Copyright
©2014 Baishideng Publishing Group Inc.
World J Radiol. May 28, 2014; 6(5): 148-159
Published online May 28, 2014. doi: 10.4329/wjr.v6.i5.148
Published online May 28, 2014. doi: 10.4329/wjr.v6.i5.148
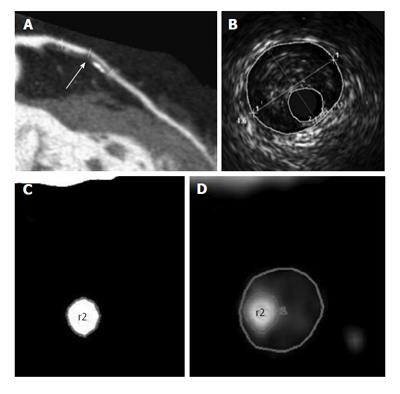
Figure 1 The window settings for the lumen and outer vessel boundary by computed tomography angiography are the same as those for intravascular ultrasound imaging[15].
A: A curved multiplanar reconstructed CTA image reveals a significant stenosis in the left anterior descending artery (arrow); B: An IVUS cross-section reveals a lumen area of 2.1 mm2 and a vessel area of 15.4 mm2; C: The cross-sectional CTA images show the luminal CSA of 2.1 mm2; D: Vessel CSA of 15.4 mm2. CTA: Computed tomography angiography; IVUS: Intravascular ultrasound; CSA: Cross-sectional area.
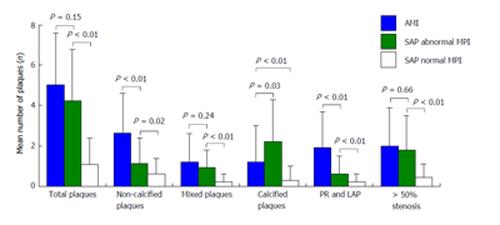
Figure 2 Mean number of the coronary plaques in the non-culprit segments of the acute myocardial infarction and stable angina pectoris patients[24].
AMI: Acute myocardial infarction; SAP: Stable angina pectoris; MPI: Myocardial perfusion imaging; PR: Positive remodeling; LAP: Low-attenuation plaques.
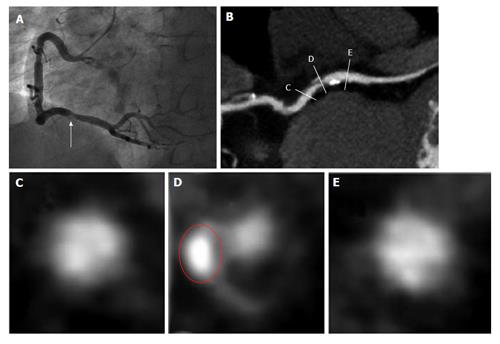
Figure 3 The computed tomography characteristics of a culprit lesion in the 52-year-old male patient with post-percutaneous coronary intervention troponin T elevation ≥ 3 × the upper limit of normal[31].
Coronary angiogram (A) and multiplanar reconstructed image (B) show severe stenosis in the mid right coronary artery. Cross-sectional images show the proximal reference (C), culprit lesion (D), and distal reference (E). The lesion has positive remodeling (remodeling index 1.28), spotty calcification, and low CT density (16 HU). Red circle indicates area of spotty calcification. CT: computed tomography; HU: Hounsfield units.
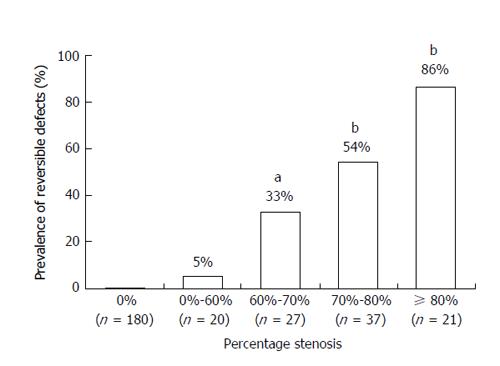
Figure 4 Prevalence of reversible defects evaluated by single-photon emission tomography in the study groups defined according to the percentage stenosis obtained by computed tomography angiography[15].
Numbers under the bars represent the number of vessels. aP = 0.018, bP < 0.0001 vs percentage stenosis of 0%-60%.
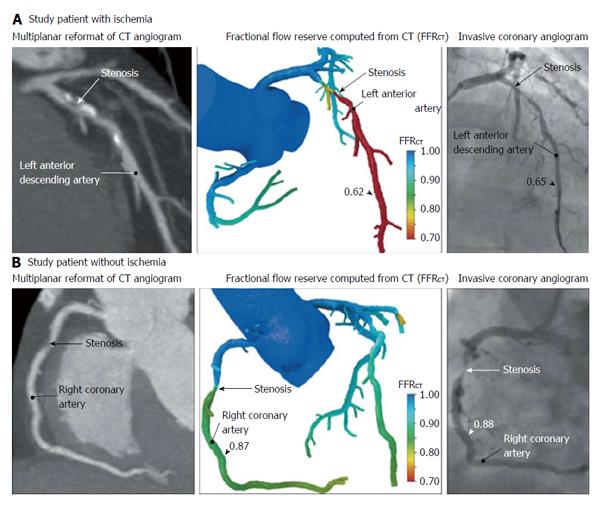
Figure 5 One patient (A) has ischemia and the other patient (B) does not have ischemia[49].
A: Multiplanar reformat of a computed tomography (CT) angiogram demonstrating obstructive stenosis of the proximal portion of the left anterior descending artery (LAD) and a computed fractional flow reserve (FFRCT) value of 0.62, indicating vessel ischemia. Invasive coronary angiogram demonstrates obstructive stenosis of the proximal portion of the LAD and measured fractional flow reserve (FFR) values of 0.65, indicating vessel ischemia; B: CT angiogram demonstrating obstructive stenosis of the mid portion of the right coronary artery (RCA) and an FFRCT value of 0.87, indicating no vessel ischemia. Invasive coronary angiogram demonstrates obstructive stenosis of the mid portion of the RCA and a measured FFR value of 0.88, indicating no vessel ischemia.
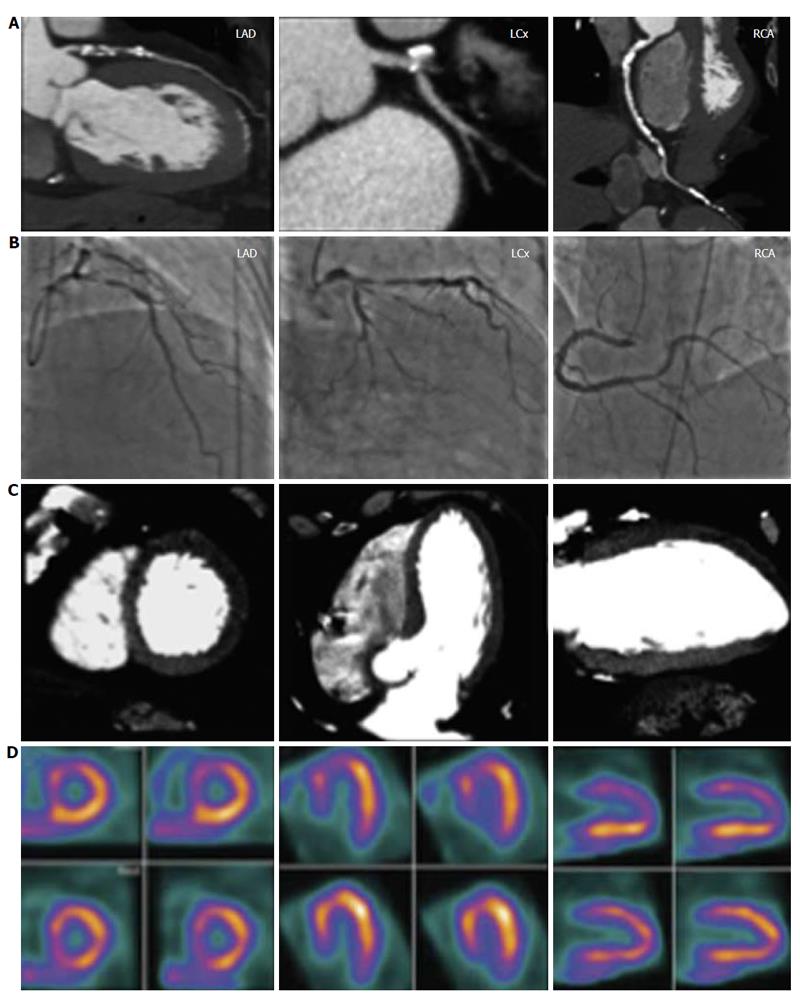
Figure 6 A complete CORE320 imaging data set for a 64-year-old male without prior history of coronary artery disease with chest pain symptoms[50].
The left anterior descending coronary artery revealed a 96% diameter stenosis by computed tomography angiography (CTA) (row A) and an 85% diameter stenosis by invasive coronary angiography (ICA) (row B). The computed tomography myocardial perfusion (CTP) (row C) study revealed a mild defect in the distal anteroseptal wall, and moderate defects in the basal anteroseptal, the basal anterior, the distal anterior, and apical walls, while the single photon emission computed tomography (SPECT) (row D) study revealed moderate defects in the distal anterior, the distal anteroseptal, the basal anteroseptal and apical walls. The left circumflex artery revealed an 87% diameter stenosis by CTA, a 79% diameter stenosis by ICA, mild defects in the distal inferoseptal and distal inferolateral walls, and moderate defects in the distal anterolateral and distal anterior walls by CTP, and a moderate defect in the distal anterior wall by SPECT. The right coronary artery revealed a 60% diameter stenosis by CTA, a 77% diameter stenosis by ICA, a mild defect in the distal inferoseptal wall by CTP, and no myocardial perfusion defects by SPECT.
- Citation: Sato A. Coronary plaque imaging by coronary computed tomography angiography. World J Radiol 2014; 6(5): 148-159
- URL: https://www.wjgnet.com/1949-8470/full/v6/i5/148.htm
- DOI: https://dx.doi.org/10.4329/wjr.v6.i5.148