Copyright
©The Author(s) 2025.
World J Radiol. Feb 28, 2025; 17(2): 102373
Published online Feb 28, 2025. doi: 10.4329/wjr.v17.i2.102373
Published online Feb 28, 2025. doi: 10.4329/wjr.v17.i2.102373
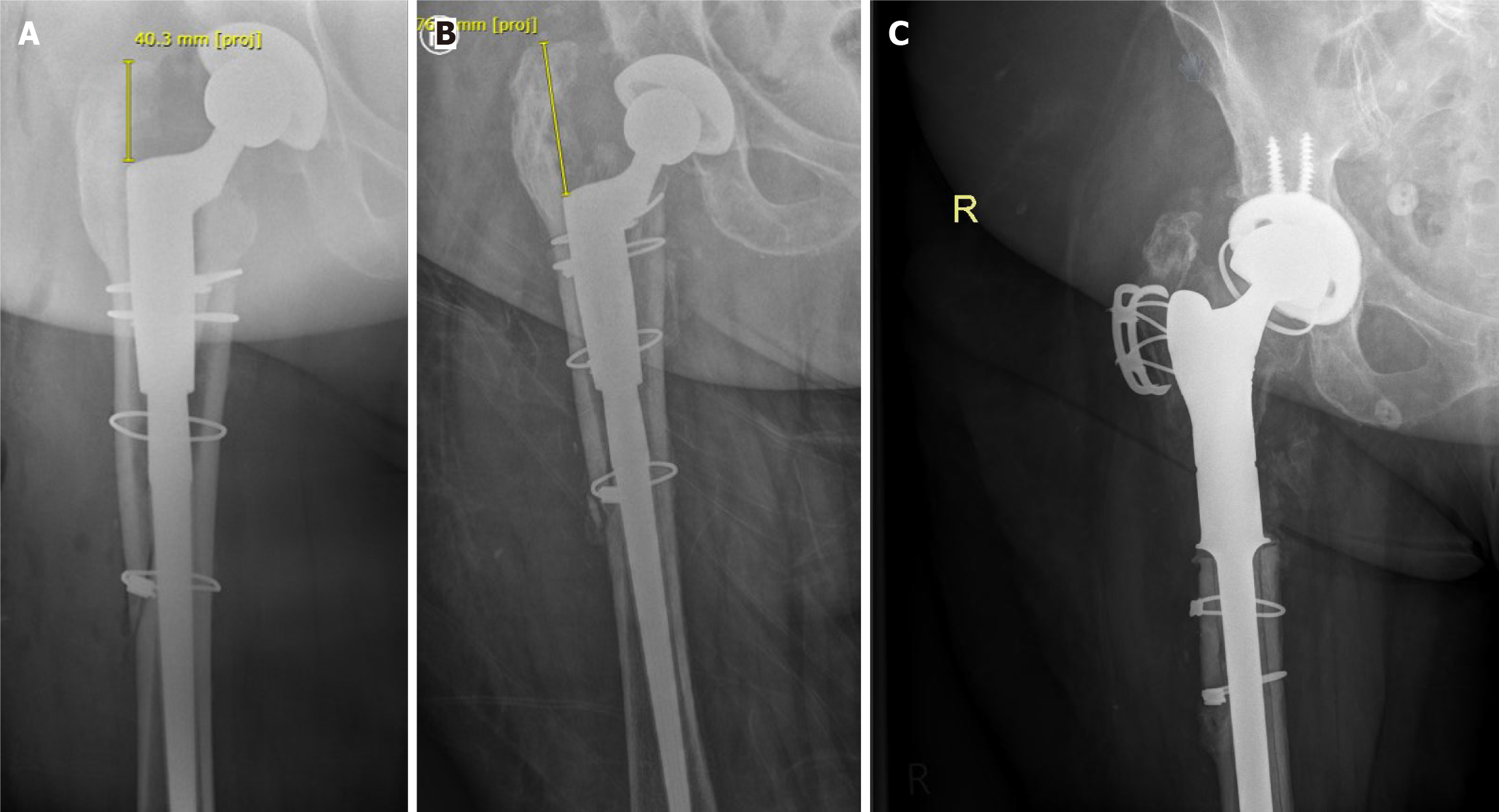
Figure 1 Subsidence of a loose femoral component in a revision total hip arthroplasty.
The above case showcases the utilisation of plain radiography in the diagnosis of aseptic loosening. This patient had presented to the outpatient’s clinic 1 year following revision total hip arthroplasty with complaints of right sided hip pain that was gradually worsening. The revision surgery utilised a diaphyseal bearing modular revision system with cerclage cables for closure of the proximal femoral osteotomy as a result of periprosthetic fracture. A–C: Immediate postoperative (A) and 1-year postoperative (B) plain radiographs are displayed with significant subsidence of the femoral component noted in the follow-up appointment. Following careful clinical evaluation and confirmation of normal biochemical markers, the patient was diagnosed with aseptic loosening and underwent a planned revision total hip arthroplasty with a proximal femoral replacement (C).
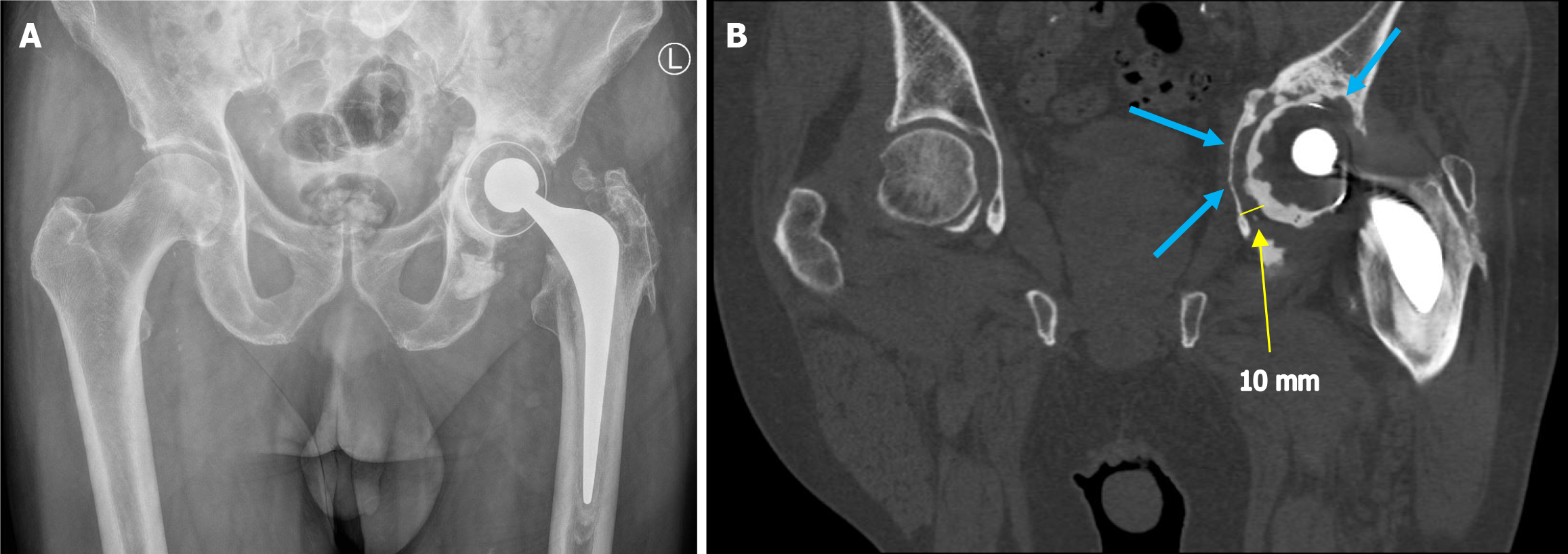
Figure 2 Computed tomography scan of loose cemented acetabular component with comparison plain radiographs.
This case displays the utility of computed tomography (CT) with metal artefact reduction in diagnosing periprosthetic loosening. The gentleman in this case was referred to the outpatient’s clinic by his family physician with complaints of gradually worsening pain and discomfort in the left hip. The patient’s blood markers were normal at the time of referral and examination findings were equivocal. A and B: Acetabular loosening in a cemented total hip arthroplasty was confirmed on initial plain radiography of the pelvis (A). However, characterisation with CT was required in this case to determine the extent of loosening and appropriately plan revision surgery (B). Both images were acquired on the same day. Although acetabular loosening is visible in Figure 2A around DeLee Charnley Zones 1 & 2, the extent of loosening and bony erosion is far clearer in Figure 2B (blue arrows). An approximate 10 mm rim of lucency was demonstrated on the CT scan which was not easily appreciated on the initial plain radiographs (yellow arrow). The patient proceeded to a successful revision hip arthroplasty following review of the CT images.
Figure 3 Triple phase bone scintigraphy and magnetic resonance imaging demonstrating loose femoral component.
The above case displays the importance of planar bone scintigraphy and magnetic resonance imaging (MRI) with multi-acquisition variable resonance image combination selective sequencing in the diagnosis of periprosthetic loosening. The patient in this case had presented 4 years following bilateral primary total hip replacements with discomfort in the right hip only. A and B: Initial plain radiographs were unremarkable, therefore higher order imaging in the form of planar bone scintigraphy (A) and MRI (B) were acquired. Marked increased uptake of the technetium-99m MDP radiotracer in the region of the right greater trochanter and shoulder of the femoral component was noted (yellow arrows). Physical examination findings of a soft tissue mass and raised inflammatory markers prompted the acquisition of MRI for further characterisation. MRI findings of a soft tissue collection (blue arrows) led to the diagnosis of septic loosening in this patient. This was later confirmed intraoperatively during revision surgery.
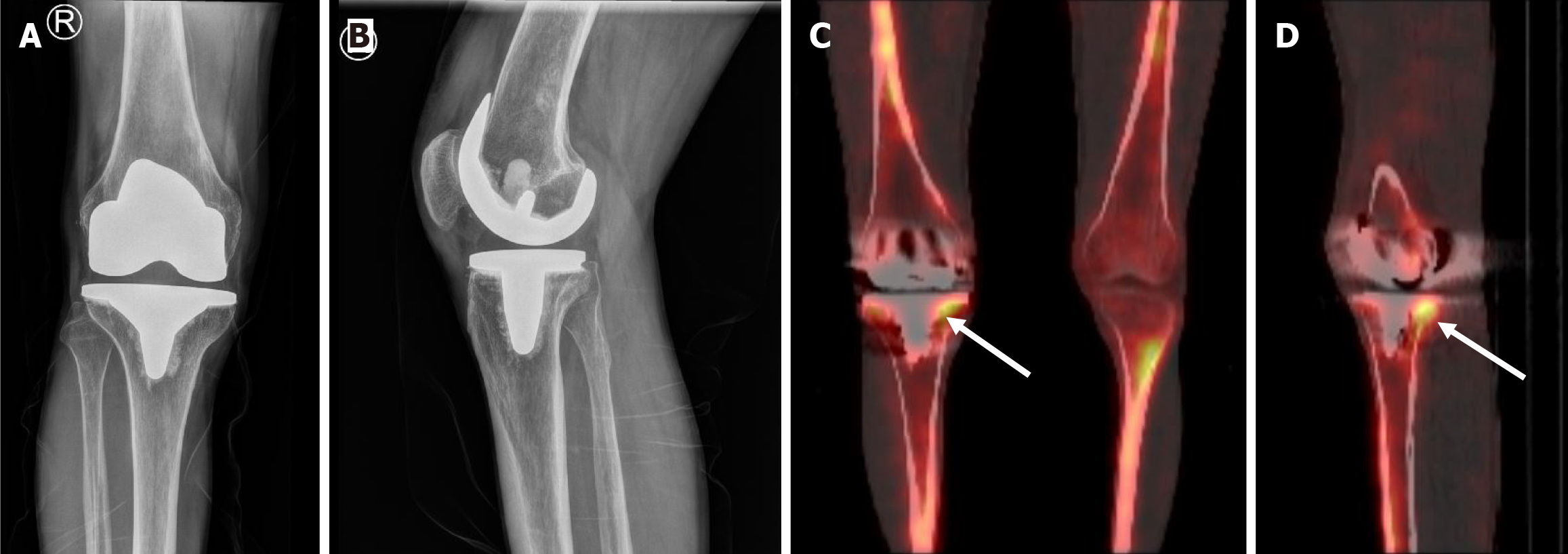
Figure 4 Plain radiographs and corresponding single-photon emission computed tomography/computed tomography of tibial component loosening.
A–D: This is a recent case within our institution demonstrating the capability of single-photon emission computed tomography (SPECT)/computed tomography (CT) in diagnosing periprosthetic loosening. Initially, anteroposterior (A) and lateral (B) radiographs were performed to investigate the cause of right sided knee pain 8 years after cemented primary total knee replacement. The radiographs did not display typical signs of loosening or other abnormalities that could explain the patient’s symptoms. In addition, inflammatory markers were normal and clinical examination was unremarkable. Aseptic loosening was suspected and advanced imaging in the form of SPECT/CT was acquired. Coronal (C) and sagittal (D) SPECT/CT images demonstrate increased radiotracer uptake along the inferior aspect of the tibial base plate both medially and laterally but particularly posteromedially (white arrows). On the basis of the SPECT/CT image findings in conjunction with the clinical history, exam and blood markers, a diagnosis of aseptic loosening was made. The patient opted to undergo a revision total knee replacement at an alternative private institution.
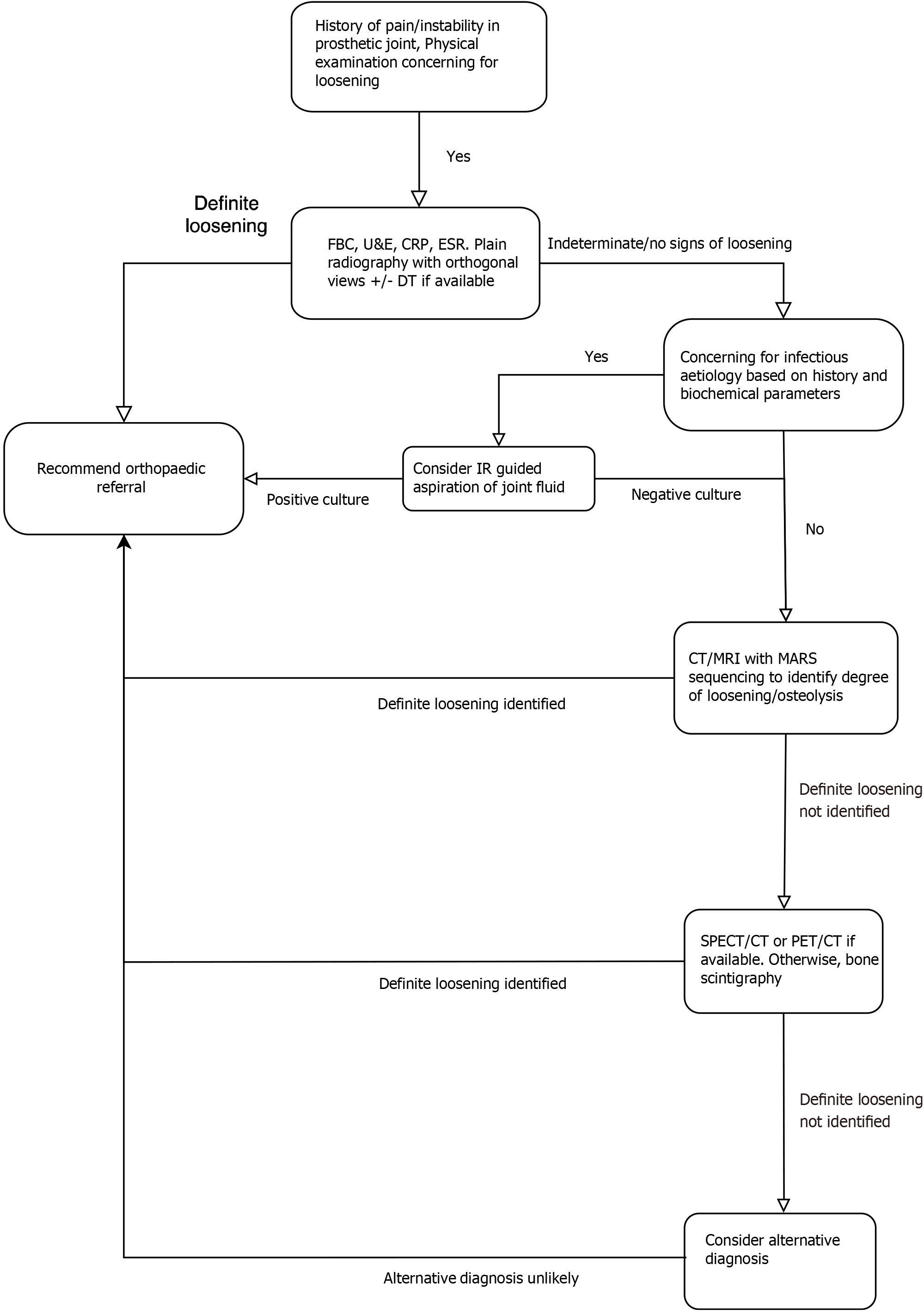
Figure 5 Summary flow diagram of recommended radiological diagnostic pathway.
The flow diagram above aims to aid the general radiologist in the diagnosis of suspected periprosthetic loosening. As with any most pathologies, the pathway begins with careful history taking and physical examination by the referring clinician. Baseline biochemical markers and plain radiography ± digital tomosynthesis form the first step in the diagnostic pathway. The recommended further steps are based on the results of the initial step and are listed above. Discussion with the clinician who is the primary carer for the patient is crucial in every step of the pathway. FBC: Full blood count; U&E: Urea and electrolytes; CRP: C reactive protein; ESR: Erythrocyte sedimentation rate; IR: Interventional radiology; DT: Digital tomosynthesis; CT: Computed tomography; MRI: Magnetic resonance imaging; MARS: Metal artefact reduction sequence; SPECT: Single-photon emission computed tomography; PET: Positron emission tomography.
- Citation: Shet SS, Kakish E, Murphy SC, Roopnarinesingh R, Power SP, Maher MM, Ryan DJ. Imaging evaluation of periprosthetic loosening: A primer for the general radiologist. World J Radiol 2025; 17(2): 102373
- URL: https://www.wjgnet.com/1949-8470/full/v17/i2/102373.htm
- DOI: https://dx.doi.org/10.4329/wjr.v17.i2.102373