Copyright
©The Author(s) 2024.
World J Radiol. Aug 28, 2024; 16(8): 337-347
Published online Aug 28, 2024. doi: 10.4329/wjr.v16.i8.337
Published online Aug 28, 2024. doi: 10.4329/wjr.v16.i8.337
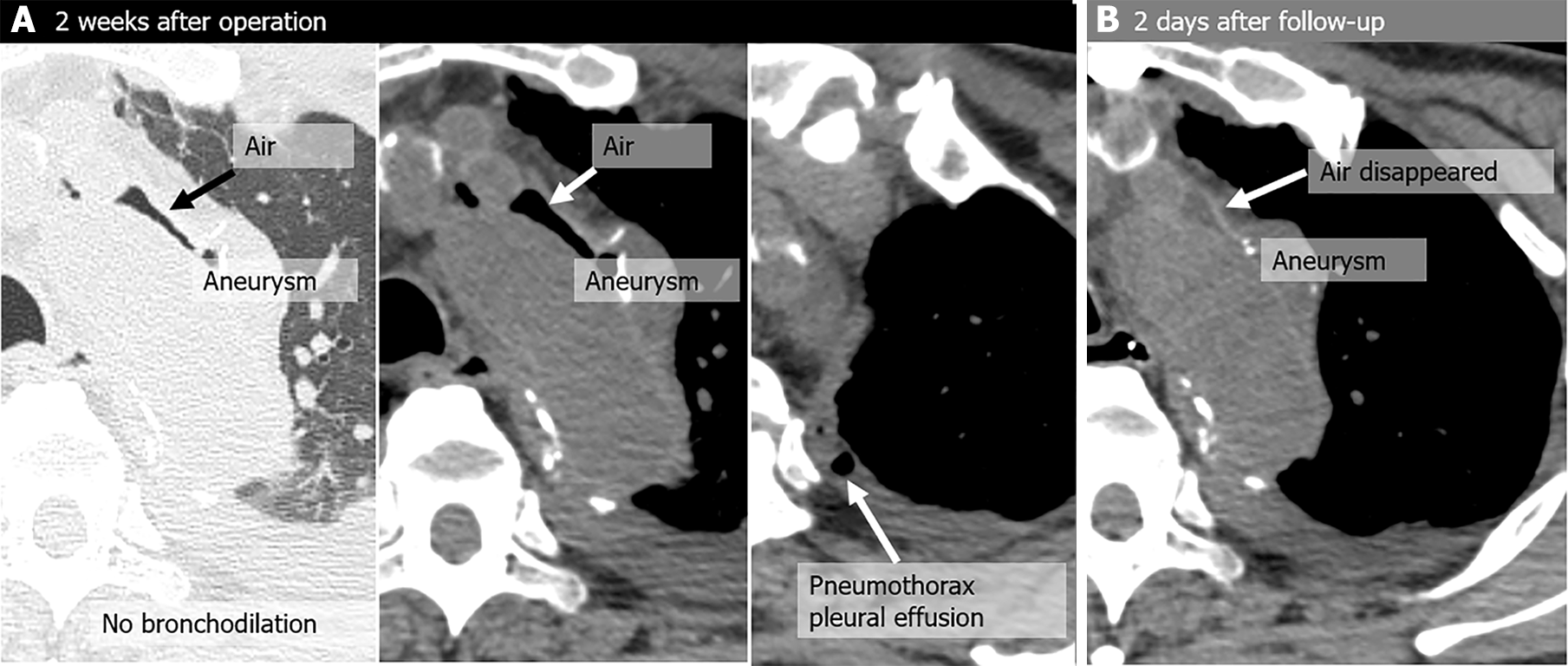
Figure 1 Pseudo-aortobronchial fistula in a 75-year-old man with dyspnea, a history of aortic arch replacement 2 weeks earlier for an aneurysm, and positive pressure ventilation performed for acute respiratory distress syndrome.
A: Two weeks after the operation, he underwent computed tomography (CT) because of dyspnea, and peri-graft air was noted (not seen immediately after the operation); B: The air disappeared on a CT scan performed 2 days later. There was no recurrence of air around the graft on imaging performed over a 6-year period, and no signs of graft infection.
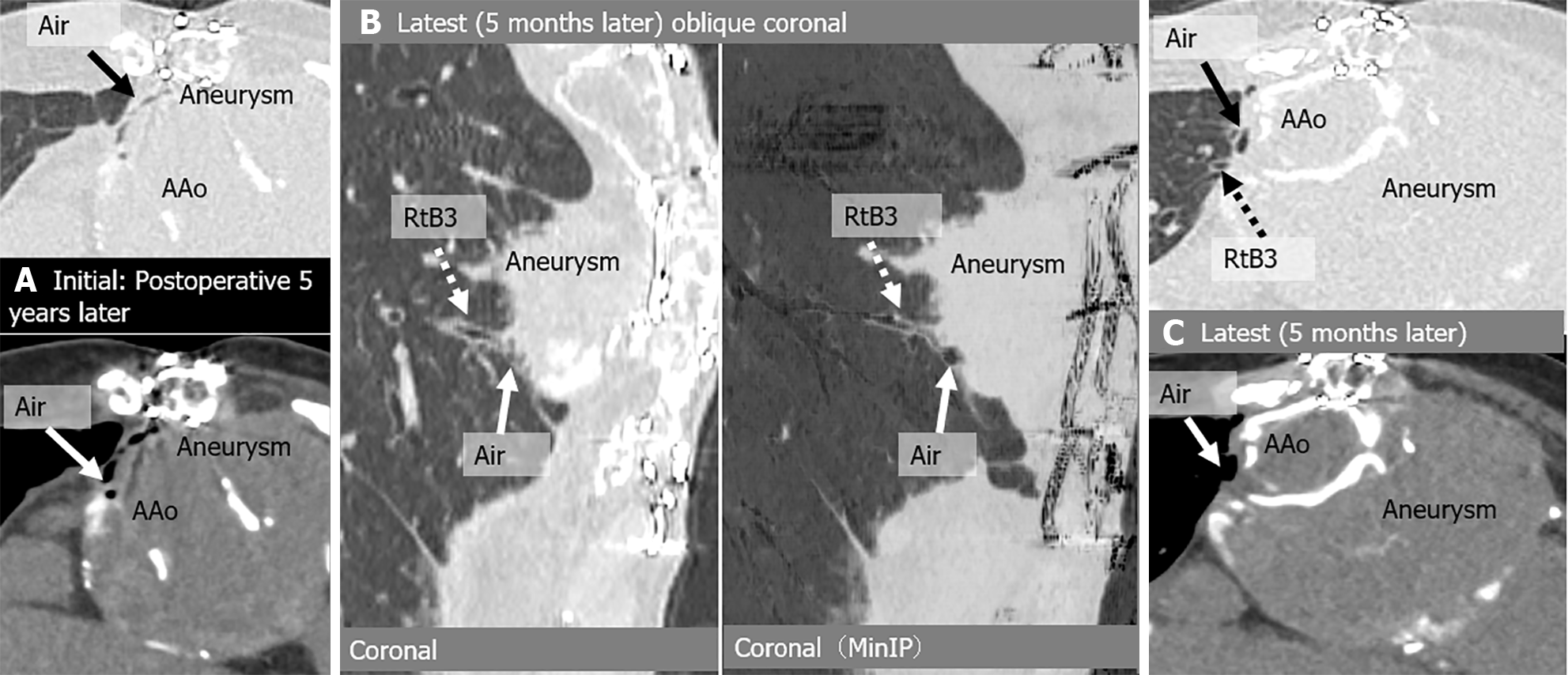
Figure 2 Aortobronchial fistula in an asymptomatic 73-year-old woman with a history of ascending aorta and aortic arch replacement + thoracic endovascular aortic repair 5 years earlier for dissection.
A: Initial computed tomography (CT) images show air shadow in the intra-aortic peri-graft space (arrow); B: Latest CT, 5 months follow-up images show dilated peripheral bronchus (right B3) communicating with peri-graft air(arrow); C: Latest CT, 5-month follow-up images show residual peri-graft air. There were no severe complications during the 5-month observation period. AAo: Ascending aorta; Rt: Right; MinIP: Minimum intensity projection.
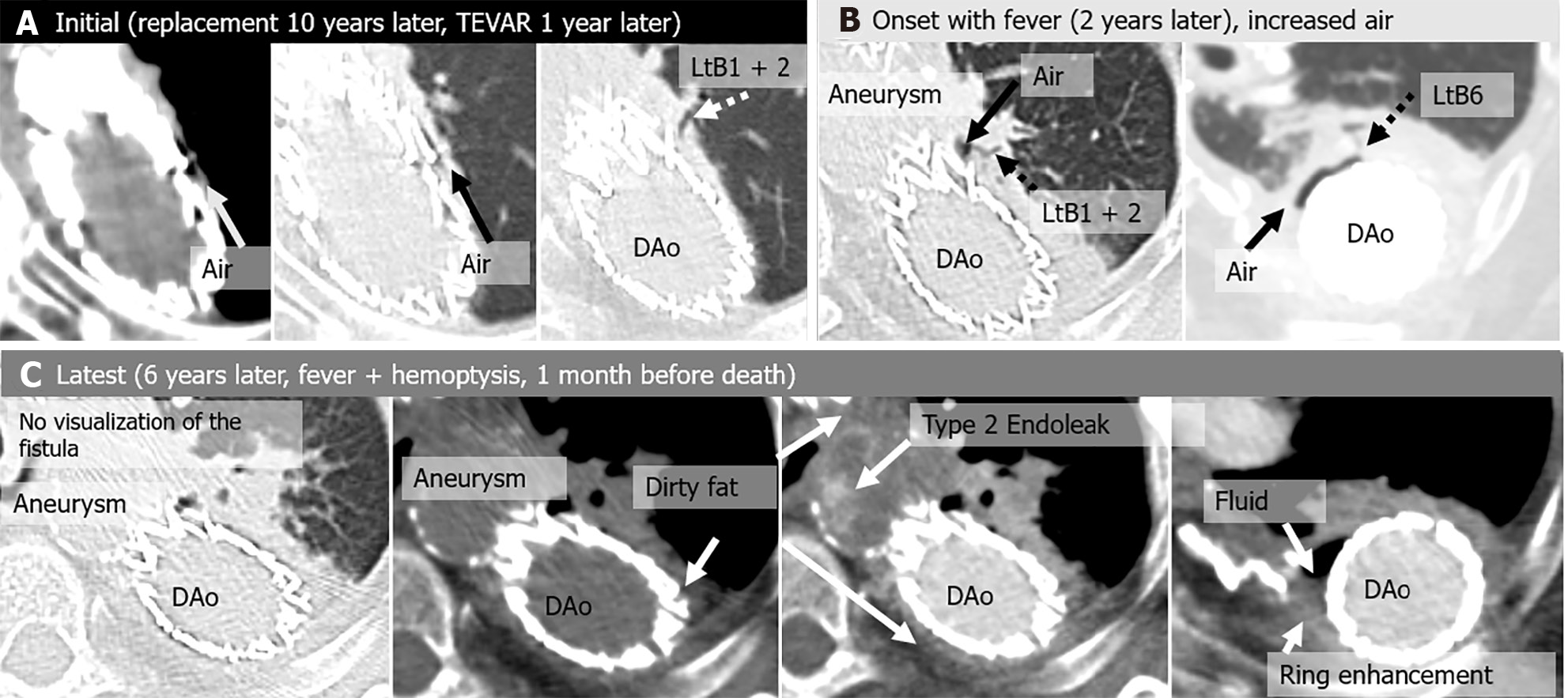
Figure 3 Aortobronchial fistula in an asymptomatic 74-year-old woman, a history of thoracic endovascular aortic repair 1 year earlier for a pseudoaneurysm after replacement of a descending aorta 10 years earlier.
Two years after the initial computed tomography (CT) scan, the patient developed fever and was diagnosed with a stent graft infection. Drainage of the peri-graft abscess was performed, and the infection was controlled, but the infection recurred repeatedly and was complicated by a Type 2 endoleak. At the latest CT scan, the patient had hemoptysis and fever. The patient died from massive hemoptysis 6 years after the initial CT. A: Initial CT images show air shadow in the intra-aortic peri-graft space (arrow) and dilated peripheral bronchi (left B1 + 2) communicating with peri-graft air (arrow); B: Onset CT, 2 years after the initial CT images show dilated peripheral bronchi (left B1 + 2 and B6) communicating with peri-graft air (arrow); C: Latest CT images show peri-graft dirty fat sign and disappearance of direct communication between peripheral bronchi and peri-graft air. CT angiogram demonstrates extravasation of contrast material into the native aneurysm, representing a Type 2 endoleak. Peri-graft fluid collection and ring enhancement are also seen. DAo: Descending aorta; TEVAR: Thoracic endovascular aortic repair; Lt: Left.
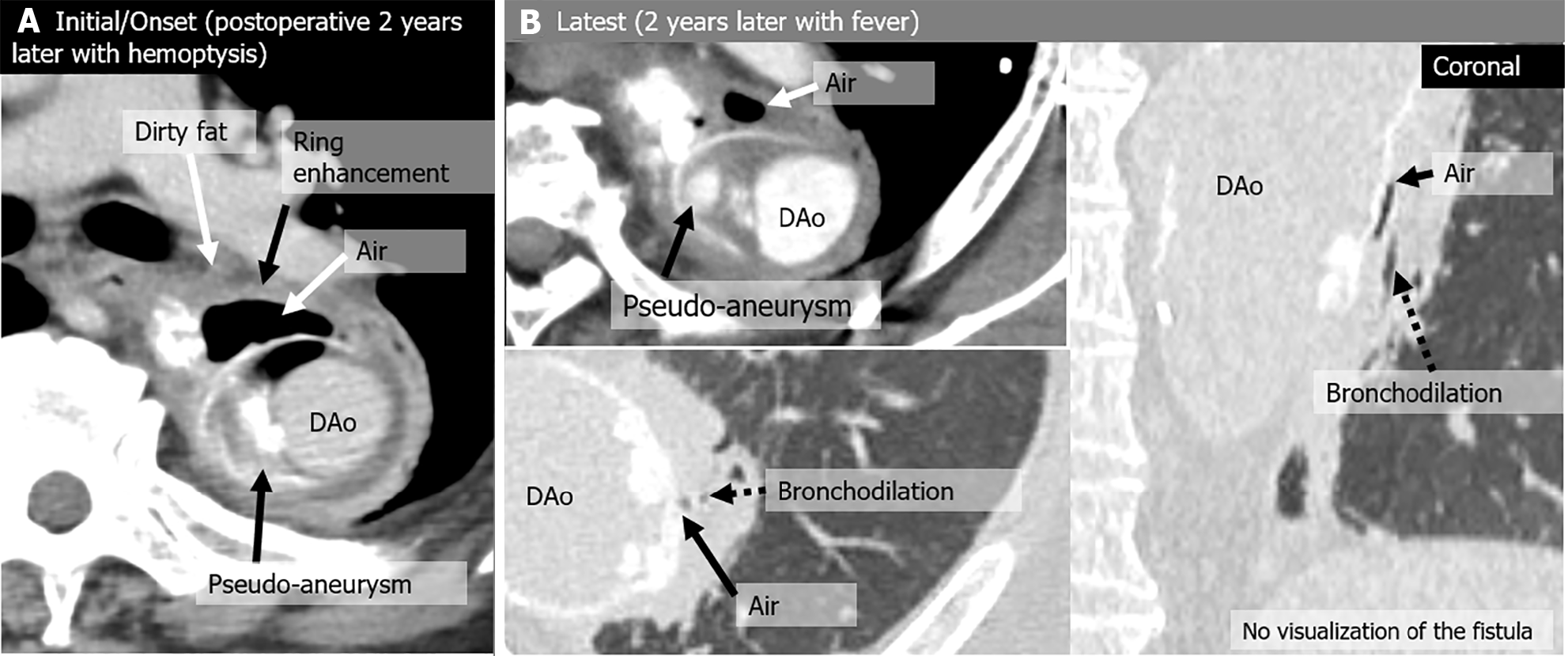
Figure 4 Aortobronchial fistula in a 67-year-old man with mild hemoptysis and a history of replacement of the descending aorta 26 years earlier for aortic coarctation and aneurysm.
Although the hemoptysis spontaneously resolved, a graft infection developed 2 years after the initial computed tomography (CT), which was treated with antibiotics. No invasive treatment was performed at the patient’s request. A: Initial/onset CT image shows air shadow in the intra-aortic peri-graft space (arrow) and a pseudo-aneurysm (arrow). A peri-graft dirty fat sign and ring enhancement are also seen; B: Latest CT, 2-year follow-up scan images show residual peri-graft air and a dilated peripheral bronchus near the graft without direct connection to peri-graft air.
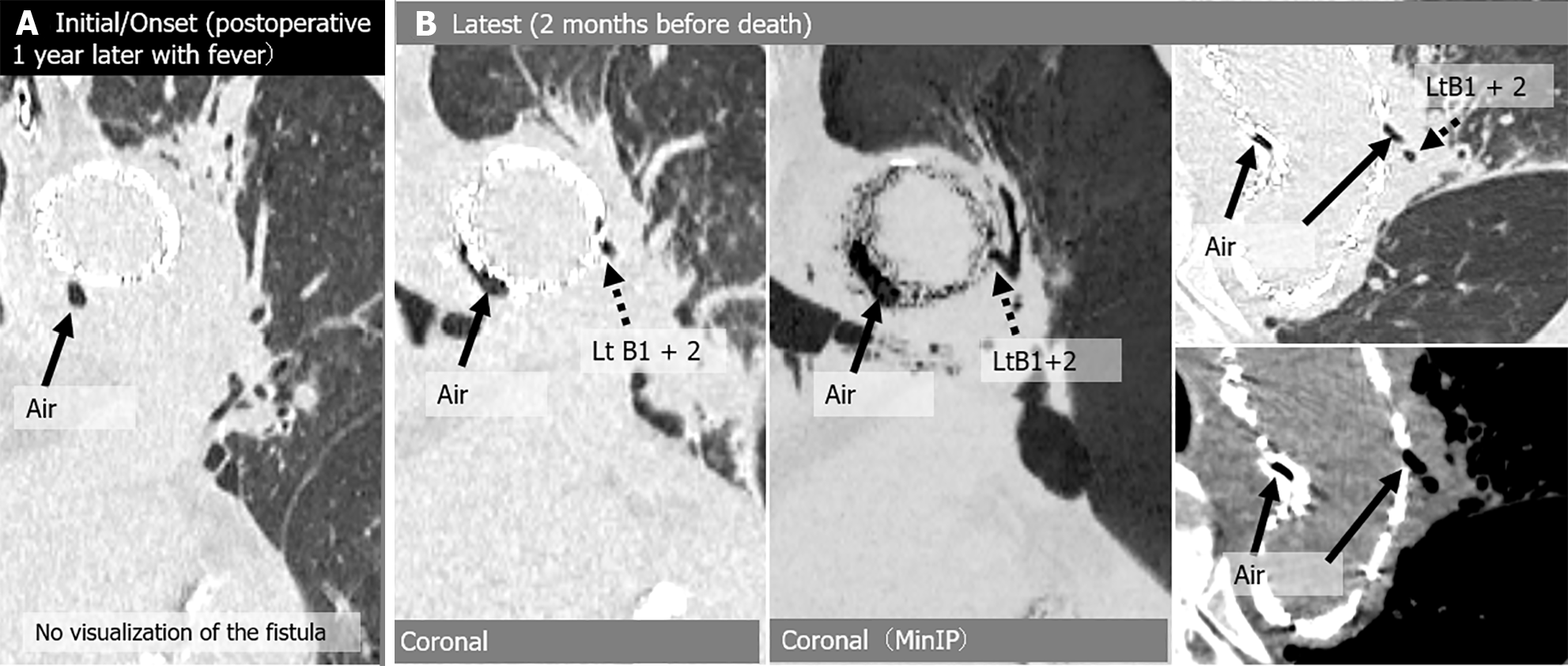
Figure 5 Aortobronchial fistula in a 73-year-old man with fever and a history of thoracic endovascular aortic repair 1 year earlier for infected aneurysm.
One year after the surgery, peri-graft air was first noted when he was diagnosed with a stent graft infection. He was treated with antibiotics, and the infection was brought under control, but a year later the stent graft infection recurred and he died of sepsis. A: Initial/onset computed tomography (CT) images show air shadow in the intra-aortic peri-graft space (arrow), but without direct connection between bronchioles and perigraft air; B: Latest CT images show increased peri-graft air (arrow) and dilated peripheral bronchi (left B1 + 2) communicating with air (arrow). Lt: Left; MinIP: Minimum intensity projection.
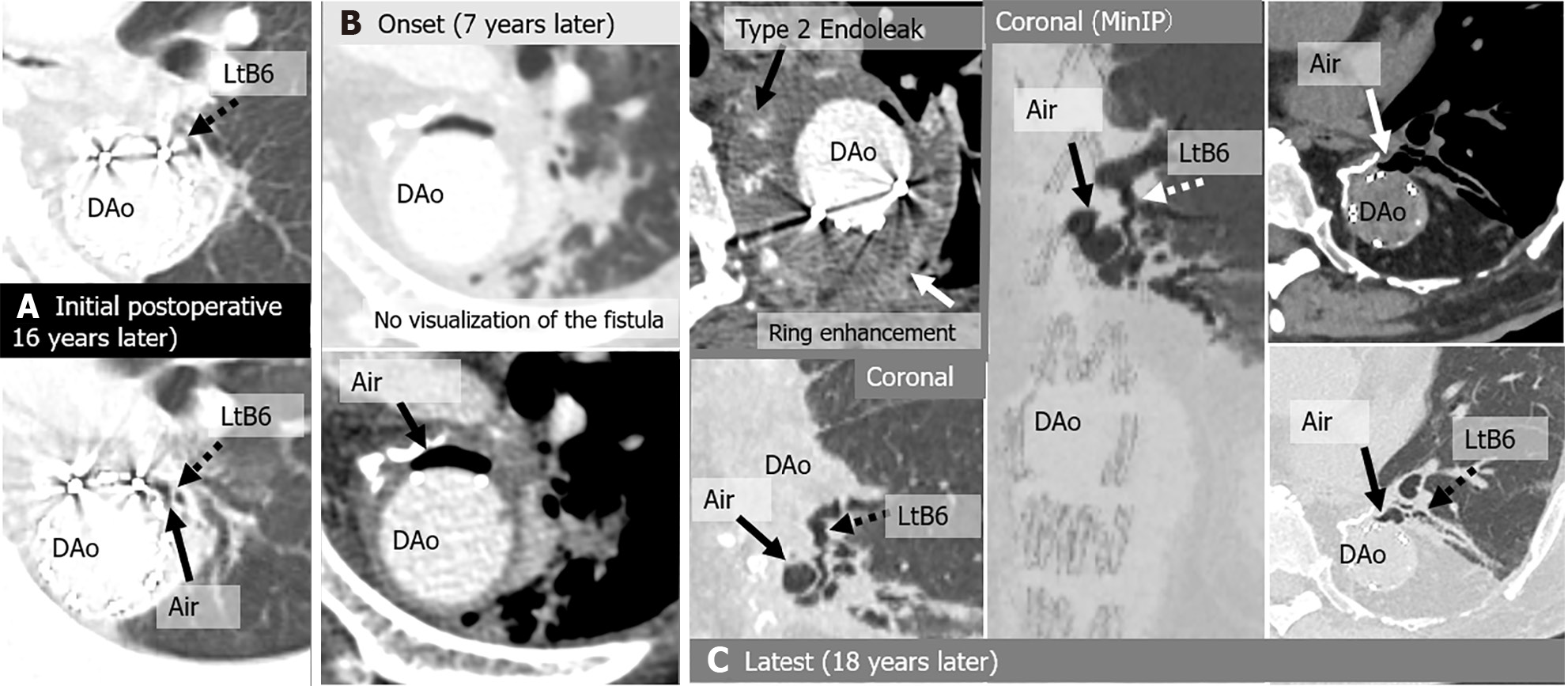
Figure 6 Aortobronchial fistula in a 57-year-old asymptomatic man, a history of bronchioles 3 years earlier for a pseudoaneurysm after thoracoabdominal aorta replacement 16 years earlier for an aneurysm.
Seven years after the first detection of peri-graft air, he developed fever and hemoptysis due to graft infection and a type 2 endoleak, and underwent aortic-arch-to-descending-aorta replacement, bronchopulmonary artery fistula closure, and intrathoracic omental repair. Ten years after the reoperation, the patient developed a pseudoaneurysm and underwent thoracic endovascular aortic repair (TEVAR). A: Initial computed tomography (CT) images show air shadow in the intra-aortic peri-graft space (arrow) and dilated peripheral bronchus (left B6) communicating with peri-graft air (arrow); B: Onset CT, 7 years after the initial CT images show increased peri-graft air (arrow), but there is no direct connection between bronchioles and peri-graft air. Axial enhanced CT demonstrates a Type 2 endoleak and ring enhancement; C: Latest CT, 18-year follow-up after initial CT images show residual peri-graft air and dilated peripheral bronchus (left B6) communicating with peri-graft air (arrow). No complications occurred during the follow-up period of 1.5 years after TEVAR for a pseudoaneurysm. DAo: Descending aorta; Lt: Left; MinIP: Minimum intensity projection.
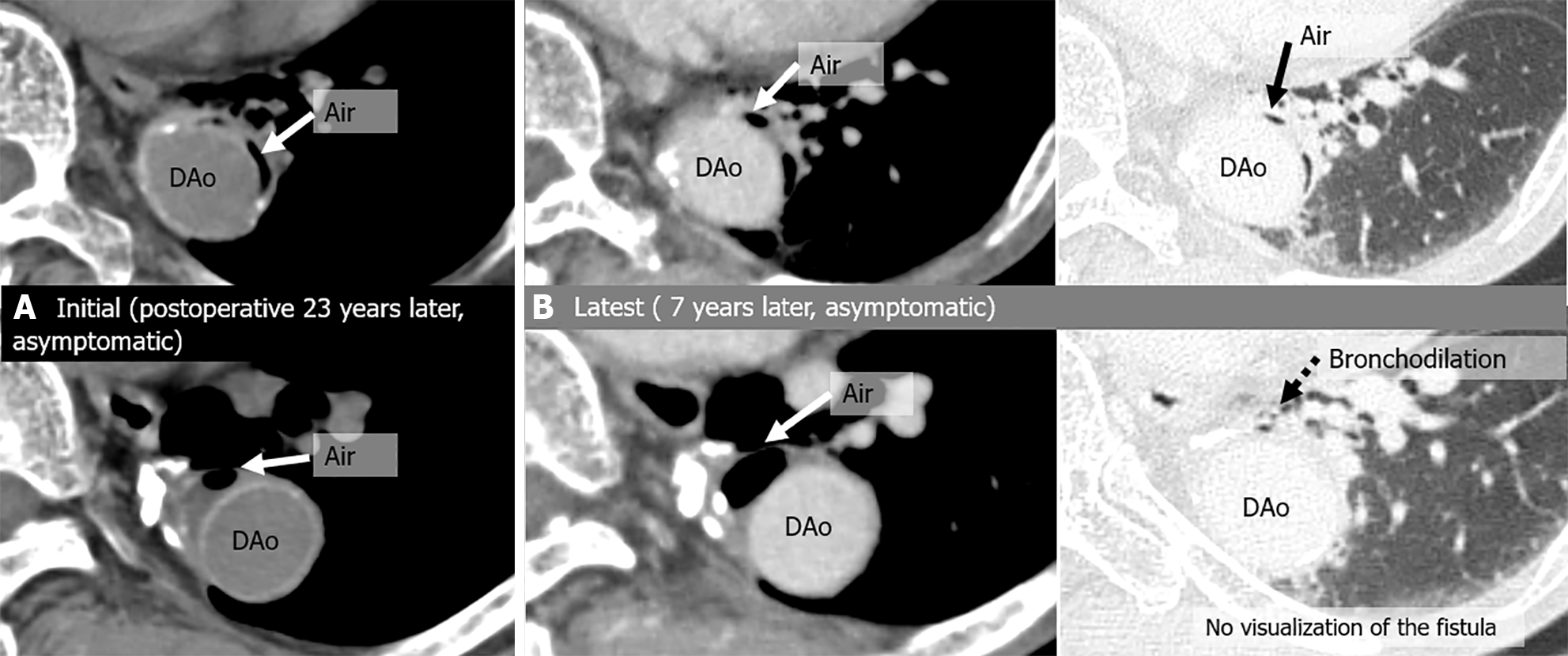
Figure 7 Aortobronchial fistula in an 83-year-old asymptomatic man and a history of descending aorta replacement 23 years earlier for an aneurysm.
A: Initial computed tomography (CT) images show air shadow in the intra-aortic peri-graft space (arrow); B: Latest CT, 7-year follow-up images show residual peri-graft air. A dilated peripheral bronchus is near the graft, but without direct connection with peri-graft air. No severe complications occurred during the 7-year observation period. DAo: Descending aorta.
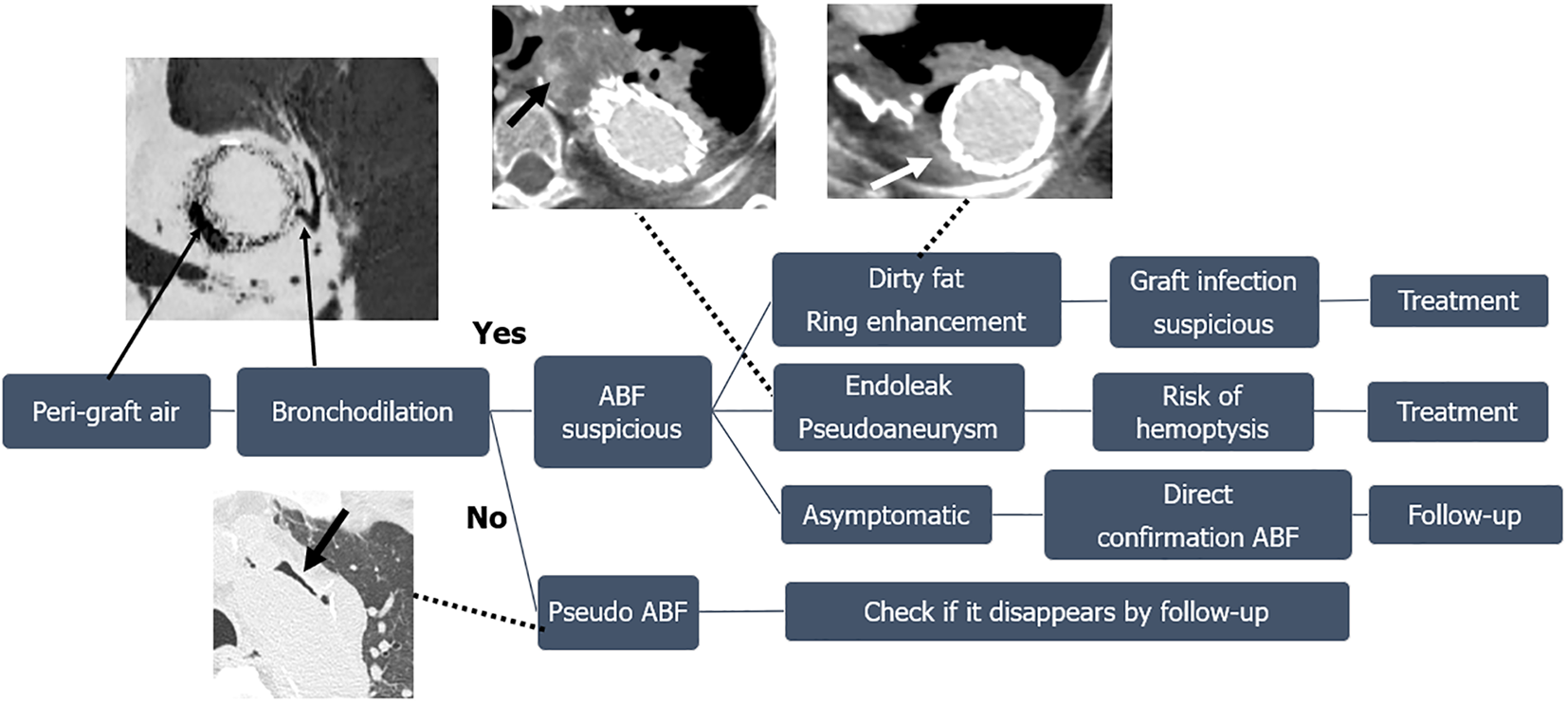
Figure 8 Diagnostic steps to treatment of peri-graft air after thoracic aorta procedure.
When peri-graft air is observed, first check for surrounding bronchiectasis, and if there is no dilated bronchiole, it may not be true aortobronchial fistula (ABF). If there is a dilated bronchiole, ABF is suspected. If the dirty fat sign or ring enhancement around peri-graft air are observed, graft infection is strongly suspected and treatment is required. Next, check for endoleaks and pseudoaneurysms, and if any are found, there is a risk of hemoptysis, so aggressive treatment should be considered. If the patient does not have any of the described findings, is asymptomatic, and persistence of the ABF can be confirmed, follow-up observation is possible. ABF: Aortobronchial fistula.
- Citation: Tsuchiya N, Inafuku H, Yogi S, Iraha Y, Iida G, Ando M, Nagano T, Higa S, Maeda T, Kise Y, Furukawa K, Yonemoto K, Nishie A. Direct visualization of postoperative aortobronchial fistula on computed tomography. World J Radiol 2024; 16(8): 337-347
- URL: https://www.wjgnet.com/1949-8470/full/v16/i8/337.htm
- DOI: https://dx.doi.org/10.4329/wjr.v16.i8.337