Copyright
©2013 Baishideng Publishing Group Co.
World J Radiol. Nov 28, 2013; 5(11): 436-445
Published online Nov 28, 2013. doi: 10.4329/wjr.v5.i11.436
Published online Nov 28, 2013. doi: 10.4329/wjr.v5.i11.436
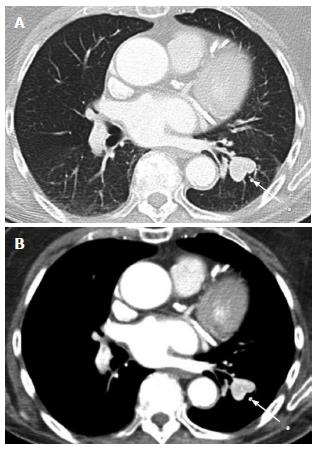
Figure 1 Axial computerized tomography images of the chest in lung and soft tissue windows in an 86-year-old female patient status post nephrectomy who developed pulmonary metastases 10 years later.
Note the bright enhancement of the lesion (arrow) on soft tissue windows.
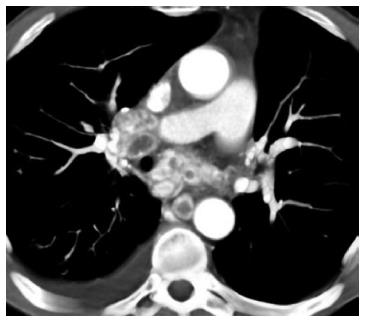
Figure 2 Numerous mediastinal nodes in a 65-year-old male patient status post nephrectomy 6 years earlier.
Note the peripheral enhancement and central necrosis.
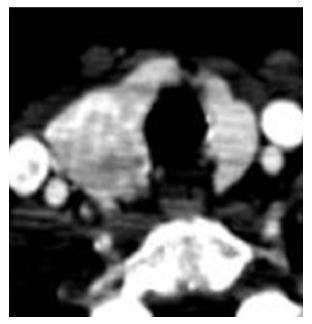
Figure 3 A 67-year-old female status post left partial nephrectomy 2 years prior to this exam.
Asymmetric enlargement of the right thyroid gland secondary to a thyroid nodule which was subsequently biopsied as metastatic renal cell carcinoma; Note the nodule enhances as brightly as the remainder of the thyroid.
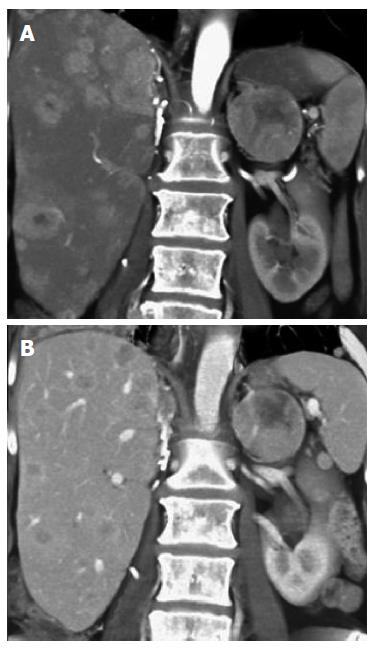
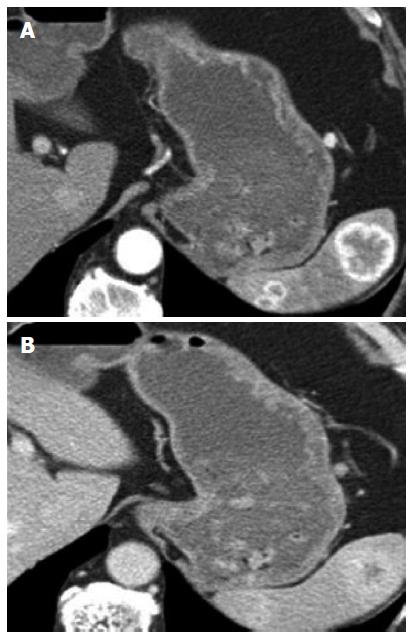
Figure 4 A 67-year old-female with widespread liver metastases after right nephrectomy.
Note the increased conspicuity of the liver lesions on arterial phase (A) compared to venous phase (B) coronal volume renderings. A left adrenal metastasis is also seen.
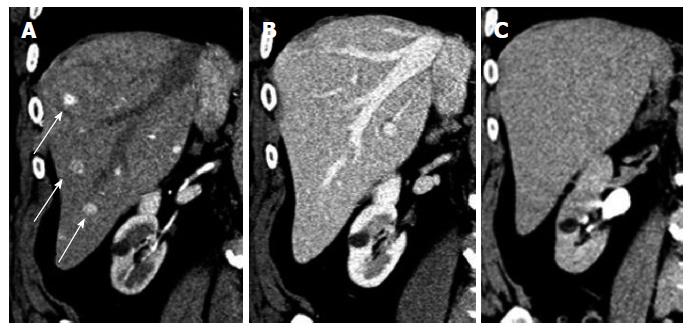
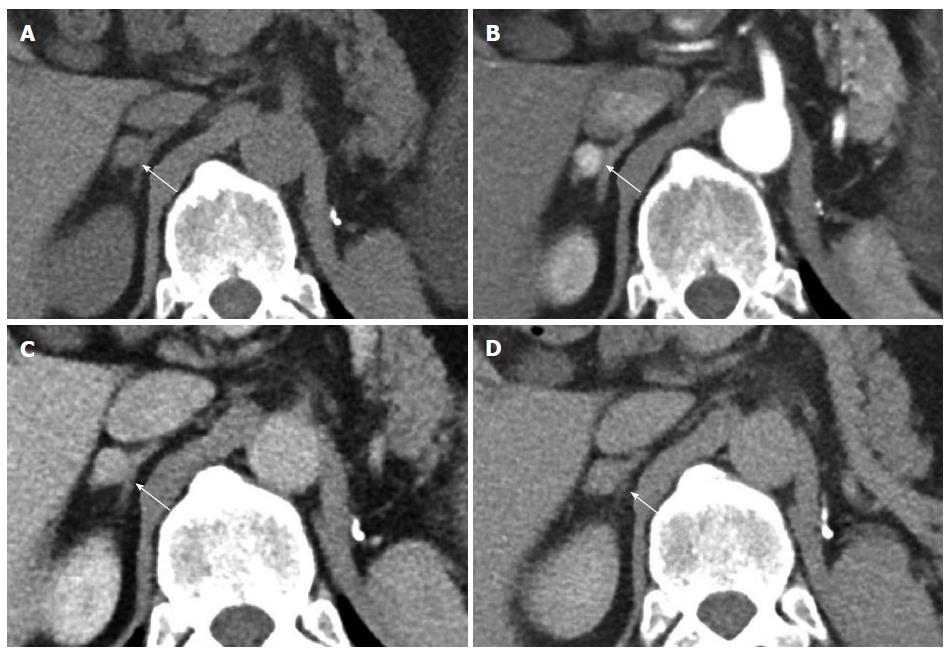
Figure 5 Multiphase exams in another 73-year-old male patient with liver metastases.
The liver metastases (arrow) are most obvious on the arterial phase (A), but are subtle or isoattenuating on venous and delayed phases (B, C).
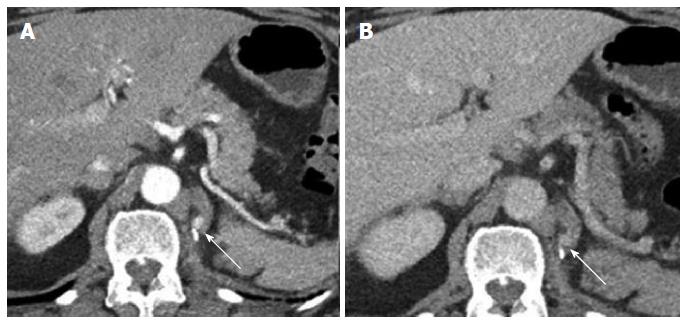
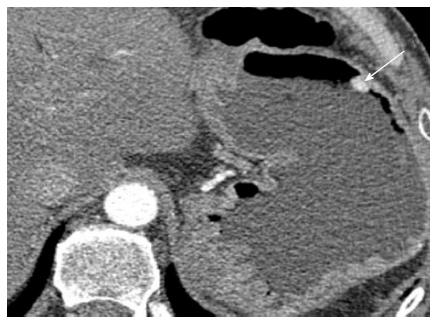
Figure 6 A 65-year-old female patient who underwent nephrectomy more than 10 years prior.
Axial IV contrast enhanced CT shows 7 mm recurrence in the surgical bed (arrow). The lesion is easily seen on arterial phase (A) and but becomes indistinguishable on the venous phase (B).
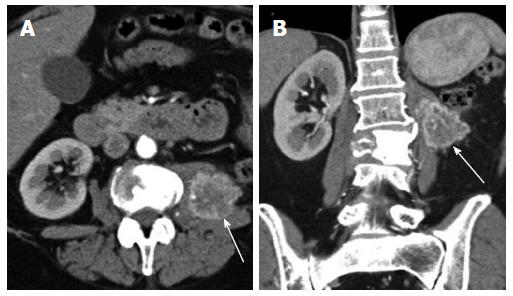
Figure 7 A 60-year-old female status post left nephrectomy with hypervascular recurrence (arrow) on the side of resection, involving the left psoas muscle.
Figure 8 A 72-year-old female status post left nephrectomy who developed a new mass in the contralateral kidney.
Note the subtle lesion in the upper pole (arrow), on coronal volume rendering (A) and axial arterial phase CT (B). CT: Computerized tomography.
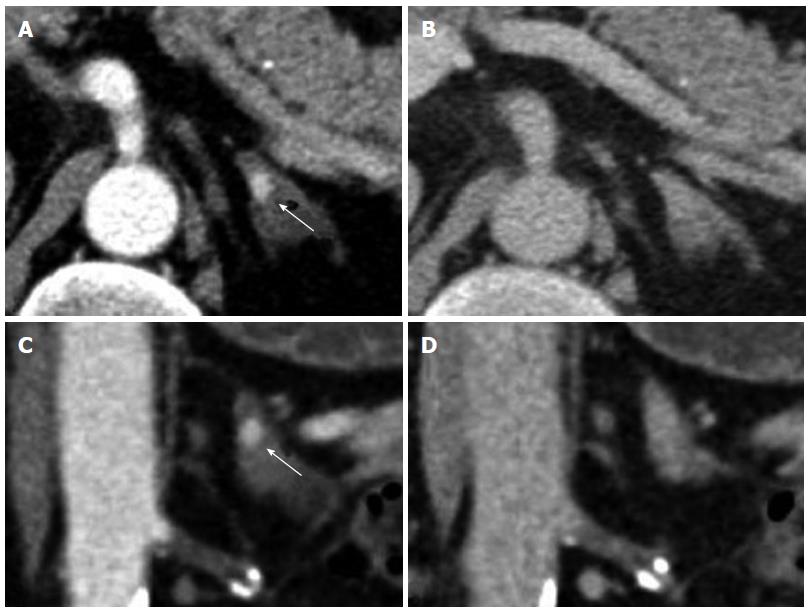
Figure 9 Right adrenal mass in a 54-year-old male patient status post left nephrectomy four years prior to the exam.
A: Non-contrast; B: Arterial; C: Venous phase; D: Delayed phase. On non-contrast the lesion measures 33 HU; on arterial phase the lesion measures 180 HU; on venous phase the lesion measures 101 HU; on delayed phase the lesion measures 57 HU (arrow, right adrenal mass). Absolute washout is 65% and the relative washout is 44%. By washout, this lesion is compatible with adenoma. However, the hypervascularity of the lesion (> 100 HU) is atypical for adenoma, suggesting metastasis.
Figure 10 Subcentimeter hypervascular lesion in the left adrenal gland of a 65-year-old male patient who underwent a left nephrectomy 3 years prior.
Note despite the small size it is easily seen on arterial phase (A, C) and is virtually undetectable on venous phase (B, D).
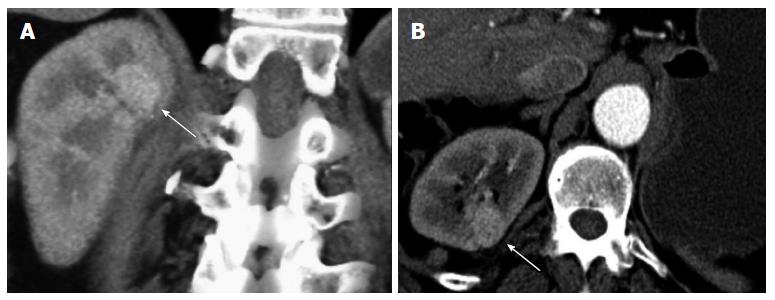
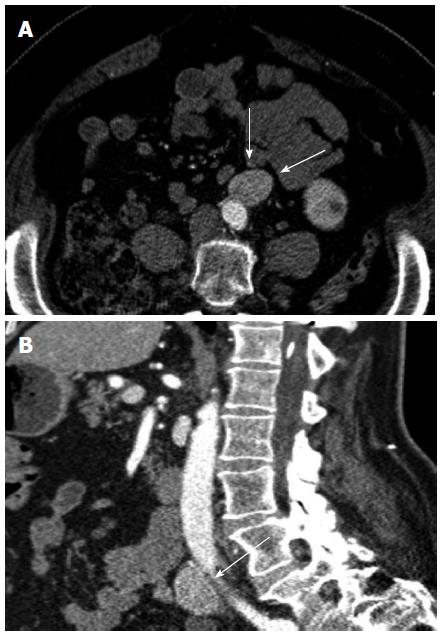
Figure 11 A 55-year-old female status post right nephrectomy.
Axial (A) and sagittal (B) images of left para-aortic lymphadenopathy in patient who underwent right nephrectomy six years earlier. The patient also had left supraclavicular lymphadenopathy.
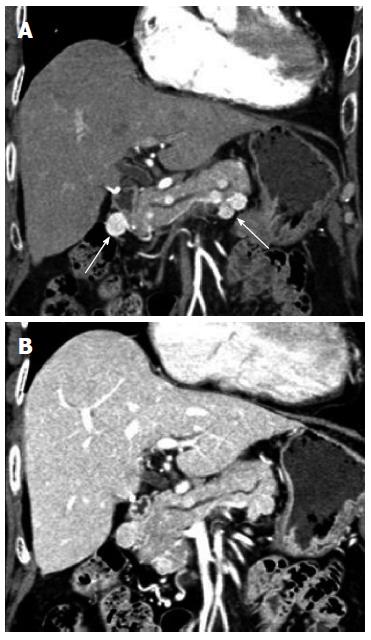
Figure 12 A 66-year-old female status post left radical nephrectomy 12 years earlier.
Multiple rounded hypervascular masses within the pancreas on arterial phase (A) which are nearly isodense to the pancreas on venous phase (B).
Figure 13 A 64-year-old male status post right nephrectomy that developed splenic metastases 7 years later.
Note the increased conspicuity of the lesions on arterial phase (A). On venous phase, the lesions are nearly isodense to the spleen (B).
Figure 14 A 65-year-old male status post left radical nephrectomy in who developed a gastric metastasis (arrow) 5 years later.
The patient subsequently underwent partial gastrectomy.
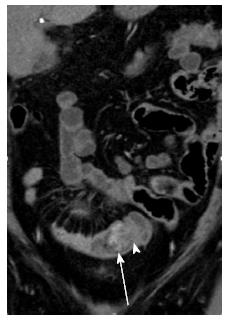
Figure 15 A 60-year-old female status post left nephrectomy presenting with a small bowel metastasis.
Note a subtle intraluminal enhancing mass (arrow) serving as lead point for short segment intussussception (arrowhead). The lesion is best appreciated on coronal MPR images in arterial phase.
Figure 16 A 60-year-old female status post left radical nephrectomy with liver and bony metastases and with bilateral ovarian metastases.
Axial CT image in arterial phase shows a large cystic and solid mass seen in right ovary and solid hypervascular mass in left ovary. The solid components of the cystic mass are hypervascular on arterial phase.
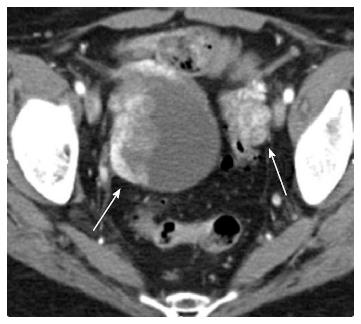
Figure 17 A 63-year-old male status post right nephrectomy subsequently developed bone metastasis in the left iliac wing.
Axial arterial phase image shows a lytic lesion with a soft tissue component that shows prominent enhancement peripherally with central necrosis.
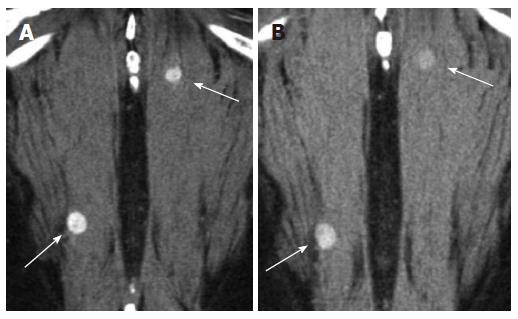
Figure 18 A 66-year-old male status post left nephrectomy, developed metastases within the paraspinal muscles 3 years later.
These small lesions (arrows) are often best visualized on the arterial acquisition (A) and inconspicuous on venous (B) and delayed phase.
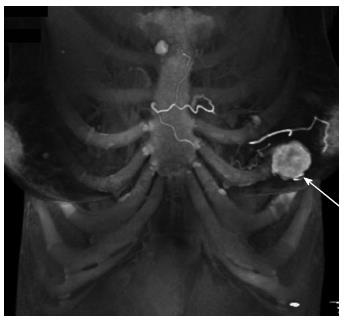
Figure 19 A 67-year-old female with widespread metastatic renal cell carcinoma.
A hypervascular metastasis (arrow) in the left breast, seen on this 3D volume rendered image in arterial phase.
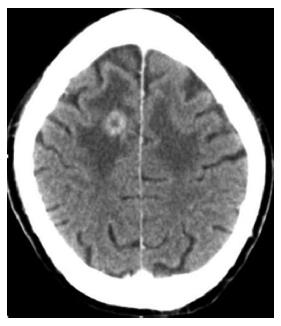
Figure 20 A 81-year-old male status post left radical nephrectomy with bilateral frontal lobe metastases.
Enhancing lesion in the right frontal lobe with surrounding vasogenic edema. Vasogenic edema is also seen in the left frontal lobe secondary to another metastatic lesion located more inferiorly.
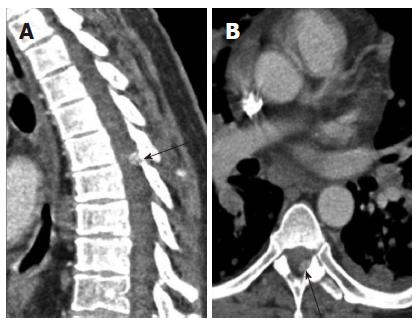
Figure 21 A 56-year-old male with diffuse metastatic disease and an enhancing dural based nodule.
A: In the thoracic spine seen on sagittal (arrow); B: Axial images. Subsequent magnetic resonance imaging showed a dural based metastasis; Sagittal multiplanar reconstruction is helpful in lesion detection for spinal metastasis.
- Citation: Coquia SF, Johnson PT, Ahmed S, Fishman EK. MDCT imaging following nephrectomy for renal cell carcinoma: Protocol optimization and patterns of tumor recurrence. World J Radiol 2013; 5(11): 436-445
- URL: https://www.wjgnet.com/1949-8470/full/v5/i11/436.htm
- DOI: https://dx.doi.org/10.4329/wjr.v5.i11.436