Published online Apr 28, 2020. doi: 10.4329/wjr.v12.i4.29
Peer-review started: November 6, 2019
First decision: December 4, 2019
Revised: December 9, 2019
Accepted: January 28, 2020
Article in press: January 28, 2020
Published online: April 28, 2020
Processing time: 173 Days and 13.3 Hours
Chronic airspace diseases are commonly encountered by chest, body or general radiologists in everyday practice. Even though there is significant overlap in the imaging findings of different causes of chronic airspace disease, some key clinical, laboratory and imaging findings can be used to guide the radiologist to the correct diagnosis. The goal of this article is to review and compare these features.
Core tip: This manuscript reviews the imaging findings of causes of chronic airspace opacification in the lungs. This manuscript is based on an education exhibit that was presented by the corresponding author in the Radiological Society of North America Annual Meeting, 2018 Chicago and received Certificate of Merit in recognition.
- Citation: Ansari-Gilani K, Chalian H, Rassouli N, Bedayat A, Kalisz K. Chronic airspace disease: Review of the causes and key computed tomography findings. World J Radiol 2020; 12(4): 29-47
- URL: https://www.wjgnet.com/1949-8470/full/v12/i4/29.htm
- DOI: https://dx.doi.org/10.4329/wjr.v12.i4.29
Filling of the alveoli with material that attenuates X-ray beams more than the surrounding parenchyma causes airspace opacification. This is equivalent to the pathological term consolidation[1]. Ground glass opacification (GGO) or consolidative opacification of the lungs can be caused by different materials, including water, pus, blood, cells, protein, and fat. There is no definite definition of chronic airspace disease, however. An opacity that persists in follow-up studies and does not resolve in the expected time and after appropriate treatment can be called chronic. Chronic airspace opacification, while persistent, may show minor or major changes in distribution and appearance[2].
The list of causes of chronic airspace disease is long and exhaustive. The goal of this study was to review the causes of chronic airspace disease and discuss the clinical, laboratory and radiological findings that can help radiologists and clinicians to narrow down the differential diagnosis.
As stated above, airspace opacification is caused by filling of the alveoli with material that attenuates X-rays more than the surrounding parenchyma[1]. Airspace opacity can be seen as GGO when the bronchial and vascular markings are still visible, or can manifest as consolidation opacification, usually with air-bronchogram, when the bronchial or vascular markings are obscured[3]. Also stated above, airspace opacity can be caused by different materials, including water, pus, blood, cells, protein and fat. Chronic airspace opacities may persist throughout multiple imaging studies over time, with minimal or no significant change. It bears repeating from above that, alternatively, while persistent, they may show minor or major changes in distribution and appearance[2].
Causes of chronic airspace disease can be divided into four general groups, namely inflammatory, infectious, neoplastic, and miscellaneous.
As stated in the Introduction, given the overlapping presentation and appearances of many of the causes of chronic airspace disease, clinical and laboratory information, together with imaging findings, are crucial to narrow down the differential diagnosis.
A patient’s past medical history can provide clues to the etiology of chronic airspace disease. For example, history of asthma can suggest eosinophilic pneumonia or eosinophilic granulomatosis, with polyangiitis as cause of the airspace disease. A history of sarcoidosis is suggestive of alveolar sarcoidosis. Malignancy risk factors, such as smoking history, may suggest pulmonary adenocarcinoma. Immu-nocompromised state may raise concern for pulmonary tuberculosis or post-transplant lymphoproliferative disorder (PTLD). History of collagen vascular disease may raise concern for pulmonary hemorrhage and organizing pneumonia (OP). Multiorgan involvement may suggest collagen vascular disease or PTLD. History of treatment with anticancer medication should raise the concern for pneumonitis, which may have imaging patterns of different chronic airspace disease (Tables 1-4).
| Causes of chronic airspace disease/ General category | Clinical information | Laboratory findings | Imaging findings | Prognosis and treatment |
| Alveolar sarcoidosis/ Inflammatory | History of sarcoidosis | Elevated ACE | Infiltrative and consolidative opacities with ill-defined margins and sometimes air bronchograms; Typical findings of sarcoidosis may or may not be present (perilymphatic nodules, enlarged lymph nodes in the right paratracheal region and bilateral hila) | Corticosteroids only given for active disease; Presence of alveolar sarcoidosis is more suggestive of active disease; Relatively rapid response to treatment; May recur |
| Chronic eosinophilic pneumonia/ Inflammatory | History of asthma in 50% of cases; Middle-aged women | Chronic eosinophilic pneumonia; Increased eosinophils in bronchoalveolar lavage; Elevated IgE | Middle/upper and peripheral lung predominant chronic airspace opacity and consolidations; Opacities may show subtle or major changes in appearance (migratory); GGO and interlobular septal thickening (crazy-paving) | Good prognosis; Often require long-term low-dose oral corticosteroid therapy in order to prevent relapse |
| Organizing pneumonia/ Inflammatory | No obvious cause in most of the cases (therefore cryptogenic organizing pneumonia); History of vasculitis or connective tissue disorder may be present; History of anticancer treatment may be present | Classic findings: Bilateral peribronchovascular and/or subpleural consolidations with mid-lower lung zone preference; Less common findings: Small, ill-defined peribronchial or peribronchiolar nodules large nodules or masses; Halo sign; Reverse halo sign; Crazy paving arcade-like or polygonal opacities; Opacities may show subtle changes in appearance overtime (migratory) | Most (especially cryptogenic forms) respond very well to corticosteroid treatment; A small percentage of patients many develop progressive fibrosis | |
| EGPA (Churg-Strauss syndrome)/ Inflammatory | Small to medium vessel necrotizing pulmonary vasculitis; History of asthma is usually present; May have extrapulmonary findings (sinusitis, diarrhea, skin purpura, arthralgias) | Eosinophilia; ANCA (+) | More common: Peripheral or random parenchymal opacification either consolidation or ground glass; Opacities can be transient and change in appearance and distribution in the follow-up imaging; Less common: Centrilobular nodules and bronchial wall thickening; Cavitation is rare | Corticosteroids; May need addition immunosuppression with cyclosporine, azathioprine if there is cardiac, renal, GI or CNS involvement; Low mortality rate; Cardiac involvement is a major contributor to death |
| Granulomatosis with polyangiitis (Wegner granulomatosis)/ Inflammatory | Multisystem necrotizing non-caseating granulomatous vasculitis affecting small to medium; May involve sinuses and kidneys | ANCA (+) | Chronic airspace opacity and consolidation; Nodules and masses which may cavitate in 50% of cases; Halo or reverse halo sign may be present due to hemorrhage and associated ground-glass appearance | Immunosuppression with cyclophosphamide, methotrexate and/or corticosteroids; Rapidly fatal if not treated |
| Treatment and drug-related/ Inflammatory | History of cancer treatment; Respiratory symptoms related to pneumonitis including dyspnea and fever | Can have the following appearances; Organizing pneumonia; Nonspecific interstitial pneumonia; ARDS; Eosinophilic pneumonia; Pulmonary hemorrhage | Supportive treatment; Withholding treatment. May or may not recur after reintroduction of treatment |
| Causes of chronic airspace disease/ General category | Clinical information | Laboratory findings | Imaging findings | Prognosis and treatment |
| Fungal infection, including angio-invasive aspergillosis/ Infectious | History of immunosuppression including: Neutropenia; High-dose steroid treatment; Bone marrow transplant; End-stage AIDS; Symptoms are nonspecific (fever, cough, pleuritic chest pain, hemoptysis) | Neutropenia, especially severe (absolute neutrophil count < 500 cells/µL) | Parenchymal nodules or consolidation with a surrounding area of ground glass opacity (halo sign); Reverse halo sign; Peripheral wedge-like areas of consolidation representing hemorrhagic pulmonary infarct; Pleural effusion and lymphadenopathies are rare | Intravenous amphotericin B; Poor prognosis; Early diagnosis improves survival |
| Pulmonary tuberculosis/ Infectious | Immunosuppression such as AIDS; Recent travel to endemic countries | Low CD4 count in AIDS patients (< 350 cells/mm3) | Primary tuberculosis: Not detectable; Patchy or even lobar consolidation; Cavitation is rare; Military (numerous tiny nodules) tuberculosis can be seen Post-primary tuberculosis: Mostly involve the posterior segments of the upper lobes or superior segments of the lower lobes; Patchy consolidation with or without ground-glass opacity; Cavitation is more common; Military (numerous tiny nodules) tuberculosis can be seen | Appropriate antibiotics based on sensitivity; Respiratory isolation if needed |
| Non-tuberculosis MAC infection/ Infectious | May have pre-existing pulmonary disease or depressed immunity; Can also happen in otherwise normal people; Predilection for older women who voluntary suppress cough (Lady Windermere syndrome) | Most common: Bronchiectasis and bronchial wall thickening with small centrilobular nodules and tree-in-bud appearance; Persistent consolidation and ground-glass patchy opacities; Upper lung cavitary lesions | No clear gold-standard for treatment; Usually need multiple antibiotics; May be candidate for resection of the involved lung if the disease is localized; More aggressive course in upper lung cavitary form More indolent course in nodular bronchiectatic form | |
| Incompletely treated bacterial infection/ Infectious | History of recent bacterial pneumonia with incomplete treatment | Persistent leukocytosis | Persistent consolidation | Continued treatment with appropriate antibiotic |
| Pneumocystis jirovecii pneumonia/ Infectious | HIV (+) patients; Post-transplant patients; Patients undergoing chemotherapy or with hematologic malignancies; Patients with connective tissue disorder on corticosteroid treatment | CD4 counts < 200 cells/mm | Ground-glass opacity mainly with perihilar or mid zone distribution, most common findings; Less common/less typical findings septal thickening and crazy paving, pneumatocele; Pleural effusion and lymphadenopathy are unusual | Trimethoprim-sulfamethoxazole as treatment or for prophylaxis |
| Causes of chronic airspace disease/ General category | Clinical information | Laboratory findings | Imaging findings | Prognosis and treatment |
| Pulmonary adenocarcinoma in situ or minimally invasive/ Neoplastic | History of smoking is usually present | Predominantly GGO ≤ 3 cm with or without a small solid nodular component; Fried-egg sign; Mildly hypermetabolic on FDG/PET; Pseudocavitation may be present; Fissural or pleural retraction may be seen; Adenopathy and pleural effusion are uncommon at this stage | Surgical resection; Chemotherapy; Radiation treatment | |
| Invasive adenocarcinoma of the lung/Neoplastic | History of smoking is usually present | Solid or subsolid and sometimes even ground glass nodule or mass; Consolidation with air-bronchogram, mimicking pneumonia has been mostly described in invasive mucinous adenocarcinoma subtype | Surgical resection; Chemotherapy; Radiation treatment | |
| Pulmonary lymphoma/ Neoplastic | Primary (usually non-Hodgkin’s lymphoma) or secondary pulmonary lymphoma (can be Hodgkin’s or non-Hodgkin’s lymphoma) | Most common imaging finding: Mass or mass-like consolidation with or without cavitation | Surgery for localized diseas;e Chemotherapy; Radiation treatment; Good prognosis | |
| PTLD/ Neoplastic | Occurs in 10% of solid organ transplant cases; Highest incidence in small bowel transplant; Can affect multiple organs | Pulmonary consolidation; Pulmonary nodules and masses which may cavitate | Treatment depends on location and extent of the disease; Treatment options: Reduction in immunosuppression; Resection of localized disease; Radiation treatment Chemotherapy | |
| Pulmonary metastasis/ Neoplastic | Seen in adenocarcinoma of gastrointestinal tract and less commonly of breast and ovarian origin | Uncommon appearance of pulmonary metastasis appearing as persistent airspace opacity and consolidation; Due to lepidic growth of tumor cells along the intact alveolar walls | Treatment of the underlying cancer |
| Causes of chronic airspace disease/ General category | Clinical information | Laboratory findings | Imaging findings | Prognosis and treatment |
| Lipoid pneumonia/ Miscellaneous | Usually elderly individuals; History of chronic inflammation in primary (endogenous) form; History of chronic constipation and aspiration in the secondary (exogenous) form | Chronic consolidative and GGOs; Nodules and masses; More in the dependent portions of the lungs; May or may not have fat attenuation | Biopsy may be needed in lipid poor cases to exclude malignancy | |
| Alveolar hemorrhage/ Miscellaneous | May have history of vasculitides, connective tissue disorders, or coagulation disorders | GGO or consolidation in the acute phase; GGO and interlobular septal thickening in subacute phase; May develop fibrosis if recurrent or chronic; Opacities may show subtle or major changes in appearance (migratory) | Supportive treatment; Treatment of underlying disease | |
| PAP/ Miscellaneous | Due to abnormal intra-alveolar accumulation of surfactant-like material; More common in smokers | Crazy-paving which is due to combination of GGO and smooth interlobular septal thickening; This finding is very suggestive but not pathognomonic; Usually bilateral and extensive, with more severe involvement of the lower lobes | Whole-lung bronchoalveolar lavage to remove alveolar material; Variable prognosis, ranging from improvement with treatment to a chronic and terminal course. |
Reviewing the patient’s laboratory values can help the radiologist to narrow down the differentials for chronic airspace disease. For example, presence of eosinophilia suggests eosinophilic pneumonia, while presence of neutropenia will be more suggestive of atypical/fungal infection, such as angio-invasive aspergillosis. Elevated serum angiotensin-converting enzyme (commonly known as ACE) suggest sarcoidosis. Positive antineutrophil cytoplasmic antibody (commonly referred to as ANCA) can be seen in eosinophilic granulomatosis with polyangiitis (EGPA) and granulomatosis with polyangiitis (Tables 1-4).
The imaging findings and imaging signs can also be very helpful in narrowing down the differential diagnosis (Tables 1-5). For example, the presence of specific imaging signs, such as halo sign or reverse halo sign, can be seen in OP or angio-invasive aspergillosis. Pseudocavitation and fissural retraction can suggest the diagnosis of adenocarcinoma. Distribution of the opacity, whether involving the upper (sarcoid) or lower (lipoid pneumonia) lung, can also be helpful. In addition, the appearance of opacification, which can be either GGO (adenocarcinoma, hemorrhage), consolidation (lymphoma) or mixed (OP, angio-invasive aspergillosis, adenocarcinoma), can provide helpful information.
| Imaging finding/sign | Cause |
| Imaging signs | Halo sign: Fungal infection including angio-invasive pulmonary aspergillosis, pulmonary tuberculosis, lung adenocarcinoma, organizing pneumonia, granulomatosis with polyangiitis |
| Reverse halo sign: Fungal infection including angio-invasive aspergillosis, organizing pneumonia, granulomatosis with polyangiitis, pulmonary tuberculosis, alveolar sarcoidosis | |
| 1-2-3 sign (right paratracheal and bilateral hilar lymphadenopathy): Alveolar sarcoidosis | |
| Crazy paving: Pulmonary alveolar proteinosis, pulmonary hemorrhage, chronic eosinophilic pneumonia, organizing pneumonia, alveolar sarcoidosis | |
| Pseudocavitation: Lung adenocarcinoma | |
| Fried egg sign: Lung adenocarcinoma | |
| Fissural retraction: Lung adenocarcinoma | |
| Distribution | Upper lung: Sarcoid, chronic eosinophilic pneumonia (mid and upper), tuberculosis |
| Lower lung: Lipoid pneumonia, organizing pneumonia (mid and lower) | |
| Ground glass vs consolidation | Ground-glass opacity: Adenocarcinoma, pulmonary hemorrhage |
| Mixed: Adenocarcinoma, organizing pneumonia, angio-invasive aspergillosis | |
| Consolidation: Invasive mucinous adenocarcinoma, lymphoma, PTLD | |
| Presence of cavitary lesion | Pulmonary tuberculosis |
| Granulomatosis with polyangiitis and other vasculitis | |
| Fungal infection | |
| Peri-lymphatic nodules | Alveolar sarcoidosis |
| Minor or major change in the distribution and severity | Chronic eosinophilic pneumonia |
| Organizing pneumonia | |
| Pulmonary hemorrhage | |
| Arcade-like or polygonal opacities | Organizing pneumonia |
| Fat density | Lipoid pneumonia |
| Interlobular septal thickening and subpleural sparing | Organizing pneumonia |
| Pulmonary hemorrhage | |
| Involvement of other organs | Liver and bowel: PTLD |
| Renal involvement: Granulomatosis with polyangiitis | |
| Involvement of upper respiratory tracts and paranasal sinuses: Granulomatosis with polyangiitis, eosinophilic granulomatosis with polyangiitis |
Presence of extrathoracic disease may shed light on the correct diagnosis (e.g., renal or upper respiratory tract involvement in granulomatosis with polyangiitis, or involvement of liver and gastrointestinal tract in PTLD). Also, the presence of other ancillary imaging findings, such as presence and distribution of lymphadenopathy, presence of cavitation or presence of fat, can help (Tables 1-5). It should be noted that, while some imaging findings are suggestive and relatively specific for a diagnosis (e.g., reverse halo sign in OP), they may not be very sensitive.
In the following sections, we will discuss the causes of chronic airspace disease and review the key clinical, laboratory and characteristic imaging findings that are helpful in making the diagnosis or in narrowing down the list of differential diagnosis.
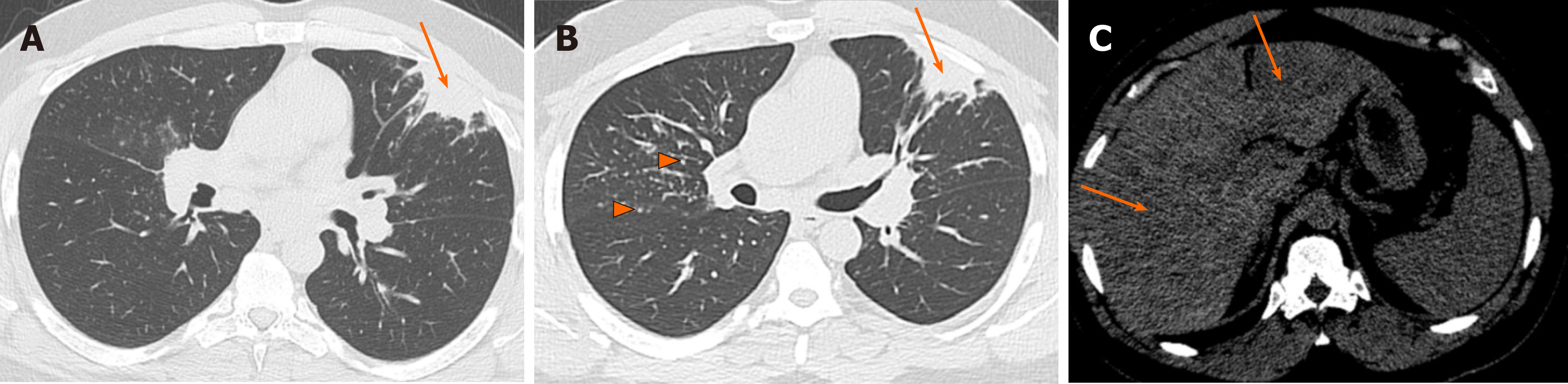
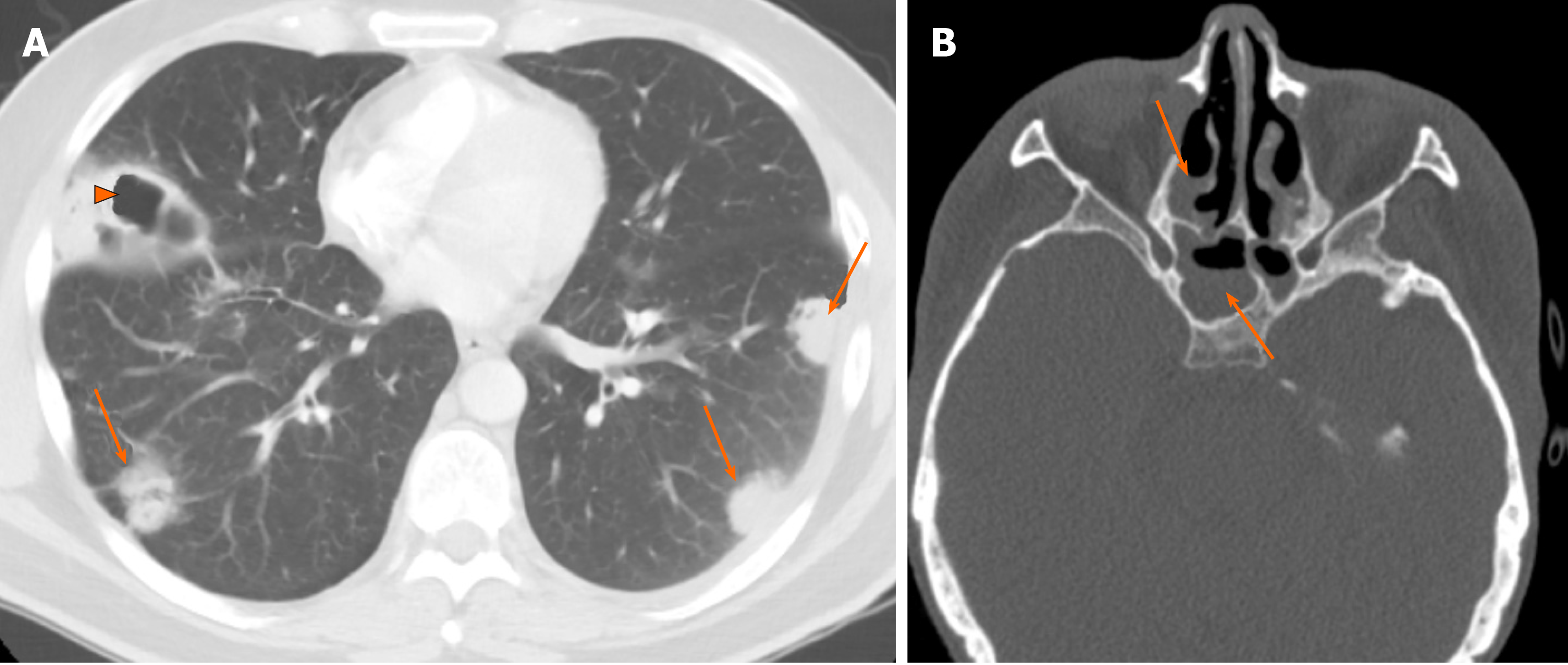
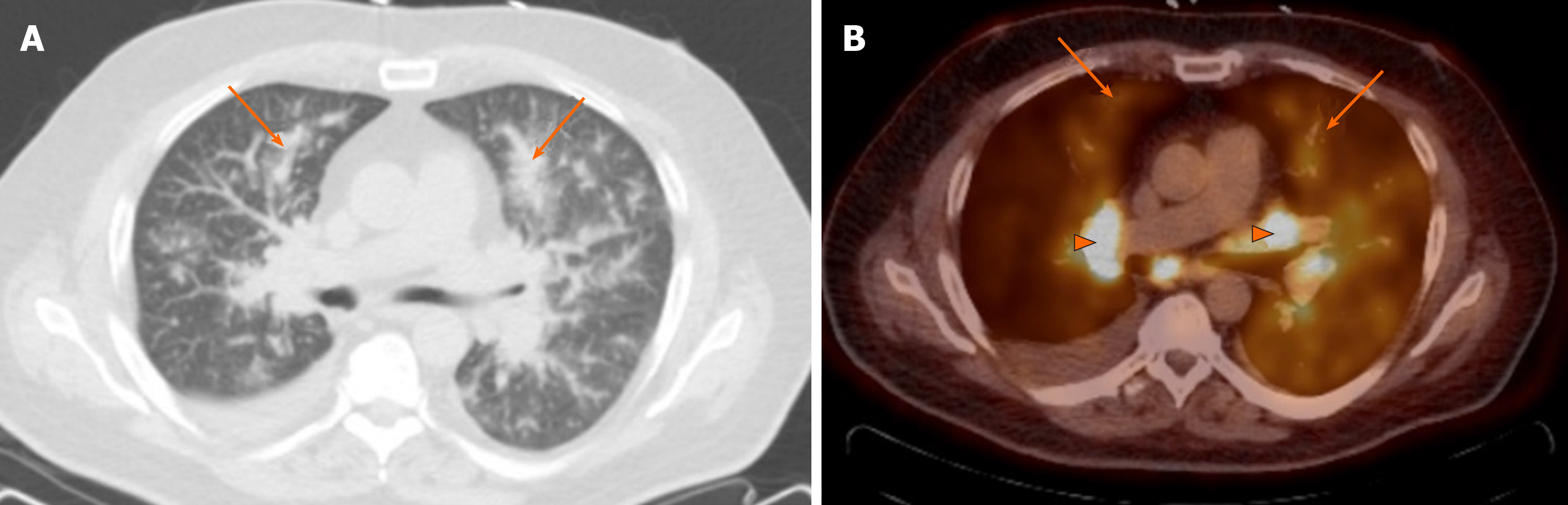
Even though not a true airspace or alveolar process pathologically (noncaseating granulomas are mostly seen in the alveolar septa and around the small vessels), alveolar sarcoidosis can appear as persistent airspace opacities on imaging, mimicking intra-alveolar process. It is an atypical manifestation of thoracic sarcoidosis with estimated occurrence rate of 1%–4.4%[4]. The more common and classic appearance of pulmonary sarcoidosis is upper-lung predominant and fairly symmetric perilymphatic nodules, while alveolar sarcoidosis presents as infiltrative and consolidative opacities with ill-defined margins and sometimes air bronchograms, or large nodules/masses that persist over time[5], mimicking infiltrative malignancies, such as multifocal adenocarcinoma or pulmonary lymphoma (Figure 1). Reverse halo sign with central GGO and peripheral rim of consolidation is well described in alveolar sarcoidosis[6]. Also, interlobular septal thickening and GGO causing crazy-paving pattern has been described[7] (Table 1).
Alveolar sarcoidosis is associated with a more acute and symptomatic phase of thoracic sarcoidosis and is therefore expected to show a more severely increased metabolic activity on fluorodeoxyglucose-positron emission tomography (commonly known as FDG/PET)[8]. Active disease is treated with corticosteroids, generally giving a relative rapid response to the treatment; however, the disease may recur after discontinuation of treatment[4].
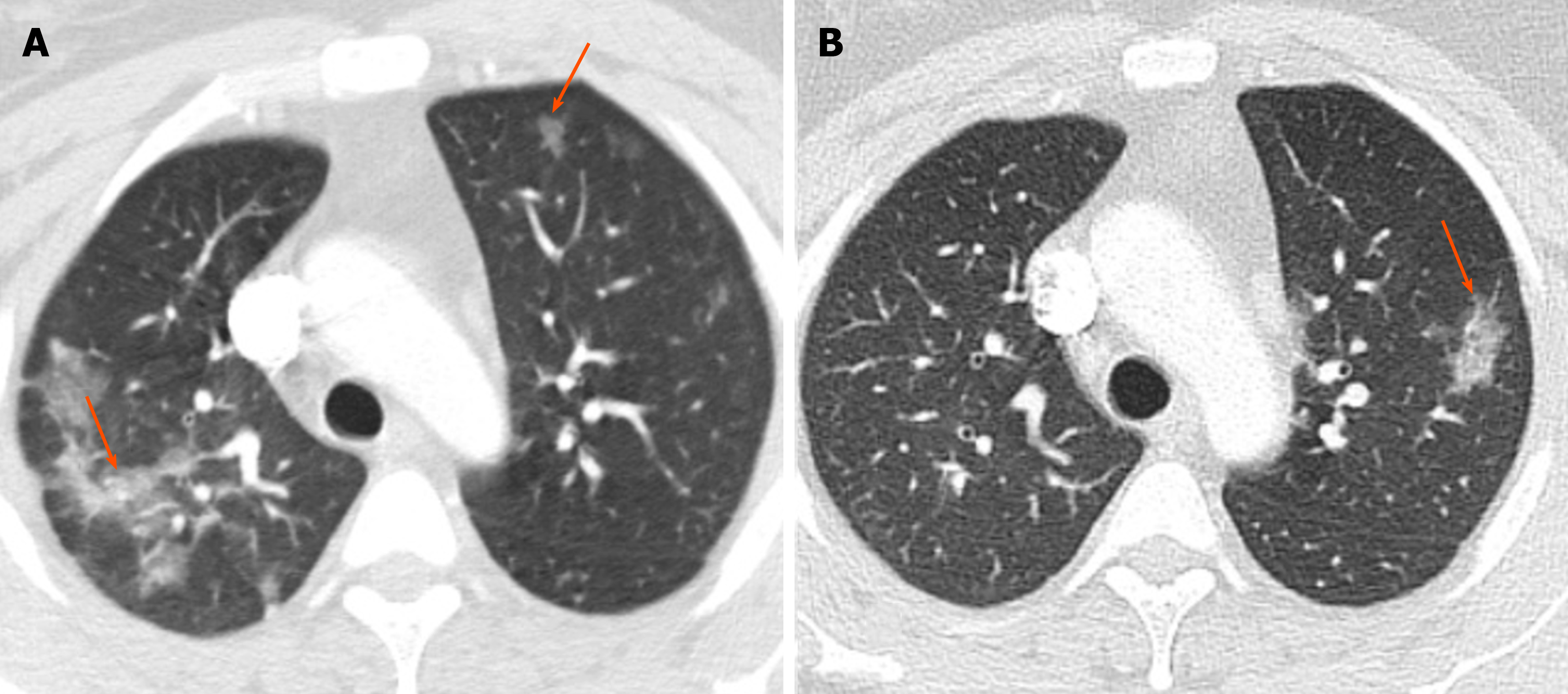
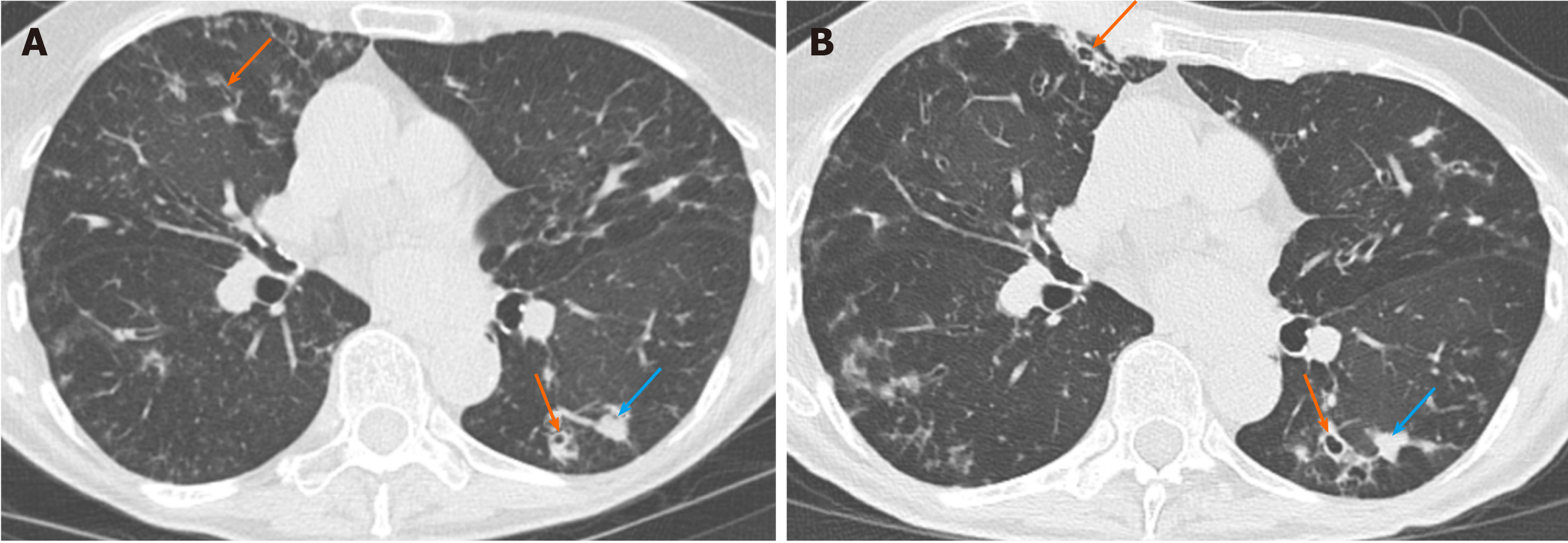
This is an idiopathic condition, more common in middle-aged women, and with a history of asthma present in up to 50% of patients[9]. It is characterized by filling of the alveoli with an inflammatory, eosinophil-rich infiltrate[9]. Increased serum IgE level is seen in two-thirds of patients and high erythrocyte sedimentation rate is also present. High eosinophil counts are seen in the bronchoalveolar lavage fluid[9,10].
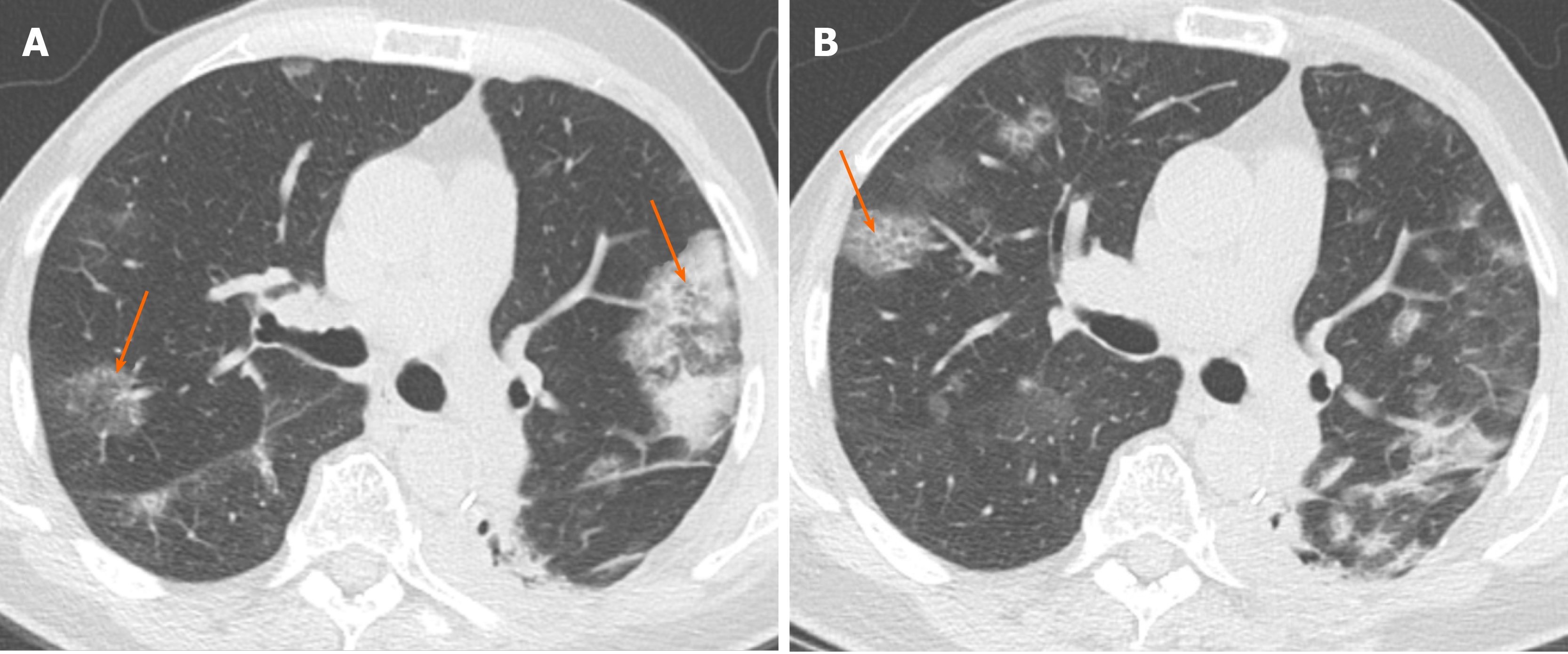
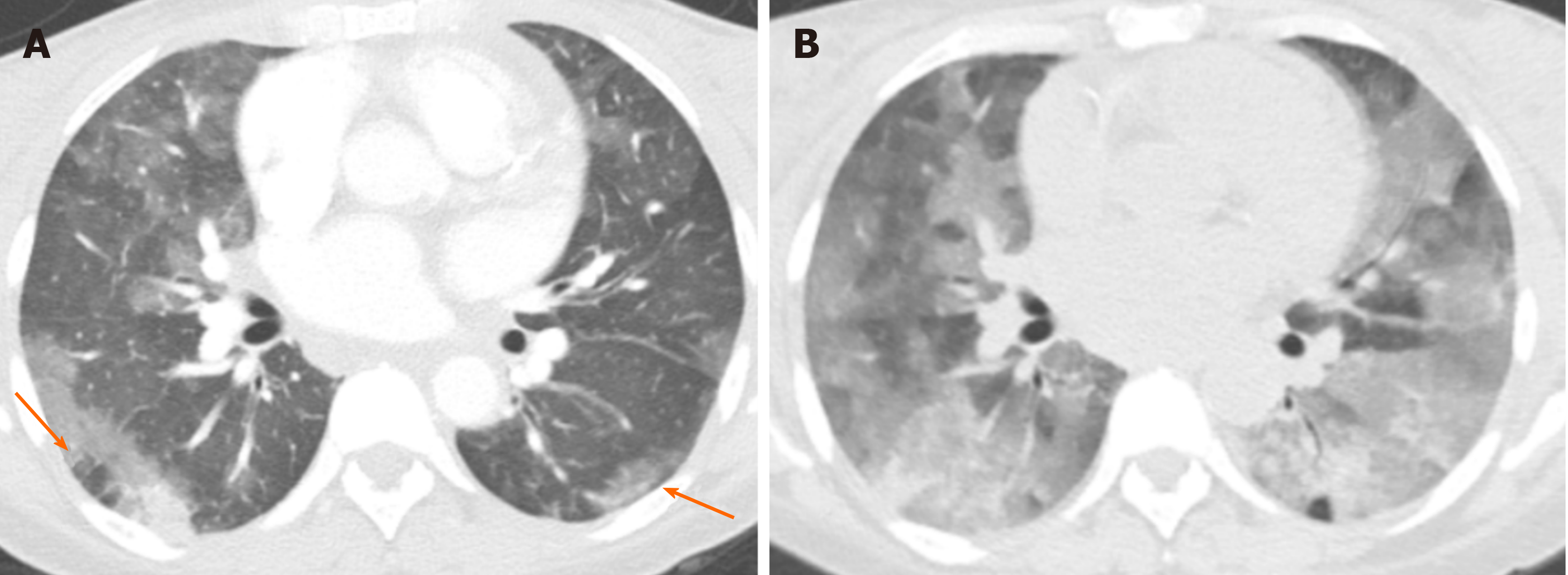
The typical imaging finding is presence of middle/upper and peripheral lung predominant chronic airspace opacity and consolidations[9]. The opacities may persist over time but usually show subtle or major changes in appearance and therefore are migratory (Figure 2). Crazy-paving with GGO and interlobular septal thickening have also been described[7].
The diagnosis is based on respiratory symptoms, alveolar and/or blood eosinophilia, airspace opacifications, and exclusion of other causes of eosinophilic lung disease[10]. Overall, chronic eosinophilic pneumonia carries a good prognosis. However, it often needs long-term low-dose corticosteroid treatment in order to prevent relapse[10].
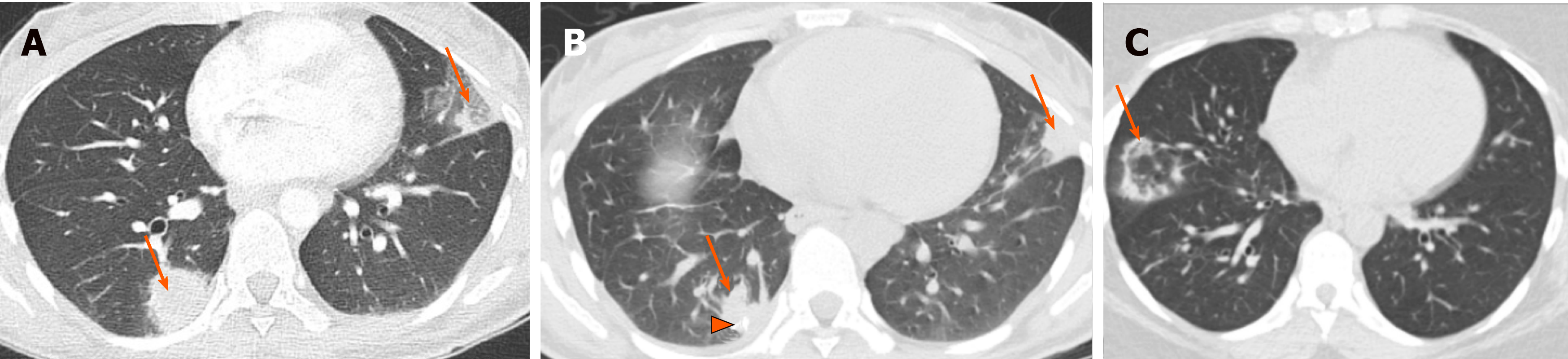
Cryptogenic organizing pneumonia (COP) is a disease of unknown etiology that affects bronchioles and alveoli[11]. The inflammatory process may cause bronchiolar occlusion. Hence, it was previously termed bronchiolitis obliterans organizing pneumonia. A wide variety of infectious as well as noninfectious causes may result in a similar histologic pattern of OP, however the idiopathic form of OP is termed COP[11].
Even though OP or COP can present as small, ill-defined peribronchial or peribronchiolar nodules as well as large nodules or masses, the classic imaging finding is presence of bilateral peribronchovascular and/or subpleural consolidations with mid-lower lung zone preference[11] (Figure 3). Reverse halo sign can be seen in 20% of the cases[12]. The areas of consolidation may be migratory and show subtle or major changes in their appearance and distribution[11]. In addition to the mentioned classic imaging findings, the presence of arcade-like or polygonal opacities are suggestive of this diagnosis[11]. Interlobular septal thickening and GGO causing crazy-paving pattern have also been described[7]. Most cases, especially of the cryptogenic form, respond well to corticosteroid treatment. A small percentage of patients, however, may develop progressive fibrosis[11].
Also known as Churg-Strauss syndrome, EGPA is a small to medium vessel necrotizing pulmonary vasculitis. It is characterized by hypereosinophilia and is almost exclusively seen in patients with asthma[13].
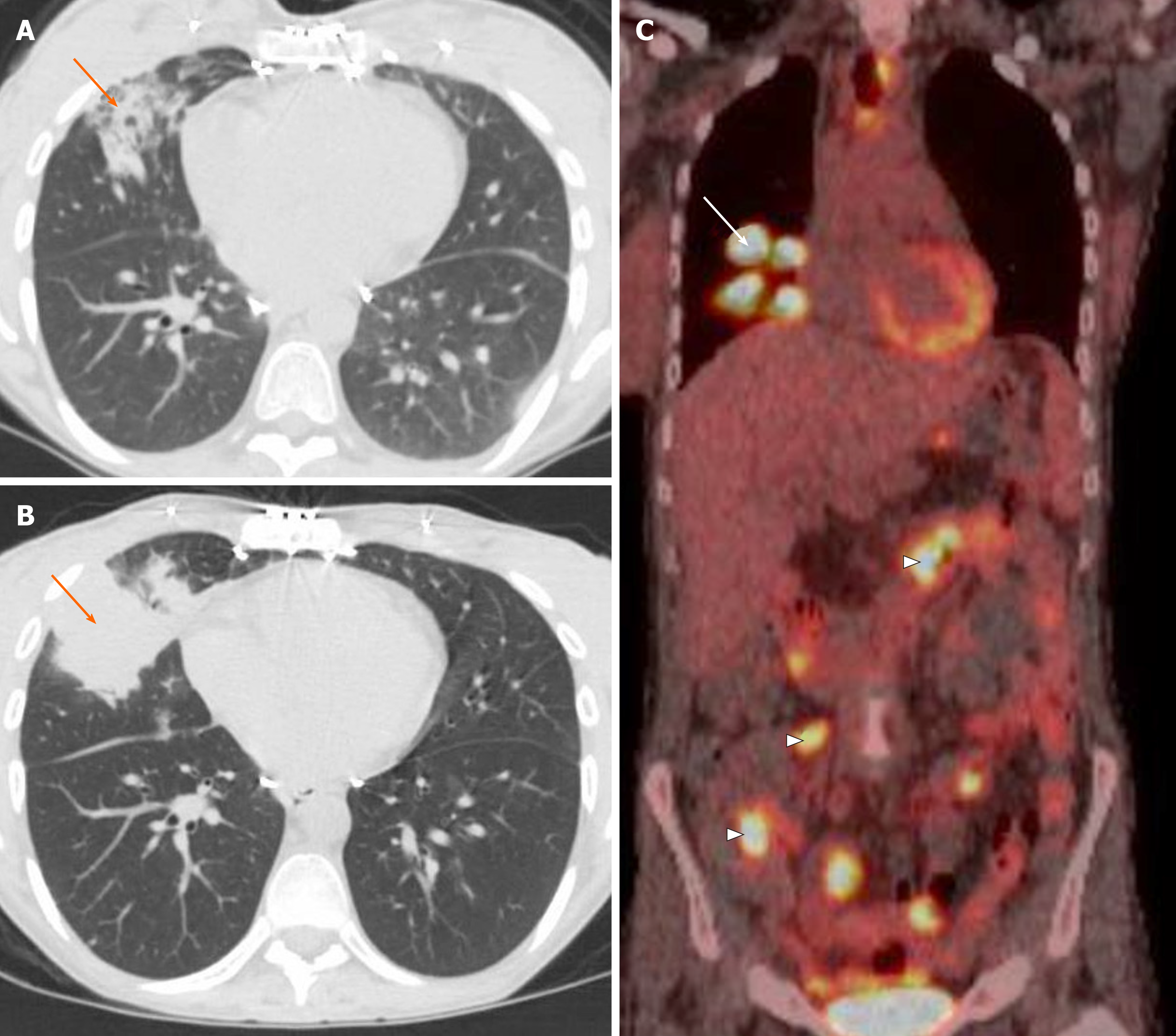
In addition to the pulmonary symptoms and asthma, patients also have such extrapulmonary findings as signs and symptoms related to sinusitis, diarrhea, skin purpura, and/or arthralgias. The most common imaging finding is peripheral or random parenchymal opacification, either as consolidation or ground glass, which can be transient and change in appearance and distribution in the follow-up imaging[13] (Figure 4). There is no zonal predominance. Less common imaging findings are centrilobular nodules and bronchial wall thickening and/or dilatation. Cavitation is rare[13].
EGPA is treated with corticosteroids. Further immunosuppression with cyclosporine or azathioprine may be needed, especially in cases with cardiac, renal, gastrointestinal and central nervous system involvement[13]. Even though the mortality is low, cardiac involvement is the major reason for death[13].
Granulomatosis with polyangiitis, previously known as Wegener granulomatosis, is a multisystem necrotizing noncaseating granulomatous c-ANCA-positive vasculitis affecting small- to medium-sized arteries, capillaries and veins[14]. The vasculitis mainly involves the respiratory system, sinuses, and kidneys, and is slightly more common in men[14].
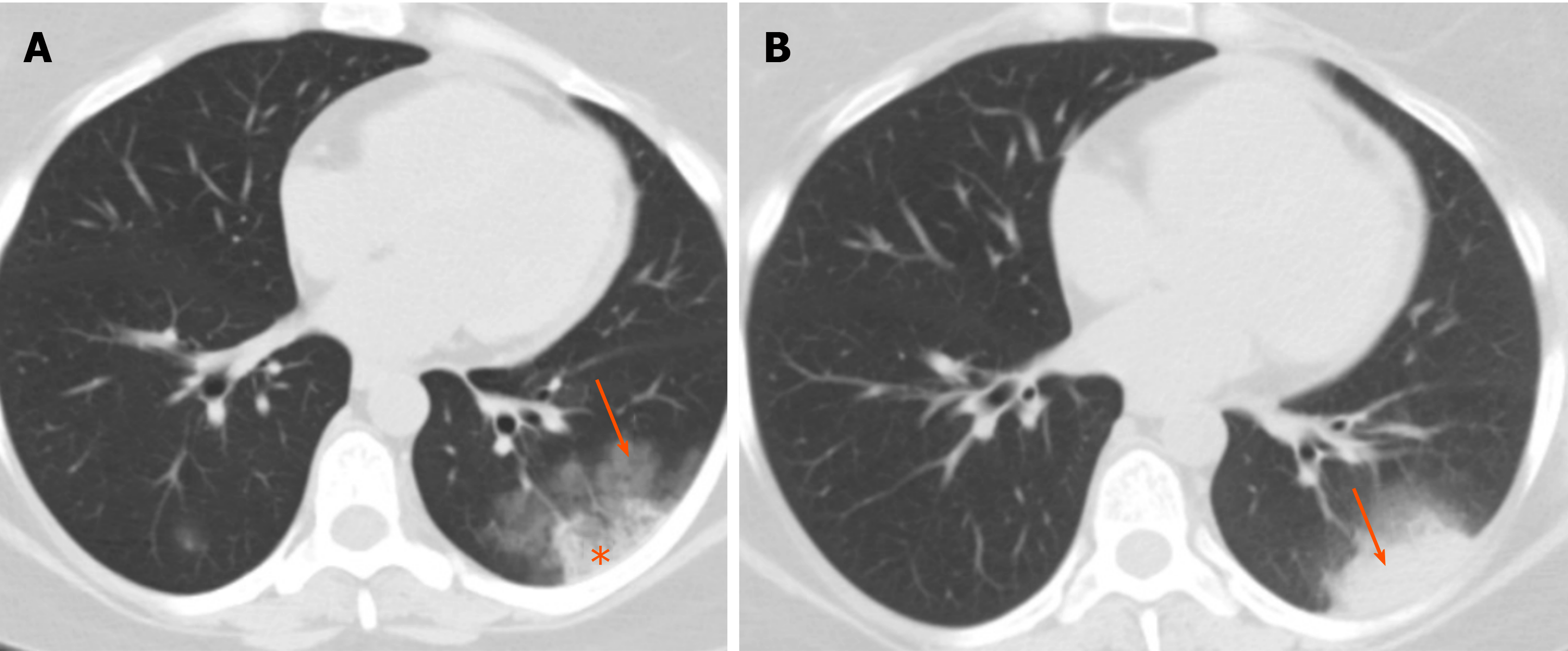
Although granulomatosis with polyangiitis can appear as chronic airspace opacity and consolidation on computed tomography (CT), presence of nodules and masses which cavitate in about 50% of the time is the more common manifestation[14] (Figure 5). Presence of ground glass appearance due to hemorrhage can cause halo or reverse halo sign appearance[14]. Consolidations can be wedge-shaped and peripheral, thereby mimicking pulmonary infarction. Consolidation may alternatively be focal or peribronchial[14]. Airspace consolidation can be due to pulmonary hemorrhage or pneumonia. Pleural effusion is seen in about 10% of cases, and mediastinal lymphadenopathy is relatively uncommon[14].
Immunosuppression with cyclophosphamide, methotrexate and corticosteroids is needed. Granulomatosis with polyangiitis can be rapidly fatal without treatment[14].
Different medications, especially those for cancer-related treatment, can negatively affect the lung parenchyma. Lung response to these medications can appear as different patterns of chronic airspace disease, such as OP (bleomycin, methotrexate, amiodarone), nonspecific interstitial pneumonia (amiodarone, methotrexate), eosinophilic pneumonia (penicillamine, sulfasalazine, nitrofurantoin, nonsteroidal anti-inflammatory drugs), and pulmonary hemorrhage (anticoagulants, amphotericin B)[15]. In addition, newer anticancer agents, such as immune check inhibitors, can cause different patterns of pneumonitis and airspace diseases; these patterns include OP, nonspecific interstitial pneumonia, hypersensitivity pneumonitis, and acute respiratory distress syndrome[16] (Figure 6).
Symptomatic and supportive treatment is the main part of treatment. However, there might be need to withhold the offending medication, depending on the severity of pneumonitis[16].
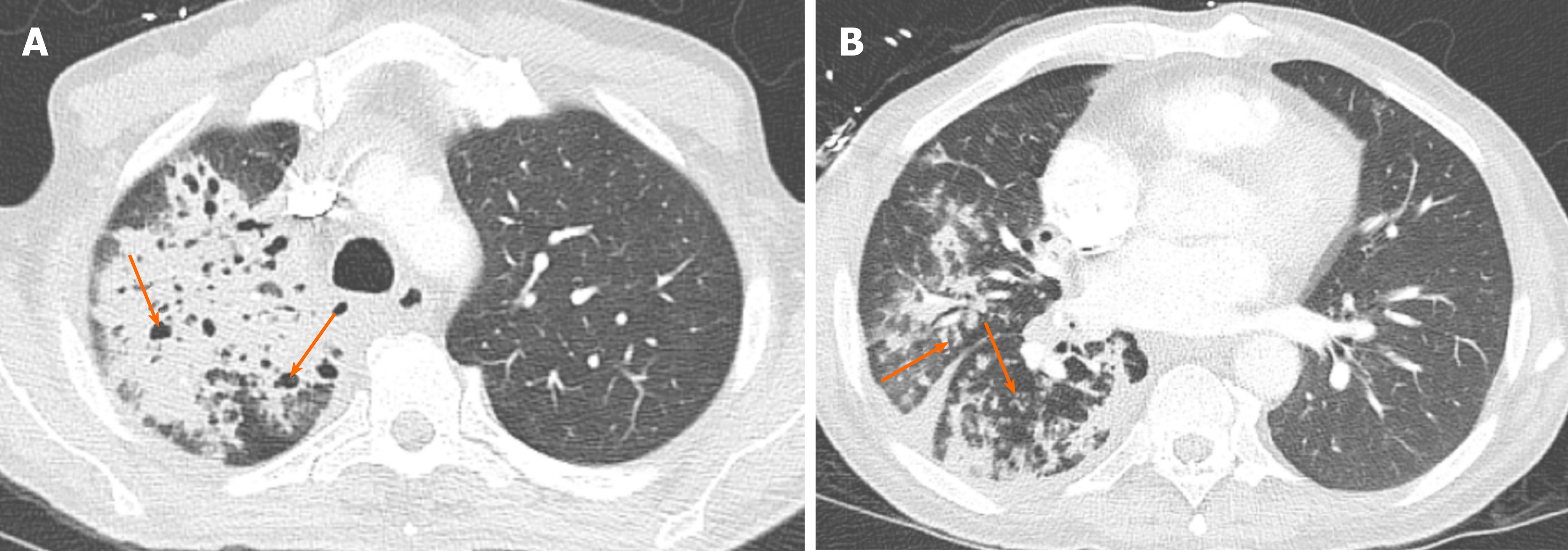
Pulmonary fungal infections are a relatively common complication in immunocompromised patients. Imaging findings can be variable, ranging from an airway-centered bronchopneumonia with associated tree-in-bud nodules to a more classic lobar or segmental appearing consolidation, with GGOs being the predominant findings in many cases[17]. Most angio-invasive fungal pneumonias, including angio-invasive aspergillosis, manifest as parenchymal nodules or consolidation with a surrounding area of GGO (“halo” sign) that results from hemorrhage[18] (Figure 7). In addition to the halo sign, reverse halo sign has been described in angio-invasive aspergillosis[19]. Peripheral wedge-like areas of consolidation, representing hemorrhagic pulmonary infarcts, are also well described in these patients[18]. Pleural effusion and lymphadenopathy are usually absent[20]. In the correct clinical setting, which includes severe immunocompromised state with neutropenia (absolute neutrophil count < 500/μL), these findings are strongly suggestive of angio-invasive aspergillosis until proven otherwise[17] (Table 2).
As it may take days to weeks for cultures to yield results, radiologist input is critical in facilitating timely, targeted therapy. Treatment is usually with intravenous amphotericin B. Without early diagnosis and prompt treatment, prognosis remains poor[17].
Imaging findings in primary pulmonary tuberculosis are nonspecific and can range from an almost undetectable area of small airspace opacity to patchy areas of consolidation or even lobar consolidation[21]. However, cavitation is uncommon in this phase[21]. Post-primary tuberculosis is more symptomatic clinically, with more profound imaging manifestations, and usually presents many years after the primary infection; the latter is usually due to compromise in the patient’s immune status. Moreover, it is usually seen in the posterior segments of the upper lobes or superior segments of the lower lobes.
Imaging findings are variable, but the typical appearance of post-primary tuberculosis is that of patchy consolidation with or without GGO (halo or reverse halo sign) or poorly defined linear and nodular opacities which persist and may cavitate in up to 40% of the cases[21]. Areas of cavitation may communicate with the airways resulting in endobronchial spread of infection and tree-in-bud appearance[21], suggesting a highly contagious form of disease (Figure 8).
Treatment is with multiple antibiotics, based on the sensitivity of the organism.
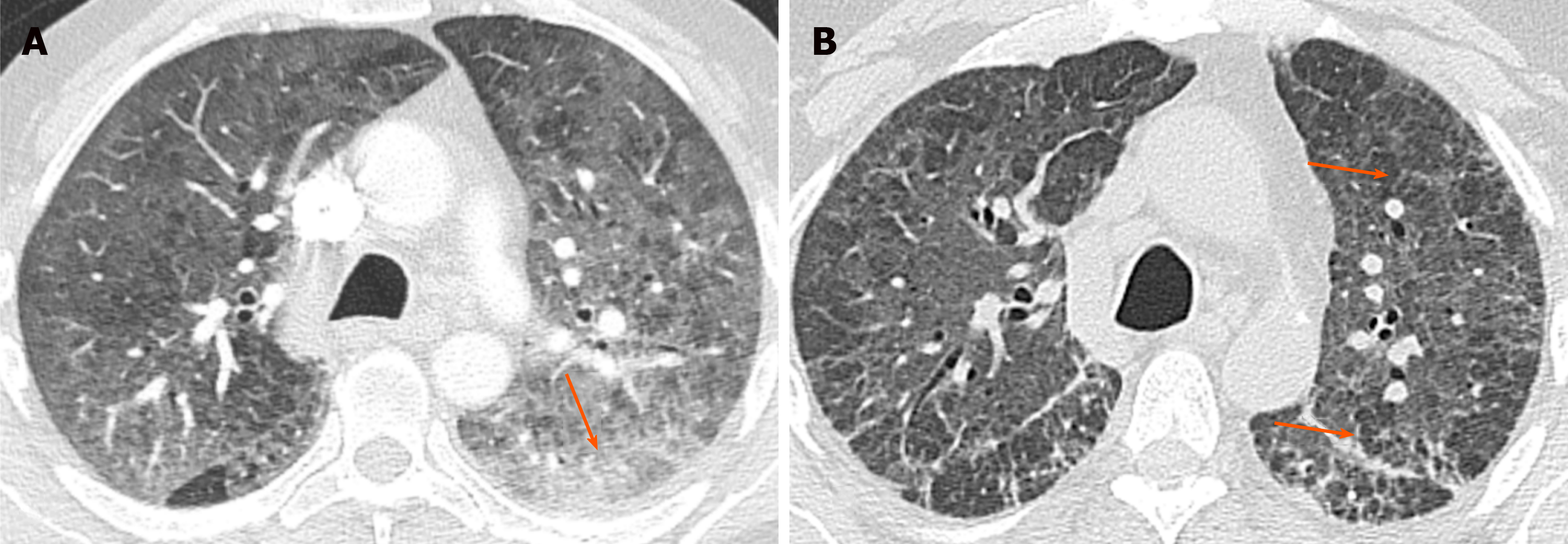
Non-tuberculosis mycobacterium avium complex infection: The incidence of nontuberculous mycobacterial pulmonary disease in the United States and Canada has been increasing and this is mainly due to mycobacterium avium complex organisms[22]. Although this infection can happen in patients with pre-existing pulmonary disease or depressed immunity, it has been increasingly reported in otherwise healthy individuals, especially in elderly women[23], and may be due voluntary suppression of the cough reflex (Lady Windermere syndrome).
Two main forms of pulmonary mycobacterium avium complex infections have been described. The first is the upper lobe fibrocavitary form, which has a more rapid and aggressive course, and needs prompt treatment. The second is the nodular bronchiectatic form, which tends to progress more slowly, and the diagnosis of the disease does not require immediate treatment and may be managed with observation alone.
In addition to the upper lobe cavitary lesions and right middle lobe/lingular bronchiectasis, CT findings include persistent patchy consolidation and ground glass patchy opacities[22] (Figure 9).
There is no clear gold-standard for treatment. Patients may be followed if asymptomatic. Symptomatic cases usually need multiple antibiotics. Surgical resection can be an option in localized disease[22]. The disease has a more aggressive course in the upper lung fibrocavitary form, while showing a more indolent course in the nodular bronchiectatic form[22].
Partially treated bacterial infection can present as an area of consolidation that is persistent with some or minimal improvement on follow-up imaging. This should be suspected when a patient with a proven diagnosis of bacterial infection is still symptomatic and the imaging findings are more or less unchanged.
Pneumocystis jirovecii pneumonia is an atypical pulmonary infection, which almost never happens in immunocompetent individuals but is one of the most common causes of life-threatening pulmonary infections in human immunodeficiency virus-positive patients. It typically occurs at CD4 counts < 200 cells/mm[24]. Other patient populations that are at increased risk of Pneumocystis jirovecii pneumonia infection are post-transplant patients, patients with hematologic malignancies, patients undergoing chemotherapy for malignancy, and patients undergoing long-term corticosteroid therapy for inflammatory and connective tissue diseases, such as Wegener granulomatosis and systemic lupus erythematosus[25].
The principal finding on chest CT is GGO, mainly with perihilar or mid zone distribution (Figure 10). Depending on presence or absence of prophylactic aerosolized medication; mid, upper or lower zone involvement may be dominant[24]. Other imaging findings include septal thickening and therefore crazy paving and pneumatoceles. Pleural effusion and lymphadenopathies are uncommon. Consolidation and cavitation are more atypical and seen mainly in patients who are on prophylactic treatment[26].
Most patients with acute infection are treated with trimethoprim-sulfamethoxazole, combined with corticosteroids in moderate to severe infections[27]. Trimethoprim-sulfamethoxazole is also used as a prophylactic regimen[27].
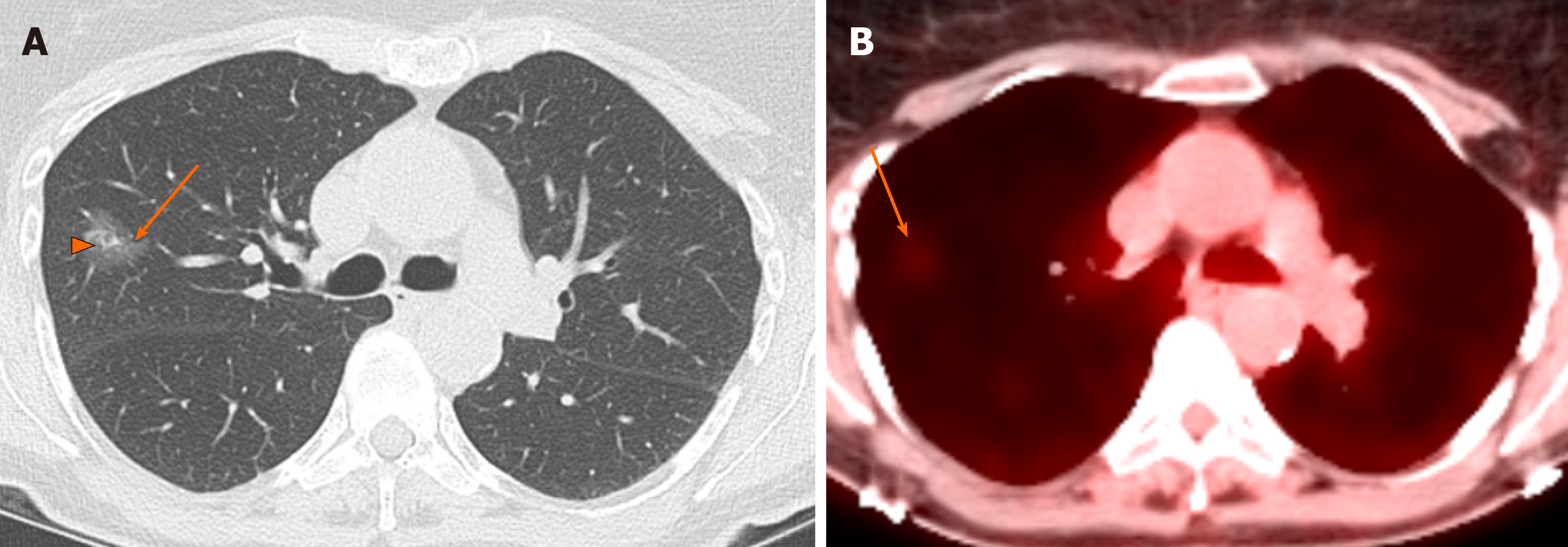
Lung adenocarcinoma is the most common histologic subtype of lung cancer. It is classified as adenocarcinoma in situ, minimally invasive adenocarcinoma, or invasive adenocarcinoma (Table 3).
Adenocarcinoma in situ and minimally invasive adenocarcinoma are seen as predominantly GGO ≤ 3 cm, with or without a small solid nodular component, that persist over multiple follow-up CT scans and show gradual and slow growth[28]. Presence of GGO with associated solid component is described as fried-egg sign[29,30] (Figure 11). FDG-PET/CT may be falsely negative for smaller lesions or show only mildly increased metabolic activity for larger lesions[28] (Figure 11). Pseudocavitation has been described as a well-recognized feature of adenocarcinoma in situ and minimally invasive adenocarcinoma[29] and refers to the central bubble-like low-density region seen within a pulmonary nodule on CT. Fissural or pleural retraction can also be seen with these tumors[30]. Hilar and mediastinal adenopathy and pleural effusion are uncommon at this stage[30].
Invasive adenocarcinoma appears as a solid or subsolid and sometimes even ground glass nodule or mass. The ground glass area corresponds to a lepidic growth pattern and the solid component corresponds to invasive patterns[31]. Persistent air-space opacity and consolidation with air-bronchogram, mimicking pneumonia, has been mostly described in the invasive mucinous adenocarcinoma subtype that was formerly called mucinous bronchoalveolar adenocarcinoma[32] (Figure 12). Other imaging findings described in this variant are multifocal subsolid nodules or masses[33].
Pulmonary lymphoma refers to lung parenchymal involvement with lymphoma and can be categorized as primary or secondary. Primary pulmonary lymphoma is rare and is usually non-Hodgkin’s lymphoma. It is limited to the lung and there is no evidence of extrathoracic involvement for at least 3 mo after the diagnosis[34]. Secondary pulmonary lymphoma, on the other hand, is relatively common and can be Hodgkin’s lymphoma or non-Hodgkin’s lymphoma[34].
Mass or mass-like consolidation > 1 cm with or without cavitation or air-bronchogram has been described as the most common imaging finding of pulmonary lymphoma[34] (Figure 13). Other less common findings are pleural-based mass, small (< 1 cm) nodules, alveolar or interstitial infiltrate, pleural effusion, and hilar or mediastinal lymphadenopathy[35].
Patients are treated with chemotherapy and radiation. Surgical resection can be done for localized disease. Pulmonary lymphoma carries a good prognosis[34].
PTLDs are uncommon complications following organ transplantation, affecting 10% of cases after solid organ transplant[36]. They include a variety of conditions ranging from lymphoid hyperplasia to malignancy and can be manifest a life-threatening condition. The incidence varies depending on the type of transplanted organ, with the highest incidence reported after small bowel transplant. The disease can be focal or systemic, and can affect any organ system and even the allograft. Liver is the most common organ to be involved[37] but other organs, such as small bowel, colon and lungs, are commonly involved[37].
Pulmonary findings of PTLD include pulmonary nodules and masses which may cavitate, with pulmonary consolidation in 55% of the cases and intra-thoracic lymphadenopathy in 45% of cases[36] (Figure 14).
The choice of treatment depends on severity, location and extent of the disease. Treatment options include, reduction in immunosuppression, resection of localized disease, radiation treatment, and/or chemotherapy[37]. Negative serology for Epstein-Barr virus and cytomegalovirus at the time of the transplant increases the risk of PTLD[36].
Although the most common pattern of pulmonary metastases is multiple pulmonary nodules with random distribution, persistent air-space opacity can be an unusual appearance of lung metastasis[38]. This pattern can be seen with adenocarcinomas of gastrointestinal tract origin but can also be seen in adenocarcinomas originating from the breast and ovary (Figure 15). This pattern is due to tumoral spread into the lung along the intact alveolar walls (lepidic growth), in a fashion similar to invasive primary adenocarcinoma of the lung.
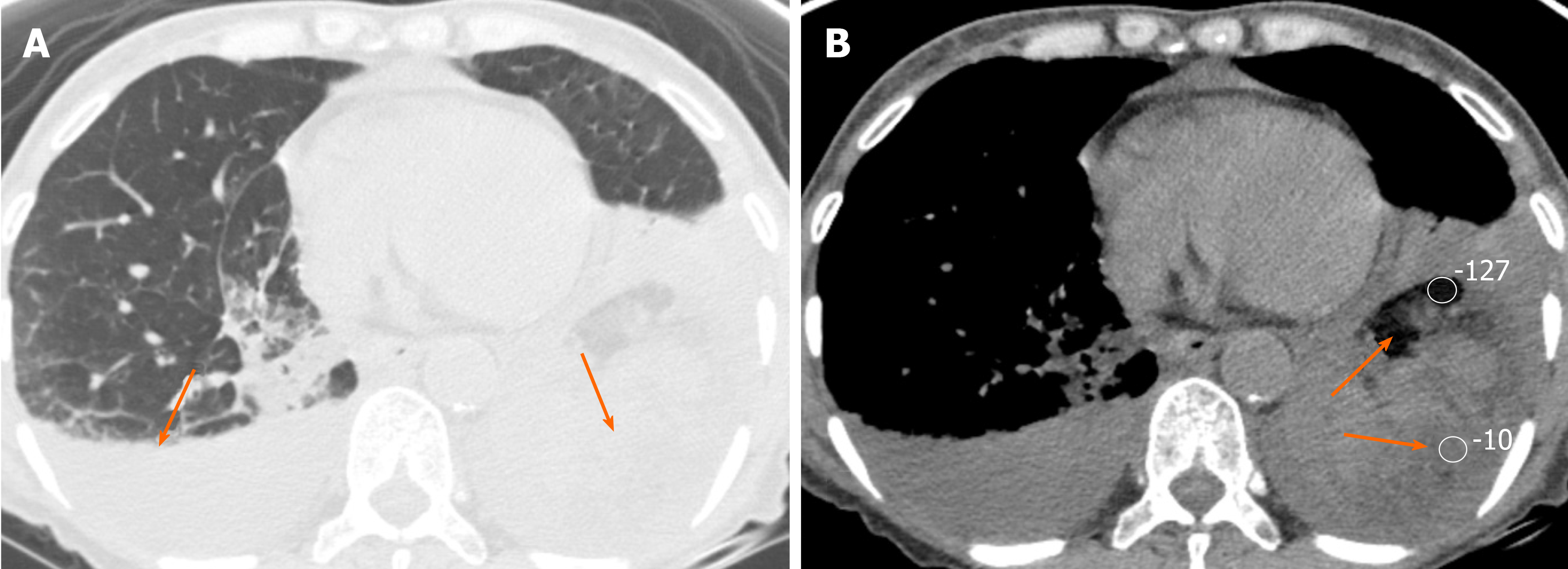
Lipoid pneumonia is uncommon and can mimic the clinical and imaging features of other lung diseases, including primary lung carcinoma. Imaging findings of lipoid pneumonia include chronic consolidative and GGOs as well as nodules and masses, more in the dependent portions of the lungs, and the possible presence of fatty attenuation[39] (Figure 16). Fatty attenuation may be absent, especially in the setting of chronic inflammation, and therefore tissue sampling may be needed to exclude malignancy[40]. Lipoid pneumonia can be exogeneous secondary to aspiration of oily materials or endogenous because of chronic accumulation of lipid substances, usually in the setting of chronic inflammation[39] (Table 4).
Treatment is supportive and also targets the underlying chronic inflammatory condition in the primary form or chronic aspiration in the secondary form[40].
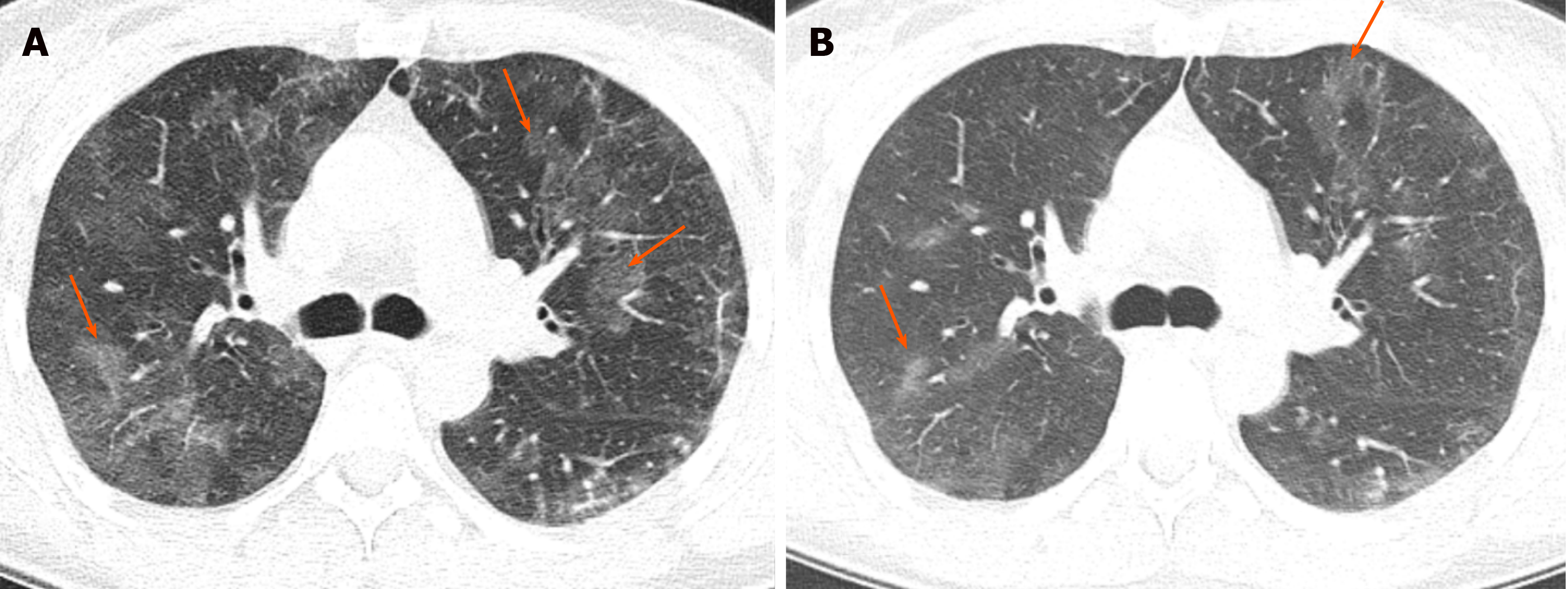
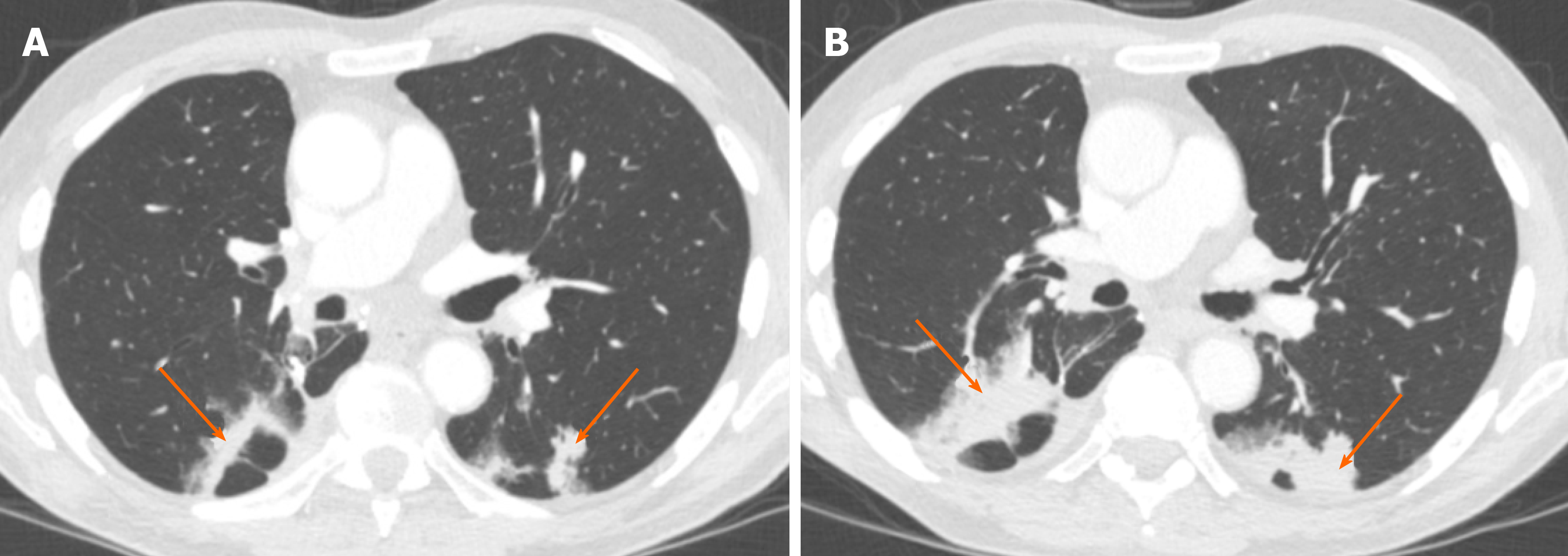
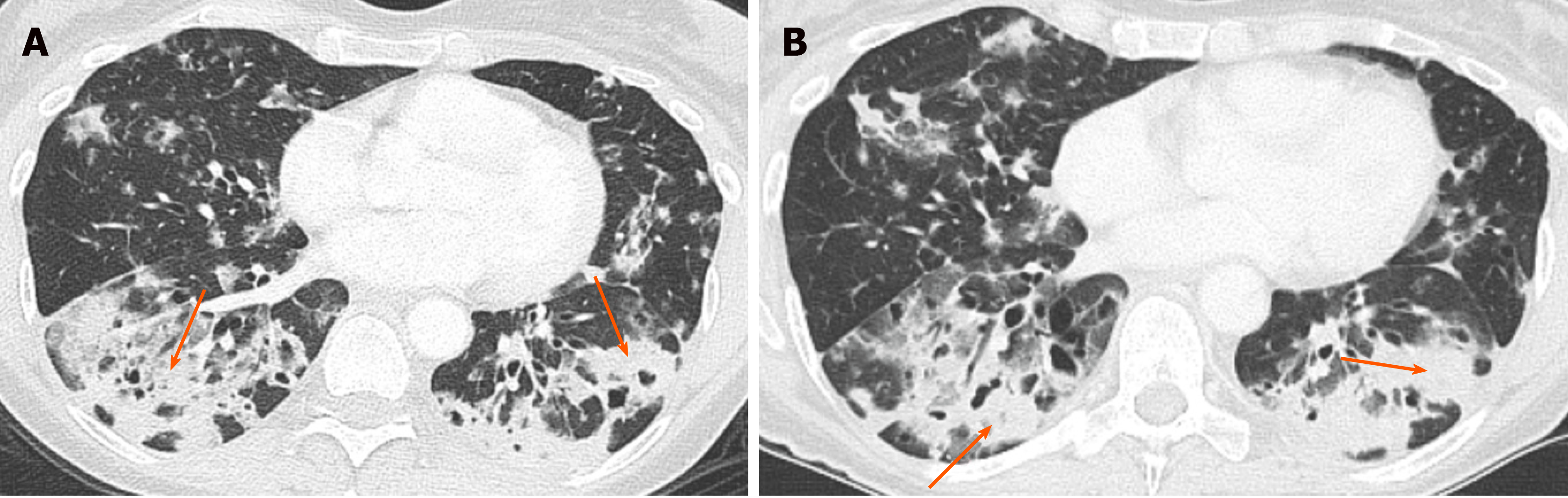
Pulmonary hemorrhage can be diffuse or localized. It can be due to a vast number of clinical situations, including pulmonary vasculitides, connective tissue disorders, coagulation disorders, and anticoagulation medication. The condition can also be life threatening, especially when diffuse[41].
In the acute phase, bleeding into the alveoli can range from GGO to consolidation[41]. Interlobular septa may remain dark as they are not filled with blood or fluid in the acute phase. The distribution and severity of opacification can change with time (Figure 17). In the subacute phase, interlobular septal thickening can be superimposed on GGO and may sometimes cause crazy-paving appearance[7]. Subpleural sparing can be seen in both acute and subacute phases[7]. Chronic recurrent bleeding can cause ill-defined centrilobular nodules, and pulmonary fibrosis if long standing[42].
Treatment of pulmonary hemorrhage is supportive and addresses the underlying etiology.
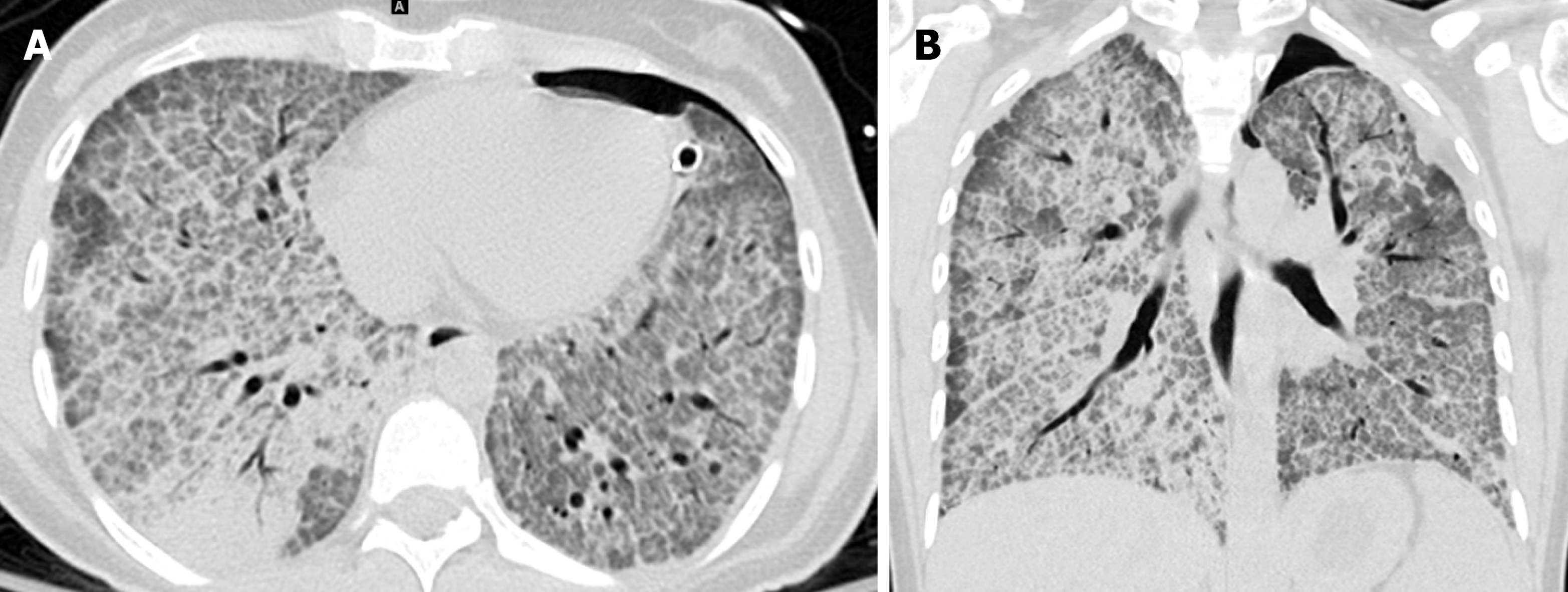
Pulmonary alveolar preoteinosis is a rare disease characterized by abnormal intra-alveolar accumulation of surfactant-like material[43]. The characteristic imaging finding of pulmonary alveolar preoteinosis on CT is crazy-paving, due to combination of GGO and smooth interlobular septal thickening[44] (Figure 18). Although this finding is very suggestive, it is not pathognomonic and many other infectious, hemorrhagic, neoplastic, inhalational and idiopathic conditions can produce the same pattern[44,45]. It is usually widespread and bilateral, with slight lower lung predominance[45]. The severity and extent of GGO or consolidation on CT correlates with severity of compromised pulmonary functional parameters[45]. In addition to crazy-paving, areas of consolidation may be seen[44].
Whole-lung bronchoalveolar lavage is used to remove alveolar material. The prognosis is variable, ranging from improvement with treatment to a chronic and terminal course[44].
The key imaging findings and imaging signs in chronic airspace disease are summarized in Table 5.
Chronic airspace diseases can cause significant diagnostic challenge due to significant overlap in their imaging findings. Knowing the imaging features and combining them with the clinical and laboratory findings can be helpful in steering the radiologist to the correct diagnosis.
Manuscript source: Unsolicited manuscript
Specialty type: Radiology, Nuclear Medicine and Medical Imaging
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent):
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair):
Grade E (Poor):
P-Reviewer: Yang L, Huerta-Franco MR S-Editor: van Velkinburgh JC L-Editor: A E-Editor: Liu MY
| 1. | Collins J. CT signs and patterns of lung disease. Radiol Clin North Am. 2001;39:1115-1135. [PubMed] |
| 2. | Johkoh T, Ikezoe J, Kohno N, Takeuchi N, Ichikado K, Arisawa J, Nakamura H, Hayaishi M. Usefulness of high-resolution CT for differential diagnosis of multi-focal pulmonary consolidation. Radiat Med. 1996;14:139-146. [PubMed] |
| 3. | Austin JH, Müller NL, Friedman PJ, Hansell DM, Naidich DP, Remy-Jardin M, Webb WR, Zerhouni EA. Glossary of terms for CT of the lungs: recommendations of the Nomenclature Committee of the Fleischner Society. Radiology. 1996;200:327-331. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 621] [Cited by in RCA: 584] [Article Influence: 20.1] [Reference Citation Analysis (1)] |
| 4. | Battesti JP, Saumon G, Valeyre D, Amouroux J, Pechnick B, Sandron D, Georges R. Pulmonary sarcoidosis with an alveolar radiographic pattern. Thorax. 1982;37:448-452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 39] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | Sharma SK, Soneja M, Sharma A, Sharma MC, Hari S. Rare manifestations of sarcoidosis in modern era of new diagnostic tools. Indian J Med Res. 2012;135:621-629. [PubMed] |
| 6. | Marchiori E, Zanetti G, Hochhegger B, Irion KL. Sarcoidosis and the reversed halo sign. Radiographics. 2011;31:892-893; author reply 893. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Johkoh T, Itoh H, Müller NL, Ichikado K, Nakamura H, Ikezoe J, Akira M, Nagareda T. Crazy-paving appearance at thin-section CT: spectrum of disease and pathologic findings. Radiology. 1999;211:155-160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 181] [Cited by in RCA: 137] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 8. | Gera K, Gupta N, Ahuja A, Shah A. Acute alveolar sarcoidosis presenting with hypoxaemic respiratory failure. BMJ Case Rep. 2014;2014. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Jeong YJ, Kim KI, Seo IJ, Lee CH, Lee KN, Kim KN, Kim JS, Kwon WJ. Eosinophilic lung diseases: a clinical, radiologic, and pathologic overview. Radiographics. 2007;27:617-637; discussion 637-639. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 190] [Cited by in RCA: 157] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 10. | Fox B, Seed WA. Chronic eosinophilic pneumonia. Thorax. 1980;35:570-580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 55] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 11. | Lee KS, Kullnig P, Hartman TE, Müller NL. Cryptogenic organizing pneumonia: CT findings in 43 patients. AJR Am J Roentgenol. 1994;162:543-546. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 220] [Cited by in RCA: 179] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 12. | Kim SJ, Lee KS, Ryu YH, Yoon YC, Choe KO, Kim TS, Sung KJ. Reversed halo sign on high-resolution CT of cryptogenic organizing pneumonia: diagnostic implications. AJR Am J Roentgenol. 2003;180:1251-1254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 222] [Cited by in RCA: 207] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 13. | Worthy SA, Müller NL, Hansell DM, Flower CD. Churg-Strauss syndrome: the spectrum of pulmonary CT findings in 17 patients. AJR Am J Roentgenol. 1998;170:297-300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 74] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 14. | Mayberry JP, Primack SL, Müller NL. Thoracic manifestations of systemic autoimmune diseases: radiographic and high-resolution CT findings. Radiographics. 2000;20:1623-1635. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 47] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 15. | Rossi SE, Erasmus JJ, McAdams HP, Sporn TA, Goodman PC. Pulmonary drug toxicity: radiologic and pathologic manifestations. Radiographics. 2000;20:1245-1259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 336] [Cited by in RCA: 269] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 16. | Nishino M, Hatabu H, Hodi FS, Ramaiya NH. Drug-Related Pneumonitis in the Era of Precision Cancer Therapy. J Clin Oncol. 2017;1-12. [RCA] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 17. | Connolly JE Jr, McAdams HP, Erasmus JJ, Rosado-de-Christenson ML. Opportunistic fungal pneumonia. J Thorac Imaging. 1999;14:51-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 40] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 18. | Orlowski HLP, McWilliams S, Mellnick VM, Bhalla S, Lubner MG, Pickhardt PJ, Menias CO. Imaging Spectrum of Invasive Fungal and Fungal-like Infections. Radiographics. 2017;37:1119-1134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 90] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 19. | Godoy MC, Viswanathan C, Marchiori E, Truong MT, Benveniste MF, Rossi S, Marom EM. The reversed halo sign: update and differential diagnosis. Br J Radiol. 2012;85:1226-1235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 110] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 20. | Franquet T, Müller NL, Giménez A, Guembe P, de La Torre J, Bagué S. Spectrum of pulmonary aspergillosis: histologic, clinical, and radiologic findings. Radiographics. 2001;21:825-837. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 289] [Cited by in RCA: 237] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 21. | Jeong YJ, Lee KS. Pulmonary tuberculosis: up-to-date imaging and management. AJR Am J Roentgenol. 2008;191:834-844. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 213] [Cited by in RCA: 207] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 22. | Cassidy PM, Hedberg K, Saulson A, McNelly E, Winthrop KL. Nontuberculous mycobacterial disease prevalence and risk factors: a changing epidemiology. Clin Infect Dis. 2009;49:e124-e129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 258] [Cited by in RCA: 300] [Article Influence: 20.0] [Reference Citation Analysis (0)] |
| 23. | Field SK, Fisher D, Cowie RL. Mycobacterium avium complex pulmonary disease in patients without HIV infection. Chest. 2004;126:566-581. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 228] [Cited by in RCA: 216] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 24. | Hidalgo A, Falcó V, Mauleón S, Andreu J, Crespo M, Ribera E, Pahissa A, Cáceres J. Accuracy of high-resolution CT in distinguishing between Pneumocystis carinii pneumonia and non- Pneumocystis carinii pneumonia in AIDS patients. Eur Radiol. 2003;13:1179-1184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 60] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 25. | Catherinot E, Lanternier F, Bougnoux ME, Lecuit M, Couderc LJ, Lortholary O. Pneumocystis jirovecii Pneumonia. Infect Dis Clin North Am. 2010;24:107-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 149] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 26. | Kanne JP, Yandow DR, Meyer CA. Pneumocystis jiroveci pneumonia: high-resolution CT findings in patients with and without HIV infection. AJR Am J Roentgenol. 2012;198:W555-W561. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 152] [Cited by in RCA: 160] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 27. | Smego RA Jr, Nagar S, Maloba B, Popara M. A meta-analysis of salvage therapy for Pneumocystis carinii pneumonia. Arch Intern Med. 2001;161:1529-1533. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 61] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 28. | Kandathil A, Kay FU, Butt YM, Wachsmann JW, Subramaniam RM. Role of FDG PET/CT in the Eighth Edition of TNM Staging of Non-Small Cell Lung Cancer. Radiographics. 2018;38:2134-2149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 115] [Article Influence: 19.2] [Reference Citation Analysis (0)] |
| 29. | Lee KS, Kim Y, Han J, Ko EJ, Park CK, Primack SL. Bronchioloalveolar carcinoma: clinical, histopathologic, and radiologic findings. Radiographics. 1997;17:1345-1357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 94] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 30. | Liu Y, Wang H, Li Q, McGettigan MJ, Balagurunathan Y, Garcia AL, Thompson ZJ, Heine JJ, Ye Z, Gillies RJ, Schabath MB. Radiologic Features of Small Pulmonary Nodules and Lung Cancer Risk in the National Lung Screening Trial: A Nested Case-Control Study. Radiology. 2018;286:298-306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 55] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 31. | Travis WD, Brambilla E, Noguchi M, Nicholson AG, Geisinger KR, Yatabe Y, Beer DG, Powell CA, Riely GJ, Van Schil PE, Garg K, Austin JH, Asamura H, Rusch VW, Hirsch FR, Scagliotti G, Mitsudomi T, Huber RM, Ishikawa Y, Jett J, Sanchez-Cespedes M, Sculier JP, Takahashi T, Tsuboi M, Vansteenkiste J, Wistuba I, Yang PC, Aberle D, Brambilla C, Flieder D, Franklin W, Gazdar A, Gould M, Hasleton P, Henderson D, Johnson B, Johnson D, Kerr K, Kuriyama K, Lee JS, Miller VA, Petersen I, Roggli V, Rosell R, Saijo N, Thunnissen E, Tsao M, Yankelewitz D. International association for the study of lung cancer/american thoracic society/european respiratory society international multidisciplinary classification of lung adenocarcinoma. J Thorac Oncol. 2011;6:244-285. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3651] [Cited by in RCA: 3627] [Article Influence: 259.1] [Reference Citation Analysis (0)] |
| 32. | Cohen JG, Reymond E, Jankowski A, Brambilla E, Arbib F, Lantuejoul S, Ferretti GR. Lung adenocarcinomas: correlation of computed tomography and pathology findings. Diagn Interv Imaging. 2016;97:955-963. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 34] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 33. | Austin JH, Garg K, Aberle D, Yankelevitz D, Kuriyama K, Lee HJ, Brambilla E, Travis WD. Radiologic implications of the 2011 classification of adenocarcinoma of the lung. Radiology. 2013;266:62-71. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 156] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 34. | Lewis ER, Caskey CI, Fishman EK. Lymphoma of the lung: CT findings in 31 patients. AJR Am J Roentgenol. 1991;156:711-714. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 75] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 35. | Raman SP, Pipavath SN, Raghu G, Schmidt RA, Godwin JD. Imaging of thoracic lymphatic diseases. AJR Am J Roentgenol. 2009;193:1504-1513. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 35] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 36. | Halkos ME, Miller JI, Mann KP, Miller DL, Gal AA. Thoracic presentations of posttransplant lymphoproliferative disorders. Chest. 2004;126:2013-2020. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 31] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 37. | Kaushik S, Fulcher AS, Frable WJ, May DA. Posttransplantation lymphoproliferative disorder: osseous and hepatic involvement. AJR Am J Roentgenol. 2001;177:1057-1059. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 38. | Seo JB, Im JG, Goo JM, Chung MJ, Kim MY. Atypical pulmonary metastases: spectrum of radiologic findings. Radiographics. 2001;21:403-417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 289] [Cited by in RCA: 236] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 39. | Ansari-Gilani K, Faraji N, Gilkeson RC. Increased FDG Uptake and Chronic Lung Changes in a Case of Persistent Lipoid Pneumonia. Clin Nucl Med. 2018;43:e477-e478. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 40. | Betancourt SL, Martinez-Jimenez S, Rossi SE, Truong MT, Carrillo J, Erasmus JJ. Lipoid pneumonia: spectrum of clinical and radiologic manifestations. AJR Am J Roentgenol. 2010;194:103-109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 142] [Cited by in RCA: 140] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 41. | Cortese G, Nicali R, Placido R, Gariazzo G, Anrò P. Radiological aspects of diffuse alveolar haemorrhage. Radiol Med. 2008;113:16-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 22] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 42. | Engelke C, Schaefer-Prokop C, Schirg E, Freihorst J, Grubnic S, Prokop M. High-resolution CT and CT angiography of peripheral pulmonary vascular disorders. Radiographics. 2002;22:739-764. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 46] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 43. | Katzenstein ALA. Katzenstein and Askin's surgical pathology of non-neoplastic lung disease. 4th ed. Philadelphia, Pa: Saunders Elsevier, 2006. |
| 44. | Holbert JM, Costello P, Li W, Hoffman RM, Rogers RM. CT features of pulmonary alveolar proteinosis. AJR Am J Roentgenol. 2001;176:1287-1294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 95] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 45. | Frazier AA, Franks TJ, Cooke EO, Mohammed TL, Pugatch RD, Galvin JR. From the archives of the AFIP: pulmonary alveolar proteinosis. Radiographics. 2008;28:883-899; quiz 915. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 68] [Article Influence: 4.0] [Reference Citation Analysis (0)] |