Copyright
©The Author(s) 2016.
World J Radiol. Feb 28, 2016; 8(2): 159-173
Published online Feb 28, 2016. doi: 10.4329/wjr.v8.i2.159
Published online Feb 28, 2016. doi: 10.4329/wjr.v8.i2.159
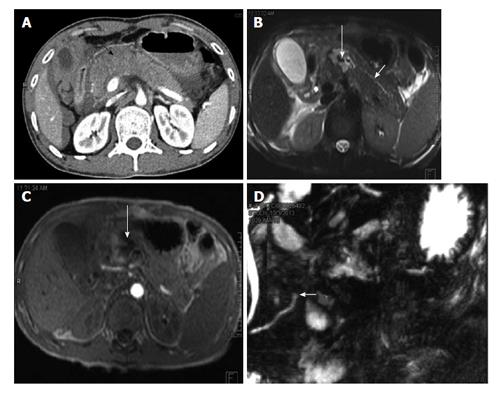
Figure 1 A 3-year-old girl with history of fall of heavy object over abdomen.
CECT axial image shows full thickness laceration (grade III injury) of neck of pancreas at level of splenoportal confluence (white arrow). Also note peripancreatic fluid (arrowhead) and fluid between splenic vein and body of pancreas (black arrow). Patient underwent a distal pancreatectomy. CECT: Contrast enhanced computed tomography.
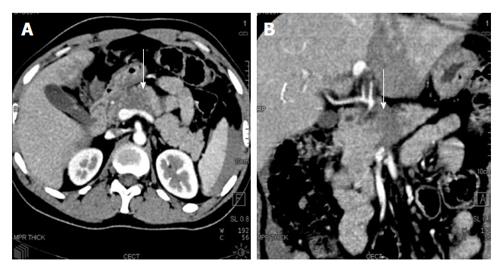
Figure 2 A 27-year-old woman with road traffic accident.
CECT axial (A) and coronal (B) images show full thickness laceration in the head of pancreas (white arrows). The laceration is located to the right of splenoportal confluence suggestive of grade IV injury. There is also fluid around the superior mesenteric vein (black arrow) and adjacent superior mesentery artery; the so-called “SMV cuff” sign seen in proximal injuries of pancreas. CECT: Contrast enhanced computed tomography; SMV: Superior mesenteric vein.
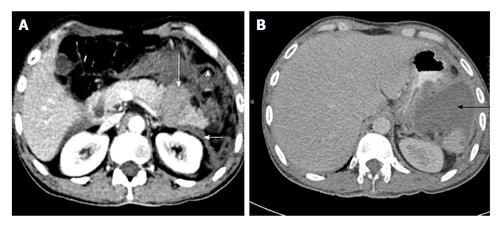
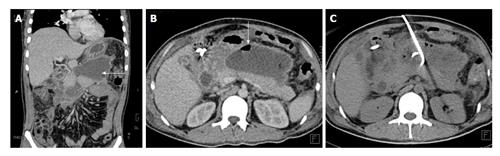
Figure 3 A 35-year-old truck driver with history of steering wheel impact injury.
CECT axial (A) and coronal oblique (B) images show a full thickness hypoattenuating band involving neck and body of pancreas (white arrow). On imaging, it was considered as a major contusion/grade II injury. Intraoperatively, full thickness laceration with duct injury was found suggestive of grade III injury and distal pancreatectomy was done. CECT: Contrast enhanced computed tomography.
Figure 4 A 30-year-old man with road traffic accident.
CECT axial (A) and coronal MPR (B) images show the hypoattenuating and bulky head of pancreas suggestive of major contusion with fluid in pancreaticoduodenal groove (arrow). Intra-operatively a hematoma was found in head and neck of pancreas (grade II injury). No active surgical intervention was done for pancreatic injury. CECT: Contrast enhanced computed tomography; MPR: Multiplanar reconstruction.
Figure 5 A 35-year-old man with road traffic accident.
CECT axial image at time of trauma (A) shows distal transection with fragments that separated by hyperattenuating fluid suggestive of hematoma (long white arrow). The left anterior renal fascia is also thickened (arrowhead). Patient underwent distal pancreatectomy and 4 wk follow up CECT axial image (B) show a post-operative collection in lesser sac (black arrow). CECT: Contrast enhanced computed tomography.
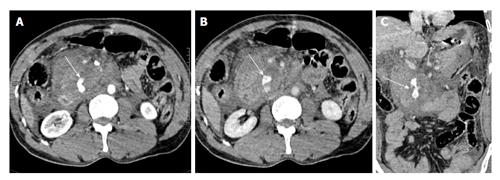
Figure 6 A 40-year-old man with history of fall of heavy object over abdomen.
CECT axial images, initial scan (A) and delayed scan (B) show complete disruption of head of pancreas with a large retroperitoneal hematoma replacing the head region. There is active extravasation of contrast (arrows). On coronal oblique image (C), the disrupted head of pancreas (arrow) with active contrast extravasation can be seen. Surgically, a crush injury (grade V) was confirmed and patient underwent Whipple’s procedure. The patient eventually died due to sepsis and multiorgan failure. CECT: Contrast enhanced computed tomography.
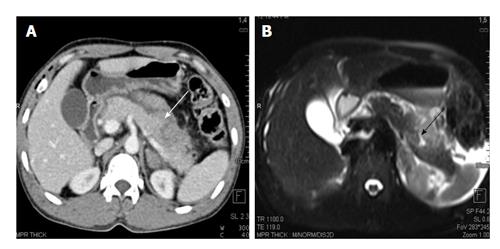
Figure 7 A 25-year-old man with history of blunt trauma abdomen.
CECT axial image (A) shows injury of distal pancreas (white arrow). MRI T2 HASTE axial image show T2 weighted hyperintensity in pancreatic body suggestive of contusion/edema with a small laceration (black arrow). CECT: Contrast enhanced computed tomography; MRI: Magnetic resonance imaging.
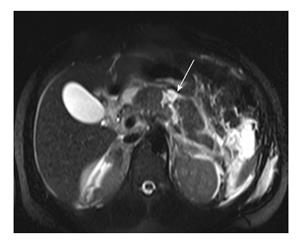
Figure 8 Magnetic resonance imaging T2 HASTE axial image of a 23-year-old man with road traffic accident show linear full thickness laceration in proximal body (arrow) suggestive of grade III injury.
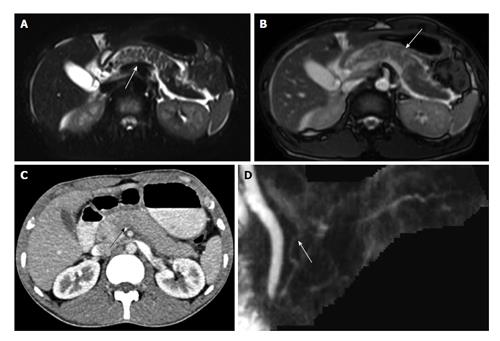
Figure 9 A 25-year-old man was involved in road traffic accident.
CECT axial image (A) shows ill-defined hypoattenuating area in neck of pancreas suggestive of contusion (arrow). MRI done 10 h after CT shows extent of contusion better with wider area of involvement on both T2 HASTE (B) and TRUFISP (C) images. MRCP thick MPR (D) image shows ductal integrity. Patient was conservatively managed and follow-up imaging showed decrease in area of contusion. CECT: Contrast enhanced computed tomography; MPR: Multiplanar reconstruction; TRUFISP: True fast imaging with steady-state free precession; MRI: Magnetic resonance imaging; MRCP: Magnetic resonance pancreatography; CT: Computed tomography.
Figure 10 A 23-year-old woman with history of road traffic accident.
Day 1 CECT axial image (A) shows ill-defined contusion in pancreatic neck (arrow). No obvious laceration was seen. Day 3 CECT axial (B) and coronal oblique (C) images show a full-thickness laceration in neck of pancreas s/o grade III injury with ductal involvement. Patient was operated and distal pancreatectomy was done. Thus there was evolution of injury from contusion to laceration. CECT: Contrast enhanced computed tomography.
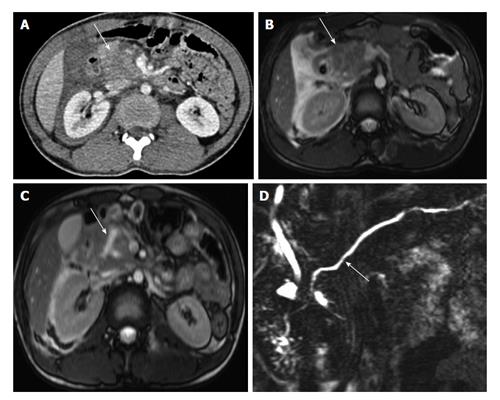
Figure 11 A 22-year-old man with history of fall of heavy object over abdomen.
CECT axial image (A) shows bulky heterogeneously attenuating head of pancreas (arrow). MRI done 28 h after CT (B) shows similar findings with bulky head and altered signal intensity with adjacent fluid (arrow B). No definite laceration seen. Follow-up MRI on day 6 (C) shows a Y shaped laceration in inferior part of head and uncinate process. However the main pancreatic duct was normal (arrow D). Since the MPD was not involved, conservative management was continued. CECT: Contrast enhanced computed tomography; MRI: Magnetic resonance imaging; CT: Computed tomography.
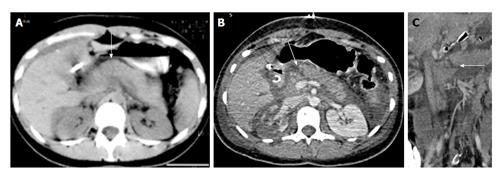
Figure 12 A 35-year-old man with history of road traffic accident.
CECT axial image (A) shows bulky hypoattenuating pancreas (black arrow) with peripancreatic fluid. No definite laceration was seen on CT and patient was kept on conservative management. MRI done 4 d later show hematoma/collection in neck of pancreas (long white arrows B and C). The duct was seen to communicate with the hematoma and MRCP showed cut off of duct at site of injury (short white arrow D). The patient subsequently underwent distal pancreatectomy. CECT: Contrast enhanced computed tomography; MRI: Magnetic resonance imaging; MRCP: Magnetic resonance pancreatography; CT: Computed tomography.
Figure 13 A 22-year-old man with history of road traffic accident, presenting on day 17 after trauma.
CECT axial image shows injury to distal body and tail of pancreas with peripancreatic collection (arrow). No imaging was done at time of trauma. Features are suggestive of traumatic pancreatitis following initial missed injury. Patient was conservatively managed with percutaneous drainage. CECT: Contrast enhanced computed tomography.
Figure 14 A 45-year-old man with missed pancreatic injury.
CECT coronal (A) and axial (B) image done weeks after injury shows an ill-defined walled off necrosis (arrow A) with air foci within (arrow B). CT guided pigtail drainage of collection was done (C) with antibiotic coverage. CECT: Contrast enhanced computed tomography; CT: Computed tomography.
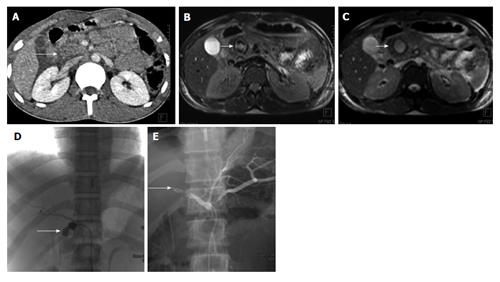
Figure 15 Post-traumatic common hepatic artery pseudoaneurysm 22 years old man with blunt trauma abdomen.
CECT axial image shows injury to head of pancreas (arrow A). MRI done 3 d later showed well defined lesion in head of pancreas with heterogeneous signal intensity on T1 weighted image (arrow B) and hyperintense on TRUFISP image (arrow C). A possibility of pseudoaneurysm was given. Angiogram showed pseudoaneurysm arising from proximal common hepatic artery (arrow D) which was embolised with Nester coils (arrow E). CECT: Contrast enhanced computed tomography; MRI: Magnetic resonance imaging; TRUFISP: True fast imaging with steady-state free precession.
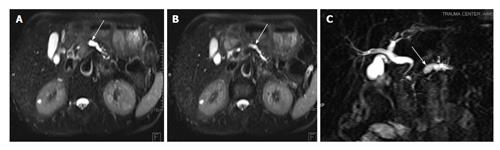
Figure 16 A 40-year-old male with previous history of pancreatic trauma.
Injury was missed at time of presentation. Follow up MRI T2 HASTE images (A and B) and MRCP image (C) show dilated main pancreatic duct and side branches (arrows A and B) with cut off in proximal body region (arrow C) suggestive of post-traumatic pancreatic stricture. MRI: Magnetic resonance imaging; MRCP: Magnetic resonance pancreatography.
- Citation: Kumar A, Panda A, Gamanagatti S. Blunt pancreatic trauma: A persistent diagnostic conundrum? World J Radiol 2016; 8(2): 159-173
- URL: https://www.wjgnet.com/1949-8470/full/v8/i2/159.htm
- DOI: https://dx.doi.org/10.4329/wjr.v8.i2.159