Copyright
©The Author(s) 2016.
World J Radiol. Jul 28, 2016; 8(7): 716-725
Published online Jul 28, 2016. doi: 10.4329/wjr.v8.i7.716
Published online Jul 28, 2016. doi: 10.4329/wjr.v8.i7.716
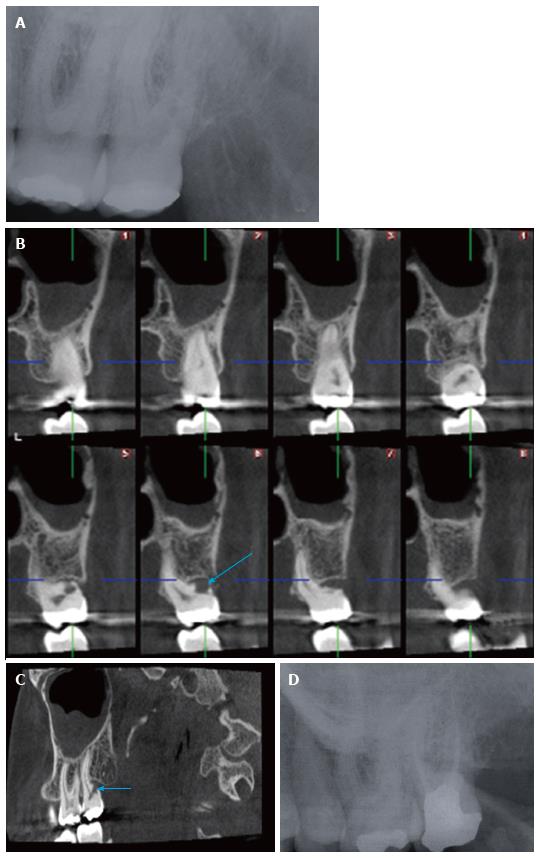
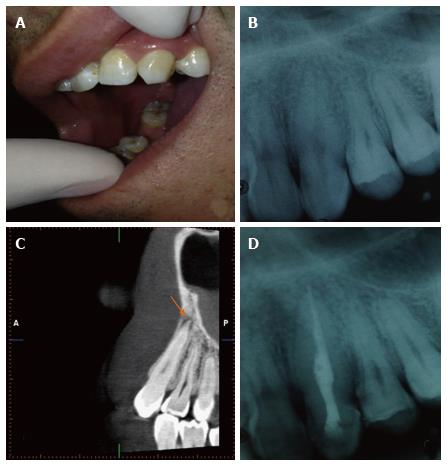
Figure 1 Radiological assessment of maxillary left second molar.
A: Periapical radiography of the left maxillary second molar tooth taken with an X-ray generator, Evolution X3000 2C/1 New Life (New Life Radiology, Grugliasco, TO, Italy) operated at 70 kVp, 8 mA and 0.3 s. using Kodak Insight F Speed Film (Kodak, Rochester, NY, United States) shows no apparent pathology; Cross sectional (B) and sagittal CBCT (C) images of the same tooth obtained by Planmeca ProMax 3D Max CBCT unit (Planmeca Oy, Helsinki, Finland) with a flat panel sensor, operating at 96 kVp, 8.0 mA, using High Definition, 0.15 mm3 voxel size, and a 55 mm × 50 mm FOV. The exposure time was 15.405 s and the DAP (mGy*cm2) value was 513 mGy*cm2. Arrows show external resorption of the buccodistal root apparently; D: Follow up periapical radiography taken 1 year after root canal treatment showed no sign of pathology. CBCT: Cone beam computed tomography; FOV: Field of view; DAP: Dose area product.
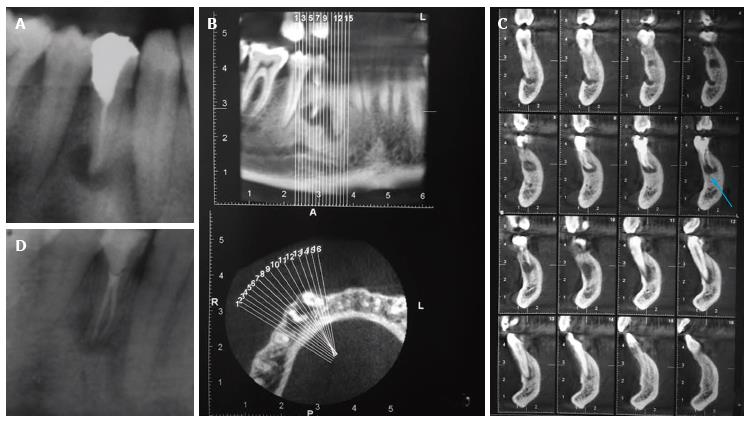
Figure 2 Radiological assessment of mandibular 1st premolar tooth.
A: Periapical radiography of the right mandibular 1st premolar tooth showed a radiolucency at the periapical region. The root canal treatment seemed to be properly conducted; Panoramic (upper) and axial (lower) CBCT images (B) and (C) cros-sectional CBCT images of the same tooth obtained by Planmeca ProMax 3D Max CBCT unit (Planmeca Oy, Helsinki, Finland) with a flat panel sensor, operating at 96 kVp, 8.0 mA, using High Definition, 0.15 mm3 voxel size, and a 55 mm × 50 mm FOV shows an unfilled root canal related to periapical radiolucency; D: Periapical radiography of the same tooth taken after treatment. CBCT: Cone beam computed tomography; FOV: Field of view.
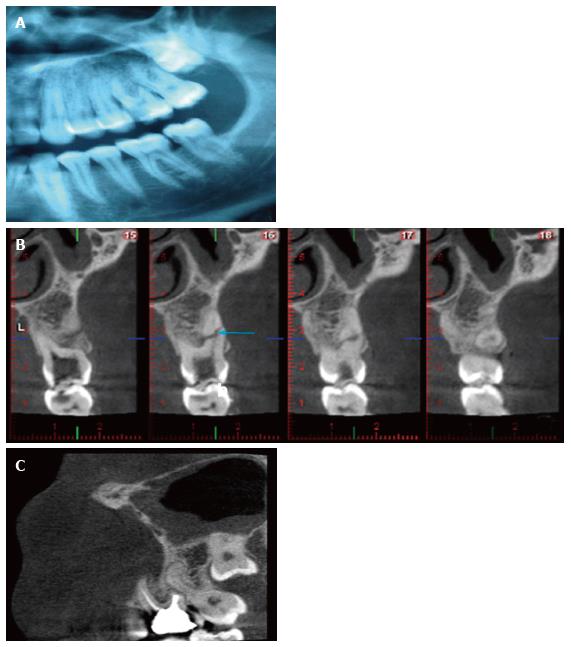
Figure 3 Radiological assessment of left 1st maxillary molar tooth.
A: Cropped panoramic radiography showed a caries lesion in the left 1st maxillary molar tooth; B: Cross-sectional CBCT images revealed an oblique radiolucent root fracture line in the middle third of the buccodistal root of maxillary 1st molar tooth; C: Sagittal CBCT images showed no resorption or fracture at 1 year follow up. The same periapical and CBCT units and settings with Case 1 and Case 2 were used. CBCT: Cone beam computed tomography.
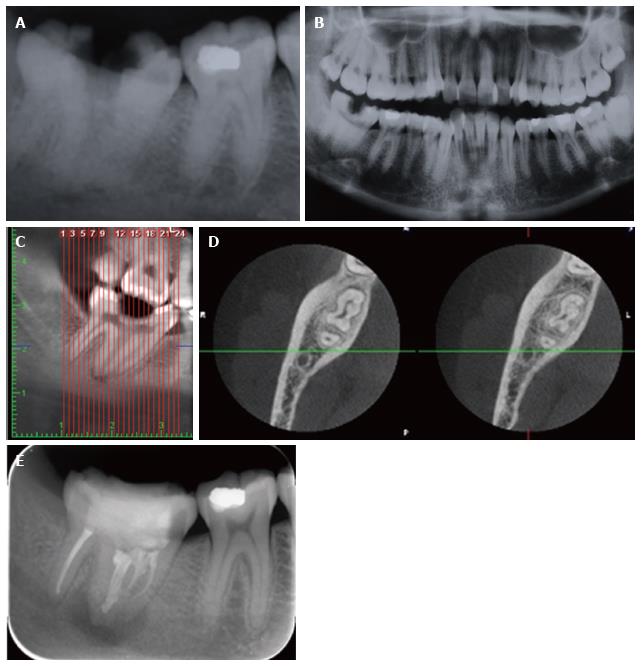
Figure 4 Radiological assessment of right mandibular 2nd molar tooth.
A: On periapical radiography, presence of caries and a periapical lesion was detected in a fused right mandibular 2nd molar tooth; B: The contrary left mandibular second molar was normal in shape on panoramic radiography; Panoramic CBCT (C) and axial CBCT (D) images showed that mandibular 2nd and 3rd molars were fused; E: The tooth was re-evaluated six months later with periapical radiography. The same periapical and CBCT units and settings with Case 1, 2, and 3 were used. CBCT: Cone beam computed tomography.
Figure 5 Clinical and radiological assessment of maxillary canine tooth.
A: Clinical appearance of the canine tooth; B: Periapical radiographic findings showed no periapical pathology or carious lesion; C: Sagittal CBCT images showed a periapical radiolucency; D: Periapcial radiography of the treated tooth. The same periapical and CBCT units and settings with Case 1, 2, 3 and 4 were used. CBCT: Cone beam computed tomography.
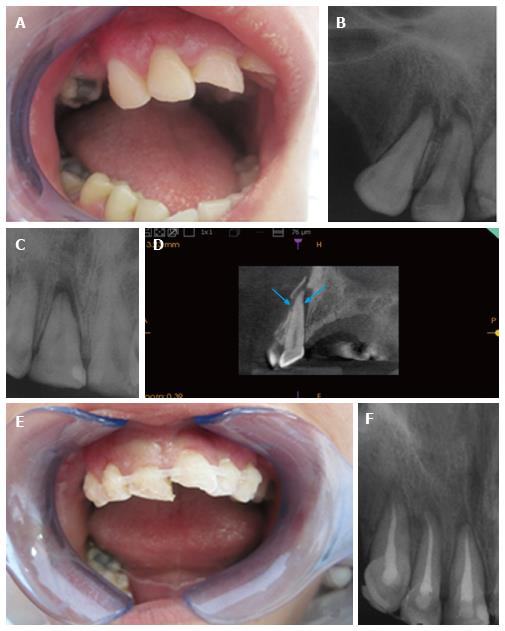
Figure 6 Clinical and radiological assessment of maxillary anterior teeth.
A: Clinical intraoral appearance of the patient; B and C: Intraoral radiographs taken from two different angels showed periapical radiolucencies in canine and incisors but they were unable to show a suspected horizontal root fracture (HRF); D: With CBCT Kodak 9000 3D (Eastman Kodak Co, Rochester, NY, United States) CMOS sensor with optical fiber, offering a single 5 cm × 3.8 cm FOV at 0.076 mm a HRF of central incisor along with alveolar bone fracture was detected in cross-sectional views; E: Intraoral appearance of the patient after splinting of canine and incisors; F:Periapical radiography showing treatment of canine and incisors with guta percha and AH Plus. CBCT: Cone beam computed tomography.
- Citation: Yılmaz F, Kamburoglu K, Yeta NY, Öztan MD. Cone beam computed tomography aided diagnosis and treatment of endodontic cases: Critical analysis. World J Radiol 2016; 8(7): 716-725
- URL: https://www.wjgnet.com/1949-8470/full/v8/i7/716.htm
- DOI: https://dx.doi.org/10.4329/wjr.v8.i7.716