Copyright
©2012 Baishideng Publishing Group Co.
World J Radiol. Mar 28, 2012; 4(3): 121-125
Published online Mar 28, 2012. doi: 10.4329/wjr.v4.i3.121
Published online Mar 28, 2012. doi: 10.4329/wjr.v4.i3.121
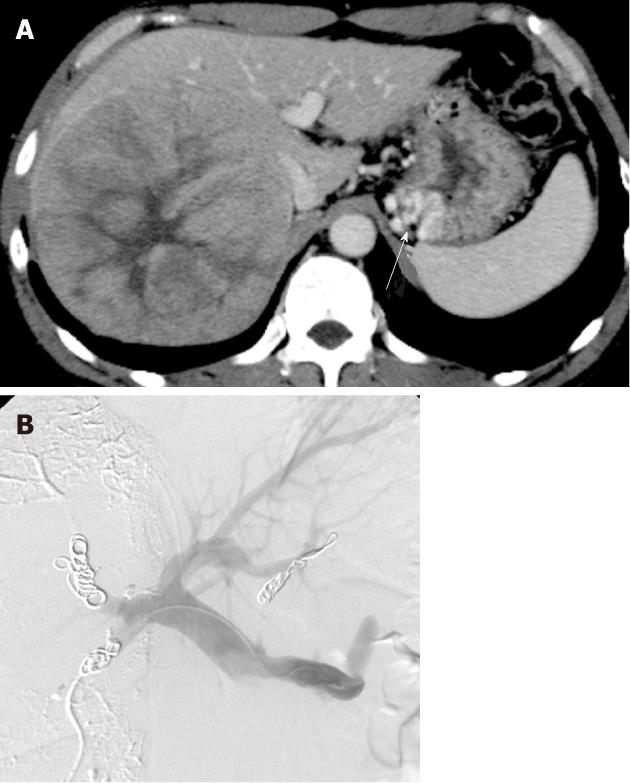
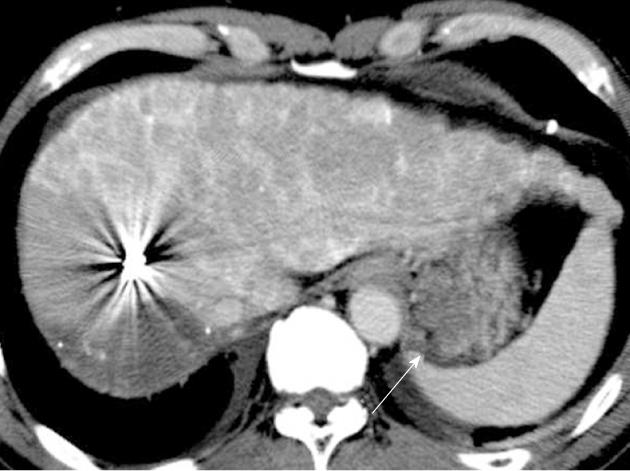
Figure 1 A 55-year-old man with gastric varices due to hepatitis B liver cirrhosis.
A: Hepatocellular carcinoma of 13 cm in the right lobe. Gastric varices were also demonstrated (arrow); B: Percutaneous transhepatic obliteration of the posterior gastric vein using 5% ethanolamine oleate-iopamidol and microcoils was performed to occlude the gastric varices. Percutaneous transhepatic portal vein embolization of the right posterior and anterior segments of the portal vein using lipiodol, gelatin sponge particles and microcoils was conducted using the same transhepatic catheter route in order to enlarge the left hepatic lobe for possible right hepatectomy.
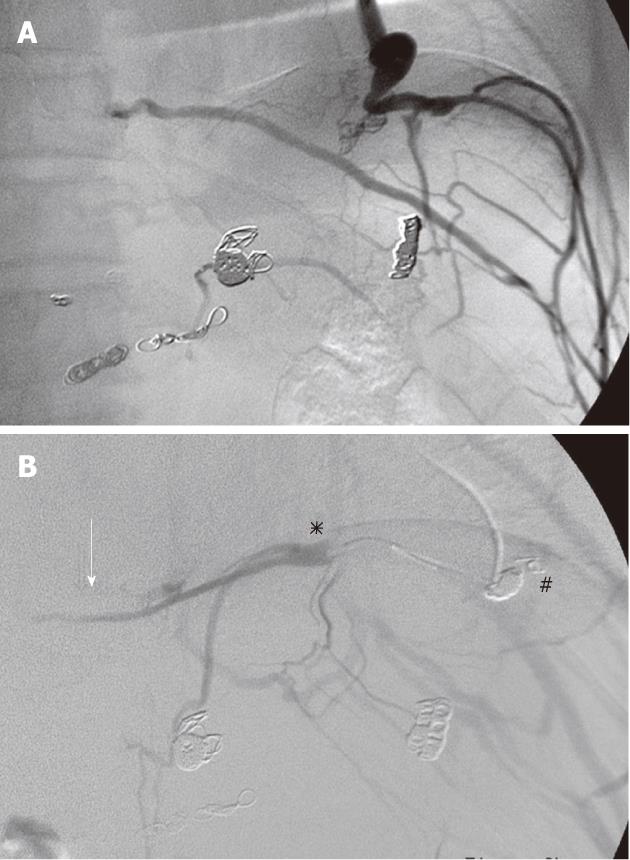
Figure 2 Micro-balloon-occluded pericardial venography.
A: Micro-balloon occluded venography (M-BOV) of the pericardial vein demonstrated the development of the cardio-phrenic vein and phrenic branch veins; B: Embolization of the cardio-phrenic vein using 9 microcoils (#) was conducted in order to reduce the collateral vessels. However, M-BOV of the left subphrenic vein (asterisk) followed by coil embolization demonstrated the narrow outlet of the subphrenic vein (arrow) and the dilated phrenic branches but not gastric varices. Further advancement of the micro-balloon catheter was difficult.
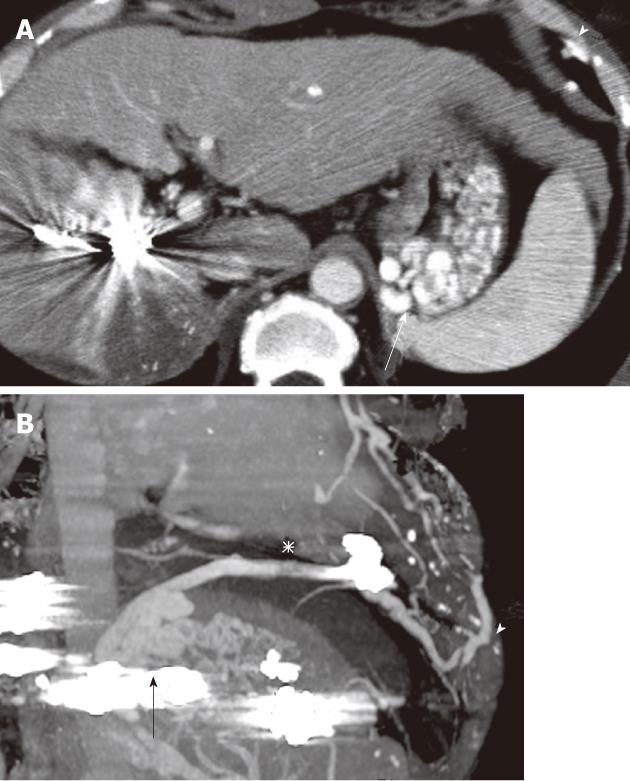
Figure 3 Portal phase of dynamic computed tomography images using contrast medium before balloon-occluded retrograde transvenous obliteration.
A: Axial image demonstrated enlargement of gastric varices (arrow) and intercostal vein (arrowhead) with marked shrinkage of hepatocellular carcinoma; B: Multi-planar reconstruction computed tomography image demonstrated the gastric varices (arrow) and the dilated phrenic branch (asterisk) communicating with intercostal vein (arrowhead).
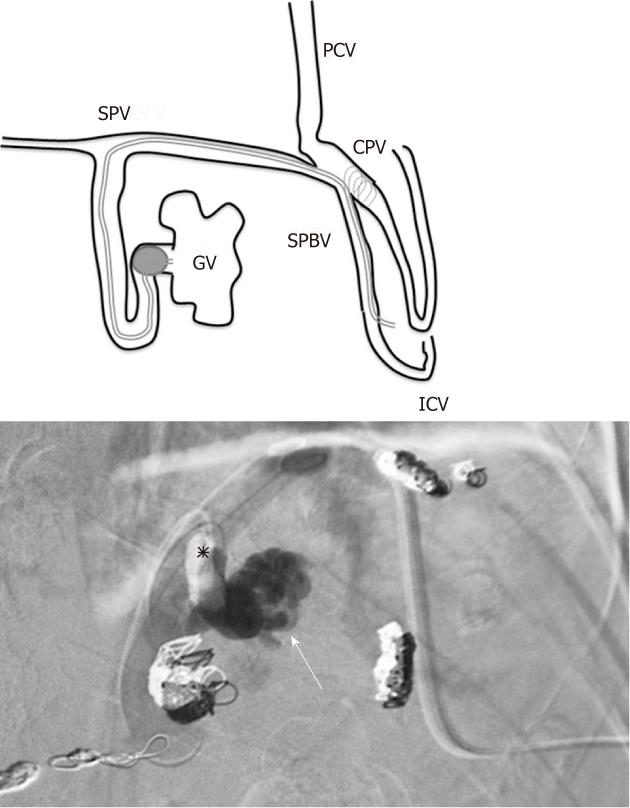
Figure 4 The strategy and actual images of balloon-occluded retrograde transvenous obliteration via the intercostal vein.
A: Schema of the micro-balloon catheter inserted via the 7th intercostal vein (ICV) and advanced to the gastric varices (GV) through the subphrenic branch vein (SPBV) and subphrenic vein (SPV); B: After balloon inflation (asterisk), balloon-occluded retrograde transvenous obliteration (BRTO) using 5% ethanolamine oleate-iopamidol (EOI) and ethanol mixed with lipiodol was conducted. The radiograph immediately after BRTO showed the accumulation of EOI corresponding to the gastric varices (arrow). PCV: Pericardial vein; CPV: Cardio-phrenic vein.
Figure 5 Dynamic computed tomography the following day showed no enhancement of gastric varices (arrow).
-
Citation: Minamiguchi H, Kawai N, Sato M, Ikoma A, Sawa M, Sonomura T, Sahara S, Nakata K, Takasaka I, Nakai M. Balloon-occluded retrograde transvenous obliteration for gastric varices
via the intercostal vein. World J Radiol 2012; 4(3): 121-125 - URL: https://www.wjgnet.com/1949-8470/full/v4/i3/121.htm
- DOI: https://dx.doi.org/10.4329/wjr.v4.i3.121