Published online Aug 28, 2019. doi: 10.4329/wjr.v11.i8.110
Peer-review started: July 26, 2019
First decision: August 2, 2019
Revised: August 14, 2019
Accepted: August 18, 2019
Article in press: August 19, 2019
Published online: August 28, 2019
Processing time: 45 Days and 12.1 Hours
Duodenal variceal bleeding is a rare cause of gastrointestinal bleeding. The most common site is the duodenal bulb. It is usually detected endoscopically but it can be very challenging to diagnose if it is located distal to the second part of duodenum. The pre- transjugular intrahepatic portosystemic shunt (TIPS) presence of SPSS was found to be associated with an increased risk of early morbidity and mortality after TIPS placement.
A 43-year-old cirrhotic male presented with melena for three days. Upper endoscopy was performed and showed active blood oozing from the distal duodenum concerning for ectopic duodenal varix. A computed tomography (CT) angiogram was performed and showed an enlarged cluster of venous collaterals around the distal duodenum. He underwent TIPS placement. He had another episode of melena three days later. Push enteroscopy with injection sclerotherapy into the duodenal varices was performed with no success. A repeat CT angiogram showed occluded TIPS shunt. Therefore, a TIPS revision was performed and there was an extensive portal venous thrombosis with a large shunt between the inferior mesenteric vein and left renal vein via the left gonadal vein. Thrombectomy and TIPS shunt balloon angioplasty was performed, followed by embolization of the portosystemic. The melena was resolved, and patient was discharged with arranged hepatology follow up.
It important to look and embolize the SPSS shunts in patients with early TIPS dysfunction and recurrent duodenal variceal bleeding.
Core tip: Portal hypertension leads to the formation of varices, which can be present at the gastroesophageal region or ectopic locations. Bleeding ectopic varices are challenging to manage, and in many cases, transjugular intrahepatic portosystemic shunt (TIPS) is a safe and effective therapy. The pre-TIPS presence of SPSS was found to be associated with an increased risk of early morbidity and mortality after TIPS placement. We have successfully treated a patient with duodenal variceal bleeding with TIPS and embolization of SPSS after he failed TIPS monotherapy.
- Citation: Anand R, Ali SE, Raissi D, Frandah WM. Duodenal variceal bleeding with large SPSS treated with transjugular intrahepatic portosystemic shunt and embolization: A case report. World J Radiol 2019; 11(8): 110-115
- URL: https://www.wjgnet.com/1949-8470/full/v11/i8/110.htm
- DOI: https://dx.doi.org/10.4329/wjr.v11.i8.110
Duodenal variceal bleeding is a rare cause of gastrointestinal bleeding. It can be life-threatening with a mortality rate of up to 40%[1]. Portal hypertension due to liver cirrhosis is the most common cause of portosystemic shunts and duodenal varices[2]. The most common site is at the duodenal bulb, and it is usually detected endoscopically[3]. However, it can be difficult to diagnose if it is located distal to the second part of duodenum. The pre-transjugular intrahepatic portosystemic shunt (TIPS) presence of SPSS was found to be associated with an increased risk of early morbidity and mortality after TIPS placement [4]. We have successfully treated a patient with duodenal variceal bleeding with TIPS and embolization of SPSS after he failed TIPS monotherapy.
A 43-year-old male presented to the emergency department complaining of melena for three days.
He had two loose bowel movements with black tarry stool every day for the last three days with lightheadedness.
He denies any hematemesis, abdominal pain, or similar episodes in the past.
Past medical history was remarkable for liver cirrhosis due to untreated hepatitis C and alcohol abuse. Family history was unremarkable.
On presentation, vitals revealed a blood pressure of 100/60 mmHg; pulse rate of 110 per minute, temperature of 98.5 Fahrenheit, and respiratory rate of 18 per minute. Physical exam revealed an ill-looking patient with mild confusion, pale conjunctiva, non-icterus sclera, mildly distended abdomen with no tenderness, and trace pitting edema in both legs.
Laboratory findings displayed hemoglobin of 6.8 g/dL, leukocytes 10000/mm3, and platelet 105000/mm3. Serum biochemistry revealed creatinine 0.6 mg/dL, blood urea nitrogen 16 mg/dL, albumin 2.4 g/dL, total protein 4.8 g/dL, aspartate aminotransferase 34 IU/L, alanine aminotransferase 60 IU/L, alkaline phosphatase 95 IU/L, international normalized ratio 1.1 and total bilirubin 1.5 mg/dL.
Duodenal variceal bleeding with large SPSS.
Emergency esophagogastroduodenoscopy (EGD) was performed on the day of admission and showed grade B esophagitis and small esophageal varices with no active bleeding.
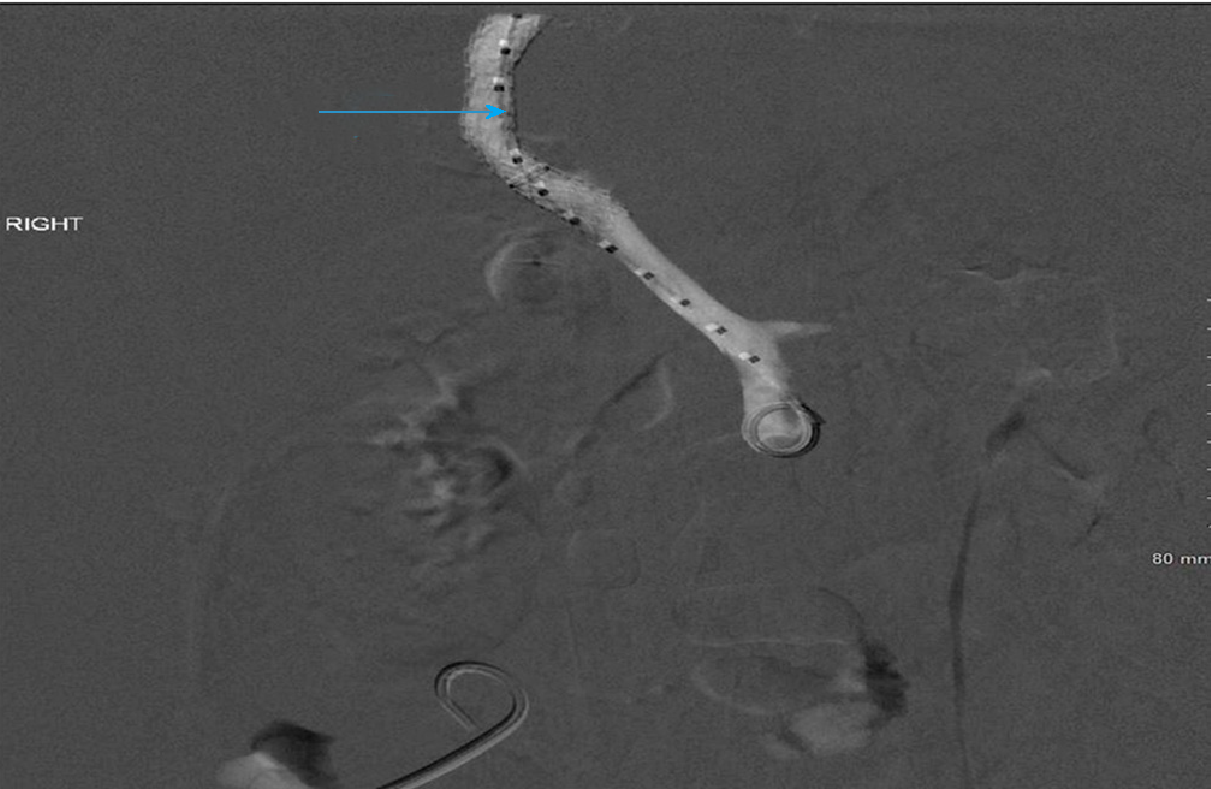
He continued to have melena, and drop in hemoglobin concertation over the next 48 h. So, repeat EGD was performed and showed oozing of fresh blood in the distal duodenum, concerning for a bleeding ectopic duodenal varix. A computed tomography (CT) angiogram was performed and showed an enlarged cluster of venous collaterals around the distal duodenum. He underwent TIPS via using VIATORR® 10 mm × 6 cm stent-graft, which decreased the portosystemic gradient from 21 mmHg to 5 mmHg with complete decompression of the intestinal varices (Figure 1).
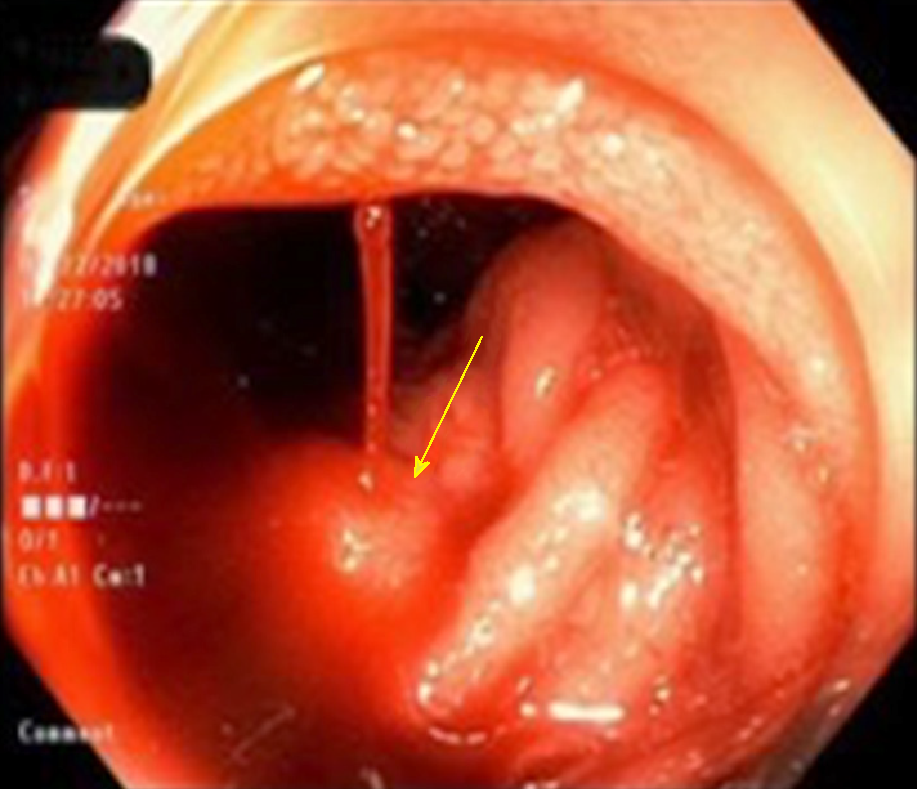
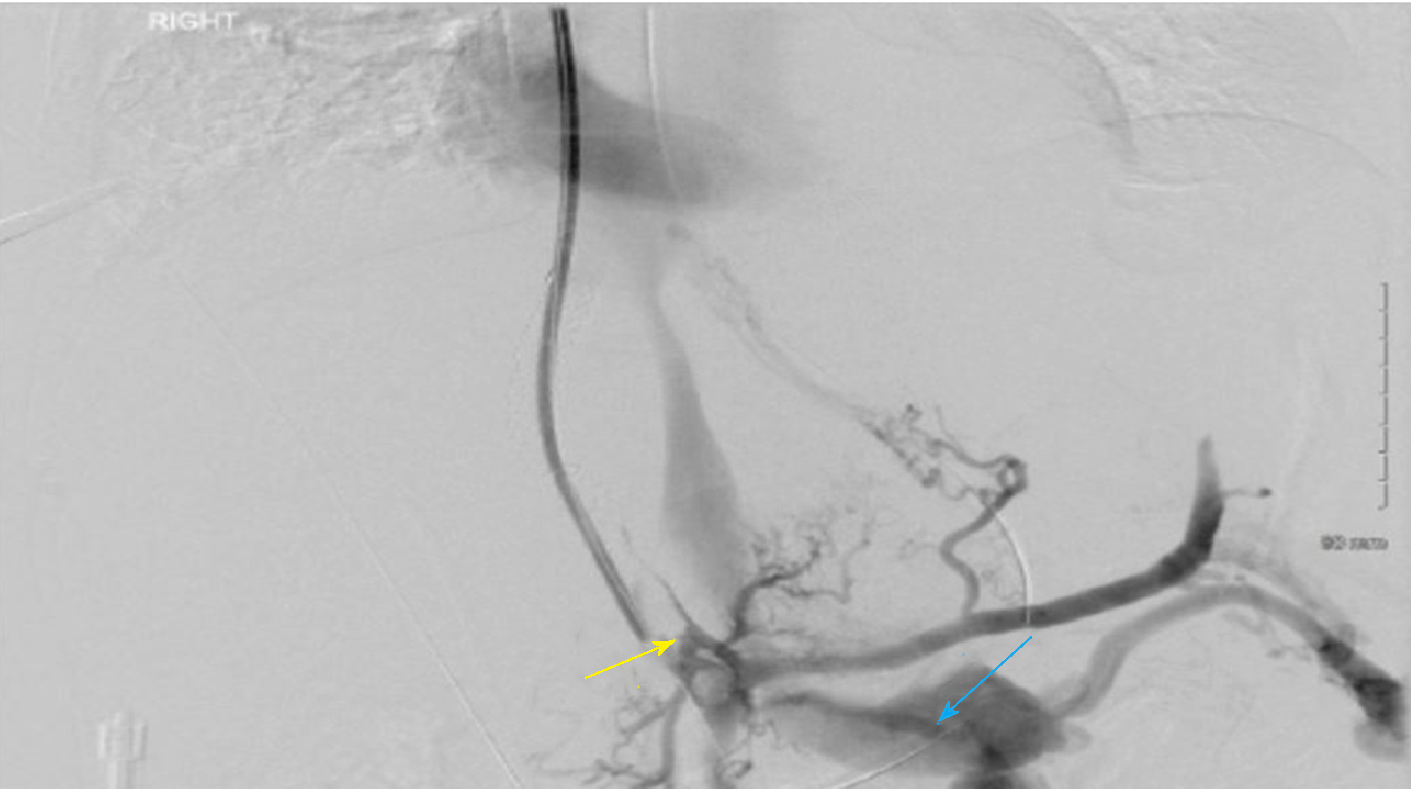
Seventy-two hours later, the patient had a recurrence of melena with worsening anemia. A push enteroscopy was performed and showed fresh blood oozing from ectopic varix in the fourth portion of the duodenum (Figure 2). One ml of glue (n-Butyl Cyanoacrylate) was injected into varix. Despite all of that, he continued to have gastrointestinal bleeding that requires a blood transfusion. A repeat CT angiogram showed a nearly occluded TIPS shunt. Therefore, a TIPS revision was preceded, and TIPS was occluded with extensive portal venous thrombosis (Figure 3).
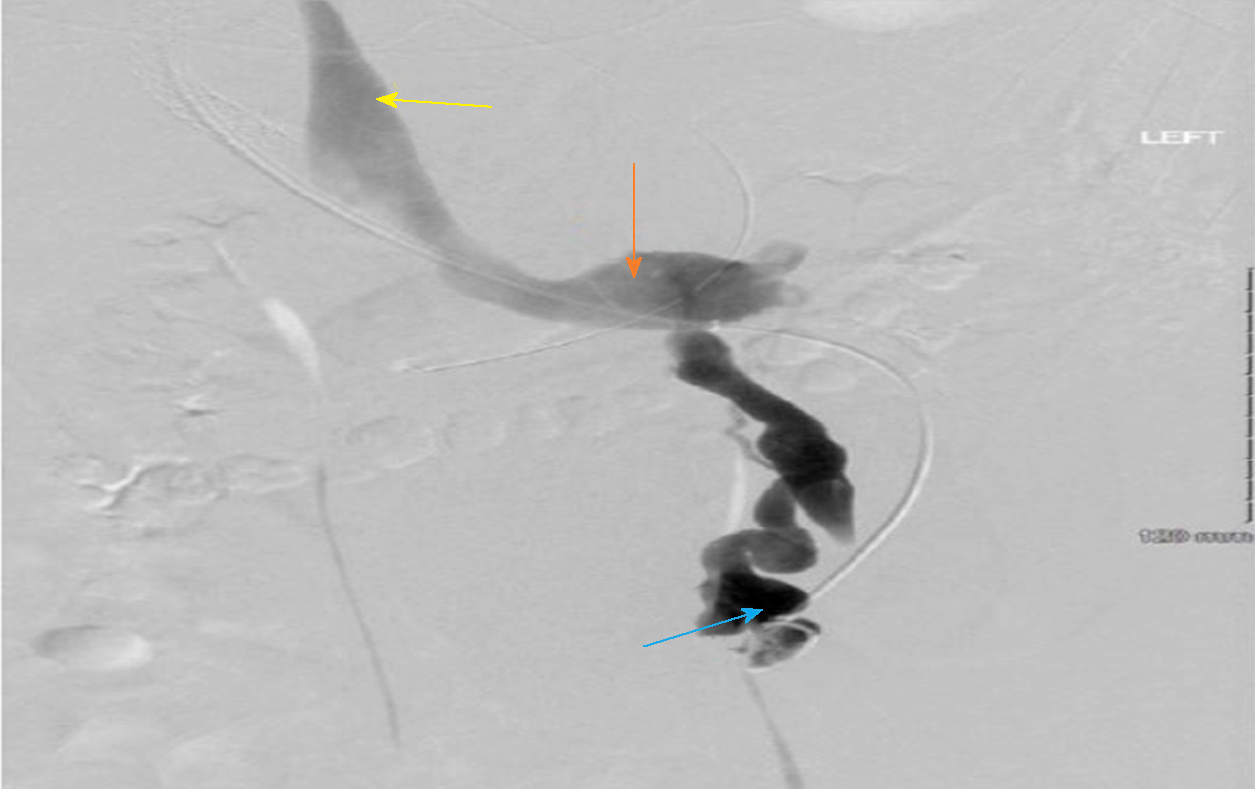
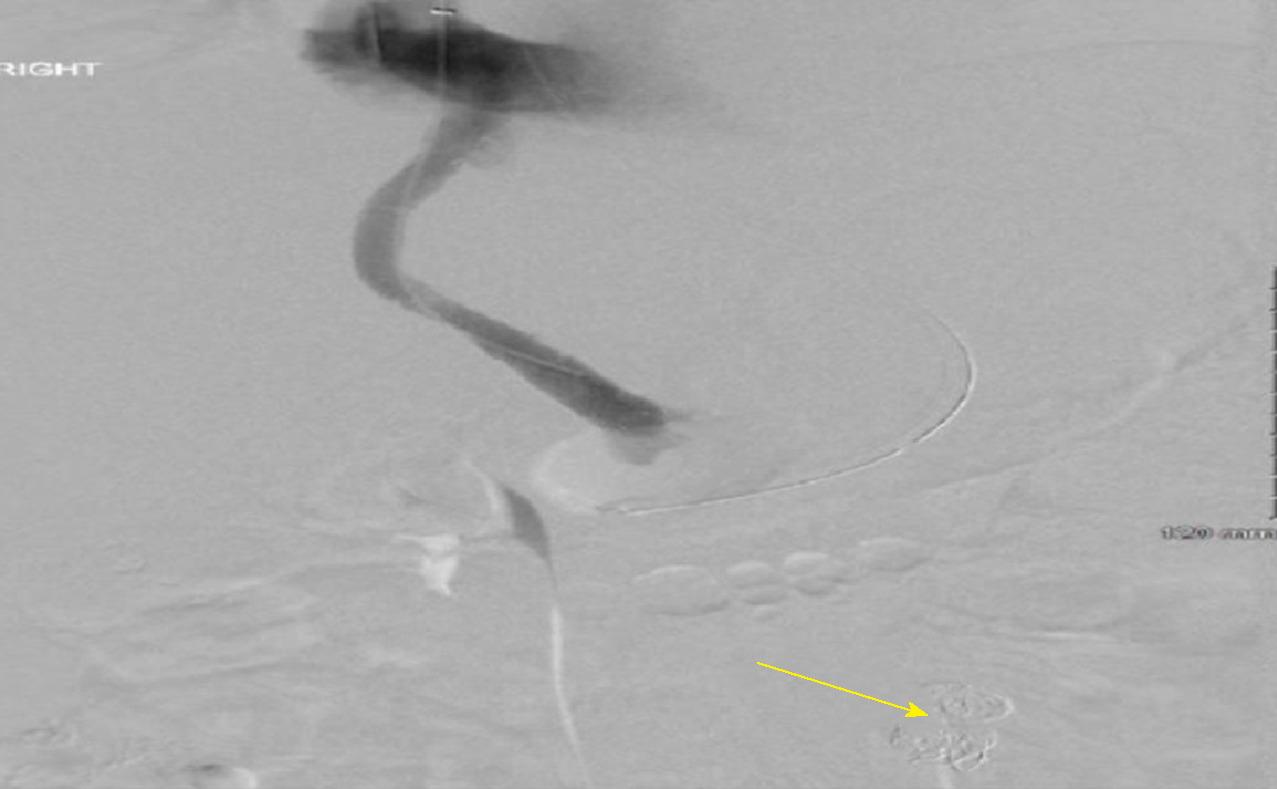
Interestingly, there was a large, competing, non-physiological shunt between the inferior mesenteric vein and left renal vein via the left gonadal vein (Figure 4). Maceration thrombectomy and TIPS shunt balloon angioplasty was performed, followed by embolization of the portosystemic (Figure 5). The patient remained stable for the rest of the hospital course with no signs of recurrent bleeding. He was discharged with arranged hepatology follow up.
Patients with portal hypertension develop SPSS with hepatofugal flow that serve as non-physiologic communications between branches of the systemic and portal venous systems which allow excess flow to bypass the liver. One of these SPSS is the splenorenal shunt (SRS), which is associated with boosted occurrence of hepatocellular carcinoma in an obese patient[5]. SPSS when dilating form varices, which can be present at numerous regions of the body. Since duodenal varices were initially defined by Alberti[6] in 1931 and envisioned via the scope by Kunisaki et al[7] in 1973, there have been hundreds of cases published. In a study reviewing 169 cases of bleeding ectopic varices, 17% were in the duodenum[1]. Bleeding ectopic varices account for up to 5% of all variceal bleeding noted in cirrhotic patients. They can be very challenging to diagnose and manage, and as a result, in some cases, can have mortality rates as high as 40%[1,8,9]. Currently, there are no set guidelines for the treatment of ectopic variceal bleeding. Management varies based on the location and size of these ectopic varices. Endoscopic band ligation (EBL) and endoscopic injection sclerotherapy (EIS) has been tried in multiple studies for bleeding ectopic varices with some degree of success[10-15]. However, as in our case, EBL or EIS can fail to control the bleeding, and TIPS can be used as second-line therapy[16,17]. A combined therapeutic technique such as a balloon-occluded retrograde transvenous obliteration (BRTO) with embolization or sclerotherapy has been investigated by Copelan et al[18] and showed a bleeding control rate of 90% and it suggested to be a safe treatment option when TIPS is contraindicated.
TIPS reduce the hepatic venous pressure gradient (HVPG), which results in portal venous decompression and variceal bleeding control. Studies have shown that bleeding risk from varices decreases significantly once the HVPG falls below 12 mmHg[19,20]. TIPS dysfunction is a complication with TIPS placement. It is defined as a loss of portal vein system decompression, due to thrombosis or stenosis (> 50%) of the TIPS. The pre-TIPS presence of SPSS was found to be associated with an increased risk of early morbidity and mortality after TIPS placement[4].
Our patient had an infrequent and unusual cause for TIPS thrombosis. He was noted to have a large non-physiological SPSS between the inferior mesenteric vein and left renal vein via the left gonadal vein. The shunt promoted hepatofugal flow that was competing with the TIPS. As a result, it decreased the flow across the shunt and led to early thrombosis and TIPS dysfunction, which led to recurrent variceal bleeding. Once the shunt was embolized, TIPS revision was successful, and the patient’s variceal bleeding resolved.
This case illustrates the importance to look for these competing shunts in patients with early TIPS dysfunction and recurrent bleeding when other causes have been ruled out. Also, as noted in our case, portosystemic pressure gradient measurements are unreliable in patients with large competing SPSS. Embolization of these shunts is crucial to control the duodenal variceal bleeding and prevent early thrombosis of TIPS.
Manuscript source: Unsolicited manuscript
Specialty type: Radiology, nuclear medicine and medical imaging
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Garbuzenko DV, Tarantino G S-Editor: Ma RY L-Editor: A E-Editor: Zhou BX
| 1. | Norton ID, Andrews JC, Kamath PS. Management of ectopic varices. Hepatology. 1998;28:1154-1158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 239] [Cited by in RCA: 254] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 2. | Kotfila R, Trudeau W. Extraesophageal varices. Dig Dis. 1998;16:232-241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 22] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Christidou A, Tzathas C, Khuffash O, Triantaphyllou G. Upper gastrointestinal bleeding due to ectopic varices in a patient with alcoholic cirrhosis. Ann Gastroentol. 2003;16:179-182. |
| 4. | Borentain P, Soussan J, Resseguier N, Botta-Fridlund D, Dufour JC, Gérolami R, Vidal V. The presence of SPSS increases the risk of complications after transjugular intrahepatic portosystemic shunt (TIPS) placement. Diagn Interv Imaging. 2016;97:643-650. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 30] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 5. | Tarantino G, Citro V, Conca P, Riccio A, Tarantino M, Capone D, Cirillo M, Lobello R, Iaccarino V. What are the implications of the spontaneous spleno-renal shunts in liver cirrhosis? BMC Gastroenterol. 2009;9:89. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 75] [Cited by in RCA: 75] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 6. | Alberti W. Uberden roentgenologischen nachweis von varizen in buolbus duodeni. Fortschro Geb Koentgenstr. 1931;43:60-65. |
| 7. | Kunisaki T, Someya N, Shimokava Y. Varices in the distal duodenum seen with a fiberduodenoscope. Endoscopy. 1973;5:101-104. [RCA] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Graham DY, Smith JL. The course of patients after variceal hemorrhage. Gastroenterology. 1981;80:800-809. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 708] [Cited by in RCA: 601] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 9. | Sarin SK, Kumar CKN. Ectopic varices. Clin Liver Dis (Hoboken). 2012;1:167-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 35] [Article Influence: 2.7] [Reference Citation Analysis (35)] |
| 10. | Akhter NM, Haskal ZJ. Diagnosis and management of ectopic varices. Gastrointest Intervention. 2012;1:3-10. [RCA] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 17] [Article Influence: 1.3] [Reference Citation Analysis (1)] |
| 11. | Akazawa Y, Murata I, Yamao T, Yamakawa M, Kawano Y, Nomura N, Isomoto H, Mizuta Y, Murase K, Kohno S. Successful management of bleeding duodenal varices by endoscopic variceal ligation and balloon-occluded retrograde transvenous obliteration. Gastrointest Endosc. 2003;58:794-797. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 36] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 12. | Yoshida Y, Imai Y, Nishikawa M, Nakatukasa M, Kurokawa M, Shibata K, Shimomukai H, Shimano T, Tokunaga K, Yonezawa T. Successful endoscopic injection sclerotherapy with N-butyl-2-cyanoacrylate following the recurrence of bleeding soon after endoscopic ligation for ruptured duodenal varices. Am J Gastroenterol. 1997;92:1227-1229. [PubMed] |
| 13. | Hekmat H, Al-toma A, Mallant MP, Mulder CJ, Jacobs MA. Endoscopic N-butyl-2-cyanoacrylate (Histoacryl) obliteration of jejunal varices by using the double balloon enteroscope. Gastrointest Endosc. 2007;65:350-352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 23] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 14. | Chen WC, Hou MC, Lin HC, Chang FY, Lee SD. An endoscopic injection with N-butyl-2-cyanoacrylate used for colonic variceal bleeding: a case report and review of the literature. Am J Gastroenterol. 2000;95:540-542. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 15. | Ota K, Shirai Z, Masuzaki T, Tanaka K, Higashihara H, Okazaki M, Arakawa M. Endoscopic injection sclerotherapy with n-butyl-2-cyanoacrylate for ruptured duodenal varices. J Gastroenterol. 1998;33:550-555. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 35] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 16. | Selçuk H, Boyvat F, Eren S, Korkmaz M, Gür G, Yilmaz U, Boyacioğlu S. Duodenal varices as an unusual cause of gastrointestinal bleeding due to portal hypertension: a case report. Turk J Gastroenterol. 2004;15:104-107. [PubMed] |
| 17. | Jonnalagadda SS, Quiason S, Smith OJ. Successful therapy of bleeding duodenal varices by TIPS after failure of sclerotherapy. Am J Gastroenterol. 1998;93:272-274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 54] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 18. | Copelan A, Chehab M, Dixit P, Cappell MS. Safety and efficacy of angiographic occlusion of duodenal varices as an alternative to TIPS: review of 32 cases. Ann Hepatol. 2015;14:369-379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 19. | Vangeli M, Patch D, Terreni N, Tibballs J, Watkinson A, Davies N, Burroughs AK. Bleeding ectopic varices--treatment with transjugular intrahepatic porto-systemic shunt (TIPS) and embolisation. J Hepatol. 2004;41:560-566. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 150] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 20. | Boyer TD, Haskal ZJ; American Association for the Study of Liver Diseases. The role of transjugular intrahepatic portosystemic shunt in the management of portal hypertension. Hepatology. 2005;41:386-400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 315] [Cited by in RCA: 297] [Article Influence: 14.9] [Reference Citation Analysis (0)] |