Copyright
©2014 Baishideng Publishing Group Inc.
World J Radiol. Jul 28, 2014; 6(7): 424-436
Published online Jul 28, 2014. doi: 10.4329/wjr.v6.i7.424
Published online Jul 28, 2014. doi: 10.4329/wjr.v6.i7.424
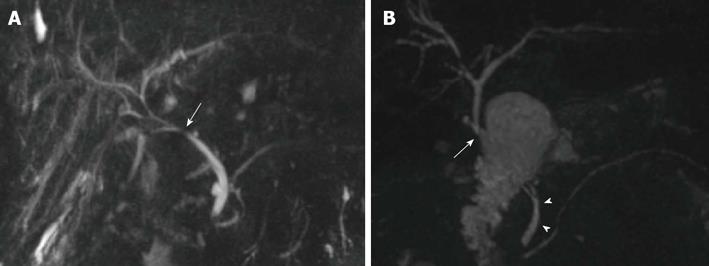
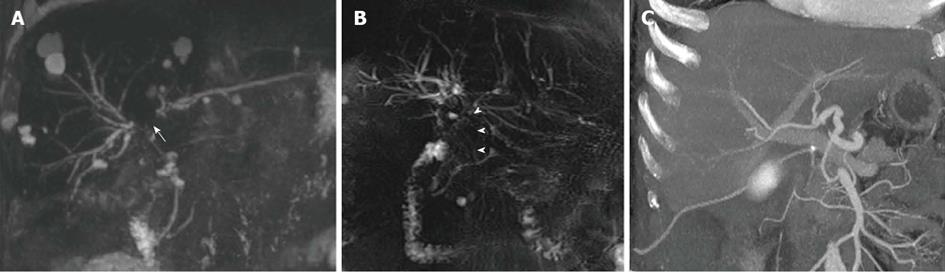
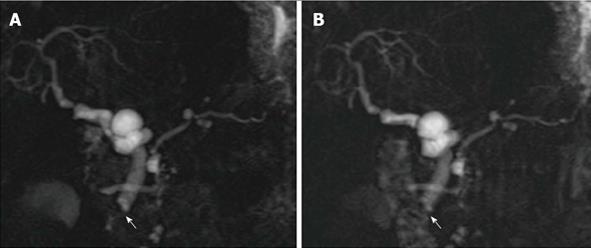
Figure 1 Biliary reconstructions variants after orthotopic liver transplantation illustrated by coronal maximum intensity projection reconstruction from 3D magnetic resonance cholangiography.
A: Choledocho-choledochostomy with mild donor-to-recipient discrepancy in ductal calibers giving prominence to the anastomotic site (arrow); B: Bilioenteric anastomosis (arrow) between donor’s common bile duct and a jejuneal loop. Note the recipient common bile duct remnant (arrowheads).
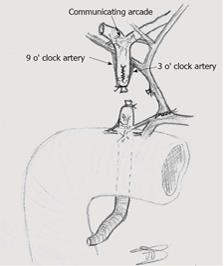
Figure 2 Arterial supply to the biliary tree in liver-transplanted patients.
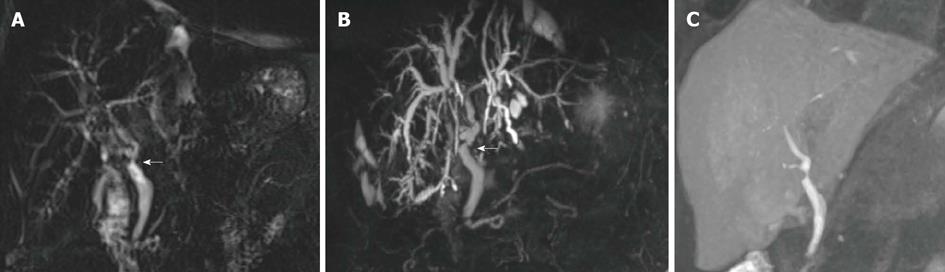
Figure 3 Technical variants of magnetic resonance cholangiography, as shown in coronal images of a 66-year-old male patient transplanted for alcoholic cirrhosis.
A: Conventional, T2-weighted 2D MRC; B: MIP reconstruction from conventional, T2-weighted 3D MRC; C: Thick MIP reconstruction from T1-weighted, contrast-enhanced MRC. Both the degree and functional significance of the mild anastomotic stricture indicated by arrows are better showed by contrast passage in (C). MRC: Magnetic resonance cholangiography; MIP: Maximum intensity projection.
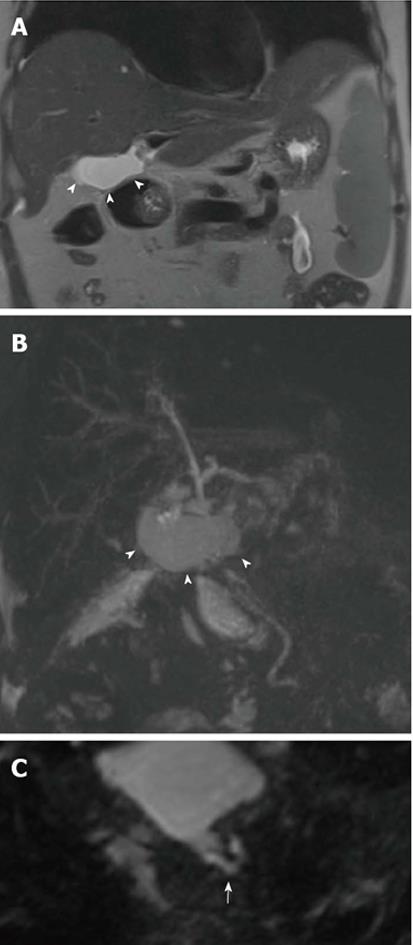
Figure 4 Bile leakage in a 54-year-old male subject transplanted for hepatitis C virus-related cirrhosis.
Perihilar biloma shown by arrowheads on coronal T2-weighted HASTE image (A) and paracoronal MIP reconstruction from 3D MRC (B). Thin communication between the anastomotic site and fluid collection is visible on the axially-reformatted 3D source image (arrow in C). MRC: Magnetic resonance cholangiography; MIP: Maximum intensity projection.
Figure 5 Nonanastomotic strictures in two different transplanted patients.
A: MIP reconstruction shows early effects of HAT in a 58-year-old subject with hepatitis B virus infection, consisting in a stricture of the hepatic confluence (arrow) and multiple intrahepatic bilomas; B: ITBL in a 68 male patient transplanted for alcoholic cirrhosis. 2D MRC image shows a stricture of the hepatic confluence extended to the donor common hepatic duct (arrowheads); C: CT angiography found patent hepatic artery in this patient. MRC: Magnetic resonance cholangiography; MIP: Maximum intensity projection; ITBL: Ischemic-type biliary lesions.
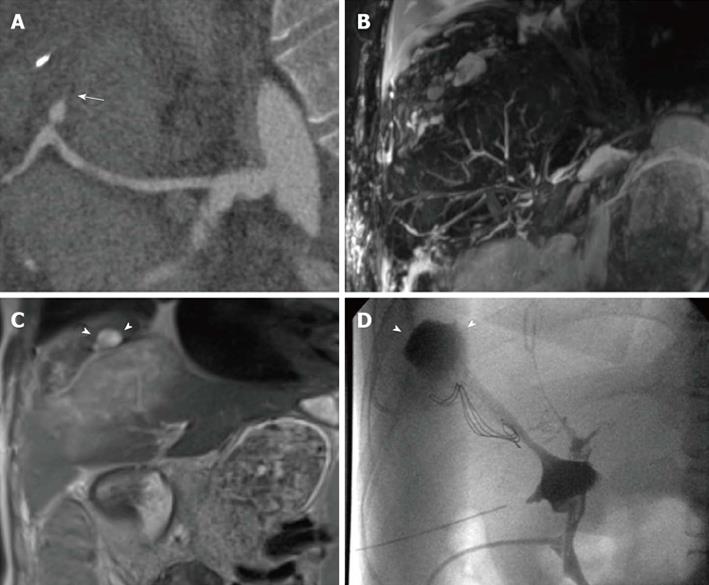
Figure 6 Multiple findings in a 28-year-old female patient transplanted for primary sclerosing cholangitis.
Because of the hepatic artery thrombosis shown on curved-reformatted CT image (arrow in A), the biliary tree appears as fragmented and anatomically ill-defined on a panoramic maximum intensity projection view (B). Coronal T2-weighted HASTE image (C) shows extensive, hyperintense ischemic damage of liver parenchyma, together with intrahepatic fluid collections (arrowheads) confirmed to be the effect of bile leakage on T-tube cholangiography (arrowheads in D).
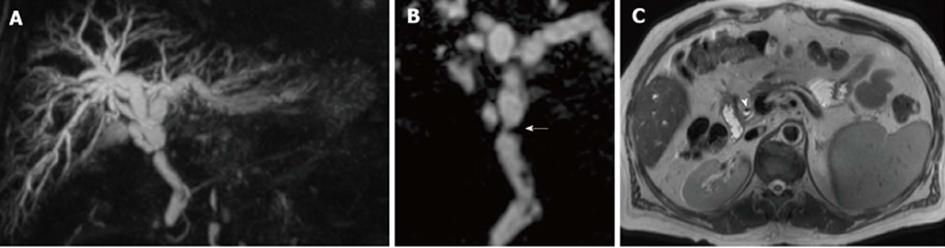
Figure 7 Calculi in a 62-year-old male subject who underwent orthotopic liver transplantation for hepatitis C virus-infection and hepatocellular carcinoma.
A: The patient shows chronic kinking and moderate anastomotic stricture without biliary obstruction; B: Filling defect visible in the distal common bile duct were confirmed on axial HASTE image (arrow) and proven to be small calculi on ERC.
Figure 8 Anastomotic stricture in a 54-year-old male patient who underwent orthotopic liver transplantation for alcoholic cirrhosis.
A: Coronal MIP reconstruction shows the stricture at the middle third of the extrahepatic bile duct, with biliary dilatation upstream; B: The degree of the stricture is better delineated on the paracoronally-reformatted thin 3D image (arrow); C: Filling defects visible on MRC images correspond to pneumobilia, appearing as air-fluid levels (arrowhead) on the axial T2-weighted HASTE sequence. MRC: Magnetic resonance cholangiography; MIP: Maximum intensity projection.
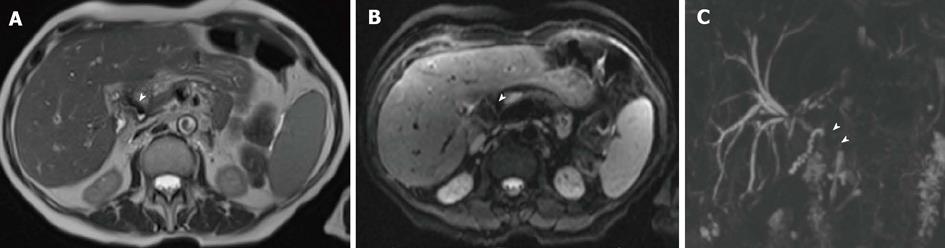
Figure 9 Aerobilia in a 62-year-old female patient transplanted for alcoholic cirrhosis.
Anintense filling defect in the common bile duct on T2-weighted axial HASTE image (arrowhead in A) is associated to distortion artifact on axial Diffusion-weighted sequence (arrowhead in B). The effect of pneumobilia was to extensively mask the common bile duct on 3D magnetic resonance cholangiography (arrowheads in C).
Figure 10 Sphincter of Oddi dysfunction in a liver-transplanted female patient with cholestasis and abdominal complaint years after orthotopic liver transplantation.
Serial 2D cinematic magnetic resonance cholangiography images (A) and (B) acquired after few seconds show redundancy of the reconstructed common bile duct, which appear slightly dilated in the recipient tract, and persistent lack of visualization of the vaterian sphincter complex, with typical “meniscus sign” (arrow) suggesting spasm.
- Citation: Girometti R, Cereser L, Bazzocchi M, Zuiani C. Magnetic resonance cholangiography in the assessment and management of biliary complications after OLT. World J Radiol 2014; 6(7): 424-436
- URL: https://www.wjgnet.com/1949-8470/full/v6/i7/424.htm
- DOI: https://dx.doi.org/10.4329/wjr.v6.i7.424