Copyright
©The Author(s) 2016.
World J Radiol. Jun 28, 2016; 8(6): 635-655
Published online Jun 28, 2016. doi: 10.4329/wjr.v8.i6.635
Published online Jun 28, 2016. doi: 10.4329/wjr.v8.i6.635
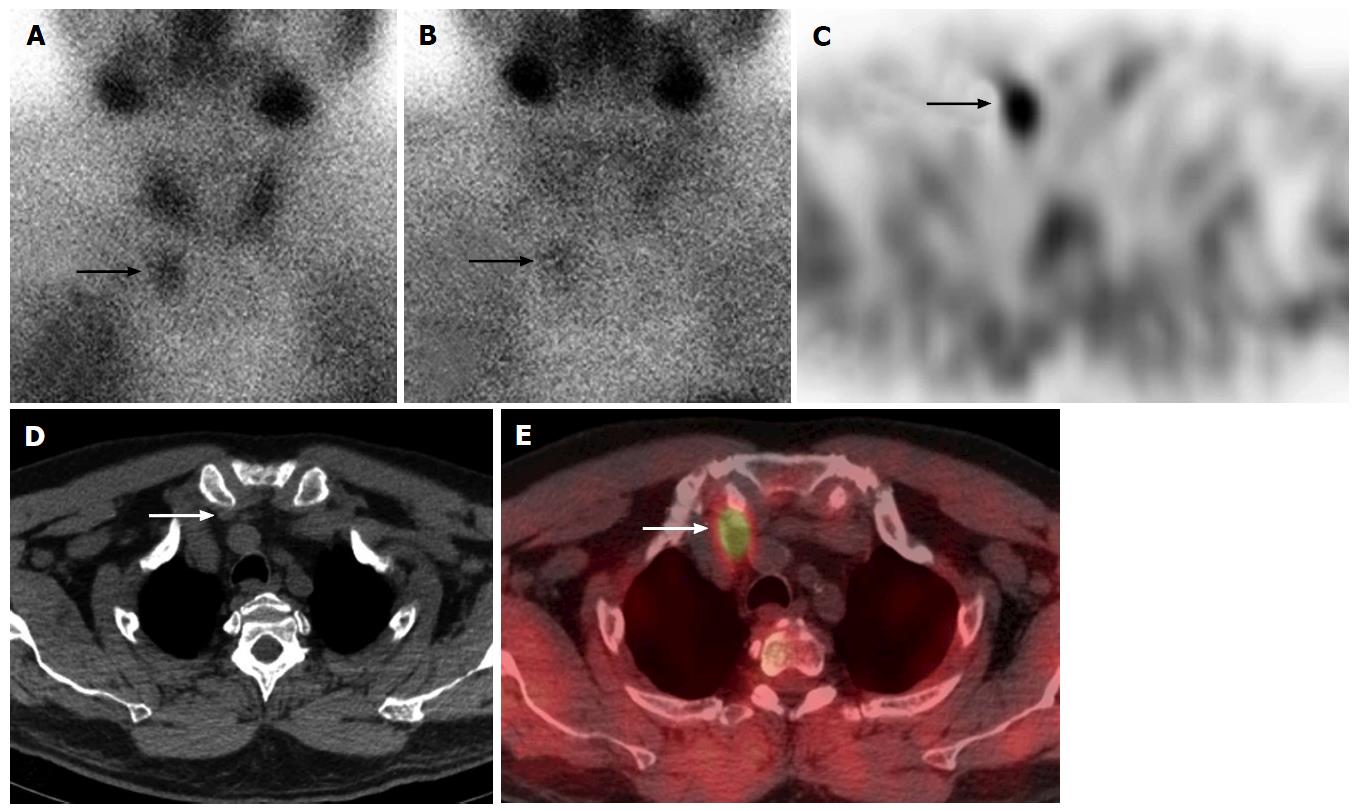
Figure 1 Right inferior parathyroid adenoma in a 60-year-old man.
99mTc-sestamibi parathyroid scan anterior early 20 min (A) and delayed 2 h planar images (B) show focal radiotracer uptake and retention at the juncton of the right lower neck/superior mediastinum (arrows). Axial SPECT, CT and SPECT/CT (C-E) imaging localizes this activity to a soft tissue abnormality in the right lower neck posterior to the sternoclavicular joint (arrows), consistent with ectopic inferior parathyroid adenoma in the lower neck. This was surgically removed via a lower neck incision approach. SPECT: Single photon emission computed tomography; CT: Computed tomography.
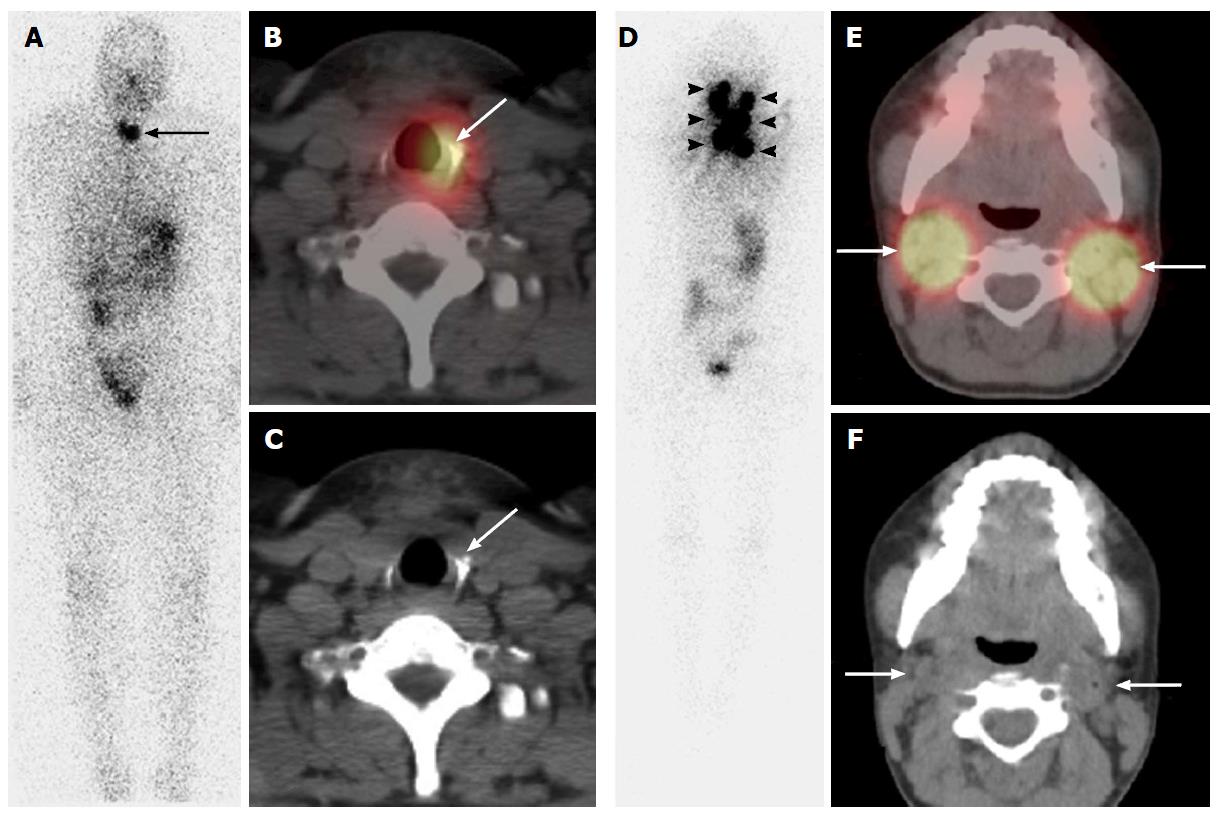
Figure 2 Pre-ablation 131I single photon emission computed tomography/computed tomography scan in a 29-year-old woman with papillary thyroid cancer, the largest lesion measuring 4.
2 cm in the right lobe. Post-surgical thyroglobulin was 0.9 ng/mL with a thyrotropin (TSH) of 57 mIU/L. Planar scan (A) depicts two foci of neck activity (long arrow). SPECT/CT (B, C) localized uptake to soft tissue in the left thyroid bed compatible with remnant thyroid tissue (long arrows) and the patient was given a low dose 131I treatment for remnant ablation. Pre-ablation 131I SPECT/CT scan in a 18-year-old woman with multifocal papillary thyroid cancer, the largest lesion measuring 2.0 cm in the left lobe, with capsular invasion;metastatic lymph nodes were resected from the central compartment. Post-surgical thyroglobulin was 223 ng/mL with a TSH of 68 mIU/L. Planar scan (D) depicts multiple foci of neck activity (arrowheads). SPECT/CT (E,F) localized uptake to bilateral bulky iodine-avid lymph nodes in the neck (long arrows), and also the left supraclavicular fossae (not shown). After imaging the patient classified as high risk for recurrence, recommendation was for medium dose 131I therapy. SPECT: Single photon emission computed tomography; CT: Computed tomography.
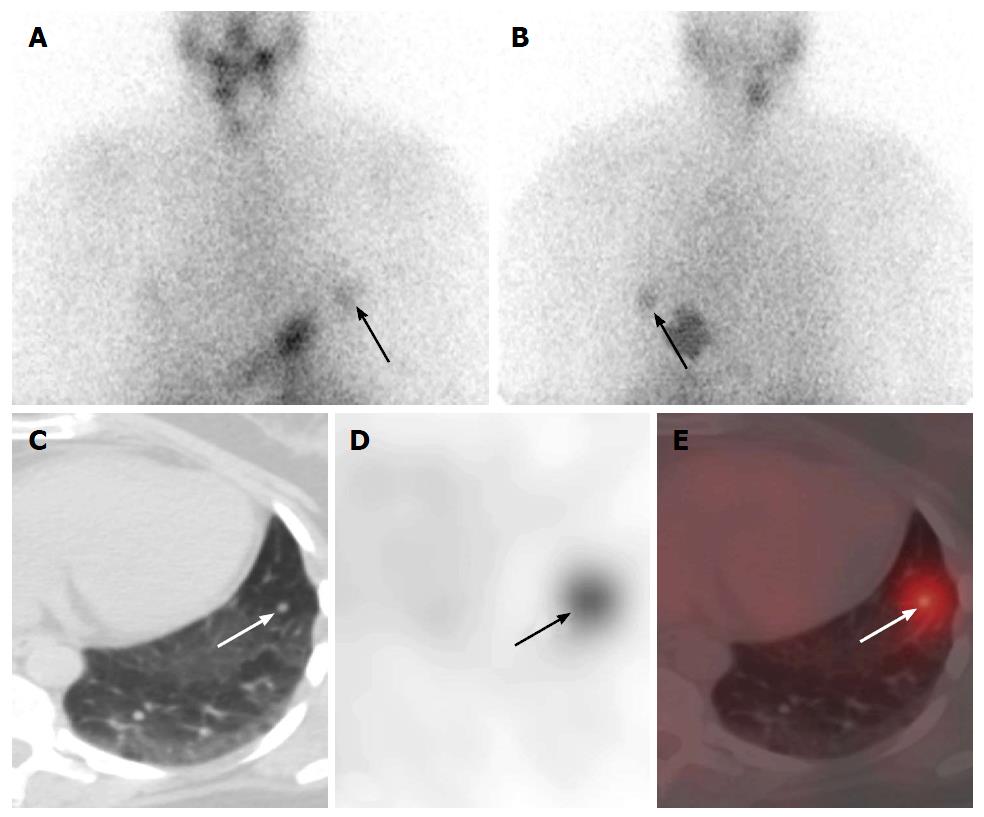
Figure 3 Pre-ablation hypothyroid 131I-radioiodine whole body planar and single photon emission computed tomography-computed tomography scan in a 45-year-old female with papillary thyroid cancer after total thyroidectomy.
Anterior (A) and posterior (B) planar images demonstrate a focus of activity in the left thorax (arrow), which is better visualized on the posterior image. Unenhanced axial CT (C), SPECT (D), and SPECT-CT (E) show a 7 mm a radioiodine avid nodule in the lingula (arrow). The utilization of SPECT-CT increases diagnostic certainty in comparison to planar-only imaging evaluation, obviates the need for concurrent diagnostic CT and allows therapeutic evaluation of this nodule after radioactive iodine thyroid treatment. SPECT: Single photon emission computed tomography; CT: Computed tomography.
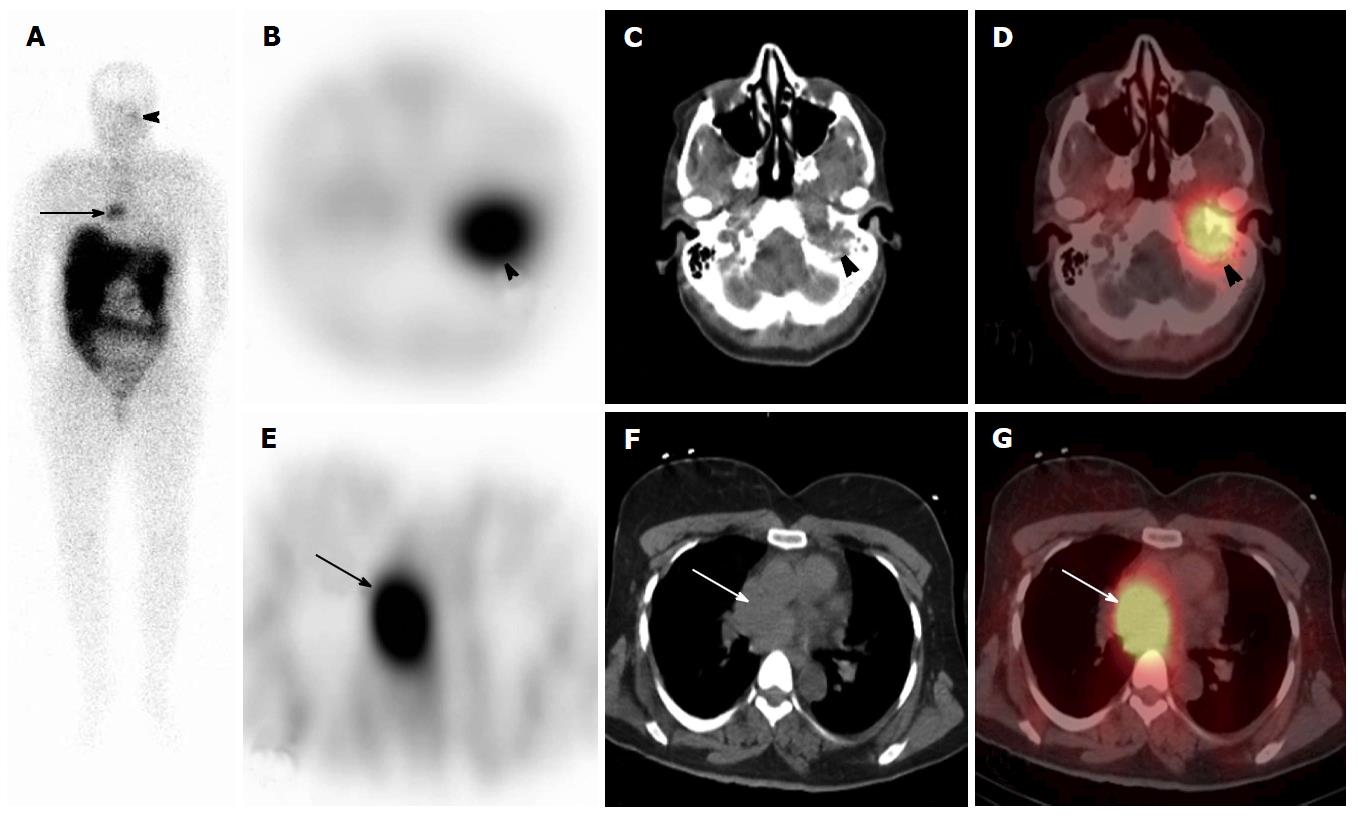
Figure 4 111In-DTPA-pentetreotide scan in a 45-year-old woman with paraganglioma and glomus tumor, to evaluate for octreotide-avidity.
On anterior (A) whole body planar images, there are 2 foci of uptake overlying the left skull base (arrowhead) and the mediastinum (arrows). On Axial SPECT, CT and SPECT/CT (B-D) the skull base radiotracer uptake localizes to a known glomus jugulare tumor adjacent to the left temporal bone and on thoracic axial SPECT, CT and SPECT/CT (E-G) the thoracic radioactivity is within a soft tissue mass in the middle mediastinum, located posterior to the ascending aorta. There is no abnormal radiotracer accumulation below the diaphragm. SPECT: Single photon emission computed tomography; CT: Computed tomography.
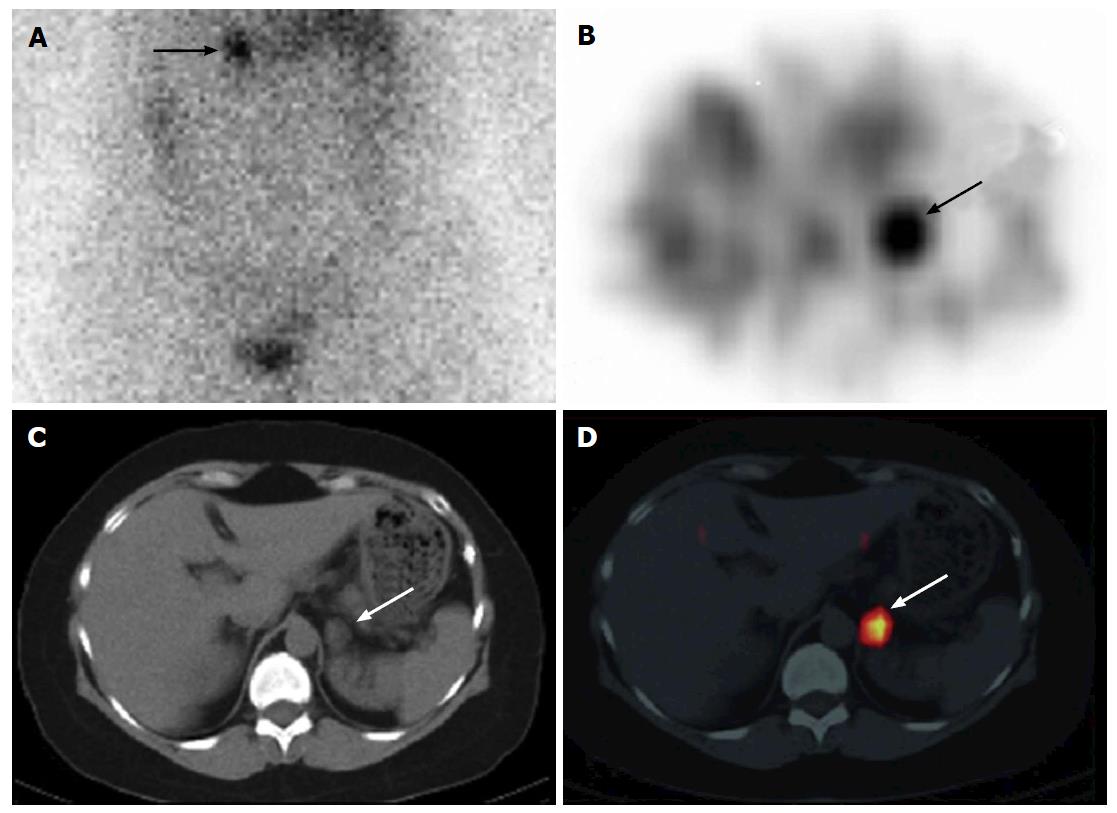
Figure 5 A 55-year-old woman with Cushing syndrome underwent 131I-NP-59 single photon emission computed tomography/computed tomography scan for localization of Cushing’s adenoma.
Planar posterior (A) abdominal image on day 5 post injection of 131I-NP-59 SPECT/CT demonstrates focal uptake in the left adrenal region (arrow). Transverse SPECT (B), CT images (C) and fused SPECT/CT (D) localize activity to a 1.5 cm × 1.8 cm nodule arising from the left adrenal gland (arrows). Findings are compatible with a hyperfunctional left adrenal adenoma. Imaging courtesy of “Adrenal Cortical Imaging with I-131 NP-59 SPECT-CT”. (By Wong et al[181], with permission). SPECT: Single photon emission computed tomography; CT: Computed tomography.
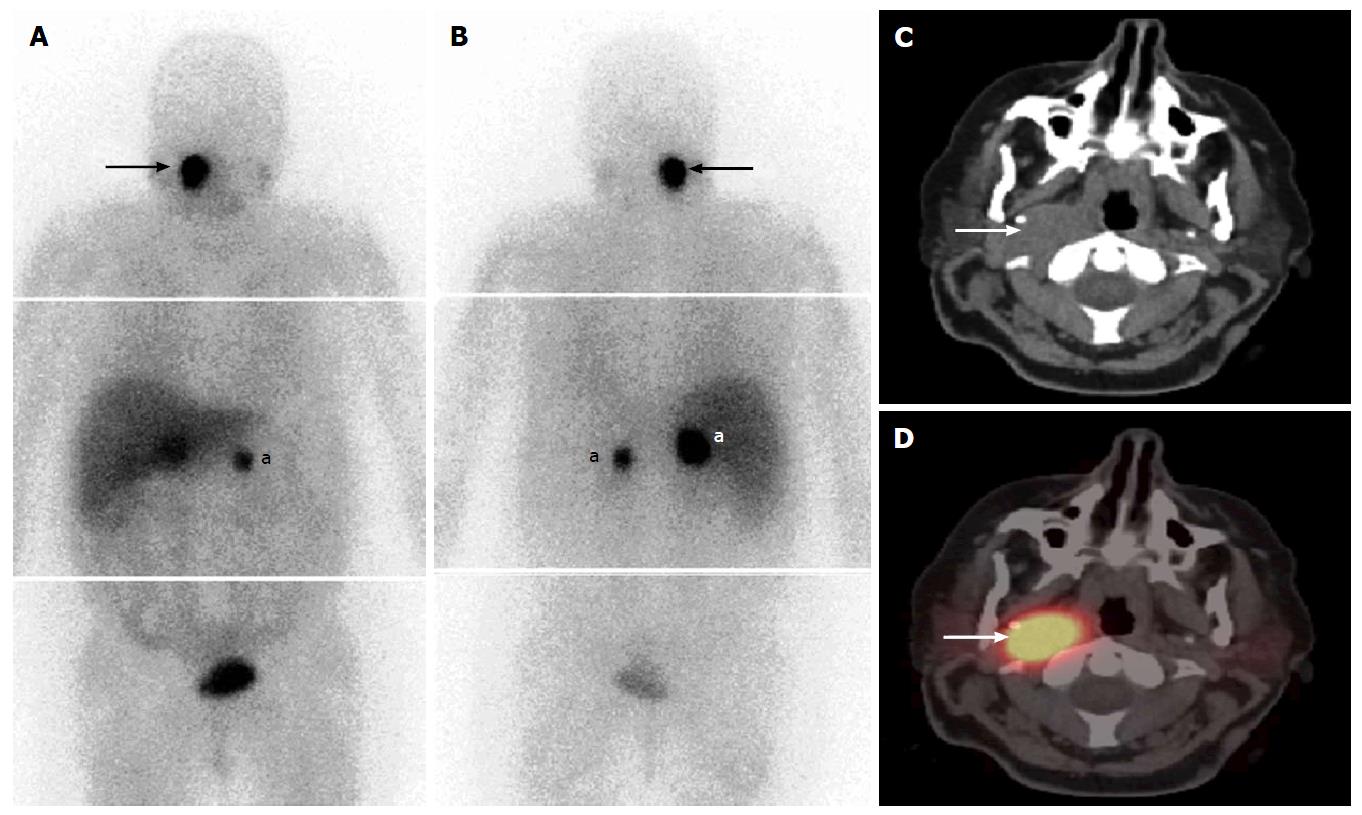
Figure 6 Fifty-three-year-old woman with uncontrolled hypertension and catecholamine hypersecretion, suspected for pheochromocytoma[123].
I-MIBG composite (A) anterior and (B) posterior whole-body images at 24 h post-injection show bilateral focal intense activity in the region of the adrenal glands (a), with unexpected MIBG avid mass in the right side of the neck (arrows). Axial fused SPECT/CT and CT (C, D) images clearly depict a right neck soft tissue mass with intense MIBG uptake (arrows). This indicates the presence of an extra-adrenal head and neck paraganglioma. SPECT: Single photon emission computed tomography; CT: Computed tomography; MIBG: Metaiodobenzylguanidine.
- Citation: Wong KK, Gandhi A, Viglianti BL, Fig LM, Rubello D, Gross MD. Endocrine radionuclide scintigraphy with fusion single photon emission computed tomography/computed tomography. World J Radiol 2016; 8(6): 635-655
- URL: https://www.wjgnet.com/1949-8470/full/v8/i6/635.htm
- DOI: https://dx.doi.org/10.4329/wjr.v8.i6.635