustainably reorganise a large general radiography service facing the COVID-19 pandemic. Radiography (Lond). 2020;26:e303-e311. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 56. | Christopher WK. Contamination of X-Ray Cassettes with MRSA During Portable X-Ray Examination. J Microbiol Pathol. 2014;1:007. |
| 57. | Stogiannos N, Fotopoulos D, Woznitza N, Malamateniou C. COVID-19 in the radiology department: What radiographers need to know. Radiography (Lond). 2020;26:254-263. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 65] [Cited by in RCA: 58] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 58. | Kooraki S, Hosseiny M, Myers L, Gholamrezanezhad A. Coronavirus (COVID-19) Outbreak: What the Department of Radiology Should Know. J Am Coll Radiol. 2020;17:447-451. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 272] [Cited by in RCA: 280] [Article Influence: 56.0] [Reference Citation Analysis (0)] |
| 59. | Yu J, Ding N, Chen H, Liu XJ, He WJ, Dai WC, Zhou ZG, Lin F, Pu ZH, Li DF, Xu HJ, Wang YL, Zhang HW, Lei Y. Infection Control against COVID-19 in Departments of Radiology. Acad Radiol. 2020;27:614-617. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 59] [Cited by in RCA: 46] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 60. | American College of Radiology. ACR Recommendations for the use of Chest Radiography and Computed Tomography (CT) for Suspected COVID-19 Infection. [cited 26 December 2020]. In: American College of Radiology [Internet]. Available from: https://www.acr.org/Advocacy-and-Economics/ACR-Position-Statements/Recommendations-for-Chest-Radiography-and-CT-for-Suspected-COVID19-Infection. |
| 61. | Yan C, Lin J, Xu Y. Recommendations for coronavirus disease 2019 (COVID-19) prevention and infection control in the radiology department: Chinese experience. Clin Imaging. 2021;69:33-36. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 62. | Qu J, Yang W, Yang Y, Qin L, Yan F. Infection Control for CT Equipment and Radiographers' Personal Protection During the Coronavirus Disease (COVID-19) Outbreak in China. AJR Am J Roentgenol. 2020;215:940-944. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 63. | The BMJ. Lessons from the frontline of the covid-19 outbreak. [cited 26 December 2020]. In: The BMJ [Internet]. Available from: https://blogs.bmj.com/bmj/2020/03/20/Lessons-from-the-frontline-of-the-covid-19-outbreak/?utm_campaign=shareaholic&utm_medium=twitter&utm_source=socialnetwork. |
| 64. | Huang Z, Zhao S, Li Z, Chen W, Zhao L, Deng L, Song B. The Battle Against Coronavirus Disease 2019 (COVID-19): Emergency Management and Infection Control in a Radiology Department. J Am Coll Radiol. 2020;17:710-716. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 104] [Cited by in RCA: 87] [Article Influence: 17.4] [Reference Citation Analysis (0)] |
| 65. | Eastgate P, Neep MJ, Steffens T, Westerink A. COVID-19 Pandemic - considerations and challenges for the management of medical imaging departments in Queensland. J Med Radiat Sci. 2020;67:345-351. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 66. | Small Caps. Coronavirus prompts more orders for Micro-X’s mobile x-ray units. [cited 26 December 2020]. In: Small Caps [Internet]. Available from: https://smallcaps.com.au/coronavirus-prompts-more-orders-micro-x-mobile-x-ray-units/. |
| 67. | Marsh S, Asthana, A, Barr C. English hospitals in urgent need of more scanners and staff to deal with backlog. [cited 26 December 2020]. In: The Guardian [Internet]. Available from: https://www.theguardian.com/society/2020/jul/14/english-nhs-hospitals-in-urgent-need-of-more-scanners-and-staff-to-deal-with-backlog. |
| 68. | Applied Radiology. Canadian Association of Radiologists Works to Restore Timely Imaging During COVID. [cited 26 December 2020]. In: Applied Radiology [Internet]. Available from: https://www.appliedradiology.com/articles/canadian-association-of-radiologists-works-to-restore-timely-imaging-during-covid. |
| 69. | The Royal College of Radiologists. RCR responds to NHSE diagnostic waiting times figures for June. [cited 26 December 2020]. In: The Royal College of Radiologists [Internet]. Available from: https://www.appliedradiology.com/articles/canadian-association-of-radiologists-works-to-restore-timely-imaging-during-covid. |
| 70. | McKay D, Heisler M, Mishori R, Catton H, Kloiber O. Attacks against health-care personnel must stop, especially as the world fights COVID-19. Lancet. 2020;395:1743-1745. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 92] [Cited by in RCA: 113] [Article Influence: 22.6] [Reference Citation Analysis (0)] |
| 71. | Vizheh M, Qorbani M, Arzaghi SM, Muhidin S, Javanmard Z, Esmaeili M. The mental health of healthcare workers in the COVID-19 pandemic: A systematic review. J Diabetes Metab Disord. 2020;1-12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 367] [Cited by in RCA: 361] [Article Influence: 72.2] [Reference Citation Analysis (0)] |
| 72. | Liu Q, Luo D, Haase JE, Guo Q, Wang XQ, Liu S, Xia L, Liu Z, Yang J, Yang BX. The experiences of health-care providers during the COVID-19 crisis in China: a qualitative study. Lancet Glob Health. 2020;8:e790-e798. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 660] [Cited by in RCA: 890] [Article Influence: 178.0] [Reference Citation Analysis (0)] |
| 73. | Tay YX, Cai S, Chow HC, Lai C. The needs and concerns of clinical educators in radiography education in the face of COVID-19 pandemic. J Med Imaging Radiat Sci. 2021;52:3-8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 74. | Khanal P, Devkota N, Dahal M, Paudel K, Joshi D. Mental health impacts among health workers during COVID-19 in a low resource setting: a cross-sectional survey from Nepal. Global Health. 2020;16:89. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 107] [Cited by in RCA: 171] [Article Influence: 34.2] [Reference Citation Analysis (0)] |
| 75. | Seidi PAM, Ardebil MD, Jaff D. COVID-19 pandemic: New challenge to securing mental well-being in conflict settings. Asian J Psychiatr. 2020;51:102151. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 76. | Ayanian JZ. Mental Health Needs of Health Care Workers Providing Frontline COVID-19 Care. JAMA Health Forum. 2020;1:e200397. [RCA] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 74] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 77. | Foley SJ, O'Loughlin A, Creedon J. Early experiences of radiographers in Ireland during the COVID-19 crisis. Insights Imaging. 2020;11:104. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 41] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 78. | Ooi JWL, Er ATW, Lee WC, Chee HC. The 12-hour shift: radiographers' perspectives and its applicability during a pandemic. Radiography (Lond). 2021;27:512-518. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 79. | Diagnostic Imaging. Radiologist wellness and burnout in the COVID-19 era. [cited 26 December 2020]. In: Diagnostic Imaging [Internet]. Available from: https://www.diagnosticimaging.com/view/radiologist-wellness-and-burnout-in-the-covid-19-era. |
| 80. | Wolfman DJ, Porter KK, Johnson DL, Parikh JR. Unsustainable: COVID-19 Demands Increased Support for Radiologists. Clin Imaging. 2021;73:18-19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 81. | Waite S, Kolla S, Jeudy J, Legasto A, Macknik SL, Martinez-Conde S, Krupinski EA, Reede DL. Tired in the Reading Room: The Influence of Fatigue in Radiology. J Am Coll Radiol. 2017;14:191-197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 59] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 82. | European Society of Radiology (ESR); European Federation of Radiographer Societies (EFRS). Patient Safety in Medical Imaging: a joint paper of the European Society of Radiology (ESR) and the European Federation of Radiographer Societies (EFRS). Insights Imaging. 2019;10:45. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 28] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 83. | Graham RNJ, Woodhead T. Leadership for continuous improvement in healthcare during the time of COVID-19. Clin Radiol. 2021;76:67-72. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 84. | Shingler-Nace A. COVID-19: When Leadership Calls. Nurse Lead. 2020;18:202-203. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 85. | NEJM Catalyst. What health care leaders and clinicians say about the covid-19 pandemic. [cited 26 December 2020]. In: NEJM Catalyst [Internet]. Available from: https://catalyst.nejm.org/doi/full/10.1056/CAT.20.0177. |
| 86. | American College of Radiology. ACR COVID-19 radiology leadership resources. [cited 26 December 2020]. In: American College of Radiology [Internet]. Available from: https://www.acr.org/Practice-Management-Quality-Informatics/Radiology-Leadership-Institute/COVID-19-Leadership-Resources. |
| 87. | Radiological Society of North America. RSNA Webinar – crisis leadership during COVID-19. [cited 26 December 2020]. In: Radiological Society of North America [Internet]. Available from: https://www2.rsna.org/shared_society_pages/standard_meeting_reg/webinar_home.cfm. |
| 88. | Georgiades C. Leadership Lessons From Prior Pandemics: Turning the Coronavirus Disease 2019 (COVID-19) Pandemic Into an Opportunity. J Am Coll Radiol. 2020;17:906-908. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 89. | Seghers VJ, Desai NK, Masand PM, Nasir S, Foster TL, Indiero DA, Johnson TD, Huisman TAGM. After the initial COVID-19 surge: a phased radiology departmental re-opening plan. Pediatr Radiol. 2020;50:1551-1559. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 90. | Mahoney MC. Radiology Leadership in a Time of Crisis: A Chair's Perspective. Acad Radiol. 2020;27:1214-1216. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 91. | Tay KH, Ooi CC, Mahmood MIB, Aw LP, Chan LP, Ng DCE, Tan BS. Reconfiguring the radiology leadership team for crisis management during the COVID-19 pandemic in a large tertiary hospital in Singapore. Eur Radiol. 2021;31:468-474. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 92. | Diagnostic Imaging. 10 traits of highly effective COVID-19 Leaders. [cited 26 December 2020]. In: Diagnostic Imaging [Internet]. Available from: https://www.diagnosticimaging.com/view/10-traits-of-highly-effective-covid-19-leaders. |
| 93. | Garver KA, Young AM, Fessell D, Dombrowski JC. How to Be a Positive Radiology Leader in Times of Crisis. Acad Radiol. 2020;27:1116-1118. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 94. | Healthcare-in-europe. How the Covid-19 crisis defines good leadership. [cited 26 December 2020]. In: Healthcare-in-europe [Internet]. Available from: https://healthcare-in-europe.com/en/news/how-the-covid-19-crisis-defines-good-leadership.html. |
| 95. | Express Healthcare. Mobile DR solutions turning the tide in COVID. [cited 26 December 2020]. In: Express Healthcare [Internet]. Available from: https://www.expresshealthcare.in/blogs/guest-blogs-healthcare/mobile-dr-solutions-turning-the-tide-in-covid-management/426038/. |
| 96. | Imaging Technology News. Carestream increasing production of mobile imaging systems during pandemic. [cited 26 December 2020]. In: Imaging Technology News [Internet]. Available from: https://www.itnonline.com/content/carestream-increasing-production-mobile-imaging-systems-during-pandemic. |
| 97. |
Informa Tech.
Combatting COVID-19 |
| 98. | Agfa-Gevaert Group. #CountOnUs: Brazil hospital turns analog mobile systems into DR with Agfa’s Retrofit in their fight against COVID-19. [cited 26 December 2020]. In: Agfa-Gevaert Group [Internet]. Available from: https://medimg.agfa.com/main/countonus-brazil-hospital-turns-analog-mobile-systems-into-dr-with-agfas-retrofit-in-their-fight-against-covid-19/. |
| 99. | Agfa-Gevaert Group. #CountOnUs: Namibia hospital selects Agfa mobile unit combined with retrofit solution to handle COVID-19 workload. [cited 26 December 2020]. In: Agfa-Gevaert Group [Internet]. Available from: https://medimg.agfa.com/main/countonus-namibia-hospital-selects-agfa-mobile-unit-combined-with-retrofit-solution-to-handle-covid-19-workload. |
| 100. | Imaging Technology News. United imaging sends out more than 100 CT scanners and X-ray machines to aid diagnosis of the coronavirus. [cited 26 December 2020]. In: Imaging Technology News [Internet]. Available from: https://www.itnonline.com/content/united-imaging-sends-out-more-100-ct-scanners-and-x-ray-machines-aid-diagnosis-coronavirus. |
| 101. | Imaging Technology News. 3 strategies to leverage medical imaging data during the pandemic. [cited 26 December 2020]. In: Imaging Technology News [Internet]. Available from: https://www.itnonline.com/article/3-strategies-leverage-medical-imaging-data-during-pandemic. |
| 102. | Gartner. Healthcare technology innovations for identifying and managing COVID-19 patients. [cited 26 December 2020]. In: Gartner [Internet]. Available from: https://www.gartner.com/en/documents/3983039/healthcare-technology-innovations-for-identifying-and-ma. |
| 103. | Mamlouk MD, McCormick CM, Jun P, MD; Tang JC; Kim BS, Shen PY, Baker BL. Fighting COVID-19: One Radiology Department’s Experience. Appl Radiol. 2020;49: 16-18. |
| 104. | Cheng LT, Chan LP, Tan BH, Chen RC, Tay KH, Ling ML, Tan BS. Déjà Vu or Jamais Vu? AJR Am J Roentgenol. 2020;214:1206-1210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 50] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 105. | Vagal A, Reeder SB, Sodickson DK, Goh V, Bhujwalla ZM, Krupinski EA. The Impact of the COVID-19 Pandemic on the Radiology Research Enterprise: Radiology Scientific Expert Panel. Radiology. 2020;296:E134-E140. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 106. | Healthcare-in-europe. Radiology and COVID-19: How to establish safe workflows. [cited 26 December 2020]. In: Healthcare-in-europe [Internet]. Available from: https://healthcare-in-europe.com/en/news/radiology-covid-19-how-to-establish-safe-workflows.html. |
| 107. | Radiological Society of North America. RSNA Structured Reporting. [cited 26 December 2020]. In: Radiological Society of North America [Internet]. Available from: https://www.rsna.org/en/covid-19/RSNA-Structured-Reporting. |
| 108. | Litmanovich DE, Chung M, R Kirkbride R, Kicska G, P Kanne J. Review of Chest Radiograph Findings of COVID-19 Pneumonia and Suggested Reporting Language. J Thorac Imaging. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 28] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 109. | Yates A, Dempsey PJ, Vencken S, MacMahon PJ, Hutchinson BD. Structured reporting in portable chest radiographs: An essential tool in the diagnosis of COVID-19. Eur J Radiol. 2021;134:109414. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 110. | British Columbia Centre for Disease Control. Provincial guidance for medical imaging services within British Columbia during the COVID-19 pandemic phases. [cited 26 December 2020]. In: British Columbia Centre for Disease Control [Internet]. Available from: http://www.bccdc.ca/Health-Professionals-Site/Documents/COVID19_MedicalImagingGuidePractitioners.pdf. |
| 111. | Vagal A, Mahoney M, Allen B, Kapur S, Udstuen G, Wang L, Braley S, Makramalla A, Chadalavada S, Choe KA, Scheler J, Brown A, England E, Hudepohl J, Rybicki FJ. Rescheduling Nonurgent Care in Radiology: Implementation During the Coronavirus Disease 2019 (COVID-19) Pandemic. J Am Coll Radiol. 2020;17:882-889. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 112. | The Royal College of Radiologists. RCR advice on non-urgent and cancer imaging during the coronavirus pandemic. [cited 26 December 2020]. In: The Royal College of Radiologists [Internet]. Available from: https://www.rcr.ac.uk/college/coronavirus-covid-19-what-rcr-doing/clinical-information/rcr-advice-non-urgent-and-cancer. |
| 113. | The American Society of Breast Surgeons. ASBrS and ACR Joint Statement on Breast Screening Exams During the COVID-19 Pandemic. [cited 26 December 2020]. In: The American Society of Breast Surgeons [Internet]. Available from: https://www.breastsurgeons.org/news/?id=45. |
| 114. | Society of Breast Imaging. Society of Breast Imaging Statement on Breast Imaging during the COVID-19 Pandemic. [cited 26 December 2020]. In: Society of Breast Imaging [Internet]. Available from: https://www.sbi-online.org/Portals/0/Position%20Statements/2020/society-of-breast-imaging-statement-on-breast-imaging-during-COVID19-pandemic.pdf. |
| 115. | Czernin J, Fanti S, Meyer PT, Allen-Auerbach M, Hacker M, Sathekge M, Hicks R, Scott AM, Hatazawa J, Yun M, Schöder H, Bartenstein P, Herrmann K. Nuclear Medicine Operations in the Times of COVID-19: Strategies, Precautions, and Experiences. J Nucl Med. 2020;61:626-629. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 58] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 116. | Pan L, Zeng J, Pu H, Peng S. How to optimize the Radiology protocol during the global COVID-19 epidemic: Keypoints from Sichuan Provincial People's Hospital. Clin Imaging. 2021;69:324-327. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 117. | Peros G, Gronki F, Molitor N, Streit M, Sugimoto K, Karrer U, Lunger F, Adamina M, Breitenstein S, Lamdark T. Organizing a COVID-19 triage unit: a Swiss perspective. Emerg Microbes Infect. 2020;9:1506-1513. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 118. | Rossi A, Prochowski Iamurri A, Cerchione C, Gentili N, Danesi V, Altini M, Paganelli G, Barone D. Radiology imaging management in an Italian cancer center (IRST IRCCS) during the COVID-19 pandemic. Insights Imaging. 2020;11:129. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 119. | Wang Q, Wang X, Lin H. The role of triage in the prevention and control of COVID-19. Infect Control Hosp Epidemiol. 2020;41:772-776. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 44] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 120. | Huang T, Guo Y, Li S, Zheng Y, Lei L, Zeng X, Zhong Q, Liu Y, Liu L. Application and effects of fever screening system in the prevention of nosocomial infection in the only designated hospital of coronavirus disease 2019 (COVID-19) in Shenzhen, China. Infect Control Hosp Epidemiol. 2020;41:978-981. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 121. | World Health Organization. Establishing COVID-19 triage stations at healthcare facilities: Key instructions and tips. [cited 26 December 2020]. In: World Health Organization [Internet]. Available from: https://www.afro.who.int/sites/default/files/Covid-19/Techinical%20documents/Establishing%20COVID-19%20triage%20stations%20at%20healthcare%20facilities%20-%20Key%20instructions%20and%20tips.pdf. |
| 122. | Chen Q, Zu ZY, Jiang MD, Lu L, Lu GM, Zhang LJ. Infection Control and Management Strategy for COVID-19 in the Radiology Department: Focusing on Experiences from China. Korean J Radiol. 2020;21:851-858. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 123. | Tay YX, Sng LH, Chow HC, Zainuldin MR. Clinical placements for undergraduate diagnostic radiography students amidst the COVID-19 pandemic in Singapore: Preparation, challenges and strategies for safe resumption. J Med Imaging Radiat Sci. 2020;51:560-566. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 124. | Garg T, Shrigiriwar A, Patel K. Trainee education during COVID-19. Neuroradiology. 2020;62:1057-1058. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 125. | Health Management. New Ways of Optimising Imaging Services. [cited 26 December 2020]. In: Health Management [Internet]. Available from: https://healthmanagement.org/c/imaging/issuearticle/new-ways-of-optimising-imaging-services. |
| 126. | Sng LH, Arlany L, Toh LC, Loo TY, Ilzam NS, Wong BSS, Lanca L. Initial data from an experiment to implement a safe procedure to perform PA erect chest radiographs for COVID-19 patients with a mobile radiographic system in a "clean" zone of the hospital ward. Radiography (Lond). 2021;27:48-53. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 127. | Singapore General Hospital. Ideas bloom amid COVID-19 pressure. [cited 26 December 2020]. In: Singapore General Hospital [Internet]. Available from: https://www.sgh.com.sg/news/singapore-health/ideas-bloom-amid-COVID-19-pressure. |
| 128. | Diagnostic Imaging. Walk-Up X-ray Booth Offers Quick Scans to COVID-19 Patients. [cited 26 December 2020]. In: Diagnostic Imaging [Internet]. Available from: https://www.diagnosticimaging.com/view/walk-x-ray-booth-offers-quick-scans-covid-19-patients. |
| 129. | Myers L, Balakrishnan S, Reddy S, Gholamrezanezhad A. Coronavirus Outbreak: Is Radiology Ready? J Am Coll Radiol. 2020;17:724-729. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 130. | European Society of Cardiology. ESC Guidance for the Diagnosis and Management of CV Disease during the COVID-19 Pandemic. [cited 26 December 2020]. In: European Society of Cardiology [Internet]. Available from: https://www.escardio.org/Education/COVID-19-and-Cardiology/ESC-COVID-19-Guidance. |
| 131. | SCMR’s COVID-19 Preparedness Toolkit. Society for Cardiovascular Magnetic Resonance. [cited 26 December 2020]. In: SCMR’s COVID-19 Preparedness Toolkit [Internet]. Available from: https://scmr.org/page/COVID19. |
| 132. | Chia AQX, Cheng LT, Wijaya L, Png MA, Sim WY, Hong WL, Chen RC. Chest Radiographs and CTs in the Era of COVID-19: Indications, Operational Safety Considerations and Alternative Imaging Practices. Acad Radiol. 2020;27:1193-1203. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 133. | Niu Y, Xian J, Lei Z, Liu X, Sun Q. Management of infection control and radiological protection in diagnostic radiology examination of COVID-19 cases. Radiat Med Prot. 2020;1:75-80. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 134. | Mohakud S, Ranjan A, Naik S, Deep N. COVID-19 preparedness for portable x-rays in an Indian hospital - Safety of the radiographers, the frontline warriors. Radiography (Lond). 2020;26:270-271. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 135. | Zhao Y, Xiang C, Wang S, Peng C, Zou Q, Hu J. Radiology department strategies to protect radiologic technologists against COVID19: Experience from Wuhan. Eur J Radiol. 2020;127:108996. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 136. | Gogna A, Yogendra P, Lee SHE, Aziz A, Cheong E, Chan LP, Venkatanarasimha N. Diagnostic Ultrasound Services During the Coronavirus Disease (COVID-19) Pandemic. AJR Am J Roentgenol. 2020;215:1130-1135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 137. | Kooraki S, Hosseiny M, Raman SS, Myers L, Gholamrezanezhad A. Coronavirus Disease 2019 (COVID-19) Precautions: What the MRI Suite Should Know. J Am Coll Radiol. 2020;17:830. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 138. | Too CW, Wen DW, Patel A, Abdul Syafiq AR, Liu J, Leong S, Gogna A, Lo RHG, Tashi S, Lee KA, Kumar P, Lie SA, Tay YC, Lee LC, Ling ML, Tan BS, Tay KH. Interventional Radiology Procedures for COVID-19 Patients: How we Do it. Cardiovasc Intervent Radiol. 2020;43:827-836. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 139. | Ierardi AM, Wood BJ, Gaudino C, Angileri SA, Jones EC, Hausegger K, Carrafiello G. How to Handle a COVID-19 Patient in the Angiographic Suite. Cardiovasc Intervent Radiol. 2020;43:820-826. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 37] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 140. | World Health Organization. Hospital Preparedness for Epidemics. [cited 26 December 2020]. In: World Health Organization [Internet]. Available from: https://apps.who.int/iris/bitstream/handle/10665/151281/9789241548939_eng.pdf. |
| 141. | Springer Nature. Research in the time of a pandemic: Healthcare preparedness and response. [cited 26 December 2020]. In: Springer Nature [Internet]. Available from: https://www.springernature.com/gp/researchers/the-source/blog/blogposts-communicating-research/research-in-the-time-of-a-pandemic--healthcare-preparedness/18099038. |
| 142. | Tay YX, Wei YM, Aw LP, Lai C. The strategy to develop newly joined radiographers in a COVID-19 world: a curated orientation programme. J Med Imaging Radiat Sci. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 143. | Chow C, Shahdadpuri R, Kai-Qian K, Hwee CY. The Next Pandemic: Supporting COVID-19 Frontline Doctors Through Film Discussion. J Med Humanit. 2020;41:585-595. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 144. | Ertl-Wagner BB, Lee W, Manson DE, Amaral JG, Bojic Z, Cote MS, Fernandes JM, Murray D, Shammas A, Therrien-Miller N, Shroff MM. Preparedness for the COVID-19 pandemic in a tertiary pediatric radiology department. Pediatr Radiol. 2020;50:1059-1068. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 145. | Mohammad SA, Osman AM, Abd-Elhameed AM, Ahmed KA, Taha NM, Saleh A, Omar A, El-Meteini M, Mohamed MA. The battle against Covid-19: the experience of an Egyptian radiology department in a university setting. Egypt J Radiol Nucl Med. 2020;51:216. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 146. | Greenberg N. Mental health of health-care workers in the COVID-19 era. Nat Rev Nephrol. 2020;16:425-426. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 99] [Cited by in RCA: 122] [Article Influence: 24.4] [Reference Citation Analysis (0)] |
| 147. | Rainford LA, Zanardo M, Buissink C, Decoster R, Hennessy W, Knapp K, Kraus B, Lanca L, Lewis S, Mahlaola TB, McEntee M, O'Leary D, Precht H, Starc T, McNulty JP. The impact of COVID-19 upon student radiographers and clinical training. Radiography (Lond). 2021;27:464-474. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 40] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 148. | Wilcha RJ. Effectiveness of Virtual Medical Teaching During the COVID-19 Crisis: Systematic Review. JMIR Med Educ. 2020;6:e20963. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 251] [Cited by in RCA: 248] [Article Influence: 49.6] [Reference Citation Analysis (0)] |
| 149. | Darras KE, Spouge RJ, de Bruin ABH, Sedlic A, Hague C, Forster BB. Undergraduate Radiology Education During the COVID-19 Pandemic: A Review of Teaching and Learning Strategies [Formula: see text]. Can Assoc Radiol J. 2021;72:194-200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 47] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 150. | Tay YX, Chow HC, Ooi CC. Impact on clinical learning during coronavirus disease 2019 pandemic: from disruption to recovery and the new norms. Korean J Med Educ. 2020;32:297-305. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 151. | McRoy C, Patel L, Gaddam DS, Rothenberg S, Herring A, Hamm J, Chelala L, Weinstein J, Smith E, Awan O. Radiology Education in the Time of COVID-19: A Novel Distance Learning Workstation Experience for Residents. Acad Radiol. 2020;27:1467-1474. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52] [Cited by in RCA: 44] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 152. | Radiological Society of North America. Simulation, Virtual Reality are the Future of Radiology Education. [cited 26 December 2020]. In: Radiological Society of North America [Internet]. Available from: https://www.rsna.org/en/news/2019/September/Future-Of-Radiology-Education. |
| 153. | Health Imaging. Simulated daily readout program mimics pre-COVID workflow, earning praise from radiology residents and faculty. [cited 26 December 2020]. In: Health Imaging [Internet]. Available from: https://www.healthimaging.com/topics/practice-management/simulated-readout-pre-covid-earning-praise-radiology-residents. |
| 154. | Ashcroft J, Byrne MHV, Brennan PA, Davies RJ. Preparing medical students for a pandemic: a systematic review of student disaster training programmes. Postgrad Med J. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 57] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 155. | University World News. Putting fairness at the heart of higher education. [cited 26 December 2020]. In: University World News [Internet]. Available from: https://www.universityworldnews.com/post.php?story=20200417094523729. |
| 156. | World Economic Forum. The COVID-19 pandemic has changed education forever. This is how. [cited 26 December 2020]. In: World Economic Forum [Internet]. Available from: https://www.weforum.org/agenda/2020/04/coronavirus-education-global-covid19-online-digital-learning/. |
| 157. | Wong ASK, Ooi CC, Leow MQH, Kiew YS, Yeo KCW, Tan SG, Tay KH. Adapting Lessons From SARS for the COVID-19 Pandemic-Perspectives From Radiology Nursing in Singapore. J Radiol Nurs. 2020;39:164-167. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 158. | Pua U, Wong D. What Is Needed to Make Interventional Radiology Ready for COVID-19? Korean J Radiol. 2020;21:629-631. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 159. | Wilder-Smith A, Chiew CJ, Lee VJ. Can we contain the COVID-19 outbreak with the same measures as for SARS? Lancet Infect Dis. 2020;20:e102-e107. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 585] [Cited by in RCA: 538] [Article Influence: 107.6] [Reference Citation Analysis (0)] |
| 160. | Hudson BJ, Loughborough WW, Oliver HC, Callow ME, Pressdee DJ, Bond SJ, Freeman RJ, Wood RJ, Laugharne MJ, Hughes-Roberts Y, Colliver RJ, Robinson G, Rodrigues JCL, Phillips AJ. Lasting lessons learnt in the radiology department from the battle with COVID-19. Clin Radiol. 2020;75:586-591. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 161. | Norbash AM, Moore AV Jr, Recht MP, Brink JA, Hess CP, Won JJ, Jain S, Sun X, Brown M, Enzmann D. Early-Stage Radiology Volume Effects and Considerations with the Coronavirus Disease 2019 (COVID-19) Pandemic: Adaptations, Risks, and Lessons Learned. J Am Coll Radiol. 2020;17:1086-1095. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 50] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 162. | World Health Organization. Diagnostic imaging. [cited 26 December 2020]. In: World Health Organization [Internet]. Available from: https://www.who.int/diagnostic_imaging/en/. |
| 163. | Alexander A, Jiang A, Ferreira C, Zurkiya D. An Intelligent Future for Medical Imaging: A Market Outlook on Artificial Intelligence for Medical Imaging. J Am Coll Radiol. 2020;17:165-170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 48] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 164. | American Medical Association. Why health care AI can’t replace medicine’s human component. [cited 26 December 2020]. In: American Medical Association [Internet]. Available from: https://www.ama-assn.org/practice-management/digital/why-health-care-ai-can-t-replace-medicine-s-human-component. |
| 165. | American Medical Association. Augmented intelligence in health care - Policy. [cited 26 December 2020]. In: American Medical Association [Internet]. Available from: https://www.ama-assn.org/system/files/2019-08/ai-2018-board-policy-summary.pdf. |
| 166. | Harvard Business Review. How Hospitals Are Using AI to Battle Covid-19. [cited 26 December 2020]. In: Harvard Business Review [Internet]. Available from: https://hbr.org/2020/04/how-hospitals-are-using-ai-to-battle-covid-19. |
| 167. | European Society of Radiology. What the increasing presence of AI means for radiographers. [cited 26 December 2020]. In: European Society of Radiology [Internet]. Available from: https://ai.myesr.org/healthcare/what-the-increasing-presence-of-ai-means-for-radiographers/. |
| 168. | Ahuja AS. The impact of artificial intelligence in medicine on the future role of the physician. PeerJ. 2019;7:e7702. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 153] [Cited by in RCA: 281] [Article Influence: 46.8] [Reference Citation Analysis (0)] |
| 169. | Centers for Disease Control and Prevention. Healthcare Facilities: Managing Operations During the COVID-19 Pandemic. [cited 26 December 2020]. In: Centers for Disease Control and Prevention [Internet]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-hcf.html. |
| 170. | Blandford A, Wesson J, Amalberti R, AlHazme R, Allwihan R. Opportunities and challenges for telehealth within, and beyond, a pandemic. Lancet Glob Health. 2020;8:e1364-e1365. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 160] [Cited by in RCA: 150] [Article Influence: 30.0] [Reference Citation Analysis (0)] |
| 171. | Calton B, Abedini N, Fratkin M. Telemedicine in the Time of Coronavirus. J Pain Symptom Manage. 2020;60:e12-e14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 267] [Cited by in RCA: 263] [Article Influence: 52.6] [Reference Citation Analysis (0)] |
| 172. | Health Imaging. Radiology uses telemedicine more than any other specialty, AMA survey finds. [cited 26 December 2020]. In: Health Imaging [Internet]. Available from: https://www.healthimaging.com/topics/imaging-informatics/radiology-uses-telemedicine-most-ama-finds. |
| 173. | Radiological Society of North America. Teleradiology Soars During COVID-19 Pandemic. [cited 26 December 2020]. In: Radiological Society of North America [Internet]. Available from: https://www.rsna.org/en/news/2020/April/Telehealth-Surge. |
| 174. | Bhaskar S, Bradley S, Chattu VK, Adisesh A, Nurtazina A, Kyrykbayeva S, Sakhamuri S, Yaya S, Sunil T, Thomas P, Mucci V, Moguilner S, Israel-Korn S, Alacapa J, Mishra A, Pandya S, Schroeder S, Atreja A, Banach M, Ray D. Telemedicine Across the Globe-Position Paper From the COVID-19 Pandemic Health System Resilience PROGRAM (REPROGRAM) International Consortium (Part 1). Front Public Health. 2020;8:556720. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 147] [Cited by in RCA: 144] [Article Influence: 28.8] [Reference Citation Analysis (0)] |
| 175. | National Institutes of Health. NIH harnesses AI for COVID-19 diagnosis, treatment, and monitoring. [cited 26 December 2020]. In: National Institutes of Health [Internet]. Available from: https://www.nih.gov/news-events/news-releases/nih-harnesses-ai-covid-19-diagnosis-treatment-monitoring. |
| 176. | Becker’s Healthcare. AI is transforming diagnostic imaging. [cited 26 December 2020]. In: Becker’s Healthcare [Internet]. Available from: https://www.beckershospitalreview.com/healthcare-information-technology/ai-is-transforming-diagnostic-imaging.html. |
| 177. | Philips. Seven ways COVID-19 is accelerating digital transformation in healthcare. [cited 26 December 2020]. In: Philips [Internet]. Available from: https://www.philips.com/a-w/about/news/archive/blogs/innovation-matters/2020/20200608-seven-ways-covid-19-is-accelerating-digital-transformation-in-healthcare.html. |
| 178. | General Electric Company. 5 Ways to Improve Workflow and Productivity in Radiology Departments. [cited 26 December 2020]. In: General Electric Company [Internet]. Available from: https://www.gehealthcare.com/Long-article/5-ways-to-improve-workflow-and-productivity-in-radiology-departments. |
| 179. | Healthcare IT News. Tech optimization: Peak performance for imaging technology. [cited 26 December 2020]. In: Healthcare IT News [Internet]. Available from: https://www.healthcareitnews.com/news/tech-optimization-peak-performance-imaging-technology. |