Published online Dec 28, 2020. doi: 10.4329/wjr.v12.i12.316
Peer-review started: March 26, 2020
First decision: October 21, 2020
Revised: November 4, 2020
Accepted: November 28, 2020
Article in press: November 28, 2020
Published online: December 28, 2020
Processing time: 276 Days and 19.3 Hours
Malignant peritoneal mesothelioma is an unusual disease process characterized radiologically by ascites and infiltration of the peritoneum by multiple small tumor nodules. Both parietal and visceral peritoneum are involved by the multiple malignant tumor nodules. Computed tomography (CT) has been used to identify the anatomic pathology induced by the progression of this malignant process.
To identify and then describe unusual CT images in patients with malignant peritoneal mesothelioma. Recognition of these unusual radiologic findings can cause the radiologist to be suspicious of this rare malignant process.
In 100 patients who were to undergo definitive treatment of malignant peritoneal mesothelioma, the findings on preoperative CT scans were catalogued. Many of these changes were repeatedly noted on the CT scans. Other pathologic CT images were less common. These unusual radiologic presentations were specially studied in this manuscript.
Eight unusual radiologic presentations of malignant peritoneal mesothelioma were selected for study. These unusual findings included a mass occurring within a Spigelian hernia, infiltration of the splenic parenchyma by spherical mesothelioma masses, infiltration of the lower mediastinum by tumor, a mesothelioma mass within a left inguinal canal, enlarged cardiophrenic angle lymph nodes, pleural plaques associated with the progression of malignant peritoneal mesothelioma, splenic notches caused by disease surrounding the spleen, and a mass greater than 5 cm associated with the proximal jejunum and directly adjacent to the anatomic location of the Treitz ligament.
There are unusual radiologic presentations of malignant peritoneal mesothelioma that are important to recognize in order to accurately diagnose this disease by CT.
Core Tip: Malignant peritoneal mesothelioma is an unusual disease process characterized radiologically by ascites and infiltration of the peritoneum by multiple small tumor nodules. Both parietal and visceral peritoneum are involved by the multiple malignant tumor nodules. There are unusual radiologic presentations of malignant peritoneal mesothelioma that are important to recognize in order to accurately diagnose this disease by computed tomography.
- Citation: Sugarbaker PH, Jelinek JS. Unusual radiologic presentations of malignant peritoneal mesothelioma. World J Radiol 2020; 12(12): 316-326
- URL: https://www.wjgnet.com/1949-8470/full/v12/i12/316.htm
- DOI: https://dx.doi.org/10.4329/wjr.v12.i12.316
Our recent manuscript surveyed the preoperative computed tomography (CT) in 100 patients definitively treated by cytoreductive surgery and hyperthermic intraperitoneal chemotherapy (HIPEC) for malignant peritoneal mesothelioma[1]. The most common radiologic finding in the CT of patients with malignant peritoneal mesothelioma is ascites. This prior report indicated that 43% of patients had ascites[2]. The second most common radiologic finding was an infiltration of the small bowel mesentery by tumor reported in 41% of patients[2]. Other abnormalities depicted less frequently was infiltration of the greater omentum by tumor (29%), a mass of mesothelioma infiltrating the deep pelvis (21%), a mass in the porta hepatis and lesser omentum (15%), clumped bowel (16%) and obstructed bowel (7%).
However, other less frequent radiologic findings were depicted in these 100 patients studied. These unusual findings are important in a full description of the radiology of malignant peritoneal mesothelioma and are the subject of this manuscript.
In these 100 patients with malignant peritoneal mesothelioma, an exhaustive review of their radiologic findings was conducted. All patients had their cancer diagnosis confirmed by tissue biopsy. An experienced pathologist reported a histomorphology that showed an epithelial type of cell that invades through the peritoneum to underlying tissues. Stromal invasion was most frequently observed into the fat beneath visceral and/or parietal peritoneum. In all patients, immunohistochemistry was performed that was routinely positive for calretinin and cytokeratin 5/6 but negative for carcinoembryonic antigen (CEA).
Peritoneal Cancer Index (PCI score) was used intraoperatively to assess the extent of peritoneal metastases at the time of surgical exploration of the abdomen and pelvis[3]. This assessment determines the size of peritoneal nodules in 13 abdominopelvic regions within the open abdomen at the time of cytoreductive surgery. The score ranges from 0 (no visible disease) to 39 (tumor greater than 5 cm in all abdominopelvic regions. The goal of surgery in all patients was complete cytoreduction with no visible evidence of disease at the completion of the surgery. The completeness of cytoreduction score was determined after the cytoreductive surgery was completed[3]. Complete cytoreduction was indicated by CC-0; there was no peritoneal metastases visualized within the operative field at the completion of the surgical procedure. CC-1 indicated nodules persisting after cytoreduction less than 2.5 cm. A CC-2 cytoreduction indicated nodules between 2.5 and 5 cm, and CC-3 nodules greater than 5 cm or unresectable tumor nodule at any site within the abdomen or pelvis.
In these 100 patients with malignant peritoneal mesothelioma CT was available within 10 d prior to a surgical procedure. The goal of the surgical intervention was the complete resection of all tumor followed by HIPEC[1]. In all of these patients with unusual CT findings, histopathologic confirmation of the radiologic abnormality as caused by malignant peritoneal mesothelioma occurred. This close temporal relationship of the CT and the surgical procedure allowed us to confirm the gross and histopathologic nature of the pathology depicted. Also, any accompanying disease present in these patients was determined. This allowed us to confirm that the unusual radiologic finding was part of the whole abdominal and pelvic disease process of malignant peritoneal mesothelioma. Permission from the institutional review board to collect and analyze data on malignant peritoneal mesothelioma patients was obtained.
The preoperative CT findings were studied in 100 patients with malignant peritoneal mesothelioma. The incidence of the most common abnormal images associated with malignant peritoneal mesothelioma was described in a prior manuscript[2]. The less frequent CT findings were catalogued along with the more common abnormal images. The incidence of the unusual CT findings in these 100 patients was determined for this study and is indicated for each unusual radiologic image.
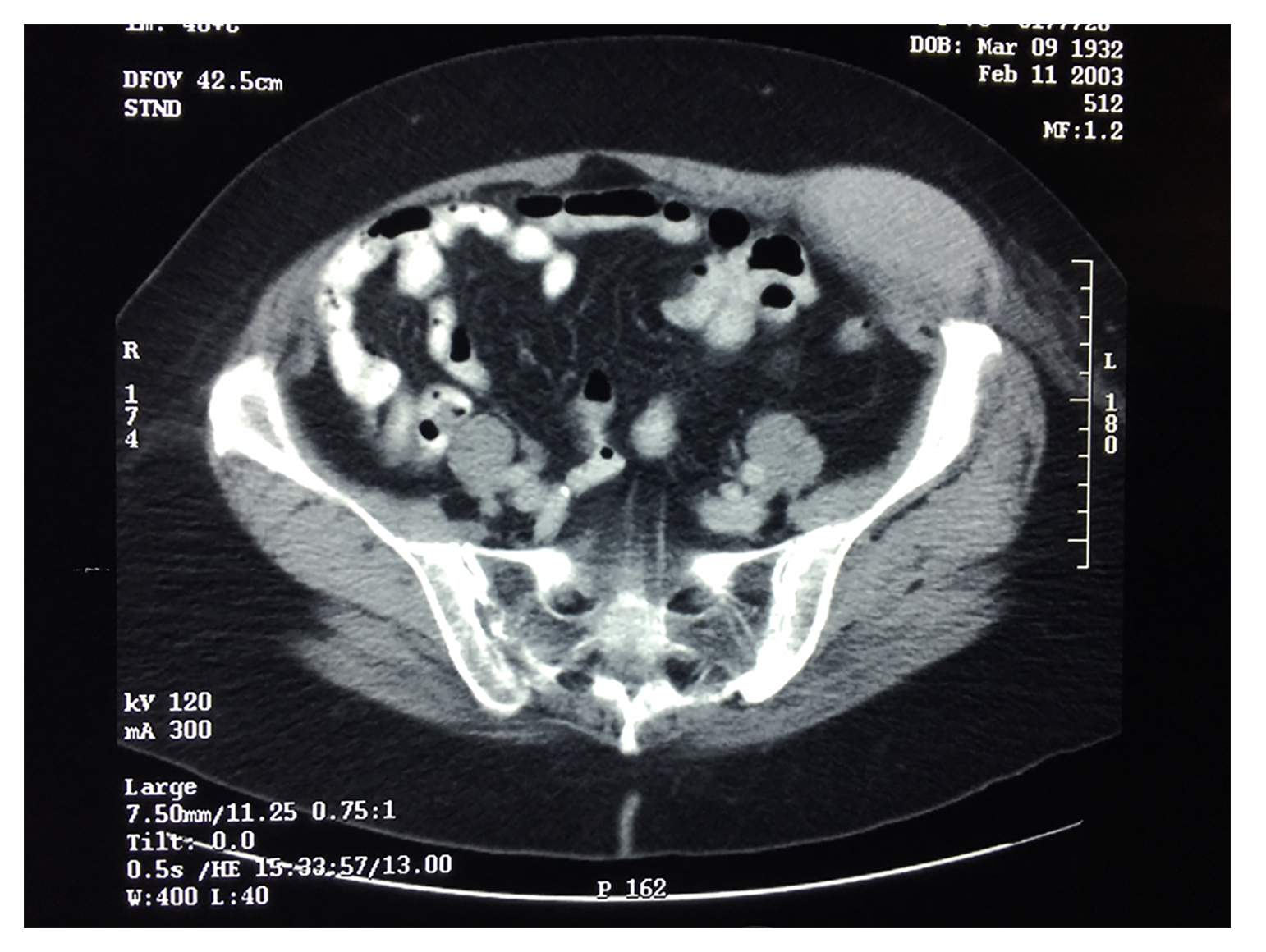
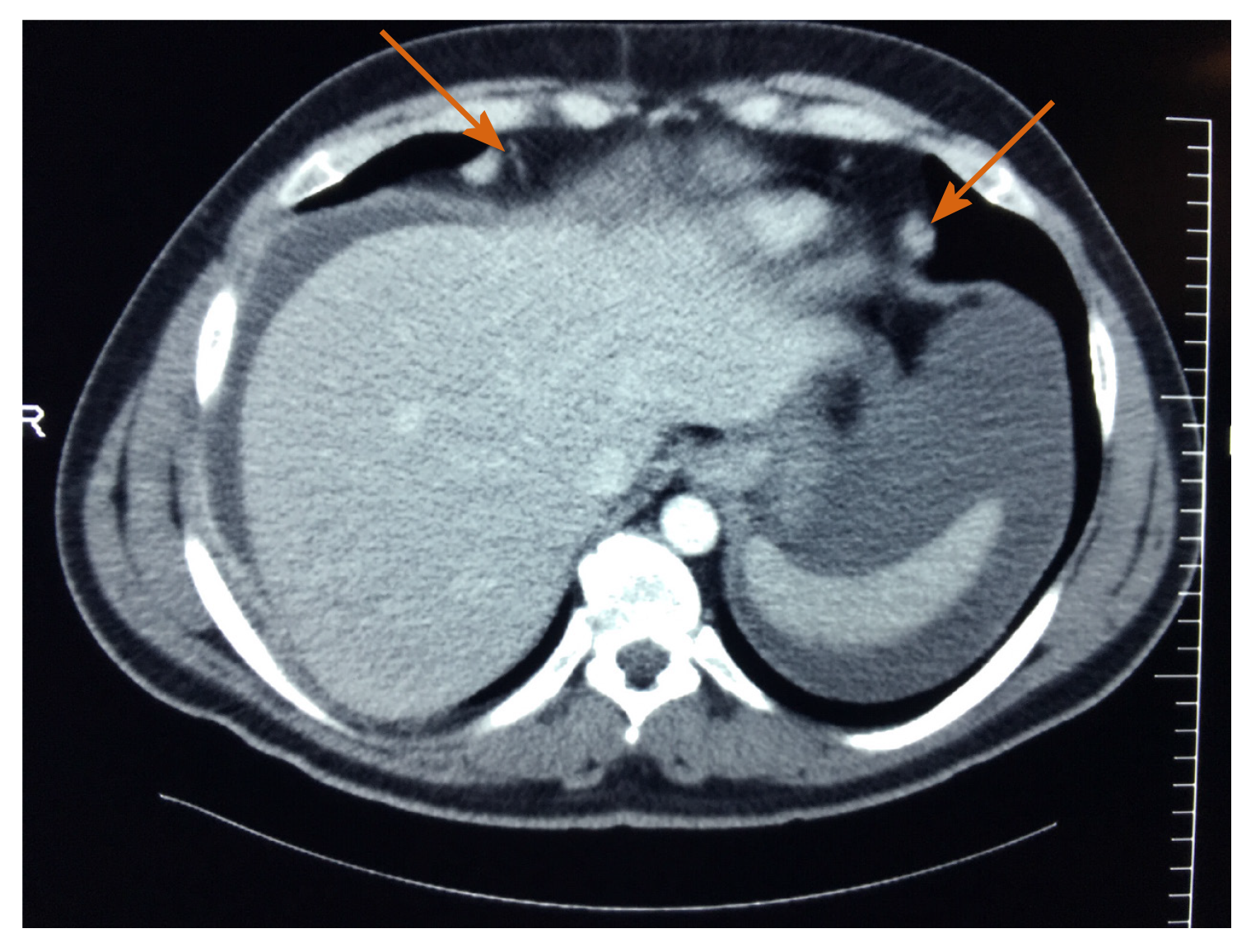
Patient 1: A large (8 cm diameter) mass was present within the abdominal wall at the site of the intersection of the left semilunar line and semicircular line. This image was recorded in a single patient (Figure 1). This mass occurred in a 70-year-old woman with no history of asbestos exposure who had no other complaints. Radiologically, the mass was determined to be solid (non-cystic) emanating from within the space defined by a Spigelian hernia[4]. Percutaneous biopsy revealed malignant peritoneal mesothelioma. At the time of cytoreductive surgery other sites of tumor resected along with this abdominal wall mass were greater omentum, spleen, uterus and ovaries, and rectosigmoid colon. These sites of smaller volume disease were not imaged on the preoperative CT. By histopathologic study, the large mass in the left inguinal region was completely composed of epithelial malignant peritoneal mesothelioma. The patient was treated with cytoreductive surgery and HIPEC according to the standard of care[1]. She died of disease 22 mo after the initiation of treatment.
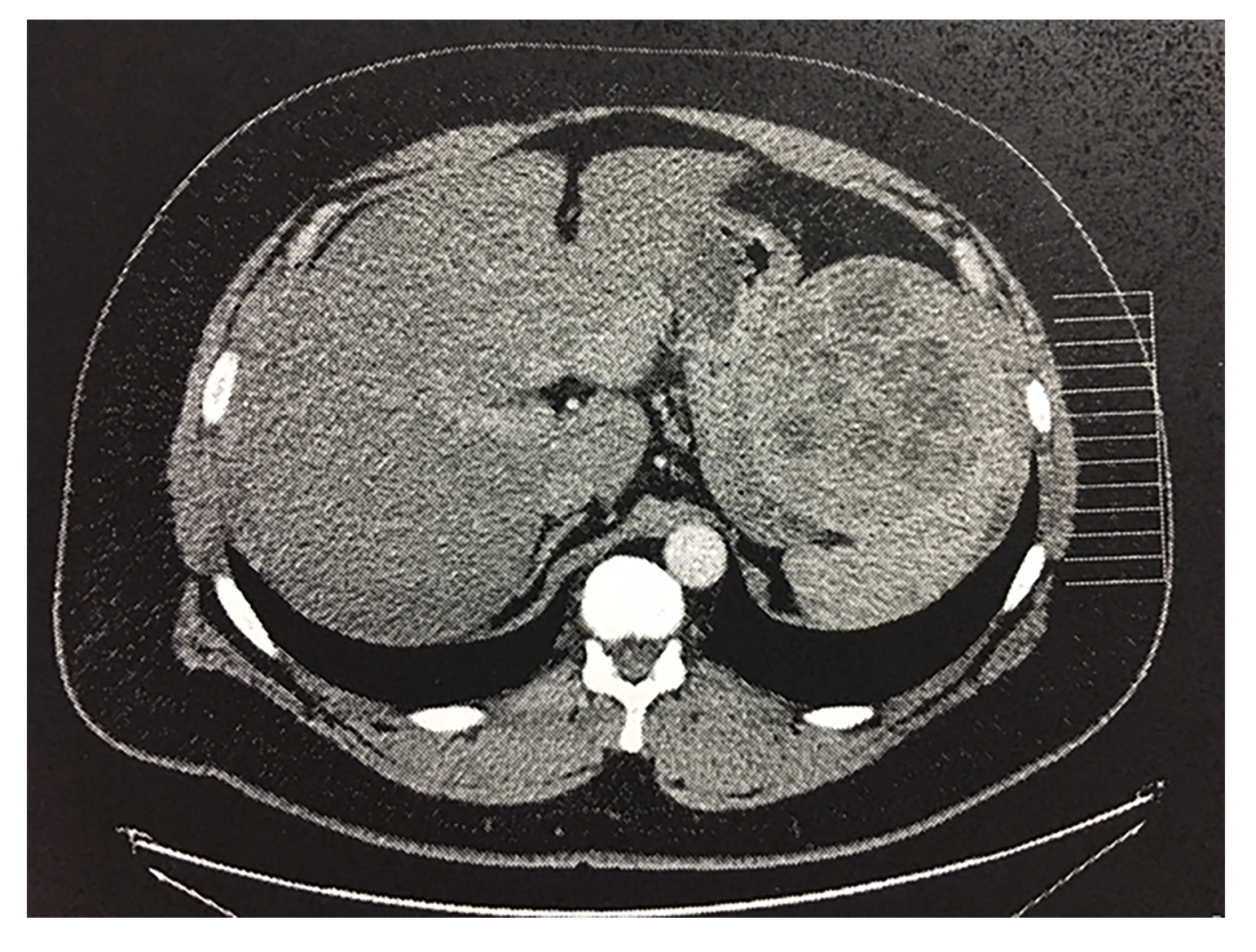
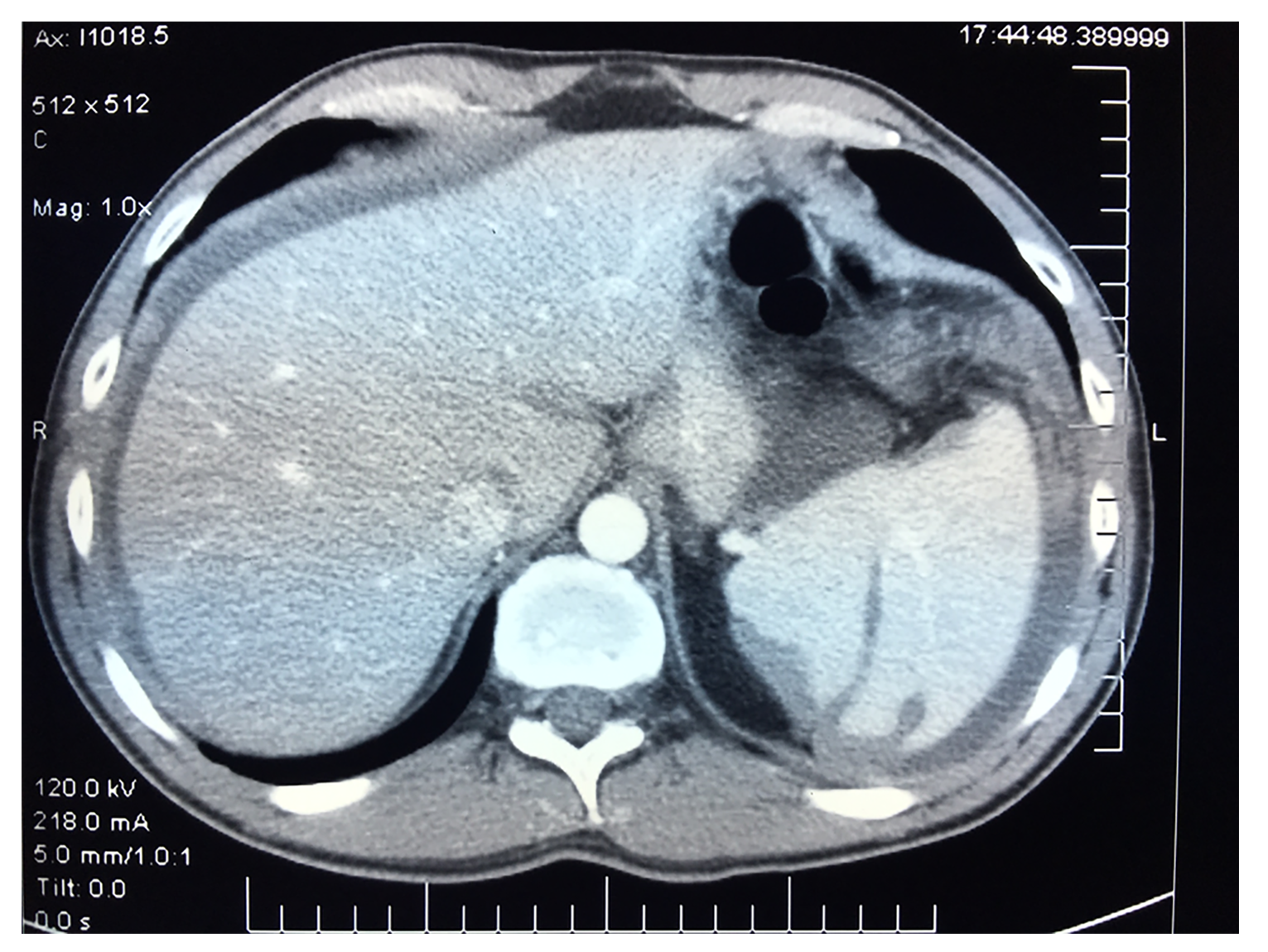
Patient 2: In a 43-year-old Hispanic male three large spherical masses were intimately associated with the spleen. The largest measured 11 cm in diameter (Figure 2). His symptom that cause the CT to be performed was intractable vomiting. As a result of these symptoms, a laparoscopic examination was performed and tissue biopsies were taken. These showed malignant peritoneal mesothelioma. There was no history of asbestos exposure. Cytoreductive surgery combined with HIPEC was discussed with the patient and he elected to undergo these treatments. At the time of cytoreductive surgery other sites of disease resected along with the left upper quadrant mass was a layering of mesothelioma beneath the left hemidiaphragm and an infiltration of the greater omentum. He had a complete cytoreduction and standard perioperative chemotherapy. He remains alive and well 10 years and 3 mo after initiation of treatment. This patient was the only one with mesothelioma masses directly invading the spleen. Two other patients had intraabdominal masses greater than 5 cm associated with extensive mesothelioma at other sites within the abdomen and pelvis.
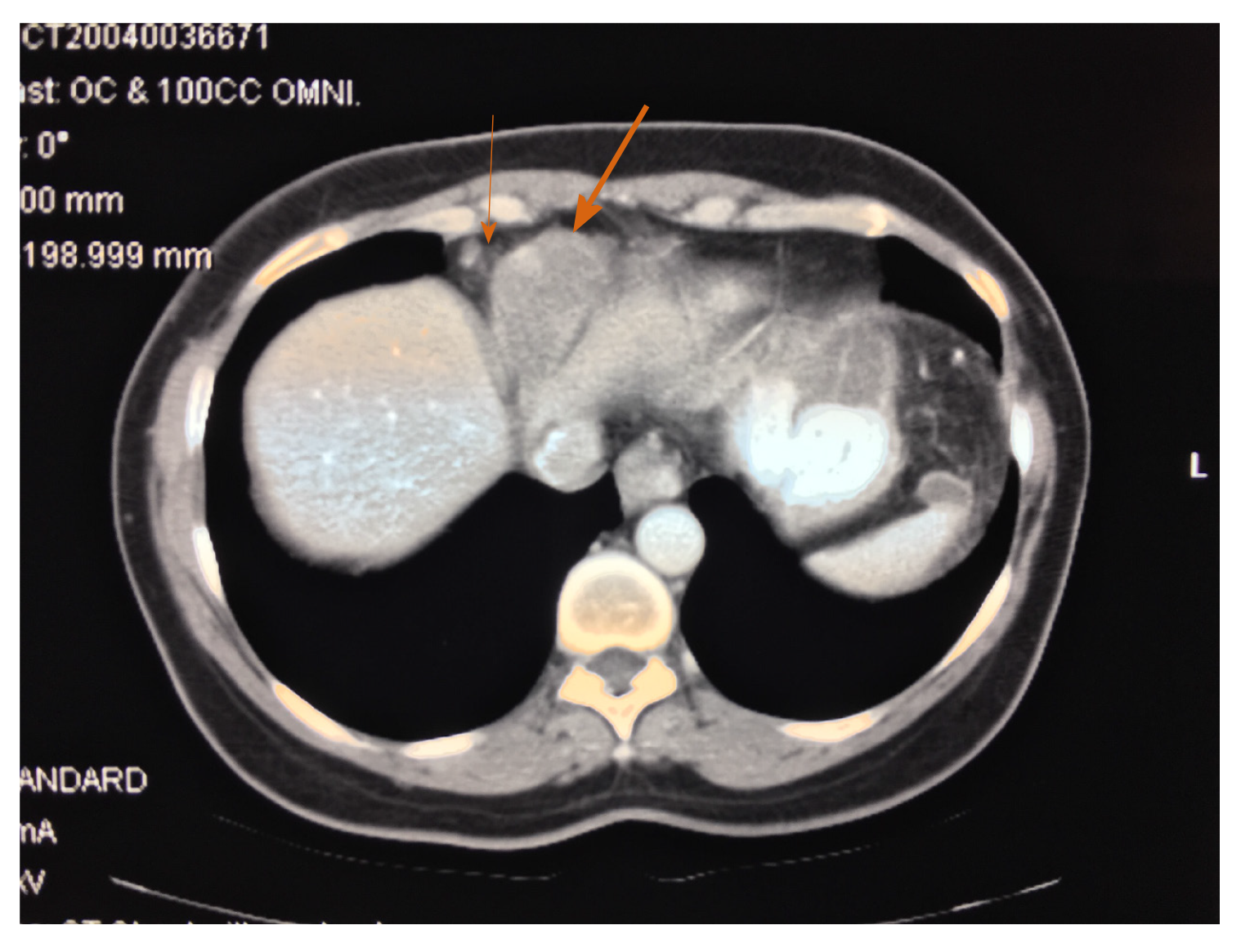
Patient 3: Another patient presenting with a mass lesion was a 48-year-old woman. Her initial complaint was pain in her right rib cage. CT showed a mass in the lower mediastinum superior to the right liver (Figure 3). There was not history of asbestos exposure. At the time of cytoreductive surgery smaller malignant peritoneal mesothelioma nodules were present diffusely on parietal and visceral peritoneal surfaces. Resection of the mass required removal of a portion of the pericardial sac and lower aspect of the right parietal pleura. This patient’s disease process may be accurately described as a combined malignant peritoneal and pericardial mesothelioma. Whether the disease is primary within the peritoneum, primary within the pericardium, or occurring at both sites simultaneously cannot be determined at this point in time. The patient died 6 years and 1 mo later of progressive disease. A second patient presented with a lower mediastinal mass more prominent on the right than left.
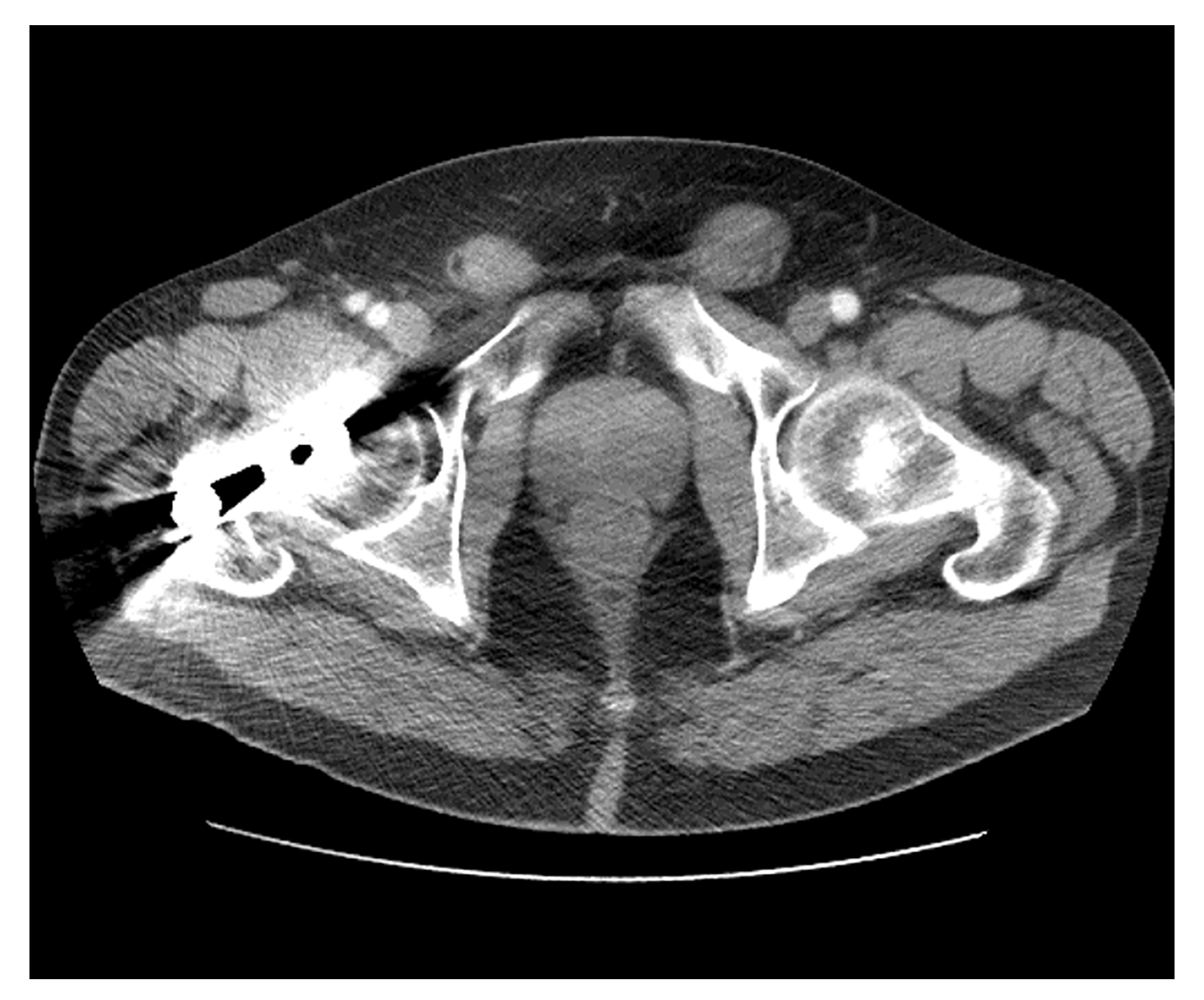
Patient 4: A 73-year-old male complained of a prominent right inguinal mass thought to be a right inguinal hernia. The mass was firm and non-reducible. He had no other complaints except rectosigmoid diverticulitis. In July of 2019, an attempt at laparoscopic right inguinal hernia repair revealed intraperitoneal fluid and nodules. There was no history of asbestos exposure. Biopsy showed malignant peritoneal mesothelioma. CT showed bilateral masses just above the symphysis pubis and thought to be within the inguinal canal (Figure 4). Cytoreductive surgery required extensive peritonectomy and rectosigmoid colon resection. At 5 mo postoperatively, the patient has recovered and is on adjuvant treatment[5].
Patient 5: A 37-year-old man presented with an inguinal hernia. Pathology showed an adenomatoid tumor which was considered a benign process. However, 10 mo later ascites developed with weight loss. In July of 2010, the patient had an exploratory laparotomy which showed extensive malignant peritoneal mesothelioma. There was no history of asbestos exposure. Preoperative CT showed moderate ascites and a thickened omentum but no gross disease. There were prominent bilateral cardiophrenic angle lymph nodes[6,7] approximately 1.5 cm in diameter depicted (Figure 5). In October of 2010, the patient had a 10-h cytoreductive surgery plus HIPEC. It was thought that ascites had caused extensive disease layered out on peritoneal surfaces to go undetected. The cardiophrenic lymph nodes were not resected. Currently, the patient is free of disease 9 years and 1 mo following definitive treatment. The cardiophrenic lymph nodes have not progressed in size.
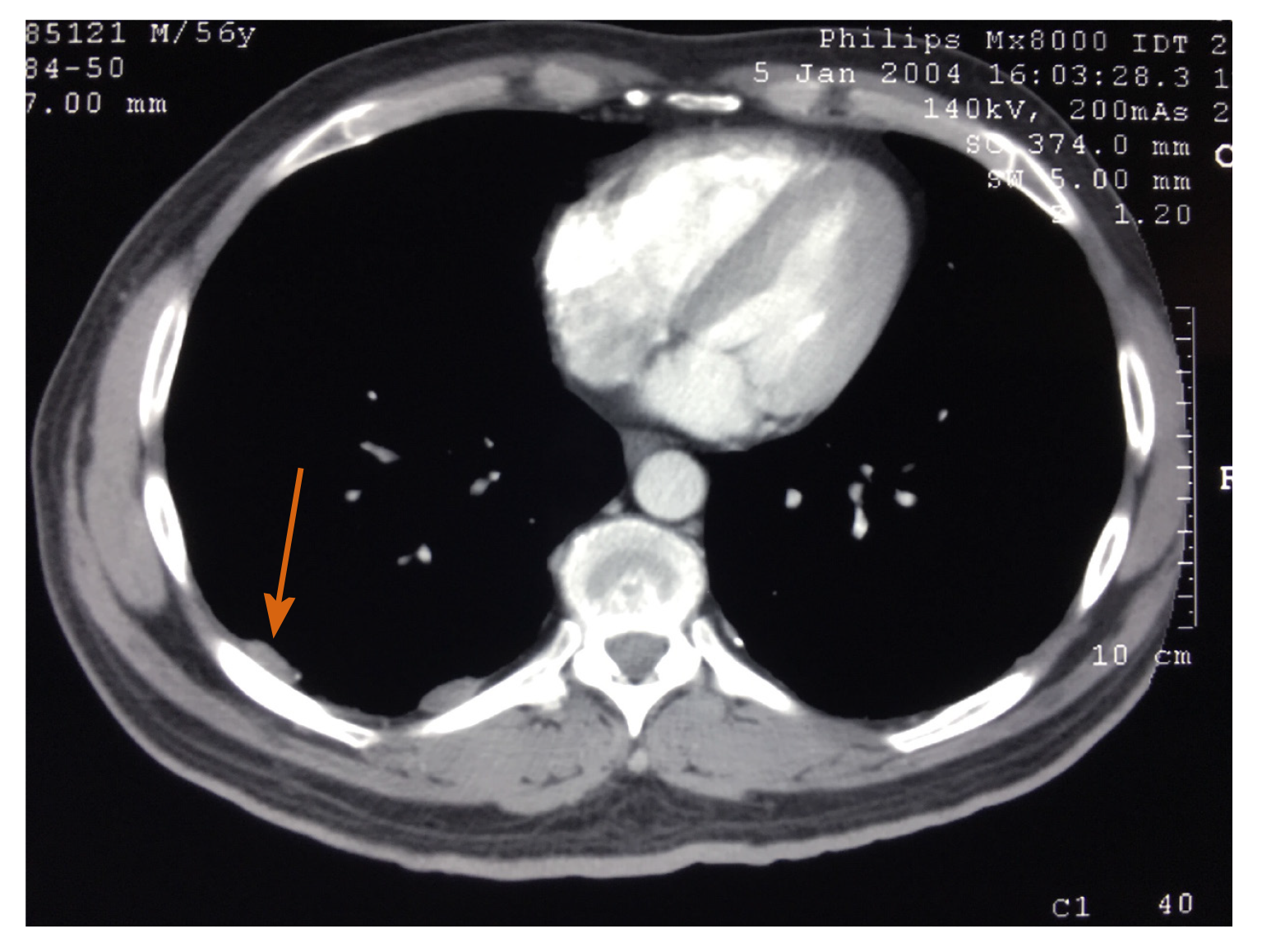
Patient 6: Pleural plaques are a radiologic sign of direct exposure to asbestos. A single patient with known prior asbestos exposure showed pleural plaques in the right hemithorax and was in a surveillance program for early detection of malignant mesothelioma. The CT examination was performed just prior to cytoreductive surgery plus HIPEC to treat malignant peritoneal mesothelioma (Figure 6). This 56-year-old man developed ascites and some weight loss. Laparoscopic biopsy was positive for peritoneal mesothelioma. Complete removal of all visible disease in the abdomen and pelvis required 11 h. Procedures performed included complete parietal peritonectomy, greater and lesser omentectomy and rectosigmoid colon resection with anastomosis[1]. He survived 7 years and 8 mo after definitive treatment. The pleural plaques did not progress to pleural mesothelioma. On other CT cuts a larger extent of calcification was present in the pleural plaques.
Patient 7: A 36-year-old otherwise healthy man complained of abdominal pain. A CT showed ascites and multiple soft tissue masses within the greater omentum. The spleen showed splenic notches infiltrated by tumor (Figure 7). No defects within the parenchyma of the spleen were depicted. Fine needle aspirate suggested a diagnosis of adenocarcinoma. A diagnosis of peritoneal carcinomatosis of unknown primary site was entertained. Exploratory laparotomy showed extensive disease on small bowel and small bowel mesentery and biopsy using the appropriate immunostains showed malignant peritoneal mesothelioma. There was no history of asbestos exposure. An incomplete cytoreduction was performed by resection of an extensive omental cake. The spleen was coated by tumor but was not removed. The patient was dead of progressive disease 17 mo after surgery. Palliation as a result of the debulking surgery occurred.
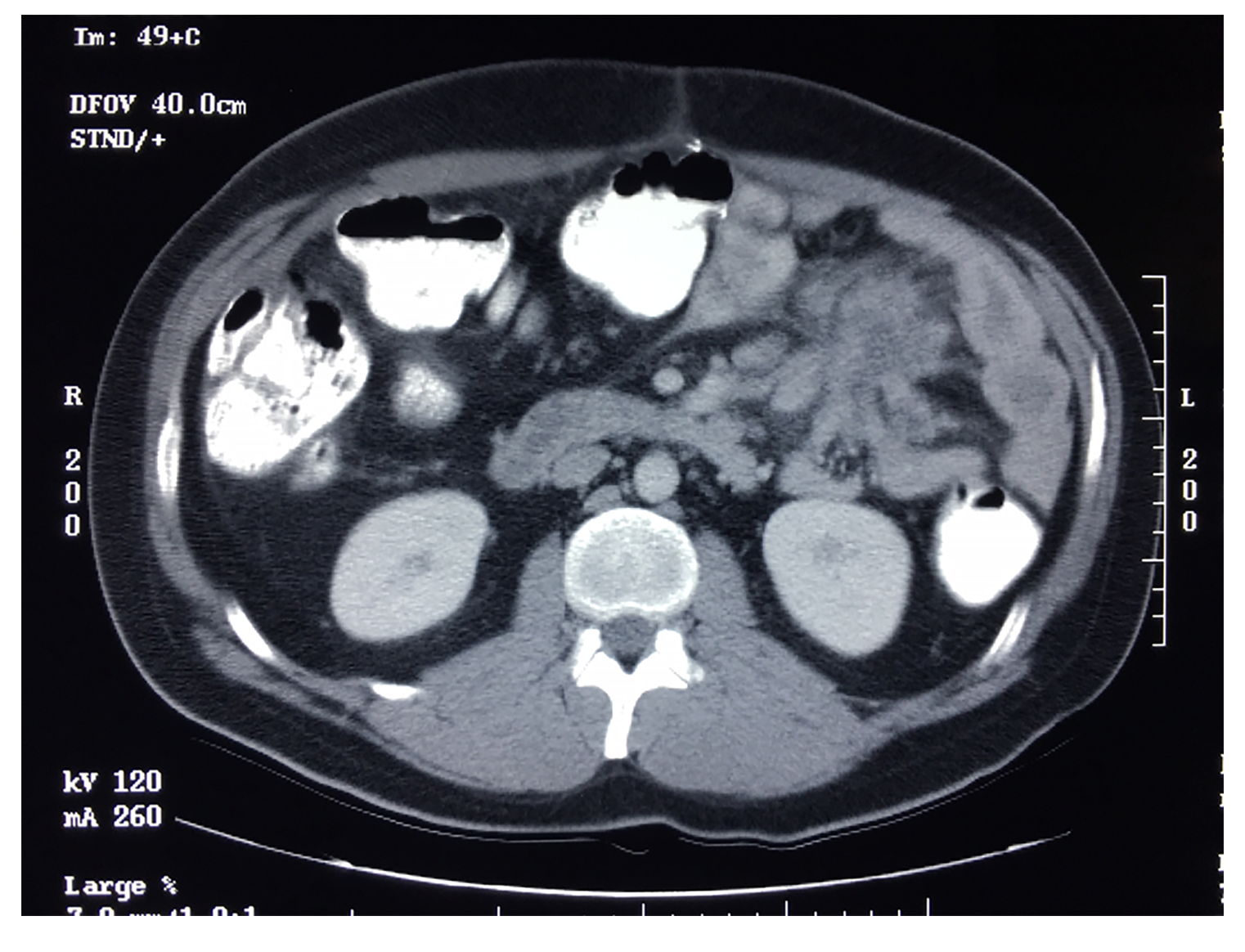
Patient 8: A 31-year-old man complained of abdominal pain. CT showed omental masses and he underwent a greater omentectomy at an outside hospital. A pathologic diagnosis of deciduoid malignant peritoneal mesothelioma was made. Because of increasing abdominal pain 2 mo later in May of 2001, he underwent a second more extensive surgery. CT preoperatively showed a mass adjacent the proximal jejunum (Figure 8). At surgery a proximal small bowel resection (estimated at 5 feet) was required to restore bowel continuity. The cytoreduction was estimated at complete but the aggressive cancer caused death from disease progression in 3 mo.
Only a single patient had malignant peritoneal mesothelioma presenting as a mass in a Spigelian hernia. Also, masses of malignant peritoneal mesothelioma infiltrating the spleen was only present in one of our 100 patients. However, 4 other patients had large (> 5 cm) intraabdominal masses for an incidence of 5%. The direct involvement of the lower mediastinum was seen in 2 patients (2%). Only a single patient presented with a malignant peritoneal mesothelioma mass in an inguinal hernia. The enlargement of pericardiophrenic angle lymph nodes greater than 1.5 cm was more common and was recorded in 10 patients (10%). Only one of the 100 patients had evidence of pleural plaques and only one had splenic notches. The mass lesion of greater than 5 cm immediately adjacent to the proximal jejunum was the most common unusual finding we chose to present with an incidence of 15% (Table 1). This unusual accumulation of tumor infiltrating proximal small bowel and mesocolon of the splenic flexure is, to our knowledge, a radiologic finding seen only in patients with malignant peritoneal mesothelioma.
| Patient | Age | Gender | Initial complaint | PCI | CC | Unusual CT Finding | Status | Survival (mo) | Incidence of CT findings (%) |
| 1 | 70 | F | Left lower abdominal wall mass | 23 | 1 | Mass within left Spigelian hernia belt | DOD | 22 | 1 |
| 2 | 43 | M | Intractable vomiting | 31 | 2 | Large splenic mass | NED | 98 | 5 |
| 3 | 48 | F | Right rib pain | 19 | 1 | Lower mediastinal mass | DOD | 73 | 2 |
| 4 | 73 | M | Right inguinal hernia | 20 | 1 | Bilateral masses in inguinal canals | NED | 3 | 1 |
| 5 | 37 | M | Umbilical hernia | 24 | 1 | Cardiophrenic angle lymph nodes > 1.5 cm | NED | 109 | 10 |
| 6 | 56 | M | Ascites | 18 | 1 | Pleural plaques | DOD | 92 | 1 |
| 7 | 36 | M | Abdominal pain | 33 | 3 | Notched spleen | DOD | 17 | 1 |
| 8 | 31 | M | Abdominal pain | 9 | 2 | Mass > 5 cm adjacent jejunum | DOD | 3 | 15 |
Malignant peritoneal mesothelioma is most often characterized on CT by ascites and multiple small tumor nodules layering out on the parietal and visceral pleura. However, in our review of the perioperative images of 100 patients, some large masses were apparent. In patient 1, the abdominal wall mass was at the intersection of the left semilunar line and the semicircular line. This is an anatomic site referred to as the Spigelian hernia belt[8]. It has been well established that malignant peritoneal mesothelioma can present as a new onset hernia[9]. The mass would progress in a predominantly lateral direction to reach the precise anatomic site for the mass in our patient 1[8].
In patient 4, a left inguinal mass thought to be an inguinal hernia was the chief complaint. Malignant peritoneal mesothelioma is associated with new onset hernia in approximately 20% of men diagnosed with malignant peritoneal mesothelioma[9]. However, the hernia bulge is nearly always a result of ascites accumulation under increased intraabdominal pressure. It is not commonly a solid tumor mass as in patient 4. Also, the CT is unusual in that the malignant peritoneal mesothelioma masses were bilateral. Bilateral inguinal canal tumor masses from malignant peritoneal mesothelioma have not been previously reported.
The three large masses seen in patient 2 and intimately associated with the spleen has not been previously reported with malignant peritoneal mesothelioma. A cause for major progression within the left upper quadrant as compared to small volume disease at multiple other sites within the abdomen and pelvis cannot be explained. One possible explanation concerns malignant peritoneal mesothelioma progression in contact with an extremely vascular structure like the spleen. It is possible that splenic invasion results in bleeding into a mesothelioma tumor mass and rapid expansion because of hemorrhage.
The mass present in the lower mediastinum in patient 3 was responsible for the patient’s initial symptoms. Complete resection required removal of a portion of the pericardium and right parietal pleura. A second patient had a lower mediastinal mass along with peritoneal mesothelioma at numerous other sites within the abdomen and pelvis. Also, in this second patient, resections of portions of the pericardium and right-sided parietal pleura were necessary. Whether mediastinal mesothelioma masses along with diffuse peritoneal disease is a result of invasion of peritoneal disease into the lower mediastinum or a dual origin of disease in the pericardium and peritoneum cannot be determined[10].
In our fifth patient with unusual CT images in malignant peritoneal mesothelioma, enlarged cardiophrenic lymph nodes were present. The significance of these enlarged nodes outside of the peritoneal space has not been clearly established in patients with peritoneal metastases or peritoneal mesothelioma. These lymph nodes are within 1-2 cm from the diaphragm and represent a major lymph drainage system of both the peritoneum and diaphragm muscle. Elias and coworkers in 114 patients with colorectal peritoneal metastases studied the impact of these nodes on survival of patients being treated by cytoreductive surgery and hyperthermic intraperitoneal chemotherapy[6]. Visible cardiophrenic lymph nodes were present in 64% of patients. There was no effect on progression-free survival or overall survival in patients with visible nodes. Unfortunately, in the patients with malignant peritoneal mesothelioma and obvious cardiophrenic angle lymph nodes, the prognostic significance of this CT finding has never been determined. Whether or not cancer is present in these nodes greater than or equal to 1.5 cm has not been determined. In our patient 5, the bilateral enlarged cardiophrenic angle lymph nodes were not removed at the time of cytoreductive surgery. He is a 9-year survivor of this disease.
Patient 6 is the only one of 100 malignant peritoneal mesothelioma patients to show pleural plaques on a preoperative CT. This association is much more common in patients with malignant pleural mesothelioma. Patients with pleural plaques compared to patients with asbestos exposure in the absence of pleural plaques have an increased hazard ratio of 8.9, 95% confidence interval = 3.0 to 26.5 to develop pleural mesothelioma. Pleural plaques are definitively related to asbestos exposure but only 20.4% of patients with asbestos exposure showed pleural plaques[11]. To our knowledge our patient 6 is the only patient with pleural plaques who went on to develop malignant peritoneal mesothelioma.
The spleen shown in our Figure 7 was present in a patient with extensive peritoneal mesothelioma who had a debulking procedure. The spleen by CT and at the time of surgical debulking was seen to be surrounded by tumor. The linear tumor density images within the spleen are suggested to be caused by mesothelioma within the notches of the spleen. These linear infoldings of the spleen surface accentuated by malignancy are remnants of the fetal lobulations of the spleen.
In patient 8, the parajejunal mass imaged by the preoperative CT is unusual but not a rare finding in patients with malignant peritoneal mesothelioma. In our survey of preoperative CTs in 100 patients, 15% showed a mass greater than 5 cm adjacent to the jejunum. A spiculated mass similar to that shown in Figure 8 can be seen with a small bowel carcinoid. A small bowel carcinoid tumor is often calcified; calcification was not seen in the 15 patients with a parajejunal mass caused by malignant peritoneal mesothelioma.
Although seen in malignant peritoneal mesothelioma patients, a mass adjacent to the jejunum is not described for peritoneal metastases patients of other diagnoses such as appendix cancer, colon cancer or ovarian cancer. In peritoneal metastases from adenocarcinoma dissemination, the largest extent of disease on bowel surfaces is observed on the terminal ileum and its mesentery. Resections of proximal small bowel as required in malignant peritoneal mesothelioma patients for complete cytoreduction is rarely, if ever, indicated. In contrast, extensive disease associated with the jejunum and the splenic flexure of the colon is common with malignant peritoneal mesothelioma. The differences in the intraperitoneal distribution of peritoneal metastases from adenocarcinoma as compared to malignant peritoneal mesothelioma have yet to be explained.
Rare diseases are often associated with bad outcomes. Delay in diagnosis and a lack of understanding of the natural history of the rare disease may contribute to unnecessary suffering.
Malignant peritoneal mesothelioma is a rare malignancy that has treatment options that provide long-term benefit. Progression within the peritoneal space in the absence of a primary site creates a challenge to its identification and radiologic description.
To identify and then describe unusual computed tomography (CT) images in patients with malignant peritoneal mesothelioma. The unusual radiologic findings are to be described along with clinical information about an individual patient.
In the pretreatment CTs of 100 patients with malignant peritoneal mesothelioma the majority of patients showed ascites, an omental cake or mesentery infiltrated by tumor. The other clearly depicted unusual CT findings and their frequency were sought to construct this manuscript.
From the 100 pretreatment CTs, eight unusual CT findings were identified, the images reproduced for the reader and the clinical features of the patient described. These unusual findings included a mass occurring within a Spigelian hernia, infiltration of the splenic parenchyma by spherical mesothelioma masses, infiltration of the lower mediastinum by tumor, a mesothelioma mass within a left inguinal canal, enlarged cardiophrenic angle lymph nodes, pleural plaques associated with the progression of malignant peritoneal mesothelioma, splenic notches caused by disease surrounding the spleen, and a mass greater than 5 cm associated with the proximal jejunum and directly adjacent to the anatomic location of the Treitz ligament.
We described eight unusual radiologic presentations of malignant peritoneal mesothelioma that are important to recognize in order to accurately diagnose this disease by CT.
The role of the radiologist in identification, description and prognosis assessment of malignancies associated with the peritoneum and peritoneal spaces is expanding. Familiarity with unusual CT findings in a rare peritoneal disease, malignant peritoneal mesothelioma, is a step toward this expanded role of the radiologist in patient management.
Manuscript source: Unsolicited manuscript
Corresponding Author's Membership in Professional Societies: Royal College of Surgeons, No. 9016460.
Specialty type: Radiology, nuclear medicine and medical imaging
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Bijelic L, Ceresoli GL, Saito H S-Editor: Gao CC L-Editor: A P-Editor: Wang LYT
| 1. | Sugarbaker PH, Turaga KK, Alexander HR Jr, Deraco M, Hesdorffer M. Management of Malignant Peritoneal Mesothelioma Using Cytoreductive Surgery and Perioperative Chemotherapy. J Oncol Pract. 2016;12:928-935. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 41] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 2. | Jelinek JS. In 100 patients with malignant peritoneal mesothelioma, concerning CT features predicted outcome of treatment. (In) Sugarbaker PH, Low RN (Eds). Pictorial Essays on Peritoneal Metastases Imaging: CT, MRI and PET-CT. Nova Science Publishers: New York, 2020: 187-212. |
| 3. | Jacquet P, Sugarbaker PH. Current methodologies for clinical assessment of patients with peritoneal carcinomatosis. J Exp Clin Cancer Res. 1996;15:49-58. |
| 4. | Skandalakis PN, Zoras O, Skandalakis JE, Mirilas P. Spigelian hernia: surgical anatomy, embryology, and technique of repair. Am Surg. 2006;72:42-48. [PubMed] |
| 5. | Sugarbaker PH, Chang D. Long-term regional chemotherapy for patients with epithelial malignant peritoneal mesothelioma results in improved survival. Eur J Surg Oncol. 2017;43:1228-1235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 61] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 6. | Elias D, Borget I, Farron M, Dromain C, Ducreux M, Goéré D, Honoré C, Boige V, Dumont F, Malka D, Pottier E, Caramella C. Prognostic significance of visible cardiophrenic angle lymph nodes in the presence of peritoneal metastases from colorectal cancers. Eur J Surg Oncol. 2013;39:1214-1218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 7. | Jeune F, Brouquet A, Caramella C, Gayet M, Abdalla S, Verin AL, Thirot Bidault A, Penna C, Benoist S. Cardiophrenic angle lymph node is an indicator of metastatic spread but not specifically peritoneal carcinomatosis in colorectal cancer patients: Results of a prospective validation study in 91 patients. Eur J Surg Oncol. 2016;42:861-868. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Reardon PR. Laparoscopic Preperitoneal Repair of Spigelian Hernia Utilizing Mesh. (In) Asbun HJ, Schwaitzberg SD (Eds). ACS Multimedia Atlas of Surgery: Hernia Surgery Volume. Cine-Med: Woodbury, CT, 2012: 211-224. |
| 9. | Sugarbaker PH, Welch LS, Mohamed F, Glehen O. A review of peritoneal mesothelioma at the Washington Cancer Institute. Surg Oncol Clin N Am. 2003;12:605-621, xi. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 194] [Cited by in RCA: 171] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 10. | Eryilmaz S, Sirlak M, Inan MB, Erden E, Eren NT, Corapçioğlu T, Akalin H. Primary pericardial mesothelioma. Cardiovasc Pathol. 2001;10:147-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Pairon JC, Laurent F, Rinaldo M, Clin B, Andujar P, Ameille J, Brochard P, Chammings S, Ferretti G, Galateau-Sallé F, Gislard A, Letourneux M, Luc A, Schorlé E, Paris C. Pleural plaques and the risk of pleural mesothelioma. J Natl Cancer Inst. 2013;105:293-301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 62] [Article Influence: 5.2] [Reference Citation Analysis (0)] |