Published online Mar 28, 2021. doi: 10.4329/wjr.v13.i3.53
Peer-review started: November 3, 2020
First decision: November 16, 2020
Revised: December 7, 2020
Accepted: March 12, 2021
Article in press: March 12, 2021
Published online: March 28, 2021
Processing time: 141 Days and 19.9 Hours
The pandemic of novel coronavirus disease 2019 (COVID-19) is an infectious disease caused by +ve strand RNA virus (SARS-CoV-2, severe acute respiratory syndrome coronavirus 2) that belongs to the corona viridae family. In March, the World Health Organization declared the outbreak of novel coronavirus for the public health emergency. Although SARS-CoV-2 infection presents with respiratory symptoms, it affects other organs such as the kidneys, liver, heart and brain. Early-stage laboratory disease testing shows many false positive or negative outcomes such as less white blood cell count and a low number of lymphocyte count. However, radiological examination and diagnosis are among the main components of the diagnosis and treatment of COVID-19. In particular, for COVID-19, chest computed tomography developed vigorous initial diagnosis and disease progression assessment. However, the accuracy is limited. Although real-time reverse transcription-polymerase chain reaction is the gold standard method for the diagnosis of COVID-19, sometimes it may give false-negative results. Due to the consequences of the missing diagnosis. This resulted in a discrepancy between the two means of examination. Conversely, based on currently available evidence, we summarized the possible understanding of the various patho-physiology, radio diagnostic methods in severe COVID-19 patients. As the information on COVID-19 evolves rapidly, this review will provide vital information for scientists and clinicians to consider novel perceptions for the comprehensive knowledge of the diagnostic approaches based on current experience.
Core Tip: Computed tomography has played an important auxiliary role in diagnosing coronavirus disease 2019 (COVID-19) patients with higher sensitivity but lower specificity. Ground glass opacities pattern is the most common finding in COVID-19 infections. Recognizing the manifestations of COVID-19 on chest X-ray may be used as first-line imaging in hospitals, especially in high prevalence areas. COVID-19 classically appears as a bilateral, peripheral and patchy consolidation on imaging. It is important to remember that there may be no radiological changes in positive COVID-19 patients. In this perspective, a diagnosis of real-time reverse transcription-polymerase chain reaction is needed.
- Citation: Verma HK. Radiological and clinical spectrum of COVID-19: A major concern for public health. World J Radiol 2021; 13(3): 53-63
- URL: https://www.wjgnet.com/1949-8470/full/v13/i3/53.htm
- DOI: https://dx.doi.org/10.4329/wjr.v13.i3.53
In December 2019, pneumonia with unknown aetiology officially reported by local hospitals in Wuhan, and it is severely impending around the world[1]. Later on January 7, 2020, the World Health Organization (WHO) declared a public health emergency named the novel coronavirus disease 2019 (COVID-19). The official classification of the International Committee on Taxonomy of Viruses is called severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)[2].
COVID-19 is spreading to more than 200 countries around the world, especially the United States, India, Germany, and Russia[3,4]. Past evidence suggests that the likelihood of a pandemic has increased over the last century. Previous to COVID-19, many infections affected world populations, such as cholera (1817-1824)[5], the plague of 1855[6], Spanish flu (1918-1920)[7], Swine Flu (2009-2010) (H1N1)[8], and the SARS-CoV (2003)[9]. The transmission rate of SARS-CoV-2 is higher than SARS-CoV due to the protein structure[10].
The most common signs and symptoms of COVID-19 among people hospitalized include fever, dry cough, or shortness of breath. It might be spread by the asympto-matic, presymptomatic, and symptomatic conditions. However, the lungs are the main organs involved in the disease. Also, patients infected with COVID-19 may potentially suffer from myocardial, renal, gastrointestinal, and nervous systems damage[11-14].
Till now, No vaccine, specific drug against coronavirus. Several clinical trials of vaccines or medicines are underway and have not been completed. Further, it was showed that convalescent plasma transfusion has the effectiveness to reduce the mortality of severe COVID-19 patients[15,16]. Due to the high rate of diagnostic tests and updated content on COVID-19 is emerging every day. As radiological examination and diagnosis are among the critical components of the diagnosis and treatment of COVID-19, clinical imaging plays a unique role in the COVID-19 pandemic situation.
Since radiographers working in medical imaging on ground zero for patients often care under ever-more difficult specific working circumstances. Although attention is required to staff mental health. While the chest computed tomography (CT) has limited accuracy, in COVID-19 patients, it plays a vital role in the initial diagnosis and disease progression assessment. Further, real-time reverse transcription polymerase chain reaction (RT-PCR) is standard for the precise information of COVID-19. Due to its low detection rates and low sensitivity, sometimes it shows false-negative results. Still, they are vital resources within healthcare systems.
In this critical situation, depth work is needed the improve early diagnosis and clinical management. In this report, we seek to address the vital elements that may improve patient experiences to date on COVID-19 and the role of the radiological aspect in the diagnosis for better management have been summarised. This review may assist researchers and clinicians in understanding this disease accurately.
CoVs are non-segmented positive-sense RNA viruses belonging to the corona viridae; typically, viruses have infected many different animals, including humans and other host species[17]. Studies have shown that COVID-19 patients have several events, including systemic inflammation, thrombosis, microvascular dysfunction and hematological symptoms[18,19]. The genome sequence analysis shows that the length of SARS-CoV-2 ranges from 26 kb to 32 kb with a 5′-capping site and 3′ polyadenylation stimulates host genome transcription and translation[20]. The human SARS-CoV and SARS-CoV-2 show variable degrees of pathogenicity, but it has 82% identical to code for structural proteins (sps) and non-structural proteins (nsps)[21].
The SARS-CoV-2 genomes contain many open reading frames (ORFs), serving as a template for subgenomic mRNAs' biosynthesis. Among these are 16 nsps encoded by ORF1a and ORF1b, code for viral protein synthesis[9,22]. The spike (S) protein of SARS-CoV-2, composed of two subunits, S1 and S2, among S1, plays a crucial role in the binding of angiotensin-converting enzyme 2 (ACE2) receptor that allows the entry of virus and highly expressed in host lung epithelial cells. The transmembrane S2 domain contains heptad repeat protein that facilitates the fusion of viral and host cell membranes. Therefore, researchers are considering the S2 domain as a promising target for COVID-19[23,24].
The transmembrane protease serine 2 (TMPRSS2) and cathepsin L also facilitate the cell surface entry into the host genome[1,25]. During COVID-19 infection, these specia-lized structural cells activate immune system events expressed by antigen-presenting cells (APCs). APCs trigger a defence system containing CD4+-T-helper (Th1) designed to interact with foreign cells. After the activation of Th1 cells, it triggers the CD8+-T-killer cells, which recognize massive Th1 and Th2 cytokine to activate B-cells to produce selected viral-specific antibodies. ACE2 found on the apical surface of nasal and larynx mucosa, then targets lung epithelial cells[26,27]. Elevated white blood cells (WBCs) stimulate the cytokines, including pro-inflammatory interleukin (IL)-6. However, a higher IL-6 level increases the aggressiveness and viral spread.
A nucleic acid-based test confirms the diagnosis of COVID19 with respiratory samples[28]. Although quantitative RT-PCR is a specific method for diagnosing COVID-19, it can give false-negative and false-positive results. Yang et al[29] noticed that about 11% of sputum, 27% of nasal, and 40% of throat samples were known to be false negative after RT-PCR tests. A study has shown that the current rate of false-positive operation in the preliminary estimates shows that it could be between 0.8% and 4.0%[30]. Similarly, Katz et al[31] has shown a 7.1% false-positive result in RT-PCR with a low detection rate. This situation may lead to severe outcomes from a missed diagnosis[32]. The quantitative RT-PCR method can only result in positive outcomes, but it has not been possible to analyze the severity of COVID-19 and its development in the organs.
The symptoms of COVID-19 are nonspecific for an accurate diagnosis. In the initial stage of the onset, patients had normal or decreased WBC count and lympho-cytopenia. Some patients had elevated liver enzymes, lactate dehydrogenase and myoglobin. Increased troponin was seen in some severe cases[33]. Patients with severe disease had respiratory difficulties, including shortness of breath, chest pain or tightness with breathing, fever diminished vocal fremitus on palpation of the chest[34].
Most patients had normal procalcitonin levels but increased C-reactive protein and erythrocyte sedimentation rate at the time of admission. In severe cases, the D-dimer level was higher, and the peripheral blood T-cell phenotype of patients gradually decreased[35].
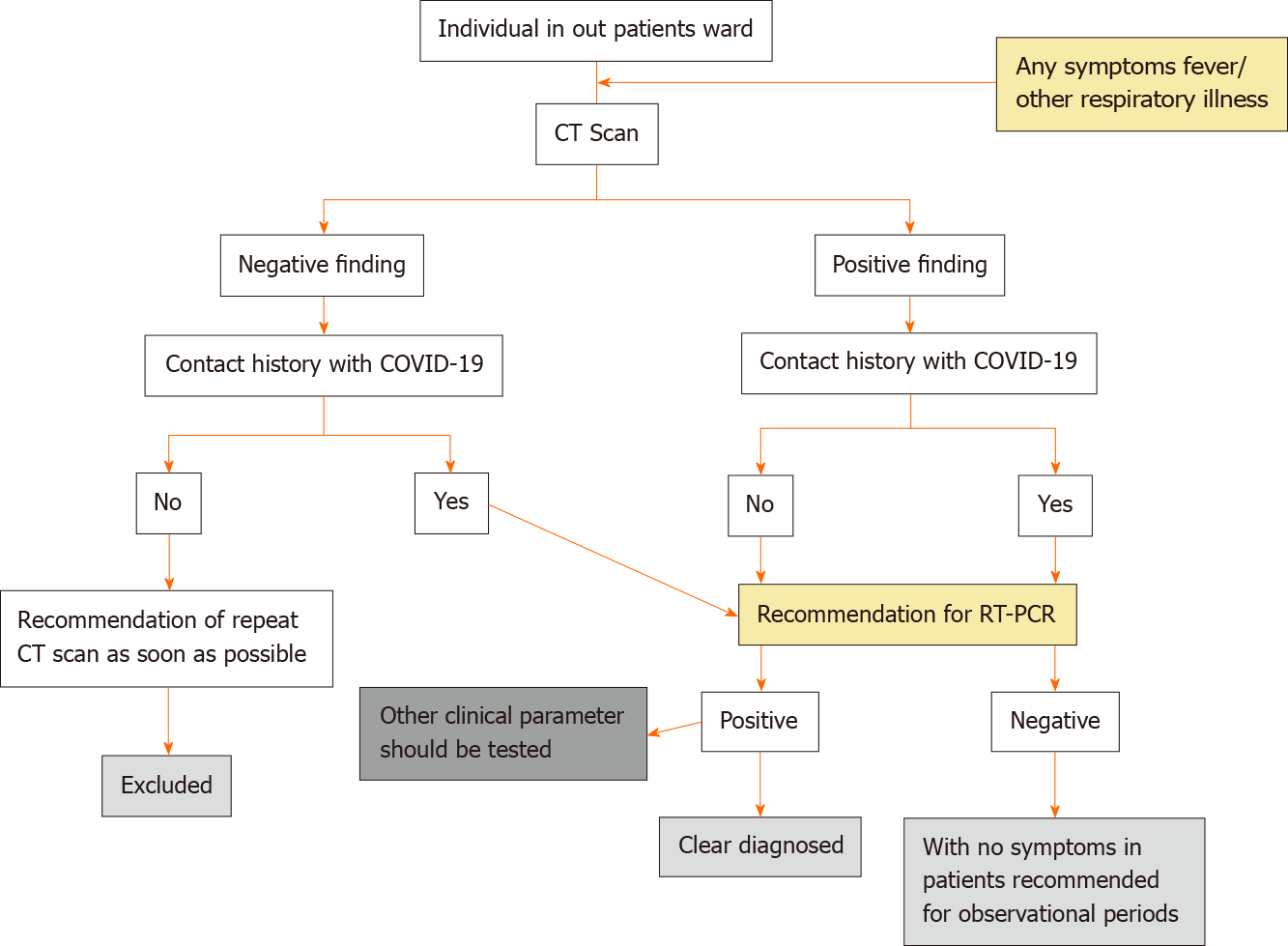
Medical imaging plays a significant role in the diagnosis and therapeutic interventions of COVID-19 patients. The recommended procedure is shown in Figure 1.
Considering that clinical ultrasound images support vital roles in early screening, diagnosis and monitoring of response to COVID-19 treatment. Across the world, the preference for radiological approaches is the same for COVID-19 as they managed in the other respiratory symptoms. The high load of the virus could be detected by chest X-ray, chest CT, lung ultrasound (LUS), and magnetic resonance imaging (MRI), that each has strengths and weakness. All of these roles have to be seen as a best-practice option.
Chest radiographs (CXR) can provide rapid and valuable information in diagnosing COVID-19 pneumonia[36]. Preliminary clinical assessment by radiologists at the time of imaging is the expected competence of professionals in many countries. As radio-logists are the first consultants to check and diagnose disease, it follows that the PCE clinical report plays a crucial role in recognizing the potential COVID-19 infection. Radiologists and referral health professionals need to know that CXR or CT does not exclude COVID-19 in high-risk patients[37]. Initial CXR report of two female COVID-19 patients showed bilateral consolidation in the lower lung areas after follow-up with patchy consolidation in Wuhan[38]. The hallmark of COVID-19 is the classical CXR patterns. Almost half of the patients with COVID-19 have an abnormal chest X-ray. The presence of ground-glass opacities (GGO), associated consolidation and crazy paving pattern linked with COVID-19 infection[39,40].
There are no abnormal results in positive COVID-19 patients on CXRs during an early or moderate stage. Pneumothorax or lung cavitation are rare complications. In severe COVID-19 cases during disease progression, the number of nodes may increase significantly and spread to central areas where the lower left lobe is more often involved than the upper and right lobes in young and middle-aged adult COVID-19 patients[41]. Imaging appearances may vary from patient to patient with the disease stages and the severity of the disease[42]. However, the existing information on the reliability of CXR in COVID-19 is limited, with fewer cases than CT in the chest and often without specific criteria for the inclusion of healthy or non-COVID-19 issues.
The sensitivity of CXRs depends on the progression of COVID-19 infection. The sensitivity (69%) of CXRs imaging is higher in mild to moderate COVID-19 patients was reported[43]. Another single-centre study found that 27 patients had a bilateral or unilateral distribution of 32 patients, and 84% had a sensitivity[44]. Besides, asymptomatic and minimally symptomatic quarantine patients' CXR results showed 58.8% sensitivity in patients positive for COVID-19, but RT-PCR confirmation was not performed[45].
Chest X-rays are the most widely used for investigating COVID-19 suspected cases due to rapid results with low sensitivity. No abnormal findings have been observed in early-stage positive COVID-19 patients. A classic picture of patchy or diffuse reticular nodule opacities and consolidation has been found in most patients with positive RT-PCR results. However, the routine chest radiography does not exclude COVID-19 pneumonia. Radiologists will be recommended for severe cases to allow quick initiation of treatments currently available for COVID-19 infection. However, there is no fixed definition for COVID-19 pneumonia to date. Radiologists may consider other respiratory symptoms when diagnosing patients[46-48].
CT, as a non-invasive imaging approach, can identify specific trademark indications in the lung related to COVID-19 pneumonia. For the precise diagnosis of COVID-19 epidemiological evidence, common symptoms and tests are crucial. Imaging will be the first choice for the diagnosis. Suspected COVID-19 patients will undergo chest X-ray as soon as possible and an urgent CT scan based on severity, also follow routine protocol[49].
Hence, CT could serve as an effective way for early screening and determination of COVID-19. The sensitivity of the CT in a present pandemic situation is the gold standard at the beginning staging with RT-PCR, which recognizes viral load and is the current reference standard in the identification of COVID-19 infection. Several researchers proposed the sensitivity of without contrast chest CT for identifying COVID-19 disease is 98% compared with initial results with 71% sensitivity in RT-PCR[50-52]. Another study has shown the chest CT has a high sensitivity of (97%). Still, a low specificity was recorded (25%), with an accuracy of 68% for the diagnosis of COVID-19, and it may be considered as a primary tool for the current pandemic situation in positively affected areas[53]. No abnormal CT findings have been observed at an early and during disease progression stage. Later on, it could appear atypical CT report, including GGO, consolidation, nodule. Further, fibrosis, predominantly in the peripheral, basal lungs, and a small amount of pleural effusion may occur[54,55].
Till-date, there is no systematic comparison study between imaging findings and clinical case-control data. There is no significant research on the imaging stage and the rating of COVID-19. Based on abnormal findings in the CT, the stages of the COVID-19 manifestation may deviate into the four categories of early-stage, progressive stage, severe stage and pneumonia-determined stage (Table 1).
| Stages | Periods | Clinical findings |
| Early-stage | < 2 d | (1) More than half of the patients have a negative chest result; (2) It shows single or multiple GGO, nodule small patchy GGO, or large patchy GGO; (3) The lesions are located predominately in the middle and lower lung lobes with subpleural, peri-fissure, or peri-bronchovascular distribution; (4) The thickening of the bronchial wall, thickening of small vessels, air bronchogram sign and the thickening of adjacent interlobular pleura are common; (5) Some large patchy GGO with subsegmental distribution and increased small vessels seems like the fine grid shadow or "crazy paving” sign; And (6) Some GGO shows "reversed halo" sign |
| Intermediate stage | 3-5 d | (1) Multiple new lesions similar to those in the early stage appeared; (2) Most of the original lesions would enlarge, with the presence of consolidation varying sizes and density; (3) Nodular, halo sign and air bronchogram sign in the consolidation could be seen; (4) Fusion or partial absorption of the original GGOs or consolidation could be seen; And (5) The scope and shape of lesions often changed after the fusion, which might not distribute along with the bronchovascular bundle thoroughly |
| Late or severe stage | 6-12 d | (1) Progression of the disease, diffuse consolidation with increased density would occur; (2) The bronchiectasis and air bronchogram sign appeared; (3) Patchy GGOs were shown in non-consolidated regions; (4) "White lung" appeared when most of the lungs were involved in the severe stage; And (5) Thickened interlobular and bilateral pleura were commonly seen with a small amount of pleural effusion |
| Resolved stage | > 14 d | (1) After the treatment, most COVID-19 patients tend to be stable and improved, showing that the range of lesions diminished, the density gradually decreased, the number of lesions reduced; (2) The GGO can be fully absorbed; And (3) In some cases, the lesions can evolve into a fibrous cord in a relatively short period |
LUS has several benefits over chest radiography and chest CT in the diagnosis of COVID-19 patients. LUS has good diagnosis efficiency, is ergonomically favourable and has less impact on preventing infections. Therefore, it is used in intensive care, cardiology and nephrology, and may also be useful in diagnosing and monitoring pneumonia. LUS may allow clinicians to assess where a patient has clinical symptoms of COVID-19 related lung damage, particularly in an intensive care setting. Although its full diagnostic role in COVID-19 patient care has not yet been identified, LUS may show alveolar damage, subpleural consolidation, white lung regions, thick irregular pleural lines and abnormal B-lines. According to LUS, the severity of COVID-19 disease is divided into moderate, severe and critical. Irregular B-lines develop and their number and distribution gradually increase across the upper and anterior areas of the lungs. However, alveolar injury, sub pleural consolidation, thick distinctive pleural lines and abnormal B-lines are not very specific to COVID-19 and can be seen in other viral pneumonia and acute respiratory distress syndrome. However, when these results are combined, they may help to diagnose during the COVID-19 pandemic. However, at present, no precise data show enhanced patient outcomes; future work should focus on further multi-center studies and the integration of LUS into clinical care pathways[59-62].
Although MRI plays a crucial role in oncology, although it is not related to evaluating lung infection, it can contribute to the defining brain and spine targets of COVID-19 positive patients. The first report of the in vivo human brain involved in a COVID-19 patient has been shown by Politi et al[63] demonstrated that a signal alteration compatible with a viral brain invasion in a cortical region. Kamishima et al[64] observed that respiratory-gated MRI is highly effective in reducing respiratory artefacts and these may use in various neurological manifestations of severe COVID-19 patients. Gulko et al[65] found that acute and sub-acute infarctions were the most common diagnosis of brain MRI imaging and leukoencephalopathy, microhemorrhage constellation, leptomeningeal contrast enhancement, and cortical fluid-attenuated inversion recovery (FLAIR) signal abnormality are common features in COVID-19 patients. In the current situation, MRI is in the diagnosis of secondary manifestations, including cardiac complications or persistent myositis. At present COVID-19 is still being explored and the use of MRI is likely to expand as we know much about this disease.
Initial screening of COVID-19 is based on clinical features, travel history in recent days, and exposure to someone confirmed to have COVID-19. Based on United States practice and WHO guidance, there are two main reasons for being tested for SARS-CoV-2, including symptoms or exposure to an infected person. Although those at higher risk, such as people over 60 years of age or underlying medical conditions, may be considered for testing when others without these high-risk factors are not considered for testing[66]. For symptomatic patients, WHO suggests that chest imaging be used for suspected COVID-19 patients for precise diagnosis even if the following condition: (1) RT-PCR test not performed; (2) RT-PCR testing performed, but results delayed; and (3) The first RT-PCR test result is negative, but patients have a severe clinical feature of COVID-19. For patients with doubted or confirmed COVID-19 who are not present in the hospital and have minor symptoms, the WHO suggests additional clinical and laboratory assessments can be done by the hospital and later maybe discharge[67]. Later on June 16, 2020, the Food and Drug Administration (FDA) took initiatives to strengthen screening tests for asymptomatic patients and recommend pooled testing for all samples. The FDA believes that the pooling of samples may be authorized for use in specific SARS-CoV-2 tests with appropriate mitigation and validation (https://www.fda.gov/medical-devices/coronavirus-covid-19-and-medical-devices/pooled-sample-testing-and-screening-testing-covid-19).
The sample may be taken from the upper (nasopharyngeal or pharyngeal) or lower respiratory tract for diagnosis of SARS-CoV-2. Accumulating data indicates that the RT-PCR tests' accuracy is more sensitive and may vary depending on the specimen[68]. Preliminary results suggested that sputum is the most accurate sample for SARS-CoV-2 diagnosis, followed by nasal and throat swabs when comparing different types of specimens[26]. Some reports have shown that nasopharyngeal or pharyngeal swab samples are more sensitive to the SARS-CoV-2diagnosis, which varies based on viral load[69-71].
Medical imaging plays a vital role in the diagnosis, management and treatment of COVID-19 patients. CXR are the most commonly used imaging method for suspected and reported COVID-19 cases, although their sensitivity is very low. On the other hand, CT in the chest is highly sensitive (97%), although not entirely specific. There are some major challenges in terms of infection control. LUS shows the benefits of chest X-rays and chests CT in the diagnosis of COVID-19 patients. It can be easily performed without the exposure of harmful radiation to patients and can be easily repeated at the bedside only. It also has more sensitivity than CXR and CT in the chest. MRI may lead to patients' diagnosis with symptoms of the central nervous system, even if it is not relevant to lung disease assessment. At present, the role of MRI is only used in the diagnosis of secondary complications of COVID-19, including cardiac complications or chronic myositis, and the use of MRI in this field is likely to increase because patients are more frequently affected by this disease[72-75].
COVID-19 is extremely infectious and people are highly vulnerable to infection in general. Medical imaging plays a crucial role in the COVID-19 pandemic, providing the benefit of additional evaluation and follow-up to critically ill patients. Based on the epidemiological evidence and clinical features, a descriptive radiological diagnosis is needed and the final diagnosis needs to be confirmed by RT-PCR testing. Even though radiological findings may be dramatic, it is not necessary to the image of all patients with suspected or confirmed COVID-19. Thus, a thorough review of the patient's epidemiological history, laboratory test results, clinical symptoms, and imaging indications are essential for early intervention, early identification, early diagnosis, first isolation, and early treatment.
Manuscript source: Invited manuscript
Specialty type: Radiology, nuclear medicine and medical imaging
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Wang DW S-Editor: Gao CC L-Editor: A P-Editor: Yuan YY
| 1. | Ou X, Liu Y, Lei X, Li P, Mi D, Ren L, Guo L, Guo R, Chen T, Hu J, Xiang Z, Mu Z, Chen X, Chen J, Hu K, Jin Q, Wang J, Qian Z. Characterization of spike glycoprotein of SARS-CoV-2 on virus entry and its immune cross-reactivity with SARS-CoV. Nat Commun. 2020;11:1620. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2003] [Cited by in RCA: 2291] [Article Influence: 458.2] [Reference Citation Analysis (0)] |
| 2. | Xiao C, Li X, Liu S, Sang Y, Gao SJ, Gao F. HIV-1 did not contribute to the 2019-nCoV genome. Emerg Microbes Infect. 2020;9:378-381. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 30] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 3. | Cucinotta D, Vanelli M. WHO Declares COVID-19 a Pandemic. Acta Biomed. 2020;91:157-160. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2625] [Reference Citation Analysis (0)] |
| 4. | Mahase E. Covid-19: WHO declares pandemic because of "alarming levels" of spread, severity, and inaction. BMJ. 2020;368:m1036. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 353] [Cited by in RCA: 387] [Article Influence: 77.4] [Reference Citation Analysis (0)] |
| 5. | Chowdhury FR, Nur Z, Hassan N, von Seidlein L, Dunachie S. Pandemics, pathogenicity and changing molecular epidemiology of cholera in the era of global warming. Ann Clin Microbiol Antimicrob. 2017;16:10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 64] [Cited by in RCA: 75] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 6. | Bramanti B, Dean KR, Walløe L, Chr Stenseth N. The Third Plague Pandemic in Europe. Proc Biol Sci. 2019;286:20182429. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 36] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 7. | Taubenberger JK, Morens DM. 1918 Influenza: the mother of all pandemics. Emerg Infect Dis. 2006;12:15-22. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 70] [Cited by in RCA: 696] [Article Influence: 36.6] [Reference Citation Analysis (0)] |
| 8. | Ratre YK, Vishvakarma NK, Bhaskar LVKS, Verma HK. Dynamic Propagation and Impact of Pandemic Influenza A (2009 H1N1) in Children: A Detailed Review. Curr Microbiol. 2020;77:3809-3820. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 9. | Luk HKH, Li X, Fung J, Lau SKP, Woo PCY. Molecular epidemiology, evolution and phylogeny of SARS coronavirus. Infect Genet Evol. 2019;71:21-30. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 164] [Cited by in RCA: 177] [Article Influence: 29.5] [Reference Citation Analysis (0)] |
| 10. | Lima CMAO. Information about the new coronavirus disease (COVID-19). Radiol Bras. 2020;53:V-VI. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 37] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 11. | Gavriatopoulou M, Korompoki E, Fotiou D, Ntanasis-Stathopoulos I, Psaltopoulou T, Kastritis E, Terpos E, Dimopoulos MA. Organ-specific manifestations of COVID-19 infection. Clin Exp Med. 2020;20:493-506. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 374] [Cited by in RCA: 323] [Article Influence: 64.6] [Reference Citation Analysis (0)] |
| 12. | Merad M, Martin JC. Pathological inflammation in patients with COVID-19: a key role for monocytes and macrophages. Nat Rev Immunol. 2020;20:355-362. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1356] [Cited by in RCA: 1805] [Article Influence: 361.0] [Reference Citation Analysis (0)] |
| 13. | Valizadeh R, Baradaran A, Mirzazadeh A, Bhaskar LVKS. Coronavirus-nephropathy; renal involvement in COVID-19. J Renal Inj Prev. 2020;9. [RCA] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 30] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 14. | Sahu T, Mehta A, Ratre YK, Jaiswal A, Vishvakarma NK, Bhaskar LVKS, Verma HK. Current understanding of the impact of COVID-19 on gastrointestinal disease: Challenges and openings. World J Gastroenterol. 2021;27:449-469. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 18] [Cited by in RCA: 15] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 15. | Verma HK, Merchant N, Verma MK, Kuru Cİ, Singh AN, Ulucan F, Verma P, Bhattacharya A, Bhaskar LVKS. Current updates on the European and WHO registered clinical trials of coronavirus disease 2019 (COVID-19). Biomed J. 2020;424-433. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 16. | Verma HK, Farran B, Bhaskar LVKS. Convalescent plasma transfusion a promising therapy for coronavirus diseases 2019 (COVID-19): current updates. Antib Therapeut. 2020;3:115-125. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 17. | Pal M, Berhanu G, Desalegn C, Kandi V. Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2): An Update. Cureus. 2020;12:e7423. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 280] [Cited by in RCA: 325] [Article Influence: 65.0] [Reference Citation Analysis (0)] |
| 18. | Słomka A, Kowalewski M, Żekanowska E. Coronavirus Disease 2019 (COVID-19): A Short Review on Hematological Manifestations. Pathogens. 2020;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 69] [Cited by in RCA: 73] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 19. | Gencer S, Lacy M, Atzler D, van der Vorst EPC, Döring Y, Weber C. Immunoinflammatory, Thrombohaemostatic, and Cardiovascular Mechanisms in COVID-19. Thromb Haemost. 2020;120:1629-1641. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 45] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 20. | Rabi FA, Al Zoubi MS, Kasasbeh GA, Salameh DM, Al-Nasser AD. SARS-CoV-2 and Coronavirus Disease 2019: What We Know So Far. Pathogens. 2020;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 493] [Cited by in RCA: 399] [Article Influence: 79.8] [Reference Citation Analysis (0)] |
| 21. | Chan JF, Kok KH, Zhu Z, Chu H, To KK, Yuan S, Yuen KY. Genomic characterization of the 2019 novel human-pathogenic coronavirus isolated from a patient with atypical pneumonia after visiting Wuhan. Emerg Microbes Infect. 2020;9:221-236. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1813] [Cited by in RCA: 1953] [Article Influence: 390.6] [Reference Citation Analysis (0)] |
| 22. | Snijder EJ, Bredenbeek PJ, Dobbe JC, Thiel V, Ziebuhr J, Poon LL, Guan Y, Rozanov M, Spaan WJ, Gorbalenya AE. Unique and conserved features of genome and proteome of SARS-coronavirus, an early split-off from the coronavirus group 2 Lineage. J Mol Biol. 2003;331:991-1004. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 946] [Cited by in RCA: 965] [Article Influence: 43.9] [Reference Citation Analysis (0)] |
| 23. | Kirchdoerfer RN, Cottrell CA, Wang N, Pallesen J, Yassine HM, Turner HL, Corbett KS, Graham BS, McLellan JS, Ward AB. Pre-fusion structure of a human coronavirus spike protein. Nature. 2016;531:118-121. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 588] [Cited by in RCA: 573] [Article Influence: 63.7] [Reference Citation Analysis (0)] |
| 24. | Xu X, Chen P, Wang J, Feng J, Zhou H, Li X, Zhong W, Hao P. Evolution of the novel coronavirus from the ongoing Wuhan outbreak and modeling of its spike protein for risk of human transmission. Sci China Life Sci. 2020;63:457-460. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1252] [Cited by in RCA: 1316] [Article Influence: 263.2] [Reference Citation Analysis (0)] |
| 25. | Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler T, Erichsen S, Schiergens TS, Herrler G, Wu NH, Nitsche A, Müller MA, Drosten C, Pöhlmann S. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell 2020; 181: 271-280. e8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11946] [Cited by in RCA: 14271] [Article Influence: 2854.2] [Reference Citation Analysis (0)] |
| 26. | Chen C, Zhang XR, Ju ZY, He WF. [Advances in the research of mechanism and related immunotherapy on the cytokine storm induced by coronavirus disease 2019]. Zhonghua Shao Shang Za Zhi. 2020;36:471-475. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 86] [Reference Citation Analysis (0)] |
| 27. | Bennardo F, Buffone C, Giudice A. New therapeutic opportunities for COVID-19 patients with Tocilizumab: Possible correlation of interleukin-6 receptor inhibitors with osteonecrosis of the jaws. Oral Oncol. 2020;106:104659. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 73] [Cited by in RCA: 73] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 28. | Xie C, Jiang L, Huang G, Pu H, Gong B, Lin H, Ma S, Chen X, Long B, Si G, Yu H, Yang X, Shi Y, Yang Z. Comparison of different samples for 2019 novel coronavirus detection by nucleic acid amplification tests. Int J Infect Dis. 2020;93:264-267. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 225] [Cited by in RCA: 228] [Article Influence: 45.6] [Reference Citation Analysis (0)] |
| 29. | Yang Y, Yang M, Yuan J, Wang F, Wang Z, Li J, Zhang M, Xing L, Wei J, Peng L, Wong G, Zheng H, Wu W, Shen C, Liao M, Feng K, Yang Q, Zhao J, Liu L, Liu Y. Comparative Sensitivity of Different Respiratory Specimen Types for Molecular Diagnosis and Monitoring of SARS-CoV-2 Shedding. Innovation (N Y). 2020;1:100061. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 70] [Cited by in RCA: 119] [Article Influence: 23.8] [Reference Citation Analysis (0)] |
| 30. | Cohen AN, Kessel B, Milgroom MG. False positives in reverse transcription PCR testing for SARS-CoV-2. 2020 Preprint. Available from: medRxiv:2020.04.26.200809. [DOI] [Full Text] |
| 31. | Katz AP, Civantos FJ, Sargi Z, Leibowitz JM, Nicolli EA, Weed D, Moskovitz AE, Civantos AM, Andrews DM, Martinez O, Thomas GR. False-positive reverse transcriptase polymerase chain reaction screening for SARS-CoV-2 in the setting of urgent head and neck surgery and otolaryngologic emergencies during the pandemic: Clinical implications. Head Neck. 2020;42:1621-1628. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 37] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 32. | Coleman JJ, Manavi K, Marson EJ, Botkai AH, Sapey E. COVID-19: to be or not to be; that is the diagnostic question. Postgrad Med J. 2020;96:392-398. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 34] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 33. | Kermali M, Khalsa RK, Pillai K, Ismail Z, Harky A. The role of biomarkers in diagnosis of COVID-19 - A systematic review. Life Sci. 2020;254:117788. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 329] [Cited by in RCA: 420] [Article Influence: 84.0] [Reference Citation Analysis (0)] |
| 34. | Xie J, Tong Z, Guan X, Du B, Qiu H. Clinical Characteristics of Patients Who Died of Coronavirus Disease 2019 in China. JAMA Netw Open. 2020;3:e205619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 223] [Cited by in RCA: 229] [Article Influence: 45.8] [Reference Citation Analysis (0)] |
| 35. | Yuan X, Huang W, Ye B, Chen C, Huang R, Wu F, Wei Q, Zhang W, Hu J. Changes of hematological and immunological parameters in COVID-19 patients. Int J Hematol. 2020;112:553-559. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 101] [Cited by in RCA: 91] [Article Influence: 18.2] [Reference Citation Analysis (0)] |
| 36. | Jacobi A, Chung M, Bernheim A, Eber C. Portable chest X-ray in coronavirus disease-19 (COVID-19): A pictorial review. Clin Imaging. 2020;64:35-42. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 371] [Cited by in RCA: 308] [Article Influence: 61.6] [Reference Citation Analysis (0)] |
| 37. | Wong HYF, Lam HYS, Fong AH, Leung ST, Chin TW, Lo CSY, Lui MM, Lee JCY, Chiu KW, Chung TW, Lee EYP, Wan EYF, Hung IFN, Lam TPW, Kuo MD, Ng MY. Frequency and Distribution of Chest Radiographic Findings in Patients Positive for COVID-19. Radiology. 2020;296:E72-E78. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 832] [Cited by in RCA: 827] [Article Influence: 165.4] [Reference Citation Analysis (1)] |
| 38. | Huang WH, Teng LC, Yeh TK, Chen YJ, Lo WJ, Wu MJ, Chin CS, Tsan YT, Lin TC, Chai JW, Lin CF, Tseng CH, Liu CW, Wu CM, Chen PY, Shi ZY, Liu PY. 2019 novel coronavirus disease (COVID-19) in Taiwan: Reports of two cases from Wuhan, China. J Microbiol Immunol Infect. 2020;53:481-484. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 45] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 39. | Carotti M, Salaffi F, Sarzi-Puttini P, Agostini A, Borgheresi A, Minorati D, Galli M, Marotto D, Giovagnoni A. Chest CT features of coronavirus disease 2019 (COVID-19) pneumonia: key points for radiologists. Radiol Med. 2020;125:636-646. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 165] [Cited by in RCA: 128] [Article Influence: 25.6] [Reference Citation Analysis (0)] |
| 40. | Ye Z, Zhang Y, Wang Y, Huang Z, Song B. Chest CT manifestations of new coronavirus disease 2019 (COVID-19): a pictorial review. Eur Radiol. 2020;30:4381-4389. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 896] [Cited by in RCA: 792] [Article Influence: 158.4] [Reference Citation Analysis (0)] |
| 41. | Toussie D, Voutsinas N, Finkelstein M, Cedillo MA, Manna S, Maron SZ, Jacobi A, Chung M, Bernheim A, Eber C, Concepcion J, Fayad ZA, Gupta YS. Clinical and Chest Radiography Features Determine Patient Outcomes in Young and Middle-aged Adults with COVID-19. Radiology. 2020;297:E197-E206. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 183] [Cited by in RCA: 223] [Article Influence: 44.6] [Reference Citation Analysis (0)] |
| 42. | Feng Z, Yu Q, Yao S, Luo L, Zhou W, Mao X, Li J, Duan J, Yan Z, Yang M, Tan H, Ma M, Li T, Yi D, Mi Z, Zhao H, Jiang Y, He Z, Li H, Nie W, Liu Y, Zhao J, Luo M, Liu X, Rong P, Wang W. Early prediction of disease progression in COVID-19 pneumonia patients with chest CT and clinical characteristics. Nat Commun. 2020;11:4968. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 121] [Cited by in RCA: 156] [Article Influence: 31.2] [Reference Citation Analysis (0)] |
| 43. | Stephanie S, Shum T, Cleveland H, Challa SR, Herring A, Jacobson FL, Hatabu H, Byrne SC, Shashi K, Araki T, Hernandez JA, White CS, Hossain R, Hunsaker AR, Hammer MM. Determinants of Chest X-Ray Sensitivity for COVID- 19: A Multi-Institutional Study in the United States. Radiology: Cardiothoracic Imag. 2020;2:e200337. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 39] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 44. | Lomoro P, Verde F, Zerboni F, Simonetti I, Borghi C, Fachinetti C, Natalizi A, Martegani A. COVID-19 pneumonia manifestations at the admission on chest ultrasound, radiographs, and CT: single-center study and comprehensive radiologic literature review. Eur J Radiol Open. 2020;7:100231. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 186] [Cited by in RCA: 179] [Article Influence: 35.8] [Reference Citation Analysis (0)] |
| 45. | Pan F, Ye T, Sun P, Gui S, Liang B, Li L, Zheng D, Wang J, Hesketh RL, Yang L, Zheng C. Time Course of Lung Changes at Chest CT during Recovery from Coronavirus Disease 2019 (COVID-19). Radiology. 2020;295:715-721. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1617] [Cited by in RCA: 1761] [Article Influence: 352.2] [Reference Citation Analysis (0)] |
| 46. | Durrani M, Haq IU, Kalsoom U, Yousaf A. Chest X-rays findings in COVID 19 patients at a University Teaching Hospital - A descriptive study. Pak J Med Sci. 2020;36:S22-S26. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 31] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 47. | Cozzi D, Albanesi M, Cavigli E, Moroni C, Bindi A, Luvarà S, Lucarini S, Busoni S, Mazzoni LN, Miele V. Chest X-ray in new Coronavirus Disease 2019 (COVID-19) infection: findings and correlation with clinical outcome. Radiol Med. 2020;125:730-737. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 155] [Cited by in RCA: 181] [Article Influence: 36.2] [Reference Citation Analysis (0)] |
| 48. | Cleverley J, Piper J, Jones MM. The role of chest radiography in confirming covid-19 pneumonia. BMJ. 2020;370:m2426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 94] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 49. | Shen K, Yang Y, Wang T, Zhao D, Jiang Y, Jin R, Zheng Y, Xu B, Xie Z, Lin L, Shang Y, Lu X, Shu S, Bai Y, Deng J, Lu M, Ye L, Wang X, Wang Y, Gao L; China National Clinical Research Center for Respiratory Diseases; National Center for Children’s Health; Beijing, China; Group of Respirology; Chinese Pediatric Society, Chinese Medical Association; Chinese Medical Doctor Association Committee on Respirology Pediatrics; China Medicine Education Association Committee on Pediatrics; Chinese Research Hospital Association Committee on Pediatrics; Chinese Non-government Medical Institutions Association Committee on Pediatrics; China Association of Traditional Chinese Medicine; Committee on Children’s Health and Medicine Research; China News of Drug Information Association; Committee on Children’s Safety Medication; Global Pediatric Pulmonology Alliance. Diagnosis, treatment, and prevention of 2019 novel coronavirus infection in children: experts' consensus statement. World J Pediatr. 2020;16:223-231. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 362] [Cited by in RCA: 383] [Article Influence: 76.6] [Reference Citation Analysis (0)] |
| 50. | Udugama B, Kadhiresan P, Kozlowski HN, Malekjahani A, Osborne M, Li VYC, Chen H, Mubareka S, Gubbay JB, Chan WCW. Diagnosing COVID-19: The Disease and Tools for Detection. ACS Nano. 2020;14:3822-3835. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1198] [Cited by in RCA: 1079] [Article Influence: 215.8] [Reference Citation Analysis (0)] |
| 51. | Chen Z, Fan H, Cai J, Li Y, Wu B, Hou Y, Xu S, Zhou F, Liu Y, Xuan W, Hu H, Sun J. High-resolution computed tomography manifestations of COVID-19 infections in patients of different ages. Eur J Radiol. 2020;126:108972. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 74] [Cited by in RCA: 85] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 52. | Jiang Y, Guo D, Li C, Chen T, Li R. High-resolution CT features of the COVID-19 infection in Nanchong City: Initial and follow-up changes among different clinical types. Radiol Infect Dis. 2020;7:71-77. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 53. | Ai T, Yang Z, Hou H, Zhan C, Chen C, Lv W, Tao Q, Sun Z, Xia L. Correlation of Chest CT and RT-PCR Testing for Coronavirus Disease 2019 (COVID-19) in China: A Report of 1014 Cases. Radiology. 2020;296:E32-E40. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3614] [Cited by in RCA: 3285] [Article Influence: 657.0] [Reference Citation Analysis (0)] |
| 54. | Pan Y, Guan H, Zhou S, Wang Y, Li Q, Zhu T, Hu Q, Xia L. Initial CT findings and temporal changes in patients with the novel coronavirus pneumonia (2019-nCoV): a study of 63 patients in Wuhan, China. Eur Radiol. 2020;30:3306-3309. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 564] [Cited by in RCA: 632] [Article Influence: 126.4] [Reference Citation Analysis (0)] |
| 55. | Xie X, Zhong Z, Zhao W, Zheng C, Wang F, Liu J. Chest CT for Typical Coronavirus Disease 2019 (COVID-19) Pneumonia: Relationship to Negative RT-PCR Testing. Radiology. 2020;296:E41-E45. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1213] [Cited by in RCA: 1211] [Article Influence: 242.2] [Reference Citation Analysis (1)] |
| 56. | Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, Liu L, Shan H, Lei CL, Hui DSC, Du B, Li LJ, Zeng G, Yuen KY, Chen RC, Tang CL, Wang T, Chen PY, Xiang J, Li SY, Wang JL, Liang ZJ, Peng YX, Wei L, Liu Y, Hu YH, Peng P, Wang JM, Liu JY, Chen Z, Li G, Zheng ZJ, Qiu SQ, Luo J, Ye CJ, Zhu SY, Zhong NS; China Medical Treatment Expert Group for Covid-19. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382:1708-1720. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19202] [Cited by in RCA: 18877] [Article Influence: 3775.4] [Reference Citation Analysis (7)] |
| 57. | Zhen-Dong Y, Gao-Jun Z, Run-Ming J, Zhi-Sheng L, Zong-Qi D, Xiong X, Guo-Wei S. Clinical and transmission dynamics characteristics of 406 children with coronavirus disease 2019 in China: A review. J Infect. 2020;81:e11-e15. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 54] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 58. | Zou L, Dai L, Zhang Y, Fu W, Gao Y, Zhang Z. Clinical Characteristics and Risk Factors for Disease Severity and Death in Patients With Coronavirus Disease 2019 in Wuhan, China. Front Med (Lausanne). 2020;7:532. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 34] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 59. | Jackson K, Butler R, Aujayeb A. Lung ultrasound in the COVID-19 pandemic. Postgrad Med J. 2021;97:34-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 38] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 60. | Soldati G, Smargiassi A, Inchingolo R, Buonsenso D, Perrone T, Briganti DF, Perlini S, Torri E, Mariani A, Mossolani EE, Tursi F, Mento F, Demi L. Is There a Role for Lung Ultrasound During the COVID-19 Pandemic? J Ultrasound Med. 2020;39:1459-1462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 298] [Cited by in RCA: 312] [Article Influence: 62.4] [Reference Citation Analysis (0)] |
| 61. | Kulkarni S, Down B, Jha S. Point-of-care lung ultrasound in intensive care during the COVID-19 pandemic. Clin Radiol 2020; 75: 710.e1-710. e4. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 43] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 62. | Brachini G, Sapienza P, Cirillo B, Fonsi GB, Crocetti D, Mingoli A. Role of lung ultrasound in patients requiring emergency surgery during COVID-19 Pandemic. Br J Surg. 2020;. [PubMed] |
| 63. | Politi LS, Salsano E, Grimaldi M. Magnetic Resonance Imaging Alteration of the Brain in a Patient With Coronavirus Disease 2019 (COVID-19) and Anosmia. JAMA Neurol. 2020;77:1028-1029. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 253] [Cited by in RCA: 271] [Article Influence: 54.2] [Reference Citation Analysis (0)] |
| 64. | Kamishima T, An Y, Fang W, Lu Y. Editorial for "Clinical Potential of UTE-MRI for Assessing the COVID-19: Patient- and Lesion-Based Comparative Analysis". J Magn Reson Imaging. 2020;52:956-957. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 65. | Gulko E, Oleksk ML, Gomes W, Ali S, Mehta H, Overby P, Al-Mufti F, Rozenshtein A. MRI Brain Findings in 126 Patients with COVID-19: Initial Observations from a Descriptive Literature Review. AJNR Am J Neuroradiol. 2020;41:2199-2203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 54] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 66. | Mossa-Basha M, Medverd J, Linnau KF, Lynch JB, Wener MH, Kicska G, Staiger T, Sahani DV. Policies and Guidelines for COVID-19 Preparedness: Experiences from the University of Washington. Radiology. 2020;296:E26-E31. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 89] [Cited by in RCA: 97] [Article Influence: 19.4] [Reference Citation Analysis (0)] |
| 67. | Chou R, Pappas M, Buckley D, McDonagh M, Totten A, Flor N, Sardanelli F, Dana T, Hart E, Wasson N, Nelson H. Use of chest imaging in COVID-19: a rapid advice guide. 2nd ed. Geneva: World Health Organization; 2020. |
| 68. | COVID-19 Investigation Team. Clinical and virologic characteristics of the first 12 patients with coronavirus disease 2019 (COVID-19) in the United States. Nat Med. 2020;26:861-868. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 238] [Cited by in RCA: 245] [Article Influence: 49.0] [Reference Citation Analysis (0)] |
| 69. | Pan Y, Zhang D, Yang P, Poon LLM, Wang Q. Viral load of SARS-CoV-2 in clinical samples. Lancet Infect Dis. 2020;20:411-412. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1120] [Cited by in RCA: 1127] [Article Influence: 225.4] [Reference Citation Analysis (0)] |
| 70. | Yan Y, Chang L, Wang L. Laboratory testing of SARS-CoV, MERS-CoV, and SARS-CoV-2 (2019-nCoV): Current status, challenges, and countermeasures. Rev Med Virol. 2020;30:e2106. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 228] [Cited by in RCA: 204] [Article Influence: 40.8] [Reference Citation Analysis (0)] |
| 71. | Mawaddah A, Gendeh HS, Lum SG, Marina MB. Upper respiratory tract sampling in COVID-19. Malays J Pathol. 2020;42:23-35. [PubMed] |
| 72. | Antúnez-Montes OY, Buonsenso D. Routine use of Point-of-Care lung ultrasound during the COVID-19 pandemic. Med Intensiva. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 73. | Kooraki S, Hosseiny M, Myers L, Gholamrezanezhad A. Coronavirus (COVID-19) Outbreak: What the Department of Radiology Should Know. J Am Coll Radiol. 2020;17:447-451. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 272] [Cited by in RCA: 280] [Article Influence: 56.0] [Reference Citation Analysis (0)] |
| 74. | Kok SSX, Mohamed Shah MTB, Cheong WK, Cheng AKC, Sng LH, Salkade PR, Wong SBS. Dealing with COVID-19: initial perspectives of a small radiology department. Singapore Med J. 2020;61:375-377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 75. | Ding J, Fu H, Liu Y, Gao J, Li Z, Zhao X, Zheng J, Sun W, Ni H, Ma X, Feng J, Wu A, Liu J, Wang Y, Geng P, Chen Y. Prevention and control measures in radiology department for COVID-19. Eur Radiol. 2020;30:3603-3608. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 31] [Article Influence: 6.2] [Reference Citation Analysis (0)] |