Published online Sep 28, 2020. doi: 10.4329/wjr.v12.i9.195
Peer-review started: June 24, 2020
First decision: July 30, 2020
Revised: August 22, 2020
Accepted: September 25, 2020
Article in press: September 25, 2020
Published online: September 28, 2020
Processing time: 95 Days and 23.8 Hours
As healthcare professionals continue to combat the coronavirus disease 2019 (COVID-19) infection worldwide, there is an increasing interest in the role of imaging and the relevance of various modalities. Since imaging not only helps assess the disease at the time of diagnosis but also aids evaluation of response to management, it is critical to examine the role of different modalities currently in use, such as baseline X-rays and computed tomography scans carefully. In this article, we will draw attention to the critical findings for the radiologist. Further, we will look at point of care ultrasound, an increasingly a popular tool in diagnostic medicine, as a component of COVID-19 management.
Core Tip: As the current coronavirus disease 2019 pandemic continues to spread and burden the healthcare system all over the world, we must explore all the resources at our disposal to give our patients the best care possible. While laboratory tests and computed tomography imaging are sensitive methods for diagnosis, the increasing burden of disease requires us to effectively utilize bedside ultrasonography to care for more people in a quick and judicious manner. Further, we must continuously look for ways to improve our efficiency while preventing spread of infection within the hospital.
- Citation: Gandhi D, Ahuja K, Grover H, Sharma P, Solanki S, Gupta N, Patel L. Review of X-ray and computed tomography scan findings with a promising role of point of care ultrasound in COVID-19 pandemic. World J Radiol 2020; 12(9): 195-203
- URL: https://www.wjgnet.com/1949-8470/full/v12/i9/195.htm
- DOI: https://dx.doi.org/10.4329/wjr.v12.i9.195
Diagnostic radiology is an integral component in assessing the initial extent and severity of several diseases, including the current coronavirus disease 2019 (COVID-19) infection, and directs the management as well[1]. Further, it provides a baseline with which to track changes, including progression and subsequent resolution of disease[1,2]. In the COVID-19 pandemic, with the high level of infectivity of this virus, and an early non-specific or even asymptomatic phase, imaging may play a crucial role in early diagnosis, timely treatment, as well as a follow-up[1,2]. While the role of imaging is helpful in assessing the phase and severity of the disease, as well as demonstrating resolution, its importance in early detection is debatable[3,4]. On one hand, Ai et al[3] studied 1014 patients in Wuhan, China and concluded that the high sensitivity of chest computed tomography (CT) imaging in detecting COVID-19 infection might make it a suitable tool for screening purposes. They advise that a high pre-test probability would further increase the suitability of this modality[3]. On the other hand, Yang et al[4] draw attention to the evidence demonstrating the possibility of confirmed COVID-19 infection with no significant chest CT findings. Further, chest CT findings, previously considered a part of the diagnostic criteria, have been removed in later guidelines[4]. At present, with the large number of people affected, the burden on healthcare imaging facilities is immense, generating interest in simpler, faster, and less expensive methods of diagnosis, such as ultrasonography[5,6]. With Point of care ultrasound becoming increasingly essential to modern medicine, the possibilities of using it as a reliable, safe, and quick diagnostic tool are being explored[6]. A study demonstrated a strong positive correlation between the findings on ultrasound and CT scans of twelve COVID-19 patients[5]. With the advantage of portability and lower expense as compared to Computed tomography, the ultrasound definitely seems like an avenue worth exploring[7].
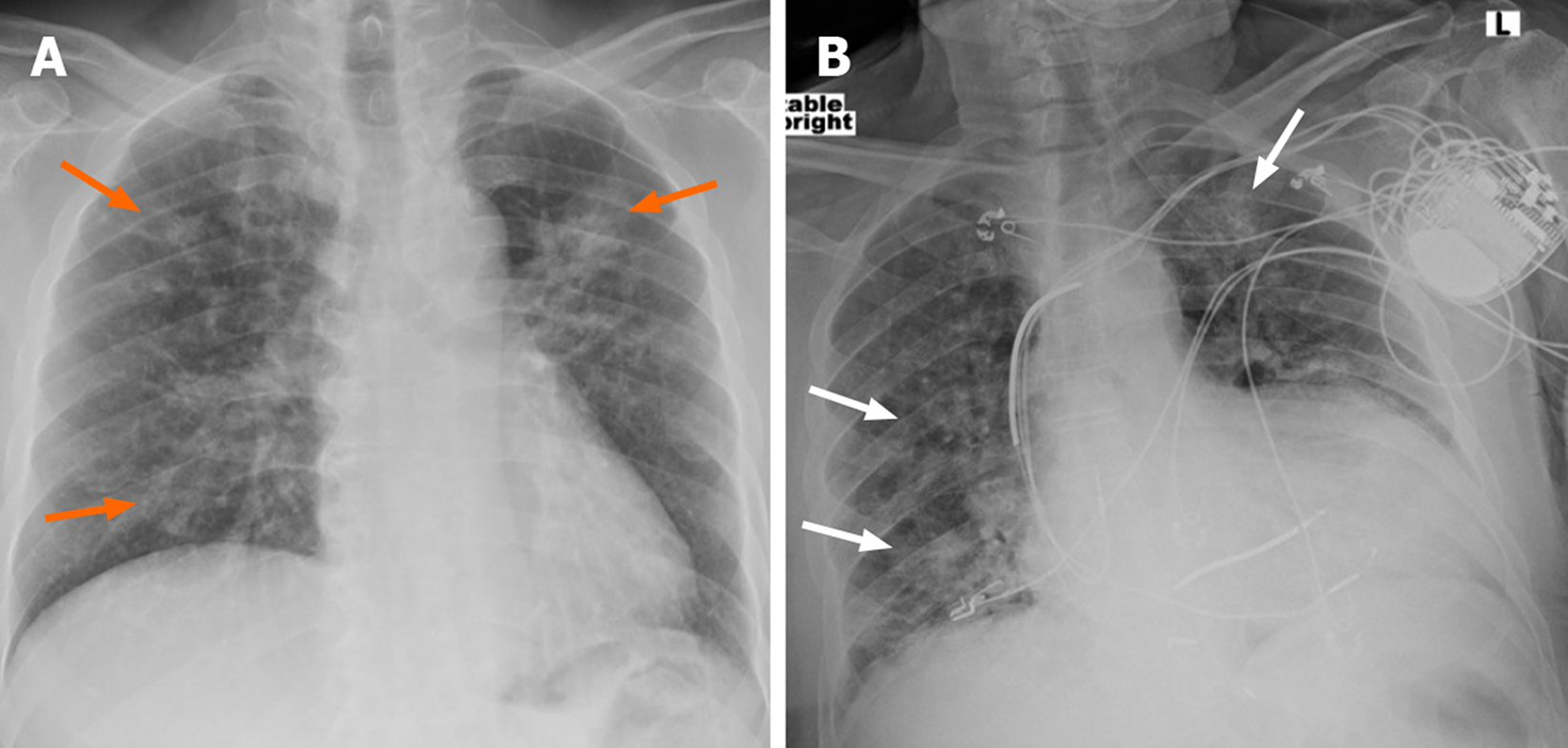
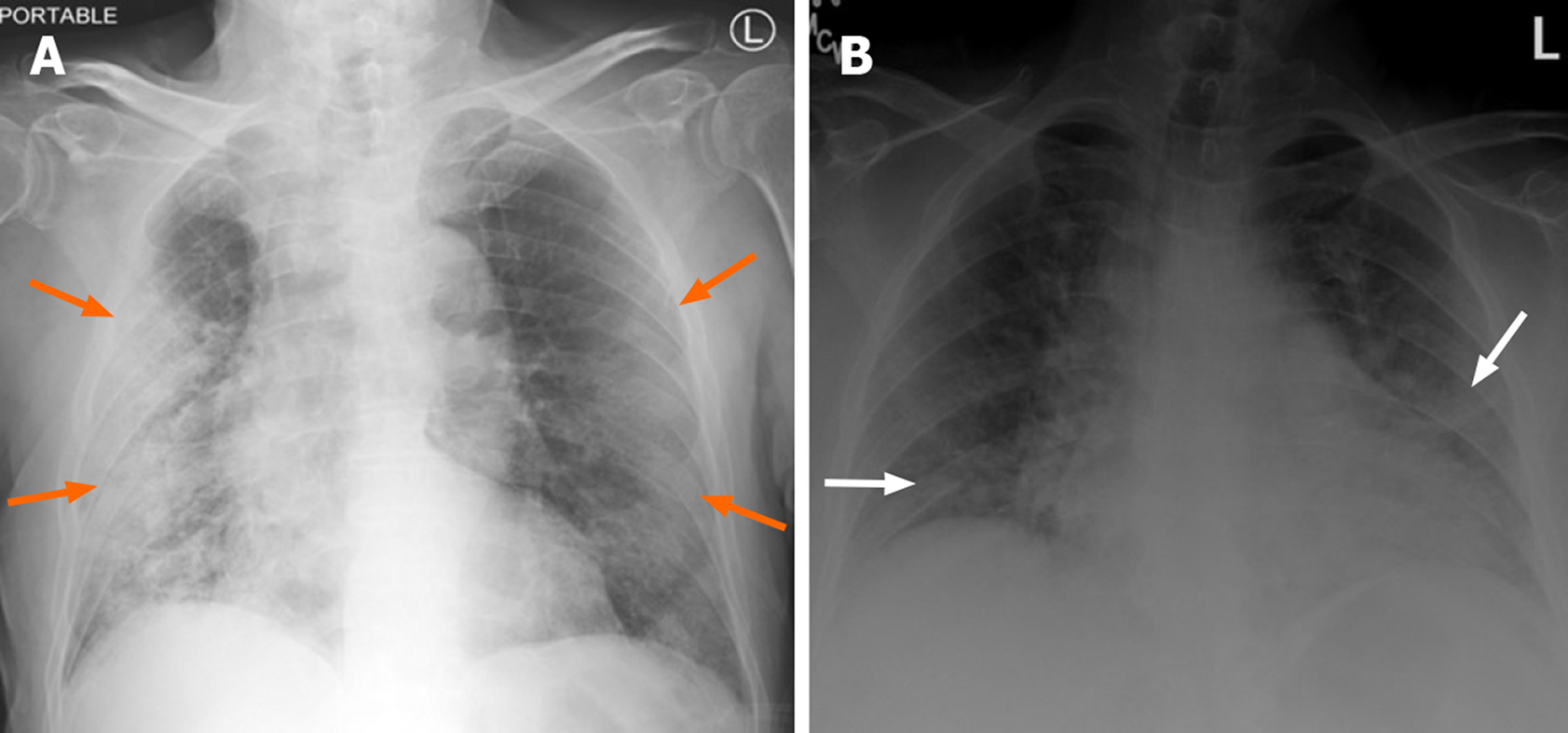
Chest radiography is not advisable for first line use for detection of COVID-19 infection due to a reduced ability to demonstrate ground-glass opacities, an early finding in this disease (Figure 1)[1]. As the disease progresses, however, extensive consolidation may develop, which may be seen on chest radiographs as well and thus helpful to assess the disease progression or resolution during management (Figure 2)[1]. Recently, however, Cellina et al[8] retrospectively studied the initial chest radiographs of 246 confirmed COVID-19 patients to determine a correlation, if any, with mild outcomes. For the purpose of their study, they consider a mild outcome to be hospitalization for 0-3 d, not requiring assisted ventilation[8]. Interestingly, they found statistically significant results for an inverse relationship between chest radiograph findings of ground glass opacification and severity scores ≥ 3 with a mild outcome[8]. Therefore, chest radiographs might be reliable in predicting outcomes, particularly in limited-resource settings and high caseload settings[8].
Further, chest radiography may be used for serial imaging to follow the course of disease in patients during their stay in the hospital and assess the effectiveness of treatment as well[9].
Chest CT imaging can demonstrate ground-glass opacities and consolidation early on, even in the absence of significant chest X-ray findings, and is, therefore, believed to have a higher sensitivity for COVID-19 detection[1,10]. Further, the use of chest CT imaging to meet the increased demand for testing has been considered by some[10,11]. Ng et al[10] studied non-contrast chest CT images of 21 COVID-19 patients and reported the most commonly observed finding to be peripheral ground-glass opacification.
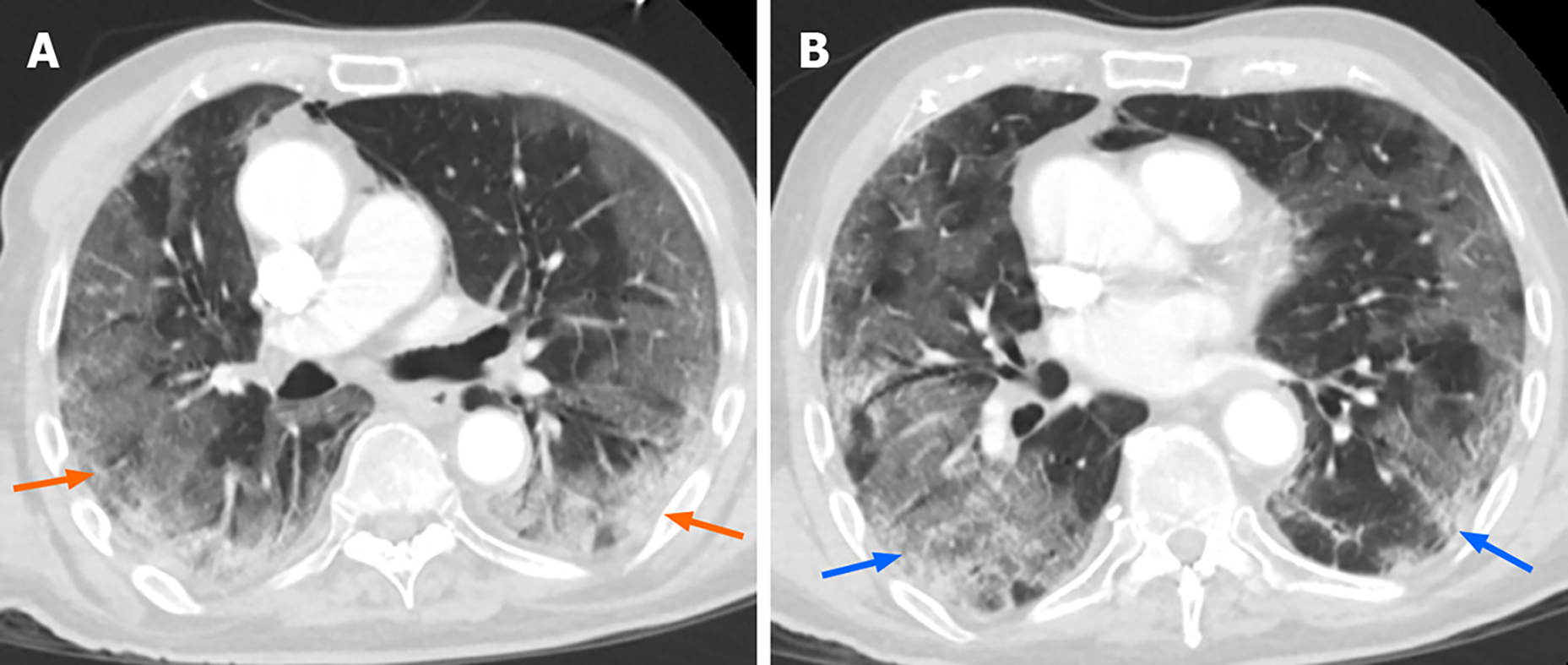
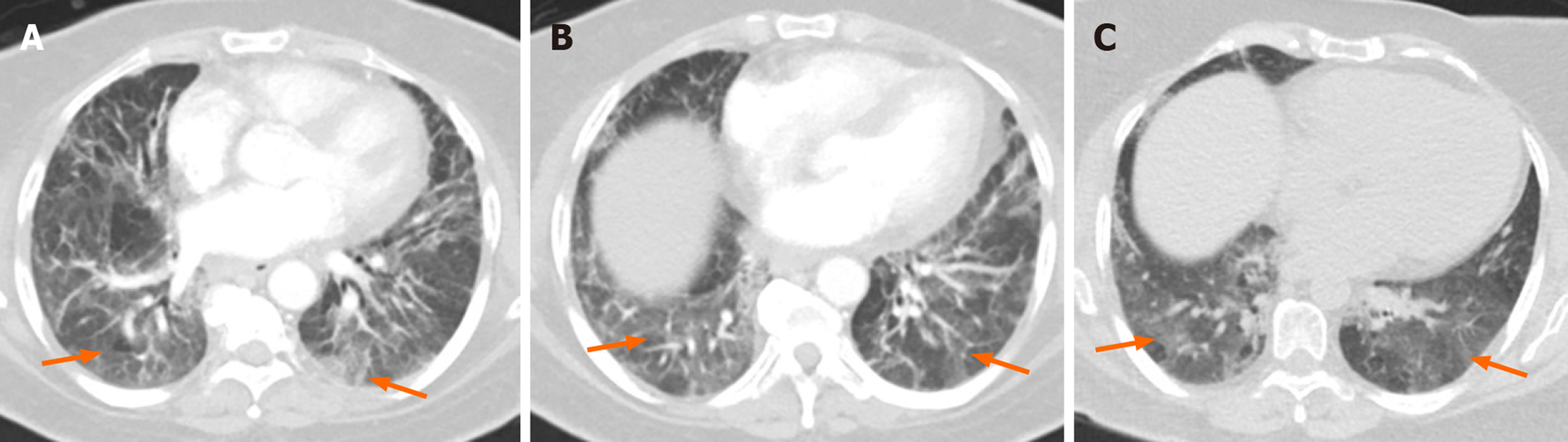
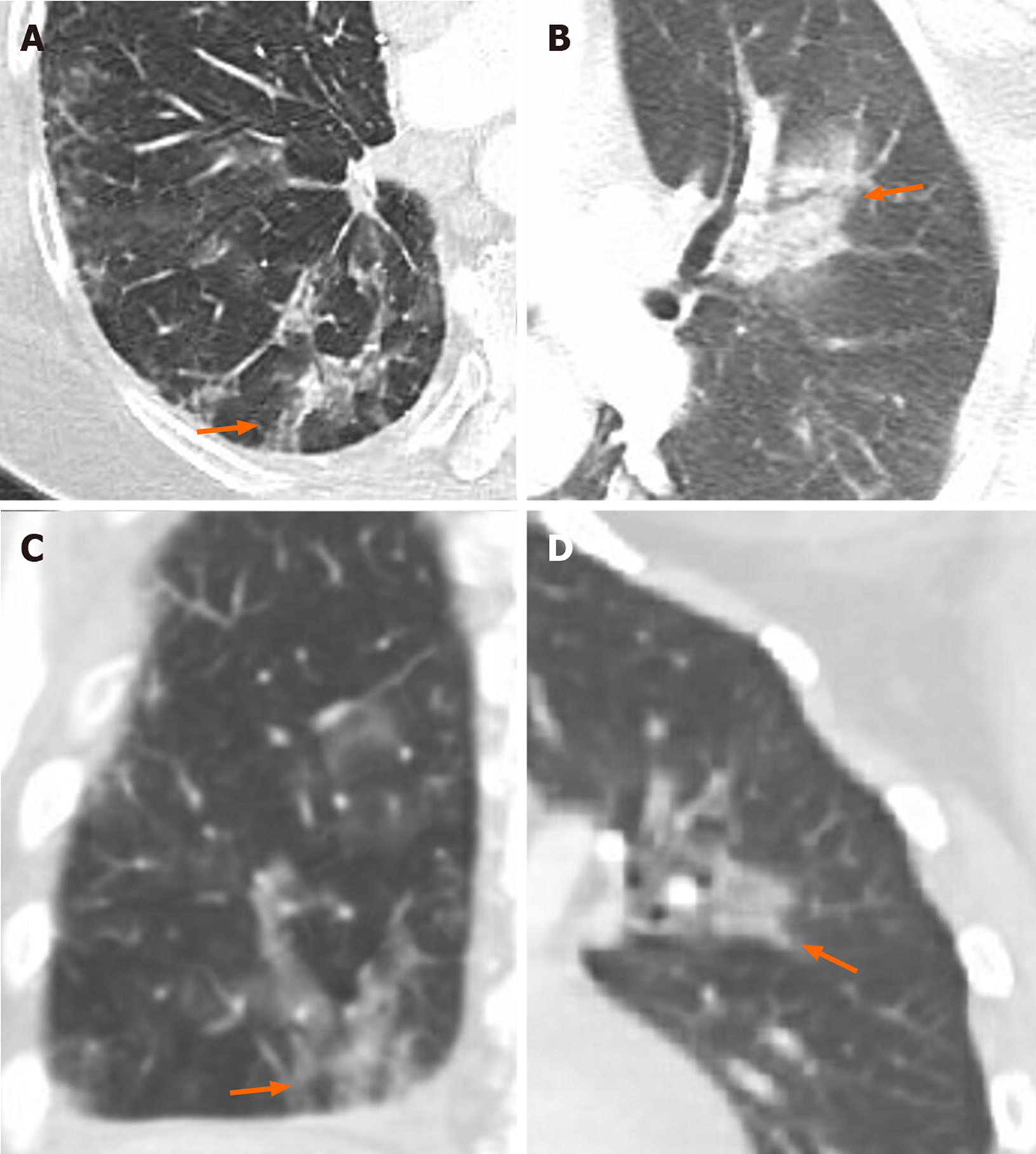
Early disease, as observed reliably on thin-slice CT, is characterized by peripheral ground-glass opacities with a bilateral distribution, which may or may not be accompanied by consolidation[11]. This infection has a predilection for the posterior aspects and lower lobes of the lungs[11]. Further, an early study of imaging patterns indicated that ICU patients were more likely to have consolidation than non-ICU patients[12]. Consolidation usually appears as the disease progresses and is significantly higher in patients over the age of 50 than those aged 50 or below, which is in keeping with the poorer prognosis observed in the elderly[13,14]. The full spectrum of chest CT findings observed in COVID-19 disease includes ground-glass opacification (pure, with crazy-paving, or with accompanying consolidation), pure consolidation, air bronchograms, pleural effusions, lymphadenopathy (Figures 3, 4 and 5)[13,14]. However, pleural effusion, lymphadenopathy, and cavitation are not common findings[12].
Crazy paving pattern, mentioned above, is a non-specific, thin-slice chest CT finding, which is commonly observed as COVID-19 disease progresses, when intralobular lines and thickening of inter-lobular septa occur in combination with ground glass opacification (Figure 3)[13,15]. Further, there have been occasional reports of interesting signs on Computed tomography imaging, such as, Halo sign (nodule with a halo of ground-glass opacification) and reverse-halo (ground-glass attenuation with halo of consolidation)[16,17,18]. Follow-up of COVID-19 patients with computed tomography also demonstrate a decrease in the size of lesions over time, and the resolution of pure consolidative lesions into organizing pneumonia[14].
Yang et al[11] developed an objective chest CT severity score (ranging from 0 to 40) and determined the disease to be “severe” for a score ≥ 19.5. Further, the changes observed in imaging as the disease progresses and resolves have helped provide us with a better idea of the patient’s condition[19]. Based on the imaging conducted over the course of 26 d, Pan[19] et al simplified the chest CT findings observed, from the onset of symptoms, into 4 stages, as described in the Table 1.
| Days (from onset of symptoms) | Stage | Typical findings |
| 0-4 | Early | GGO; Distribution: Unilateral/bilateral, lower lobes, peripheral |
| 5-8 | Progressive | GGO (diffuse); Crazy paving; Consolidation; Distribution: Bilateral, multilobar |
| 9-13 | Peak | Peak CT findings: day 10; GGO (diffuse); Crazy paving; Consolidation (dense); Parenchymal bands |
| ≥ 14 | Absorption | CT findings improve from day 14; Absorption of consolidation; GGO present; No crazy paving |
Wang et al[20] studied the non-contrast chest CT findings in 90 patients over the course of one month and observed similar findings, when categorized according to days from symptom onset. Days 0 through 5 were characterized by pure ground-glass opacities, crazy-paving, and consolidation, with 14% of chest CT scans during this time appearing normal[20]. Days 6 to 11 saw a peak in imaging findings and the development of irregular lines[20]. Further, Wang et al[20] highlight the initial decline of pure ground-glass opacities (while other imaging findings increase). This was followed by a gradual increase of pure ground-glass opacities during resolution of disease, perhaps due to the decline of the other imaging findings at this time.
Further, the relevance of chest CT imaging during the ongoing pandemic has been demonstrated by reports of RT-PCR negative patients demonstrating significant imaging findings to be confirmed later as COVID-19 patients[21,22,23]. Therefore, in a scenario where RT-PCR test yields negative results, but patient history and CT findings are concerning for COVID-19 infection, it is important to repeat the RT-PCR test to be thorough[24].
Dangis et al[25] studied the utility of low dose submillisievert computed tomography in nearly 200 patients and found a high degree of sensitivity and specificity associated with this method. The sensitivity increased by roughly 9% when patients reported symptoms for over 48 h[25]. Further, the likelihood of having COVID-19 infection was found to be over 90% in the case of positive imaging findings[25]. Also, it helped identify a co-existing illness in COVID-19 patients and provide differential diagnoses in non-COVID patients[25].
Despite the advantages of chest CT imaging in COVID-19, health care professionals must realize that it may not always yield significant findings at the time of symptom onset[4]. Bernheim et al[17] reported that 0 to 2 d from onset of symptoms, chest CT scans revealed no significant findings in 20 of the 36 patients they studied. Given the high level of infectivity associated with COVID-19, it is imperative that health care professionals remain alert to suspicious symptoms, particularly in the context of relevant history, regardless of imaging results. Volume rendered chest CT imaging has been successfully utilized in COVID-19 patients to delineate disease, demonstrate newly developed lesions and ascertain their distribution[22,26].
With increasing awareness of hypercoagulability as a component of COVID-19 disease, pulmonary CT angiography is a relevant imaging modality in these patients. In a recent study, Poyiadi et al[27] studied COVID-19 patients who underwent pulmonary CT angiography, found pulmonary embolism in roughly one-fifth of these patients.
Point of care ultrasonography (POCUS) provides a quick and safe method for imaging and procedural guidance, making it an indispensable tool for optimal care of the patient[28]. Being an operator dependent imaging modality, it has become an important aspect of the physician’s training over the years[28].
In the ongoing COVID-19 pandemic, the healthcare system must keep pace with the increasing patient load, while managing costs and preventing transmission of infection within the hospital.
As described previously, chest CT imaging helps detect findings of COVID-19 early and accurately. However, it usually requires patient transportation to radiology department and is more expensive. While POCUS may not provide as detailed a picture or as early as computed tomography does, it can be quickly performed at bedside, is an effective tool in experienced hands in diagnosis of lung infection and useful in patients who cannot accept CT examination e.g. pregnant patients.
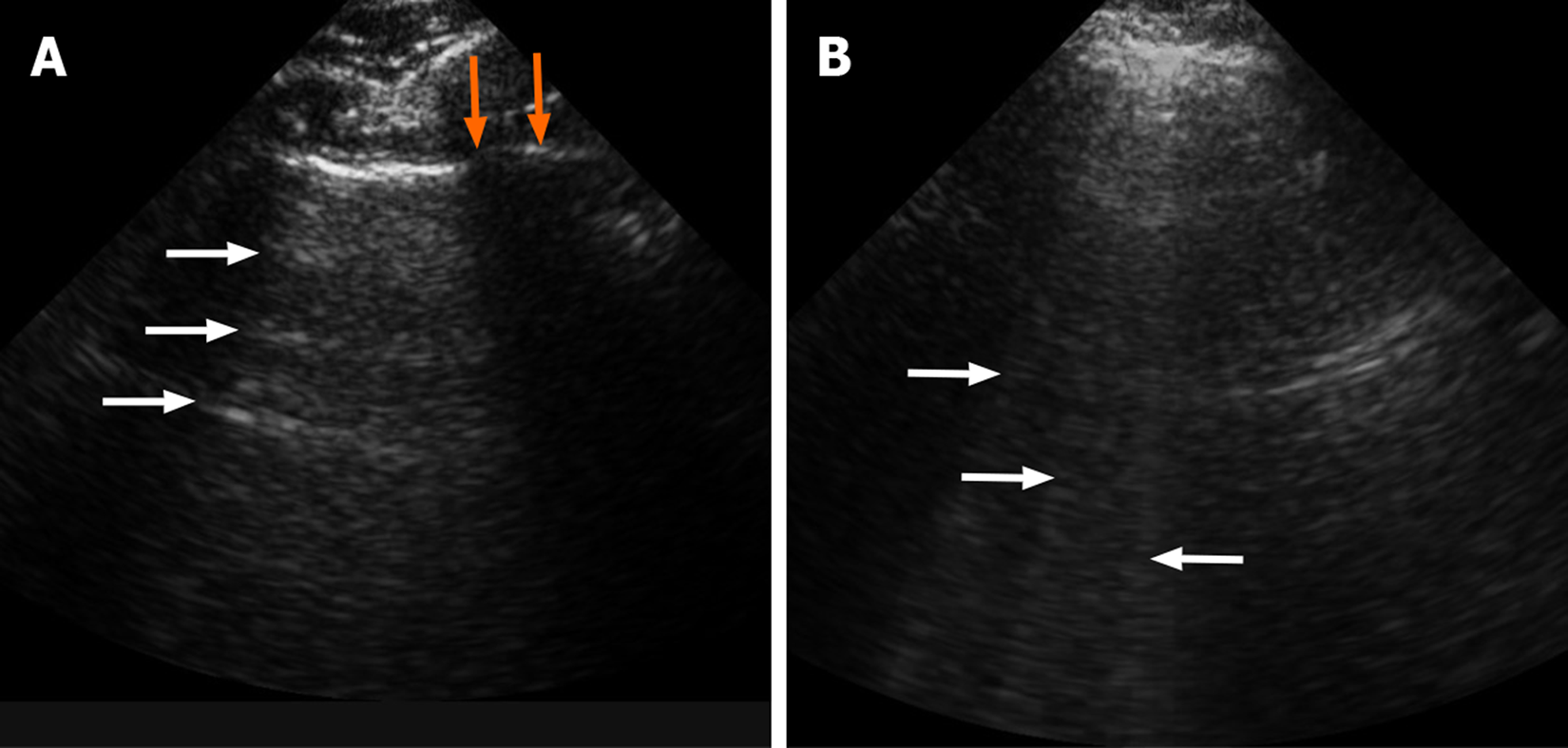
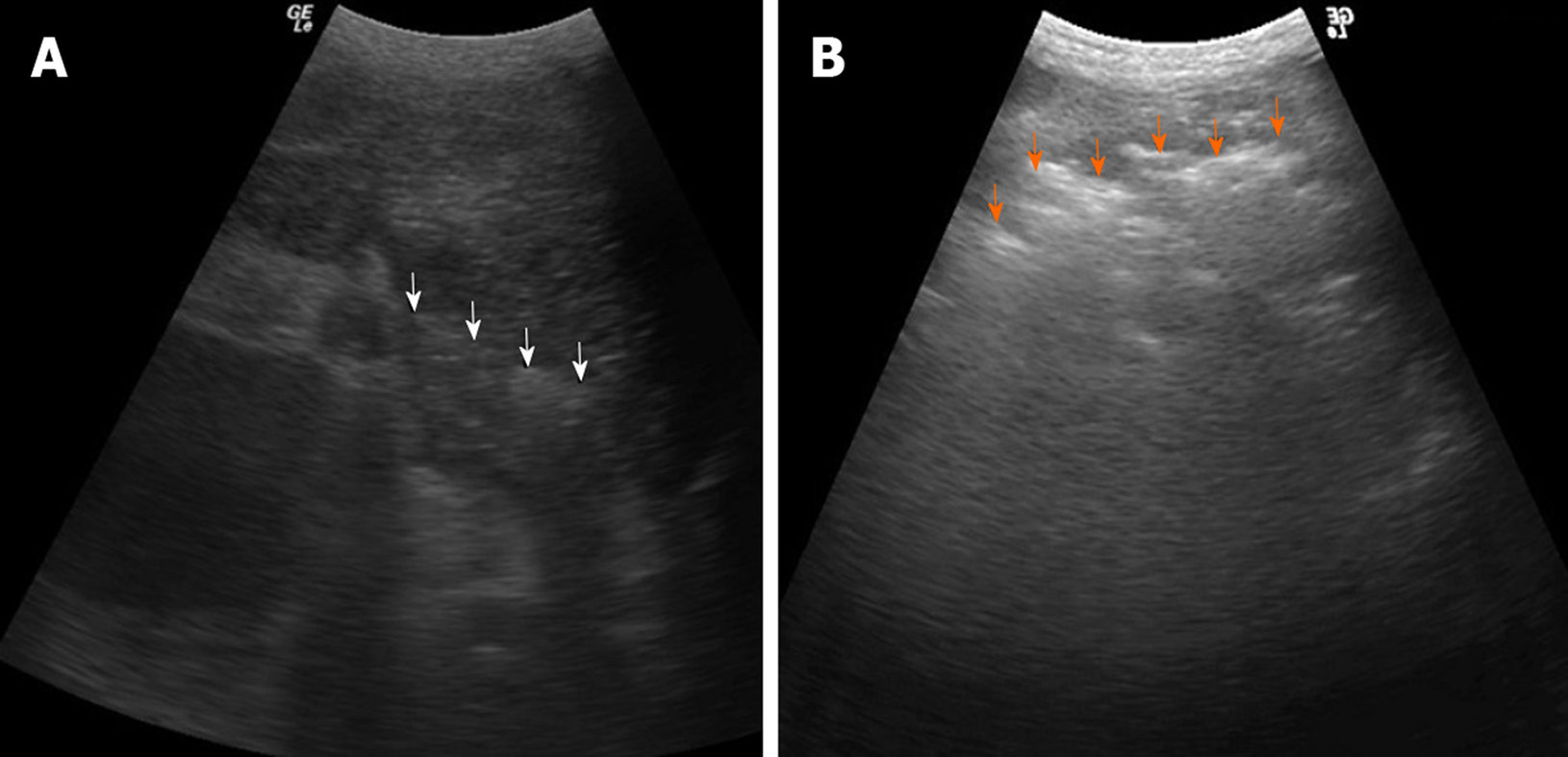
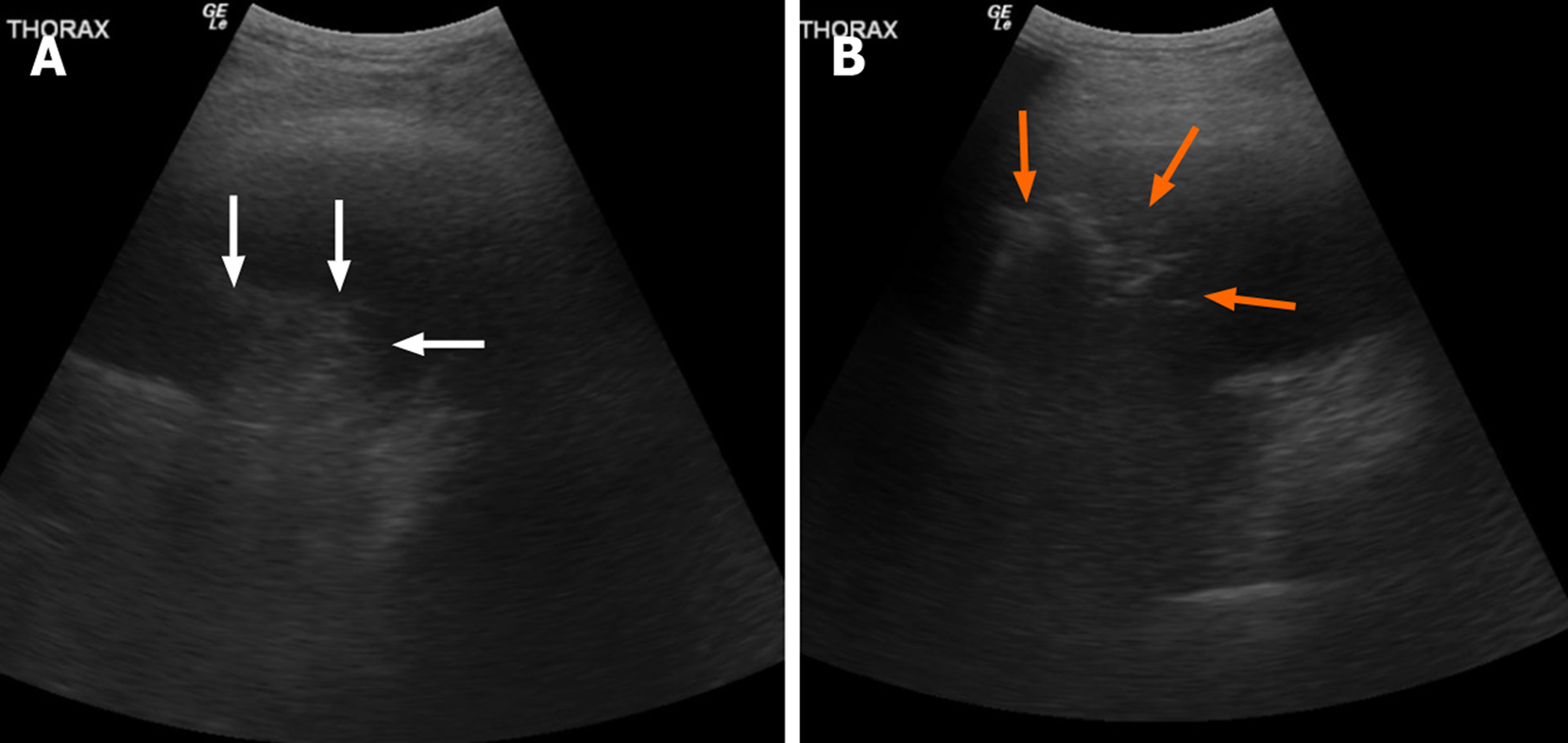
Lung ultrasound helps examine the superficial lung, with normal lung demonstrating horizontal artifacts or “A” lines[6]. The disease of the subpleural portion of lung results in heterogeneous, vertical “B” lines (Figure 6)[6]. Apart from that various other artifacts including C, E, and Z lines are described. As the consolidation develops, echogenicity of the lung becomes closer to the liver and also additional static and dynamic changes in bronchi. The use of lung ultrasound is very well described and widely used in the evaluation of patients with dyspnea especially in intensive care units[29]. Shredded appearance at the interface of the consolidated and normally aerated lung is known as the “Shred sign”, which is considered to be the most specific sign of pneumonia in lung ultrasound study (Figure 7)[29]. The increased echogenicity of the consolidated lung parenchyma shows appearance similar to liver parenchyma, known as “hepatic pattern” or “tissue pattern”, another sign of pneumonia (Figure 8)[30].
Sobh et al[30] studied 55 suspected pneumonia patients and reported that ultrasonography is superior to radiography for the purpose of detecting pneumonia. Further, its sensitivity and accuracy relative to chest CT imaging were 100% and 98.2% respectively. Similarly, a meta-analysis comprising over 1500 patients revealed the area under the curve for lung ultrasound to be 0.95, demonstrating a high level of accuracy as a diagnostic tool for pneumonia[31].
POCUS may help define severity and progression of COVID-19. The early ultrasound findings seen in COVID-19 patients demonstrate patchy interstitial involvement in the forms of vertical lines and white lung areas[6]. As the disease progresses, more lung surface is involved, with subsequent development of consolidation[6]. Further increase in consolidation particularly in the posterobasal lung is concerning for advanced disease and may predict the need for invasive ventilation[6]. Huang et al[32] studied lung ultrasound findings in 20 non-critical, confirmed COVID-19 patients. Primarily posteriorly located, the lesions included B-lines, patchy consolidation (subpleural) with reduced blood flow, air bronchograms, disrupted pleural lines, thickened pleura, among other findings[32].
Peng et al[33] also studied 20 COVID-19 patients and reported a correlation between lung ultrasound findings with the degree of involvement, making it useful for disease severity and disease progression assessment. Lung ultrasound may also be useful in understanding which lesions are recruitable, allowing for thorough management of severe COVID-19 infection with relevant maneuvers and change of PEEP[34].
POCUS has also been shown to be very useful in rapid cardiac evaluation[35]. It allows evaluation of the pericardial effusion, detects low ejection fraction and IVC measurements. COVID-19 has shown to involve heart as well and has shown to cause myocarditis, pericarditis, and congestive heart failure with or without reduced ejection fraction[36,37]. Though pericardial effusion is not common it has been reported due to COVID-19 and rapid diagnosis can avoid serious consequences[38]. COVID-19 has also shown an increased risk of venous thromboembolism and POCUS can help in the periodic vascular evaluation of early detection of venous thrombosis in experienced hands[39,40]. This added utility is also key in defining the role of POCUS in the current pandemic.
Some hypothetic examples of the role of POCUS in current pandemic would be pregnant woman hospitalized for preeclampsia develops cough and dyspnea, POCUS can help detect lung parenchyma while waiting for RT-PCR and make appropriate isolation and treatment decisions or patient with COVID develop chest discomfort, identification of pericardial effusion with POCUS can help rapid diagnosis of pericarditis in a smaller hospital where rapid echocardiography or cardiology consultation is not available.
Given the high infectivity of COVID-19, and its spread all over the world, it is imperative for healthcare professionals to follow the correct method of cleaning the ultrasound machines to prevent the spread within the hospital[7,41].
To this end, the following guidelines have been found to be useful[7,41]: (1) Clear the basket of all non-essential items, and thoroughly wipe every surface of the machine before entering the patient’s room; (2) Replace gel bottles with single-use gel sachets; (3) After performing the ultrasonography, sanitize gloves and then remove any body tissue or fluid present on the machine, using the approved wet wipes; (4) Next, wipe the entire machine (including but not limited to the power cord, probes, screen, keyboard, knobs, wells, wipe containers); (5) Take the machine out of the room while it is still wet; (6) Once outside the room, examine the machine once more for any body tissue or fluids and remove with wipes if observed; (7) Next, wipe the entire machine again; (8) Always use approved wipes and adhere to the “wet time” specific to the type of wipe; and (9) Always remember to wipe the wipes container.
As the current COVID-19 pandemic continues to spread and burden the healthcare system all over the world, we must explore all the resources at our disposal to give our patients the best care possible. While laboratory tests and computed tomography imaging are sensitive methods for diagnosis, the increasing burden of disease requires us to effectively utilize bedside ultrasonography to care for more people in a quick and judicious manner. Further, we must continuously look for ways to improve our efficiency while preventing the spread of infection within the hospital.
Manuscript source: Invited manuscript
Specialty type: Radiology, nuclear medicine and medical imaging
Country/Territory of origin: United States
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Chen P, Zhang HW S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Zu ZY, Jiang MD, Xu PP, Chen W, Ni QQ, Lu GM, Zhang LJ. Coronavirus Disease 2019 (COVID-19): A Perspective from China. Radiology. 2020;296:E15-E25. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1106] [Cited by in RCA: 952] [Article Influence: 190.4] [Reference Citation Analysis (1)] |
| 2. | Kanne JP, Little BP, Chung JH, Elicker BM, Ketai LH. Essentials for Radiologists on COVID-19: An Update-Radiology Scientific Expert Panel. Radiology. 2020;296:E113-E114. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 367] [Cited by in RCA: 421] [Article Influence: 84.2] [Reference Citation Analysis (0)] |
| 3. | Ai T, Yang Z, Hou H, Zhan C, Chen C, Lv W, Tao Q, Sun Z, Xia L. Correlation of Chest CT and RT-PCR Testing for Coronavirus Disease 2019 (COVID-19) in China: A Report of 1014 Cases. Radiology. 2020;296:E32-E40. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3614] [Cited by in RCA: 3284] [Article Influence: 656.8] [Reference Citation Analysis (0)] |
| 4. | Yang W, Yan F. Patients with RT-PCR-confirmed COVID-19 and Normal Chest CT. Radiology. 2020;295:E3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 104] [Cited by in RCA: 110] [Article Influence: 22.0] [Reference Citation Analysis (0)] |
| 5. | Poggiali E, Dacrema A, Bastoni D, Tinelli V, Demichele E, Mateo Ramos P, Marcianò T, Silva M, Vercelli A, Magnacavallo A. Can Lung US Help Critical Care Clinicians in the Early Diagnosis of Novel Coronavirus (COVID-19) Pneumonia? Radiology. 2020;295:E6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 203] [Cited by in RCA: 207] [Article Influence: 41.4] [Reference Citation Analysis (0)] |
| 6. | Soldati G, Smargiassi A, Inchingolo R, Buonsenso D, Perrone T, Briganti DF, Perlini S, Torri E, Mariani A, Mossolani EE, Tursi F, Mento F, Demi L. Is There a Role for Lung Ultrasound During the COVID-19 Pandemic? J Ultrasound Med. 2020;39:1459-1462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 298] [Cited by in RCA: 311] [Article Influence: 62.2] [Reference Citation Analysis (0)] |
| 7. | McDermott C. Combatting COVID19 – Is Lung Ultrasound an Option? Available from: https://www.stemlynsblog.org/combatting-covid19-is-lung-ultrasound-an-option/. |
| 8. | Cellina M, Panzeri M, Oliva G. Chest Radiograph Features Predict a Favorable Outcome in Patients with COVID-19. Radiology. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 9. | Bhat R, Hamid A, Kunin JR, Saboo SS, Batra K, Baruah D, Bhat AP. Chest Imaging in Patients Hospitalized With COVID-19 Infection - A Case Series. Curr Probl Diagn Radiol. 2020;49:294-301. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 10. | Ng MY, Lee EYP, Yang J, Yang F, Li X, Wang H, Lui MMS, Lo CSY, Leung B, Khong PL, Hui CKM, Yuen KY, Kuo MD. Imaging Profile of the COVID-19 Infection: Radiologic Findings and Literature Review. Radiol Cardiothorac Imaging. 2020;2:e200034. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 604] [Cited by in RCA: 474] [Article Influence: 94.8] [Reference Citation Analysis (0)] |
| 11. | Yang R, Li X, Liu H, Zhen YL, Zeng WB. Chest CT Severity Score: An Imaging Tool for Assessing Severe COVID-19. Radiol Cardiothorac Imaging. 2020;2:e200047. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 344] [Cited by in RCA: 345] [Article Influence: 69.0] [Reference Citation Analysis (0)] |
| 12. | Hosseiny M, Kooraki S, Gholamrezanezhad A, Reddy S, Myers L. Radiology Perspective of Coronavirus Disease 2019 (COVID-19): Lessons From Severe Acute Respiratory Syndrome and Middle East Respiratory Syndrome. AJR Am J Roentgenol. 2020;214:1078-1082. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 257] [Cited by in RCA: 266] [Article Influence: 53.2] [Reference Citation Analysis (0)] |
| 13. | Li B, Li X, Wang Y, Han Y, Wang Y, Wang C, Zhang G, Jin J, Jia H, Fan F, Ma W, Liu H, Zhou Y. Diagnostic value and key features of computed tomography in Coronavirus Disease 2019. Emerg Microbes Infect. 2020;9:787-793. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 70] [Cited by in RCA: 74] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 14. | Song F, Shi N, Shan F, Zhang Z, Shen J, Lu H, Ling Y, Jiang Y, Shi Y. Emerging 2019 Novel Coronavirus (2019-nCoV) Pneumonia. Radiology. 2020;295:210-217. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 903] [Cited by in RCA: 784] [Article Influence: 156.8] [Reference Citation Analysis (0)] |
| 15. | Rossi SE, Erasmus JJ, Volpacchio M, Franquet T, Castiglioni T, McAdams HP. "Crazy-paving" pattern at thin-section CT of the lungs: radiologic-pathologic overview. Radiographics. 2003;23:1509-1519. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 206] [Cited by in RCA: 190] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 16. | Li X, Zeng X, Liu B, Yu Y. COVID-19 Infection Presenting with CT Halo Sign. Radiol Cardiothorac Imaging. 2020;2:e200026. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 71] [Cited by in RCA: 69] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 17. | Bernheim A, Mei X, Huang M, Yang Y, Fayad ZA, Zhang N, Diao K, Lin B, Zhu X, Li K, Li S, Shan H, Jacobi A, Chung M. Chest CT Findings in Coronavirus Disease-19 (COVID-19): Relationship to Duration of Infection. Radiology. 2020;295:200463. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1728] [Cited by in RCA: 1596] [Article Influence: 319.2] [Reference Citation Analysis (1)] |
| 18. | Farias LPG, Strabelli DG, Sawamura MVY. COVID-19 pneumonia and the reversed halo sign. J Bras Pneumol. 2020;46:e20200131. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 19. | Pan F, Ye T, Sun P, Gui S, Liang B, Li L, Zheng D, Wang J, Hesketh RL, Yang L, Zheng C. Time Course of Lung Changes at Chest CT during Recovery from Coronavirus Disease 2019 (COVID-19). Radiology. 2020;295:715-721. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1617] [Cited by in RCA: 1760] [Article Influence: 352.0] [Reference Citation Analysis (0)] |
| 20. | Wang Y, Dong C, Hu Y, Li C, Ren Q, Zhang X, Shi H, Zhou M. Temporal Changes of CT Findings in 90 Patients with COVID-19 Pneumonia: A Longitudinal Study. Radiology. 2020;296:E55-E64. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 493] [Cited by in RCA: 591] [Article Influence: 118.2] [Reference Citation Analysis (0)] |
| 21. | Salehi S, Abedi A, Balakrishnan S, Gholamrezanezhad A. Coronavirus Disease 2019 (COVID-19): A Systematic Review of Imaging Findings in 919 Patients. AJR Am J Roentgenol. 2020;215:87-93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 769] [Cited by in RCA: 860] [Article Influence: 172.0] [Reference Citation Analysis (0)] |
| 22. | Huang P, Liu T, Huang L, Liu H, Lei M, Xu W, Hu X, Chen J, Liu B. Use of Chest CT in Combination with Negative RT-PCR Assay for the 2019 Novel Coronavirus but High Clinical Suspicion. Radiology. 2020;295:22-23. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 313] [Cited by in RCA: 324] [Article Influence: 64.8] [Reference Citation Analysis (0)] |
| 23. | Xie X, Zhong Z, Zhao W, Zheng C, Wang F, Liu J. Chest CT for Typical Coronavirus Disease 2019 (COVID-19) Pneumonia: Relationship to Negative RT-PCR Testing. Radiology. 2020;296:E41-E45. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1213] [Cited by in RCA: 1211] [Article Influence: 242.2] [Reference Citation Analysis (1)] |
| 24. | Koo HJ, Choi SH, Sung H, Choe J, Do KH. RadioGraphics Update: Radiographic and CT Features of Viral Pneumonia. Radiographics. 2020;40:E8-E15. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 23] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 25. | Dangis A, Gieraerts C, Bruecker YD, Janssen L, Valgaeren H, Obbels D, Gillis M, Ranst MV, Frans J, Demeyere A, Symons R. Accuracy and reproducibility of low-dose submillisievert chest CT for the diagnosis of COVID-19. Radiol Cardiothorac Imaging. 2020;2:e200196. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 79] [Cited by in RCA: 80] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 26. | Tang L, Zhang X, Wang Y, Zeng X. Severe COVID-19 Pneumonia: Assessing Inflammation Burden with Volume-rendered Chest CT. Radiol Cardiothorac Imaging. 2020;2:e200044. [RCA] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 27. | Poyiadji N, Cormier P, Patel PY, Hadied MO, Bhargava P, Khanna K, Nadig J, Keimig T, Spizarny D, Reeser N, Klochko C, Peterson EL, Song T. Acute Pulmonary Embolism and COVID-19. Radiology. 2020;Online ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 158] [Cited by in RCA: 165] [Article Influence: 33.0] [Reference Citation Analysis (0)] |
| 28. | Bhagra A, Tierney DM, Sekiguchi H, Soni NJ. Point-of-Care Ultrasonography for Primary Care Physicians and General Internists. Mayo Clin Proc. 2016;91:1811-1827. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 156] [Article Influence: 17.3] [Reference Citation Analysis (0)] |
| 29. | Lichtenstein DA, Mezière GA. Relevance of lung ultrasound in the diagnosis of acute respiratory failure: the BLUE protocol. Chest. 2008;134:117-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1152] [Cited by in RCA: 1192] [Article Influence: 70.1] [Reference Citation Analysis (0)] |
| 30. | Sobh E, Oraby S, Gamal F. Role of thoracic ultrasound in the diagnosis of pneumonia. Eur Res J. 2017;50:PA4113. [DOI] [Full Text] |
| 31. | Long L, Zhao HT, Zhang ZY, Wang GY, Zhao HL. Lung ultrasound for the diagnosis of pneumonia in adults: A meta-analysis. Medicine (Baltimore). 2017;96:e5713. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 84] [Cited by in RCA: 109] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 32. | Huang Y, Wang S, Liu Y, Zhang YH, Zheng CY, Zheng Y, Zhang CY, Min WL, Zhou HH, Yu M, Hu MJ. A Preliminary Study on the Ultrasonic Manifestations of Peripulmonary Lesions of Non-Critical Novel Coronavirus Pneumonia (COVID-19). SSRN J. 2020;. [RCA] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 84] [Reference Citation Analysis (0)] |
| 33. | Peng QY, Wang XT, Zhang LN; Chinese Critical Care Ultrasound Study Group (CCUSG). Findings of lung ultrasonography of novel corona virus pneumonia during the 2019-2020 epidemic. Intensive Care Med. 2020;46:849-850. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 469] [Cited by in RCA: 509] [Article Influence: 101.8] [Reference Citation Analysis (1)] |
| 34. | Schultz MJ, Sivakorn C, Dondorp AM. Challenges and Opportunities for Lung Ultrasound in Novel Coronavirus Disease (COVID-19). Am J Trop Med Hyg. 2020;102:1162-1163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 35. | Kimura BJ. Point-of-care cardiac ultrasound techniques in the physical examination: better at the bedside. Heart. 2017;103:987-994. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 72] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 36. | Inciardi RM, Lupi L, Zaccone G, Italia L, Raffo M, Tomasoni D, Cani DS, Cerini M, Farina D, Gavazzi E, Maroldi R, Adamo M, Ammirati E, Sinagra G, Lombardi CM, Metra M. Cardiac Involvement in a Patient With Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020;5:819-824. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1111] [Cited by in RCA: 1270] [Article Influence: 254.0] [Reference Citation Analysis (0)] |
| 37. | Kang Y, Chen T, Mui D, Ferrari V, Jagasia D, Scherrer-Crosbie M, Chen Y, Han Y. Cardiovascular manifestations and treatment considerations in COVID-19. Heart. 2020;106:1132-1141. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 252] [Cited by in RCA: 262] [Article Influence: 52.4] [Reference Citation Analysis (0)] |
| 38. | Allam HH, Kinsara AJ, Tuaima T, Alfakih S. Pericardial Fluid in a COVID-19 Patient: Is It Exudate or Transudate? Eur J Case Rep Intern Med. 2020;7:001703. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 39. | Pedraza García J, Valle Alonso J, Ceballos García P, Rico Rodríguez F, Aguayo López MÁ, Muñoz-Villanueva MDC. Comparison of the Accuracy of Emergency Department-Performed Point-of-Care-Ultrasound (POCUS) in the Diagnosis of Lower-Extremity Deep Vein Thrombosis. J Emerg Med. 2018;54:656-664. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 41] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 40. | Middeldorp S, Coppens M, van Haaps TF, Foppen M, Vlaar AP, Müller MCA, Bouman CCS, Beenen LFM, Kootte RS, Heijmans J, Smits LP, Bonta PI, van Es N. Incidence of venous thromboembolism in hospitalized patients with COVID-19. J Thromb Haemost. 2020;18:1995-2002. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1017] [Cited by in RCA: 1092] [Article Influence: 218.4] [Reference Citation Analysis (0)] |
| 41. | United States Environmental Protection Agency. List N: Disinfectants for Use Against SARS-CoV-2 (COVID-19). Available from: https://www.acep.org/globalassets/images/acep-us-machine-cleaning-covid-19.pdf. |