Published online Apr 28, 2021. doi: 10.4329/wjr.v13.i4.94
Peer-review started: January 21, 2021
First decision: February 12, 2021
Revised: February 19, 2021
Accepted: April 13, 2021
Article in press: April 13, 2021
Published online: April 28, 2021
Processing time: 90 Days and 13.9 Hours
Worldwide experience about coronavirus disease 2019 (COVID-19) pandemics suggests that symptomatic disease is significantly less frequent in the pediatric age range. Nevertheless, multi-system inflammatory syndrome has been consis
Core Tip: Although the pattern of lung involvement of coronavirus disease 2019 in children reproduces the pathology described in the general population, traditional imaging modalities have several limitations in this age group. Specific and unique findings are mainly related to the occurrence of multi-system inflammatory syndrome which is a peculiar complication reproducibly reported in the pediatric population. This syndrome is characterized by occurrence of atypical symptoms as compared with presentation in adult and multimodality imaging approach has to be contemplated.
- Citation: Ferrero P, Piazza I. Cardio-thoracic imaging and COVID-19 in the pediatric population: A narrative review. World J Radiol 2021; 13(4): 94-101
- URL: https://www.wjgnet.com/1949-8470/full/v13/i4/94.htm
- DOI: https://dx.doi.org/10.4329/wjr.v13.i4.94
Coronavirus disease 2019 (COVID-19) in its most frequent clinical manifestation causes a respiratory syndrome, due to a single stranded RNA beta coronavirus infection, that may results in acute respiratory distress syndrome. Due to the clinical association of this new virus with the onset of a respiratory syndrome it has been named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). However, it has been shown that many organs and tissues, including heart, vessels, and brain may be involved in SARS-CoV-2. Furthermore COVID-19 has been repeatedly reported in the pediatric population. Among the 962 million people infected worldwide so far, the pediatric age group constitute less than 2%. Overall atypical and asymptomatic infections are more frequent in children. This might be due to a lower exposure or less susceptible lung barrier due to immature angiotensin enzyme-2 receptors[1,2].
Likewise in adults, COVID-19 in infants is characterized by a background of inflammatory activation that may involve different tissues and organs in different phases. In those area particularly hit by the virus during the first pandemic phase, we observed a surge of mucocutaneous inflammatory syndrome resembling Kawasaki disease[3,4]. This condition has been subsequently named multisystem inflammatory syndrome in children (MIS-C) associated with COVID-19[5,6].
The proteus clinical presentation of COVID-19 in children together with the possible occurrence of MIS-C prompt a different diagnostic approach in this age group as compared to adults. (Table 1) Differently from the general population data about image findings in pediatric COVID-19 are scant and sometimes conflictual.
| Adults | Pediatric age group | |
| Epidemiology | 97%-98% of 962 million (worldwide) | About 2% < 18 yr |
| Clinical presentation | Respiratory symptoms frequent | Respiratory symptoms not frequent |
| Multisystem inflammatory toxic syndrome not frequent | Multisystem inflammatory toxic syndrome typical (MIS-C) | |
| Pleuro-pericardial involvement | Not frequent | Frequent |
| Myocardial dysfunction | Not frequent | Frequent in the context of MIS-C |
| Chest X-RAY | Routinely done, good sensitivity | Low sensitivity |
| GGO sub-pleural | GGO sub-pleural basal | |
| Nodular consolidation | Nodular consolidation not frequent | |
| Peri-bronchial thickening not frequent | Peri-bronchial thickening frequent | |
| Pleural effusion rare | Pleural effusion possible | |
| CT | High sensitivity | Good sensitivity, performed inly in selected cases |
| GGO sub-pleural | GGO sub-pleural basal | |
| Nodular consolidation | Nodular consolidation not frequent | |
| Peri-bronchial thickening not frequent | Peri-bronchial thickening frequent | |
| Pleural effusion rare | Pleural effusion possible | |
| Suggested screening modality | Low-dose CT | Bed-side echo |
We aim to provide an overview of peculiarity of thoracic diagnostic algorithm in the pediatric age group, focusing relevant differences with adults.
For this narrative review the following keywords: COVID-19, SARS-CoV-2, radiology, imaging and pediatric in different combinations. Papers were screened accordingly to the information provided in the abstract. Only manuscripts written in English and focused on the thoracic district were deemed eligible for inclusion. Within the pediatric age group we did not consider any specific limit of range and all papers dealing with patients younger than 18 years were included point of view papers and editorials were also excluded. Additional data were retrieved from the references of individual papers, whenever appropriate.
Several pathophysiologic issues have been advocated to explain differences in clinical presentation of pediatric patients. In particular, an association between SARS-CoV-2 infection and a multi systemic inflammatory syndrome has been consistently reported[7-10]. Diagnostic criteria of MIS-C include fever, hypotension, evidence of cardiac or other end-organ injury together with at least two of the following: maculo
This particular presentation, characterized by multi organ inflammation rather than severe respiratory syndrome, may be due to a different immune system reactivity and a more immature and different distribution of angiotensin-converting enzyme II receptor, which is the entry receptor for the virus. The association of syndromes and the degree of lung maturity can further contribute to modulate the clinical presen
Although the concept that radiological manifestations of COVID-19 vary among different age group, information about sensitivity, specificity and characteristic findings of chest X-ray in the pediatric population are limited and conflicting[11].
Chest X-ray may be negative in more than 1/3 of patients in the pediatric group age. Reported sensitivity of chest X-ray vary from 25% to 69%[12].
Commonly encountered chest X-ray abnormalities are consolidations and ground glass opacities (GGO), differently from the adult variant, peribronchial thickening is more frequent in this clinical setting (60% to 80%)[13]. Peribronchial thickening is however aspecific and can be seen in other variant of viral pneumonia in children, while hyperinflation, which is another recognized hallmark, was not reported. Reason for chest X-ray low sensitivity is the higher prevalence of lower density, smaller size and basal opacities, obscured by the diaphragm and hepatic dome[11].
Halo sign, which is deemed to be highly specific of COVID-19, has been observed also in 50% of pediatric cases in a published series, while other finding such as crazy paving pattern or organizing pneumonia pattern, which have been reported as typical in adult with COVID-19, were not consistently reported in pediatric series[13,14].
Finally, pleural effusion is a rare manifestation of COVID-19 in adults and is almost uniquely seen in the pediatric age range being associated with involvement of other serous cavities in patients with MIS-C.
Although computer tomography (CT) has a much higher sensitivity likewise chest X-ray, according to some reports, pediatric patients are three time more likely to have normal CT scan as compared to adult. However, pooling together literature data, percentage of negative CT is very variable, ranging between 10% and 30%[15,16].
In adults, several series have found that COVID-19 typically presents with peri
It has been hypothesized that the predominant localization of radiological findings at the periphery of the lung and the presence of enlargement of the vessel feeding the involved lung area (feeding vessel sign) may be explained by the inflammatory involvement of small vessels[20]. Based on these pathogenetic models, standardized reporting methodologies have been devised providing also a ranking of suspicious according to the presence of cluster of signs[19]. However application of diagnostic CT scores based on adult cohorts resulted in low probability of the disease in the pediatric population[11]. According to this background, utilization of low dose CT as screening tool in children with laboratory inconclusive findings is controversial.
As compared to adults, pediatric series show a lower total number of pulmonary lesions and smaller size of them. Bilateral GGO confirmed to be the most common finding accounting for almost 90% of the positive scans[16,21]. Likewise general popu
Lung ultrasounds (LUS) is consistently used in the diagnostic process of different lung diseases in both adults and children[24,25].
Among patients with suspected or ascertained COVID-19, elementary ultraso
Common findings were: A line in 72%, various pattern of B line in 27%, while parenchymal nodular consolidation were more rare as compared with adults (10%)[28].
As previously mentioned, clusters of inflammatory syndrome associated with SARS-CoV-2 (MIS-C) have been consistently reported. Even though these patients usually present without respiratory symptoms, LUS showed loss of aeration or pleural effusion in all of them in a small case series[29].
Despite these limited data, use of LUS in this clinical setting might be advocated since it allow early and repeated bedside assessment avoiding X-ray exposure and patient transport in the imaging department, which might potentially increase the risk of virus spread.
Coagulation disorders have been recognized as a major complication of COVID-19 significantly affecting the prognosis[30]. In this context the ventilation/perfusion single photon emission computed tomography, either as single modality or combined with computed tomography (V/Q SPECT) can be used in selected case to diagnose pulmonary embolism in case of iodinated medium allergy or to integrate CT images. In the pediatric population clinically relevant pulmonary embolism are rarely reported therefore the need to exclude this complication is far less compelling[31]. Furthermore radionuclide exposure and the risk of infection spread across different departments, deeply limits the room for this diagnostic resource in the clinical practice.
Since the first COVID-19 outbreak, different degree of myocardial injury have been reported[32-34]. Biomarker evidence of myocardial injury has been associated with a higher mortality risk in COVID-19 patients[35]. Although typical clinical presentation of COVID-19 in the pediatric age group is rare, association of MIS-C with SARS-CoV-2 exposure has been reproducibly observed. This syndrome, originally labelled ad Kawasaky-like, is characterized by various degree of myocardial and coronary inflam
Trans-thoracic echo has a high diagnostic sensitivity in the acute phase by demon
Cardiac CT scan can provide accurate evaluation of the coronary artery anatomy and may be considered in patients with difficult acoustic windows or with extensive coronary involvement. Cardiac magnetic resonance imaging may be useful during the initial hospitalization or approximately 3 mo post-acute illness to evaluate ventricular function and myocardial characteristics including edema, diffuse fibrosis, and scar by myocardial late gadolinium enhancement[42,43].
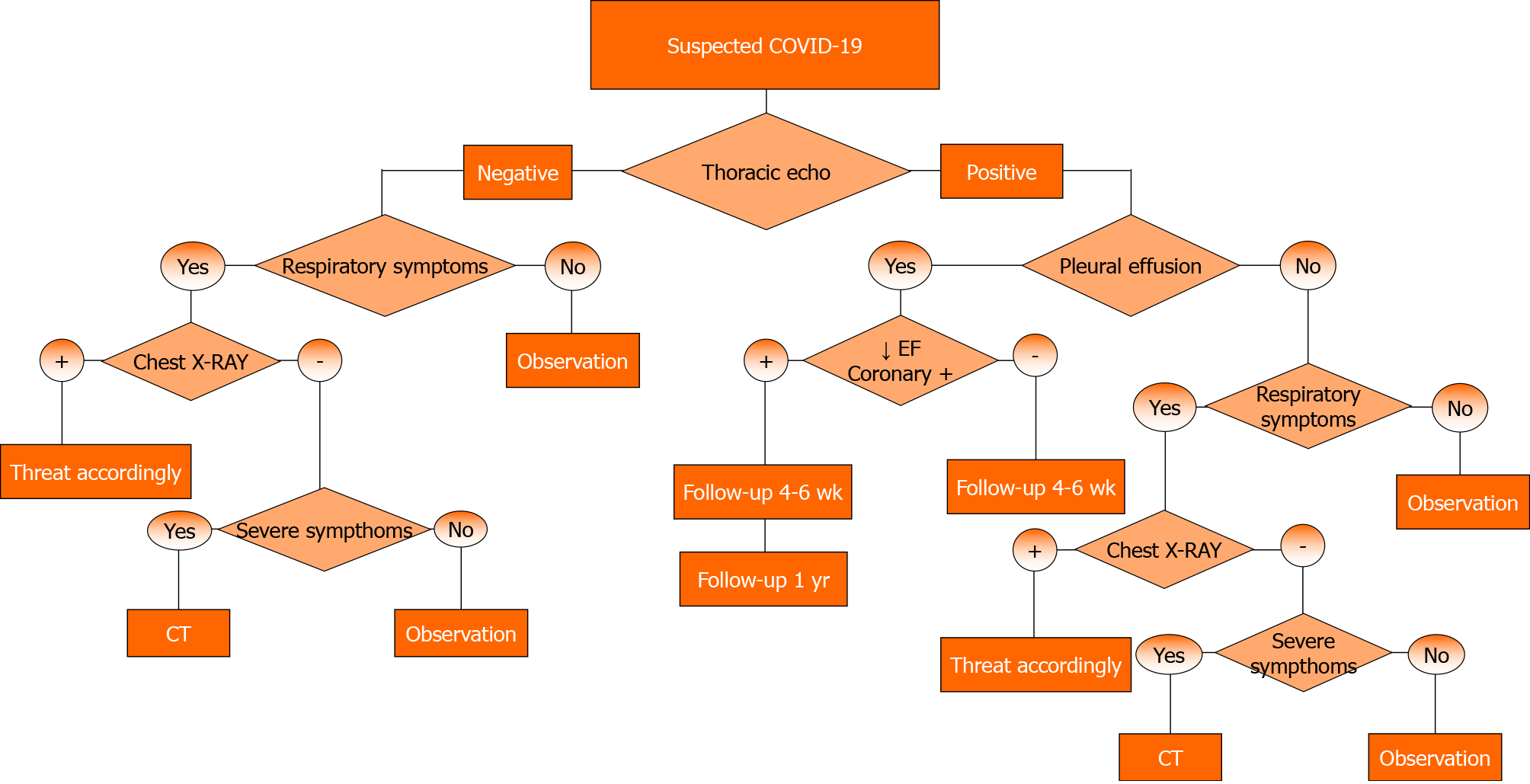
Table 1 summarizes main differences in COVID-19 that are relevant in planning the diagnostic algorithm. We considered the following nosological variables: Epidemi
So far about 96 million COVID-19 cases have been reported, of whom only less than 2% occurred in patients less than 18 years old. Furthermore, as compared with adult cohorts, fewer patients have a severe or critical course (6% vs 20%)[1].
Distribution of rate of hospitalization displays a cluster in the age group lower than two years and higher than 10 d. Although infants younger than two years rarely present pneumonia, admission is motivated by poor tolerance of fever. As far as the diagnostic algorithm is concerned, although lung involvement in SARS-CoV-2 infection in the pediatric age range may largely reproduce those reported in the general population, sensitivity of chest X-ray is significantly lower. As a consequence tradi
COVID-19 pandemics has prompted worldwide rapid reorganization of imaging departments. While the incidence of clinically relevant COVID-19 in pediatric population was previously deemed very low, the observation of a late peak of SARS-CoV-2 related disease in this age group prompted the development of specific mana
Knowledge about imaging diagnostic findings has significant grown, however significant differences in the pathophysiology and clinical presentation in children as compared with adults must be taken into account. Observational data indicate that both chest X-ray and CT have a lower diagnostic yield and can show peculiar findings, such as broncovascular thickening and pleuro-pericardial effusion, in pediatric patients. The thoracic echo may have a relevant role in the diagnostic algorithm in order to screen and monitor lung involvement as well as specific features of MIS-C in this clinical setting. Furthermore, X-ray exposure and risk of virus spread during patient transport should be taken into account when considering repeated traditional imaging.
This review is based mainly on small case series with heterogeneous populations and sometimes contradictory conclusion about findings and appropriateness of the various diagnostic tools. This limitation does not allow to pool together the data and to provide general recommendation with a sufficient grade of evidence.
Manuscript source: Invited manuscript
Specialty type: Radiology, nuclear medicine and medical imaging
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): D, D
Grade E (Poor): 0
P-Reviewer: He YF, Papazafiropoulou A S-Editor: Fan JR L-Editor: A P-Editor: Yuan YY
| 1. | Dong Y, Mo X, Hu Y, Qi X, Jiang F, Jiang Z, Tong S. Epidemiology of COVID-19 Among Children in China. Pediatrics. 2020;145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2328] [Cited by in RCA: 2411] [Article Influence: 482.2] [Reference Citation Analysis (0)] |
| 2. | Chan JF, Yuan S, Kok KH, To KK, Chu H, Yang J, Xing F, Liu J, Yip CC, Poon RW, Tsoi HW, Lo SK, Chan KH, Poon VK, Chan WM, Ip JD, Cai JP, Cheng VC, Chen H, Hui CK, Yuen KY. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395:514-523. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6483] [Cited by in RCA: 5420] [Article Influence: 1084.0] [Reference Citation Analysis (0)] |
| 3. | Verdoni L, Mazza A, Gervasoni A, Martelli L, Ruggeri M, Ciuffreda M, Bonanomi E, D'Antiga L. An outbreak of severe Kawasaki-like disease at the Italian epicentre of the SARS-CoV-2 epidemic: an observational cohort study. Lancet. 2020;395:1771-1778. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1578] [Cited by in RCA: 1667] [Article Influence: 333.4] [Reference Citation Analysis (0)] |
| 4. | Ferrero P, Piazza I, Bonino C, Ciuffreda M. Patterns of myocardial involvement in children during COVID-19 pandemic: Early experience from northern Italy. Ann Pediatr Cardiol. 2020;13:230-233. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 5. | Blumfield E, Levin TL, Kurian J, Lee EY, Liszewski MC. Imaging Findings in Multisystem Inflammatory Syndrome in Children (MIS-C) Associated With Coronavirus Disease (COVID-19). AJR Am J Roentgenol. 2021;216:507-517. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 79] [Article Influence: 19.8] [Reference Citation Analysis (0)] |
| 6. | New York City Department of Health. 2020 Health Advisory #16: Updated Reporting. Requirements for Multisystem Inflammatory Syndrome in Children Associated with COVID-19 2020. [cited 27 May 2020]. Available from: https://www1.nyc.gov/assets/doh/downloads/pdf/han/advisory/2020/covid-19-providers-mis-c.pdf. . |
| 7. | Belhadjer Z, Méot M, Bajolle F, Khraiche D, Legendre A, Abakka S, Auriau J, Grimaud M, Oualha M, Beghetti M, Wacker J, Ovaert C, Hascoet S, Selegny M, Malekzadeh-Milani S, Maltret A, Bosser G, Giroux N, Bonnemains L, Bordet J, Di Filippo S, Mauran P, Falcon-Eicher S, Thambo JB, Lefort B, Moceri P, Houyel L, Renolleau S, Bonnet D. Acute Heart Failure in Multisystem Inflammatory Syndrome in Children in the Context of Global SARS-CoV-2 Pandemic. Circulation. 2020;142:429-436. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 676] [Cited by in RCA: 862] [Article Influence: 172.4] [Reference Citation Analysis (1)] |
| 8. | Riphagen S, Gomez X, Gonzalez-Martinez C, Wilkinson N, Theocharis P. Hyperinflammatory shock in children during COVID-19 pandemic. Lancet. 2020;395:1607-1608. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1565] [Cited by in RCA: 1765] [Article Influence: 353.0] [Reference Citation Analysis (0)] |
| 9. | Blondiaux E, Parisot P, Redheuil A, Tzaroukian L, Levy Y, Sileo C, Schnuriger A, Lorrot M, Guedj R, Ducou le Pointe H. Cardiac MRI in Children with Multisystem Inflammatory Syndrome Associated with COVID-19. Radiology. 2020;297:E283-E288. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 129] [Cited by in RCA: 164] [Article Influence: 32.8] [Reference Citation Analysis (0)] |
| 10. | New York State Department of Health website. Childhood inflammatory disease relat-ed to COVID-19: overview & stats. 2020. [cited 27 May 2020]. Available from: https://profiles.health.ny.gov/#5.05/42.84/-75.88. . |
| 11. | Bayramoglu Z, Canıpek E, Comert RG, Gasimli N, Kaba O, Sarı Yanartaş M, Hançerli Torun S, Somer A, Erturk SM. Imaging Features of Pediatric COVID-19 on Chest Radiography and Chest CT: A Retrospective, Single-Center Study. Acad Radiol. 2021;28:18-27. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 12. | Choi H, Qi X, Yoon SH, Park SJ, Lee KH, Kim JY, Lee YK, Ko H, Kim KH, Park CM, Kim YH, Lei J, Hong JH, Kim H, Hwang EJ, Yoo SJ, Nam JG, Lee CH, Goo JM. Erratum: Extension of Coronavirus Disease 2019 (COVID-19) on Chest CT and Implications for Chest Radiograph Interpretation. Radiol Cardiothorac Imaging. 2020;2:e204001. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 13. | Wong HYF, Lam HYS, Fong AH, Leung ST, Chin TW, Lo CSY, Lui MM, Lee JCY, Chiu KW, Chung TW, Lee EYP, Wan EYF, Hung IFN, Lam TPW, Kuo MD, Ng MY. Frequency and Distribution of Chest Radiographic Findings in Patients Positive for COVID-19. Radiology. 2020;296:E72-E78. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 832] [Cited by in RCA: 826] [Article Influence: 165.2] [Reference Citation Analysis (1)] |
| 14. | Oterino Serrano C, Alonso E, Andrés M, Buitrago NM, Pérez Vigara A, Parrón Pajares M, Cuesta López E, Garzón Moll G, Martin Espin I, Bueno Barriocanal M, De Ceano-Vivas la Calle M, Calvo Rey C, Bret-Zurita M. Pediatric chest x-ray in covid-19 infection. Eur J Radiol. 2020;131:109236. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 34] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 15. | Nino G, Zember J, Sanchez-Jacob R, Gutierrez MJ, Sharma K, Linguraru MG. Pediatric lung imaging features of COVID-19: A systematic review and meta-analysis. Pediatr Pulmonol. 2021;56:252-263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 39] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 16. | Caro-Dominguez P, Shelmerdine SC, Toso S, Secinaro A, Toma P, Damasio MB, Navallas M, Riaza-Martin L, Gomez-Pastrana D, Ghadimi Mahani M, Desoky SM, Ugas Charcape CF, Almanza-Aranda J, Ucar ME, Lovrenski J, Gorkem SB, Alexopoulou E, Ciet P, van Schuppen J, Ducou le Pointe H, Goo HW, Kellenberger CJ, Raissaki M, Owens CM, Hirsch FW, van Rijn RR; Collaborators of the European Society of Paediatric Radiology Cardiothoracic Task Force. Thoracic imaging of coronavirus disease 2019 (COVID-19) in children: a series of 91 cases. Pediatr Radiol. 2020;50:1354-1368. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 54] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 17. | D'Andrea A, Radmilovic J, Carbone A, Forni A, Tagliamonte E, Riegler L, Liccardo B, Crescibene F, Sirignano C, Esposito G, Bossone E. Multimodality imaging in COVID-19 patients: A key role from diagnosis to prognosis. World J Radiol. 2020;12:261-271. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 5] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (1)] |
| 18. | Landete P, Quezada Loaiza CA, Aldave-Orzaiz B, Muñiz SH, Maldonado A, Zamora E, Sam Cerna AC, Del Cerro E, Alonso RC, Couñago F. Clinical features and radiological manifestations of COVID-19 disease. World J Radiol. 2020;12:247-260. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 20] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 19. | Salehi S, Abedi A, Balakrishnan S, Gholamrezanezhad A. Coronavirus Disease 2019 (COVID-19): A Systematic Review of Imaging Findings in 919 Patients. AJR Am J Roentgenol. 2020;215:87-93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 769] [Cited by in RCA: 860] [Article Influence: 172.0] [Reference Citation Analysis (0)] |
| 20. | Magro C, Mulvey JJ, Berlin D, Nuovo G, Salvatore S, Harp J, Baxter-Stoltzfus A, Laurence J. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: A report of five cases. Transl Res. 2020;220:1-13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1635] [Cited by in RCA: 1597] [Article Influence: 319.4] [Reference Citation Analysis (1)] |
| 21. | Steinberger S, Lin B, Bernheim A, Chung M, Gao Y, Xie Z, Zhao T, Xia J, Mei X, Little BP. CT Features of Coronavirus Disease (COVID-19) in 30 Pediatric Patients. AJR Am J Roentgenol. 2020;215:1303-1311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 45] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 22. | Chen A, Huang J, Liao Y, Liu Z, Chen D, Yang C, Yang R, Wei X. Differences in Clinical and Imaging Presentation of Pediatric Patients with COVID-19 in Comparison with Adults. Radiol Cardiothorac Imaging. 2020;2:e200117. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 50] [Cited by in RCA: 60] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 23. | Foust AM, Phillips GS, Chun WC, Daltro P, Das KM, Garcia-Peña P, Kilborn T, Winant AJ, Lee EY. International Expert Consensus Statement on Chest Imaging in Pediatric COVID-19 Patient Management: Imaging Findings, Imaging Study Reporting and Im-aging Study Recommendations. Radiol Cardiothorac Imaging 2020; 2: e200214. . [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 60] [Cited by in RCA: 62] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 24. | Jones BP, Tay ET, Elikashvili I, Sanders JE, Paul AZ, Nelson BP, Spina LA, Tsung JW. Feasibility and Safety of Substituting Lung Ultrasonography for Chest Radiography When Diagnosing Pneumonia in Children: A Randomized Controlled Trial. Chest. 2016;150:131-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 144] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 25. | Vazquez Martínez JL, Pérez-Caballero Macarrón C, Coca Pérez A, Tapia Moreno R, Otheo de Tejada E. Short report - Usefulness of point-of-care ultrasound in pediatric SARS-CoV-2 infection. Eur Rev Med Pharmacol Sci. 2020;24:7801-7803. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 26. | Soldati G, Smargiassi A, Inchingolo R, Buonsenso D, Perrone T, Briganti DF, Perlini S, Torri E, Mariani A, Mossolani EE, Tursi F, Mento F, Demi L. Proposal for International Standardization of the Use of Lung Ultrasound for Patients With COVID-19: A Simple, Quantitative, Reproducible Method. J Ultrasound Med. 2020;39:1413-1419. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 380] [Cited by in RCA: 421] [Article Influence: 84.2] [Reference Citation Analysis (0)] |
| 27. | Musolino AM, Supino MC, Buonsenso D, Ferro V, Valentini P, Magistrelli A, Lombardi MH, Romani L, D'Argenio P, Campana A; Roman Lung Ultrasound Study Team for Pediatric COVID-19 (ROMULUS COVID Team). Lung Ultrasound in Children with COVID-19: Preliminary Findings. Ultrasound Med Biol. 2020;46:2094-2098. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 92] [Article Influence: 18.4] [Reference Citation Analysis (0)] |
| 28. | Hizal M, Aykac K, Yayla BCC, Yilmaz A, Altun D, Akkaya HE, Bayhan GI, Kurt ANC, Karakaya J, Ozsurekci Y, Ceyhan M. Diagnostic value of lung ultrasonography in children with COVID-19. Pediatr Pulmonol. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 19] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 29. | Guitart C, Suárez R, Girona M, Bobillo-Perez S, Hernández L, Balaguer M, Cambra FJ, Jordan I; KIDS-Corona study group; Kids Corona Platform. Lung ultrasound findings in pediatric patients with COVID-19. Eur J Pediatr. 2021;180:1117-1123. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 30. | Poissy J, Goutay J, Caplan M, Parmentier E, Duburcq T, Lassalle F, Jeanpierre E, Rauch A, Labreuche J, Susen S; Lille ICU Haemostasis COVID-19 Group. Pulmonary Embolism in Patients With COVID-19: Awareness of an Increased Prevalence. Circulation. 2020;142:184-186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 724] [Cited by in RCA: 872] [Article Influence: 174.4] [Reference Citation Analysis (0)] |
| 31. | Girona-Alarcon M, Bobillo-Perez S, Sole-Ribalta A, Hernandez L, Guitart C, Suarez R, Balaguer M, Cambra FJ, Jordan I; KIDS-Corona study group; Kids Corona Platform. The different manifestations of COVID-19 in adults and children: a cohort study in an intensive care unit. BMC Infect Dis. 2021;21:87. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 33] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 32. | Wang T, Du Z, Zhu F, Cao Z, An Y, Gao Y, Jiang B. Comorbidities and multi-organ injuries in the treatment of COVID-19. Lancet. 2020;395:e52. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 414] [Cited by in RCA: 411] [Article Influence: 82.2] [Reference Citation Analysis (0)] |
| 33. | Inciardi RM, Lupi L, Zaccone G, Italia L, Raffo M, Tomasoni D, Cani DS, Cerini M, Farina D, Gavazzi E, Maroldi R, Adamo M, Ammirati E, Sinagra G, Lombardi CM, Metra M. Cardiac Involvement in a Patient With Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020;5:819-824. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1111] [Cited by in RCA: 1270] [Article Influence: 254.0] [Reference Citation Analysis (0)] |
| 34. | Gnecchi M, Moretti F, Bassi EM, Leonardi S, Totaro R, Perotti L, Zuccaro V, Perlini S, Preda L, Baldanti F, Bruno R, Visconti LO. Myocarditis in a 16-year-old boy positive for SARS-CoV-2. Lancet. 2020;395:e116. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 50] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 35. | Nie SF, Yu M, Xie T, Yang F, Wang HB, Wang ZH, Li M, Gao XL, Lv BJ, Wang SJ, Zhang XB, He SL, Qiu ZH, Liao YH, Zhou ZH, Cheng X. Cardiac Troponin I Is an Independent Predictor for Mortality in Hospitalized Patients With COVID-19. Circulation. 2020;142:608-610. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 39] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 36. | Wacker J, Malaspinas I, Aggoun Y, Bordessoule A, Vallée JP, Beghetti M. Coronary artery dilatation in a child with hyperinflammatory syndrome with SARS-CoV-2-positive serology. Eur Heart J. 2020;41:3103. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 37. | Hameed S, Elbaaly H, Reid CEL, Santos RMF, Shivamurthy V, Wong J, Jogeesvaran KH. Spectrum of Imaging Findings at Chest Radiography, US, CT, and MRI in Multisystem Inflammatory Syndrome in Children Associated with COVID-19. Radiology. 2021;298:E1-E10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 88] [Cited by in RCA: 82] [Article Influence: 20.5] [Reference Citation Analysis (0)] |
| 38. | Revzin MV, Raza S, Warshawsky R, D'Agostino C, Srivastava NC, Bader AS, Malhotra A, Patel RD, Chen K, Kyriakakos C, Pellerito JS. Multisystem Imaging Manifestations of COVID-19, Part 1: Viral Pathogenesis and Pulmonary and Vascular System Complications. Radiographics. 2020;40:1574-1599. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 64] [Cited by in RCA: 60] [Article Influence: 12.0] [Reference Citation Analysis (2)] |
| 39. | Revzin MV, Raza S, Srivastava NC, Warshawsky R, D'Agostino C, Malhotra A, Bader AS, Patel RD, Chen K, Kyriakakos C, Pellerito JS. Multisystem Imaging Manifestations of COVID-19, Part 2: From Cardiac Complications to Pediatric Manifestations. Radiographics. 2020;40:1866-1892. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 64] [Cited by in RCA: 63] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 40. | Rodriguez-Gonzalez M, Rodríguez-Campoy P, Sánchez-Códez M, Gutiérrez-Rosa I, Castellano-Martinez A, Rodríguez-Benítez A. New onset severe right ventricular failure associated with COVID-19 in a young infant without previous heart disease. Cardiol Young. 2020;30:1346-1349. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 41. | Valverde I, Singh Y, Sanchez-de-Toledo J, Theocharis P, Chikermane A, Di Filippo S, Kuciñska B, Mannarino S, Tamariz-Martel A, Gutierrez-Larraya F, Soda G, Vandekerckhove K, Gonzalez-Barlatay F, McMahon CJ, Marcora S, Napoleone CP, Duong P, Tuo G, Deri A, Nepali G, Ilina M, Ciliberti P, Miller O; AEPC COVID-19 Rapid Response Team*. Acute Cardiovascular Manifestations in 286 Children With Multisystem Inflammatory Syndrome Associated With COVID-19 Infection in Europe. Circulation. 2021;143:21-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 228] [Article Influence: 45.6] [Reference Citation Analysis (0)] |
| 42. | Alsaied T, Tremoulet AH, Burns JC, Saidi A, Dionne A, Lang SM, Newburger JW, de Ferranti S, Friedman KG. Review of Cardiac Involvement in Multisystem Inflammatory Syndrome in Children. Circulation. 2021;143:78-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 195] [Article Influence: 39.0] [Reference Citation Analysis (0)] |
| 43. | Prieto LM, Toral B, LLorente A, Coca D, Blázquez-Gamero D. Cardiovascular magnetic resonance imaging in children with pediatric inflammatory multisystem syndrome temporally associated with SARS-CoV-2 and heart dysfunction. Clin Microbiol Infect. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |