Copyright
©The Author(s) 2024.
World J Radiol. Aug 28, 2024; 16(8): 294-316
Published online Aug 28, 2024. doi: 10.4329/wjr.v16.i8.294
Published online Aug 28, 2024. doi: 10.4329/wjr.v16.i8.294
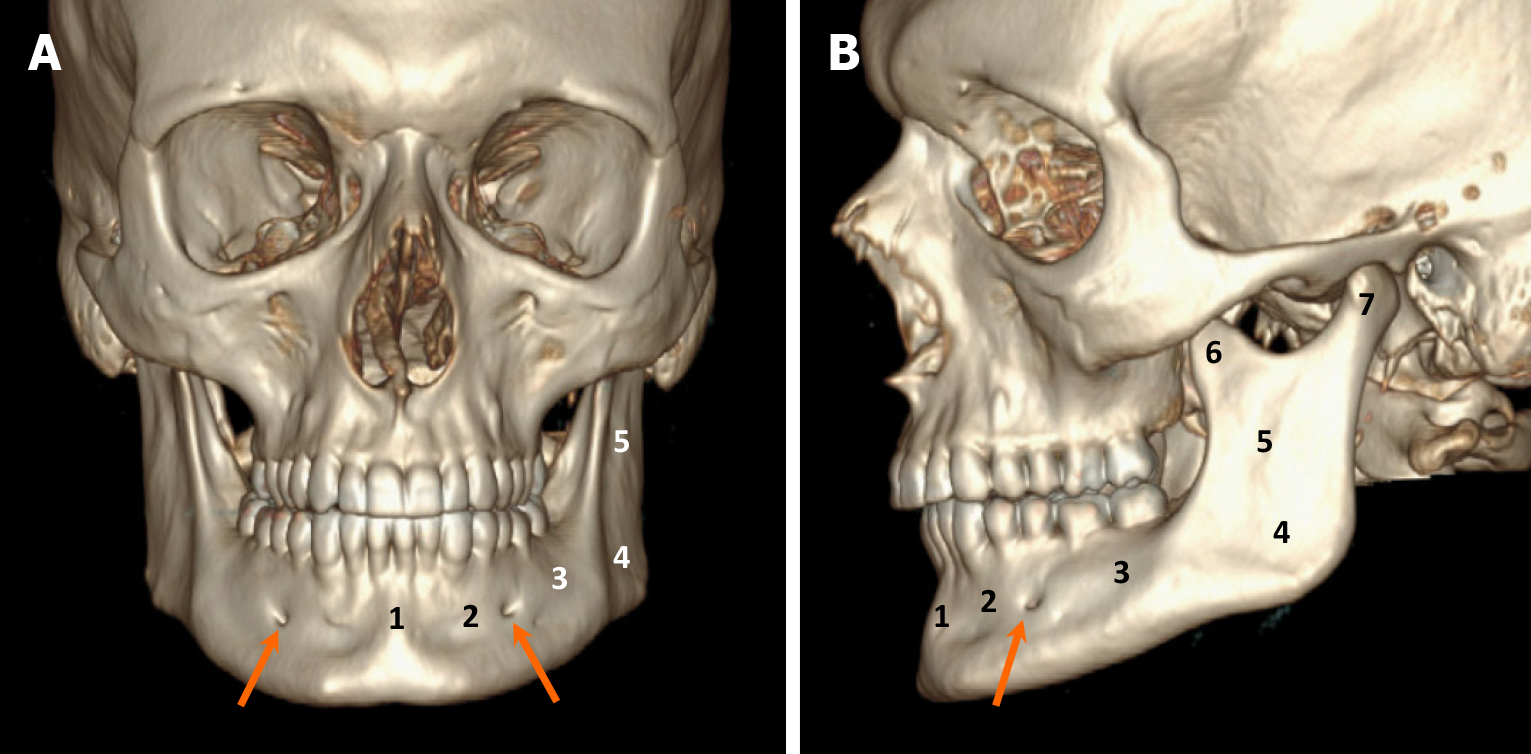
Figure 1 Anatomy of the mandible.
A and B: Computed tomography images with volume rendering reconstruction in anteroposterior (A) and lateral (B) views highlighting distinct mandibular regions: (1) Symphysis; (2) Parasymphysis; (3) Body; (4) Angle; (5) Ramus; (6) Coronoid process; and (7) Condylar process. Note the mental foramen (arrows), serving as exit points for the inferior alveolar nerves from the mandible, situated proximate to the first and second premolar teeth.
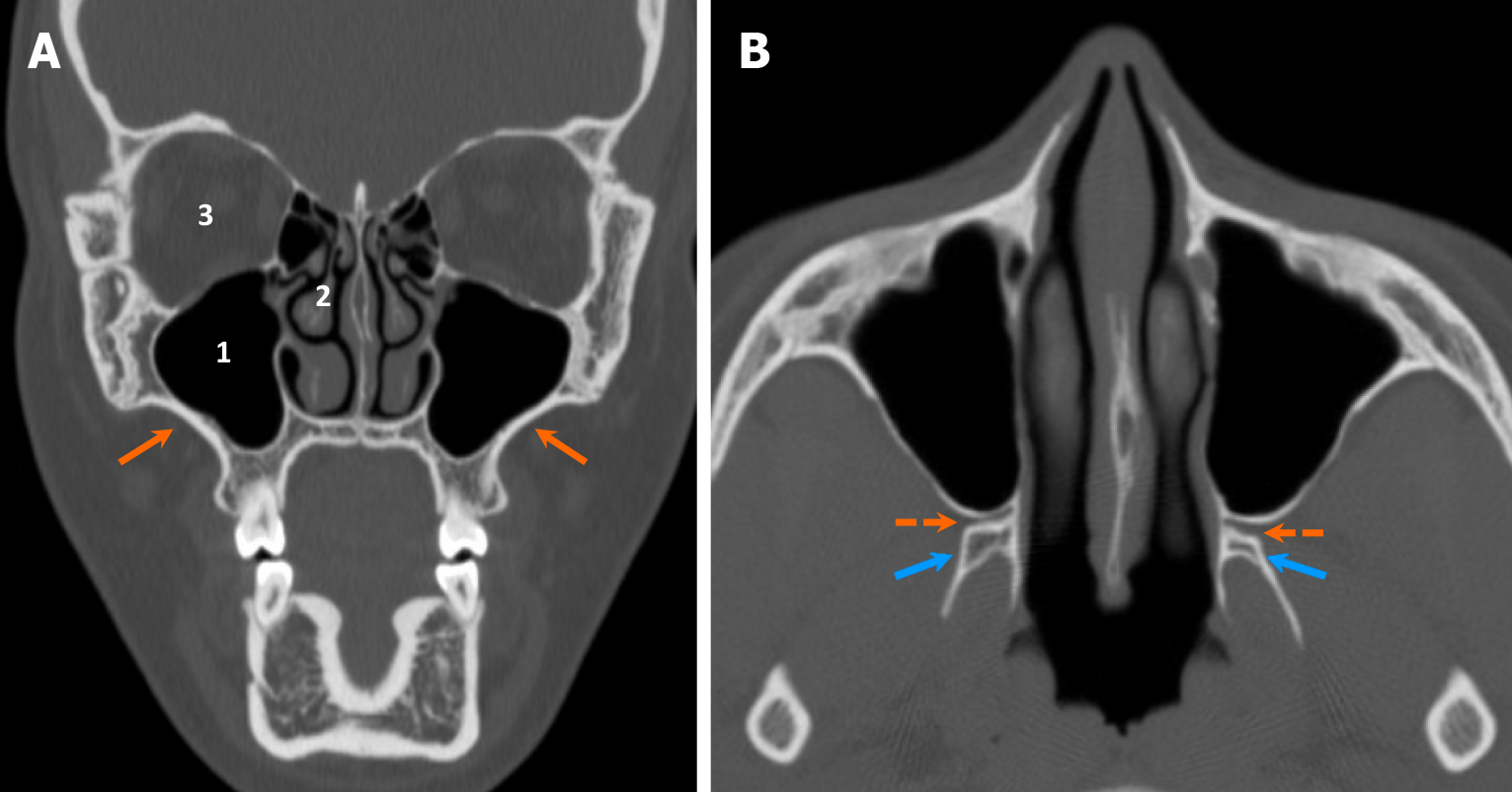
Figure 2 Anatomy of the maxilla.
A and B: Coronal (A) and axial (B) computed tomography images demonstrate the normal anatomy of the maxilla, which forms the midface (orange arrows), along with related structures: (1) Maxillary sinuses located centrally; (2) Nasal cavity located medially; and (3) Orbits located superiorly. The pterygopalatine fossae (dashed arrows) are situated between the maxillary sinuses and the pterygoid processes of the sphenoid bone (blue arrows), serving as an important location for the pterygopalatine ganglion (CN V2).
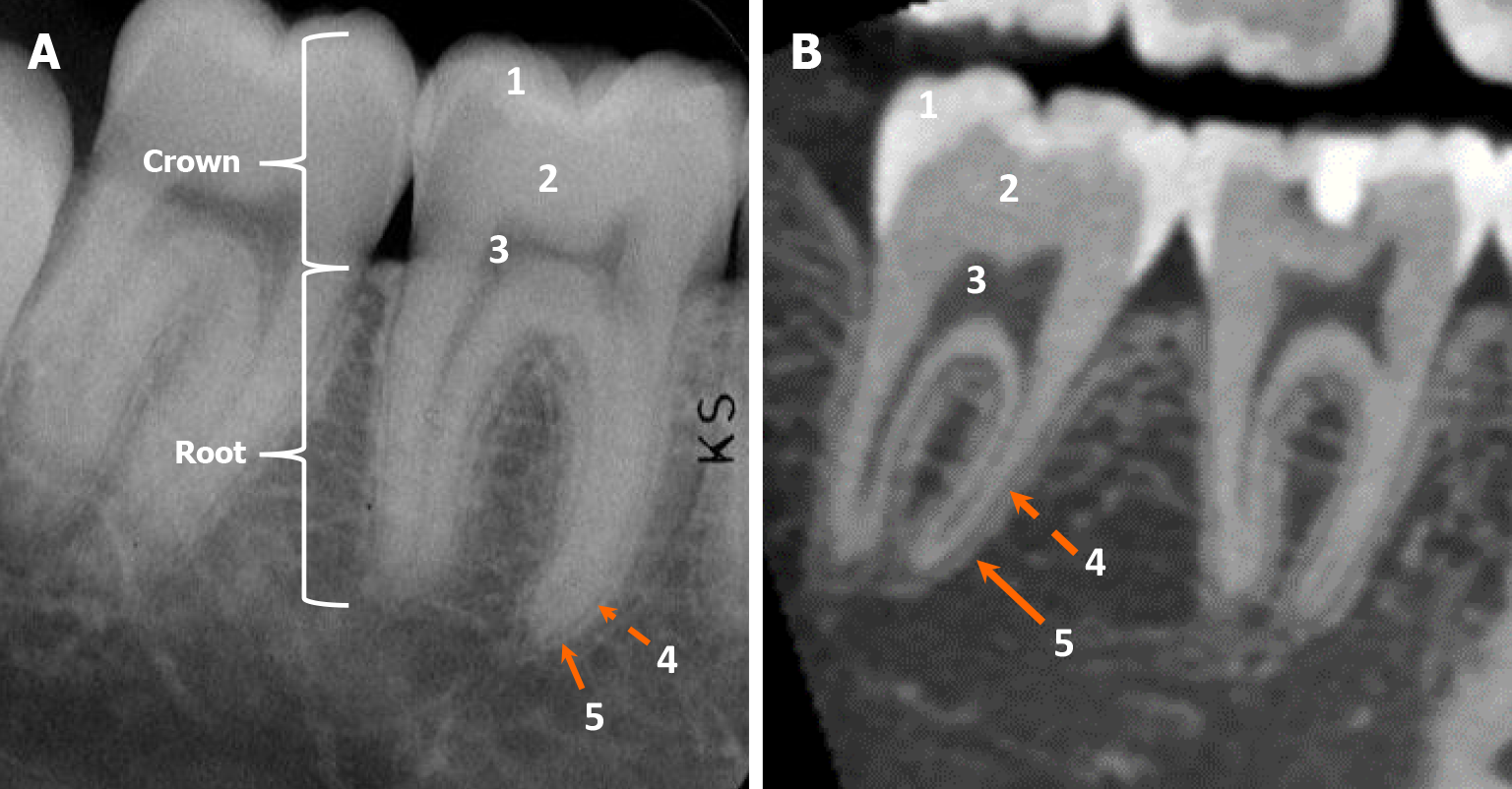
Figure 3 Dental anatomy.
A and B: The intraoral radiograph (A) and cone beam computed tomography parasagittal view (B) demonstrate normal dental anatomy with distinct anatomical features, including: (1) Enamel; (2) Dentin; (3) Pulp cavity; (4) Periodontal ligament (radiolucent line); and (5) Lamina dura (radiodense line). Radiologically, cementum appears isodense to dentin; therefore, cementum and dentin cannot be distinguished on radiographs or computed tomography.
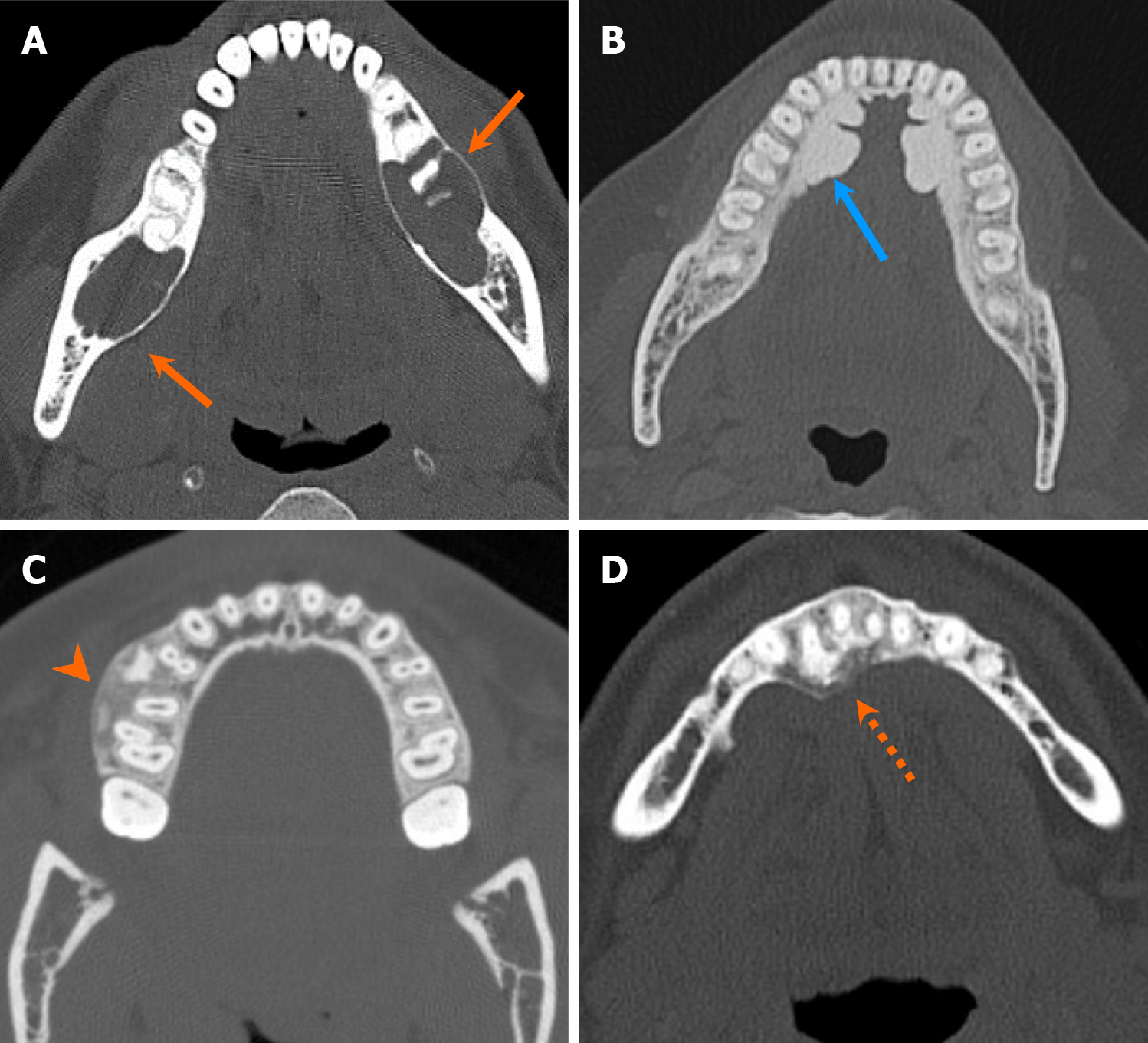
Figure 4 Radiodensity types of the jaw and maxillofacial bone lesions.
Axial computed tomography images of four cases illustrate various types of radiodensity of the jaw lesions. A: Radiolucent lesion in a patient with multiple simple bone cysts (orange arrows); B: Densely sclerotic lesion in a patient with torus mandibularis (blue arrow); C: Ground-glass density lesion in a patient with psammomatoid ossifying fibroma (arrowhead); D: Mixed lytic and sclerotic lesion in a patient with cemento-osseous dysplasia (dash arrow).
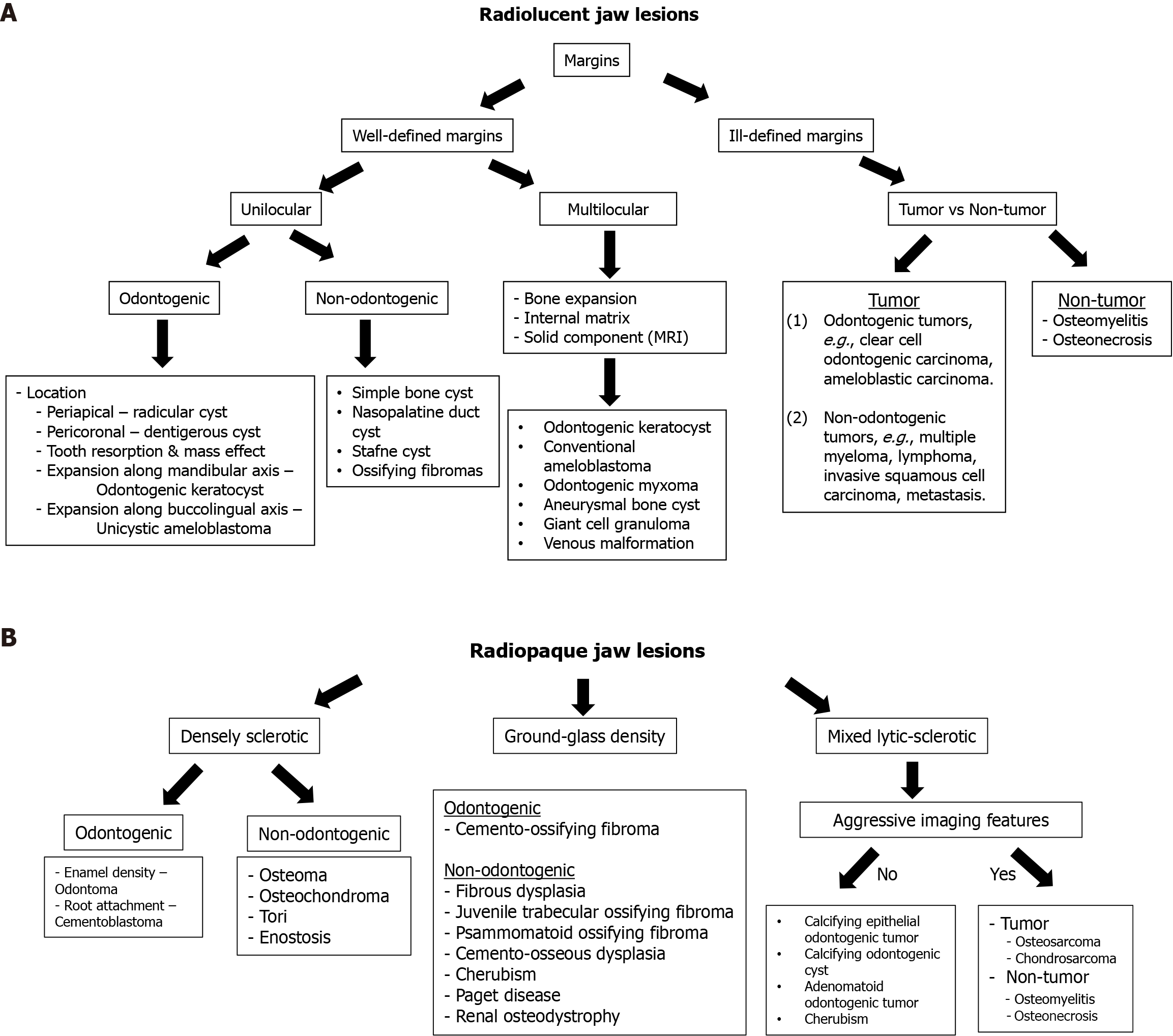
Figure 5 Imaging approach to radiolucent and radiopaque jaw lesions.
A: Imaging approach to radiolucent jaw lesions; B: Imaging approach to radiopaque jaw lesions. MRI: Magnetic resonance imaging.
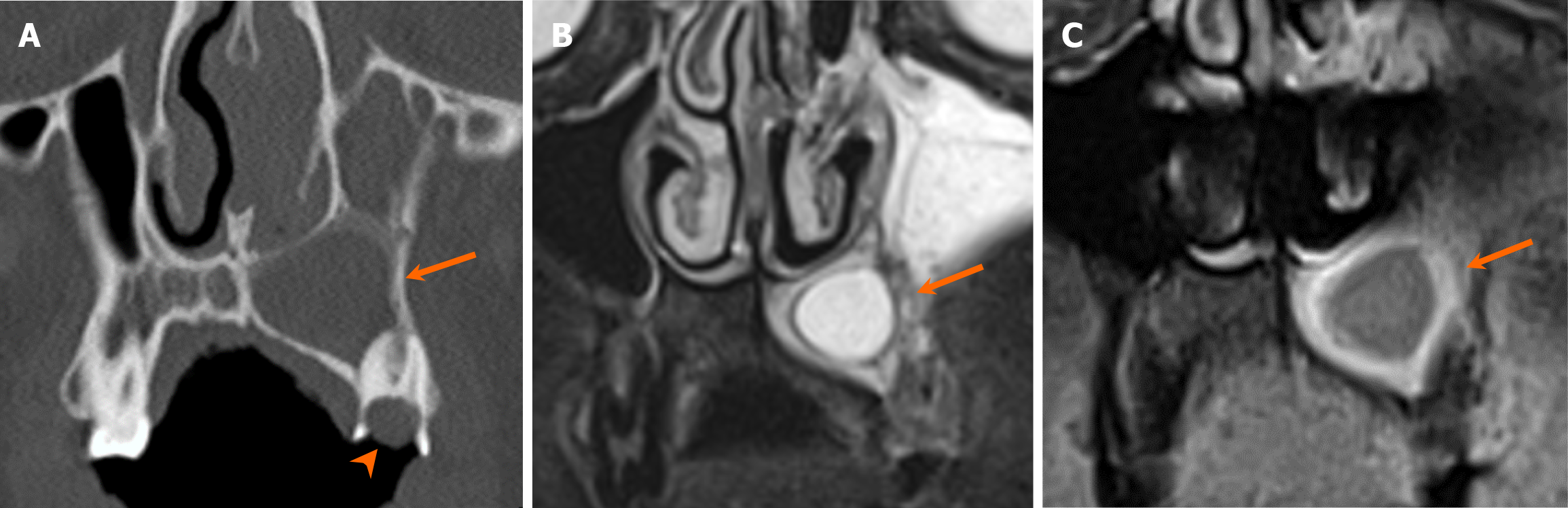
Figure 6 Radicular cyst.
A-C: Coronal computed tomography (A), T2-weighted, and contrast-enhanced T1-weighted with fat suppression (B) images reveal an unilocular expansile cystic lesion centered around the tooth apex of the left maxillary molar (arrows). The lesion demonstrates smooth rim enhancement on the contrast-enhanced T1-weighted image (arrow in C). Note large dental caries involving the crown and pulp cavity of the affected tooth (arrowhead).
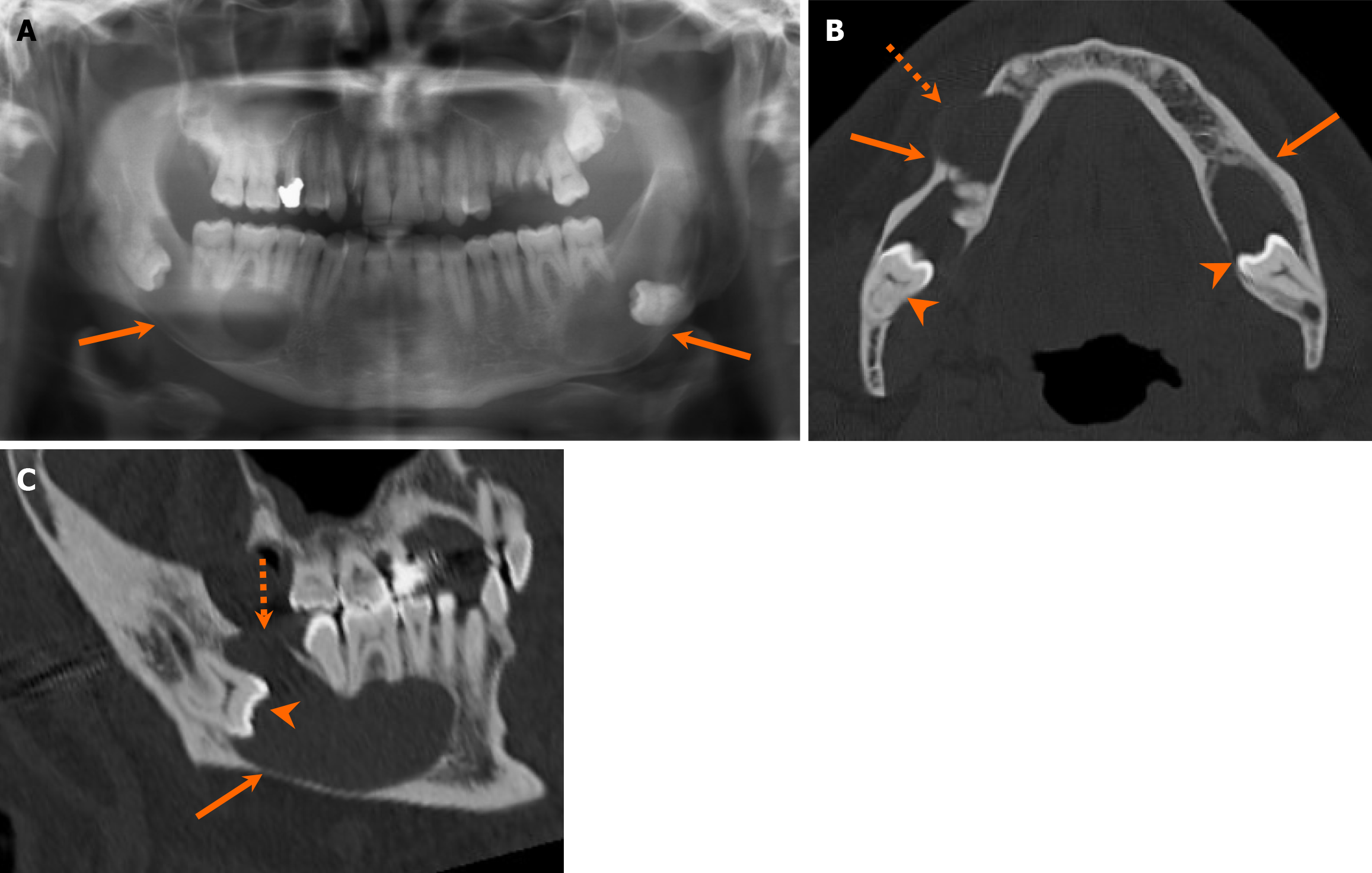
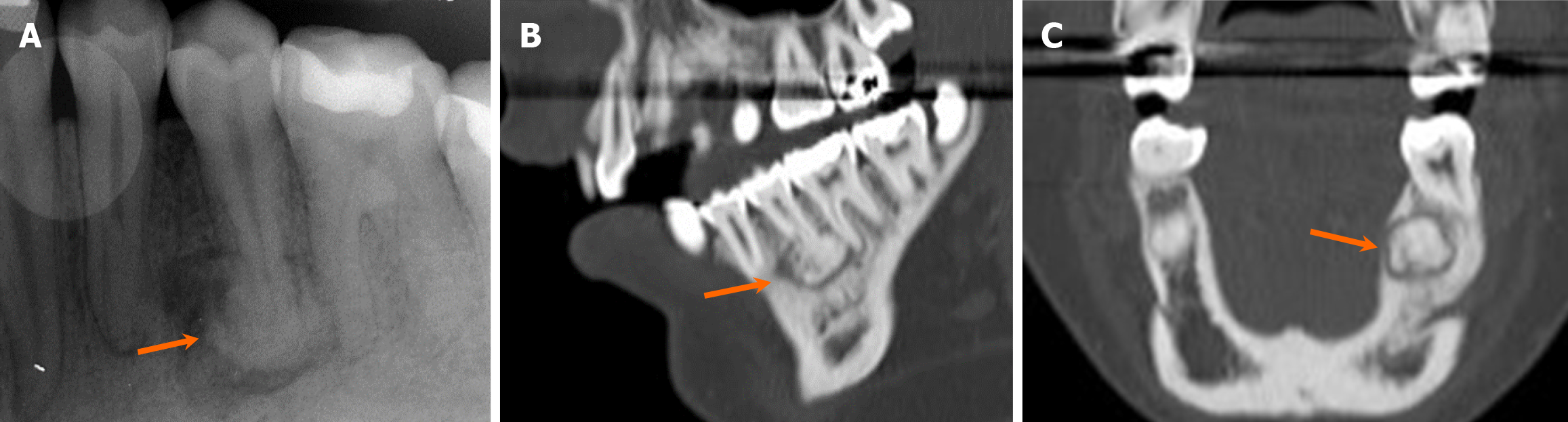
Figure 7 Dentigerous cyst.
A 51-year-old man with 6-month history of jaw swelling and liquid intermittently draining into his mouth. A-C: Orthopantomogram (A), axial (B), and sagittal (C) computed tomography images reveal large unilocular cystic lesions in the bilateral mandibular bodies (arrows) centered at the crown of unerupted molar teeth (arrowheads), characteristic features of the dentigerous cyst. The lesions expand along the longitudinal axis (i.e., anteroposterior dimension) of the mandible, with focal bone dehiscence in multiple areas (dashed arrows). Patient underwent surgical resection, with pathologically confirmed dentigerous cysts.
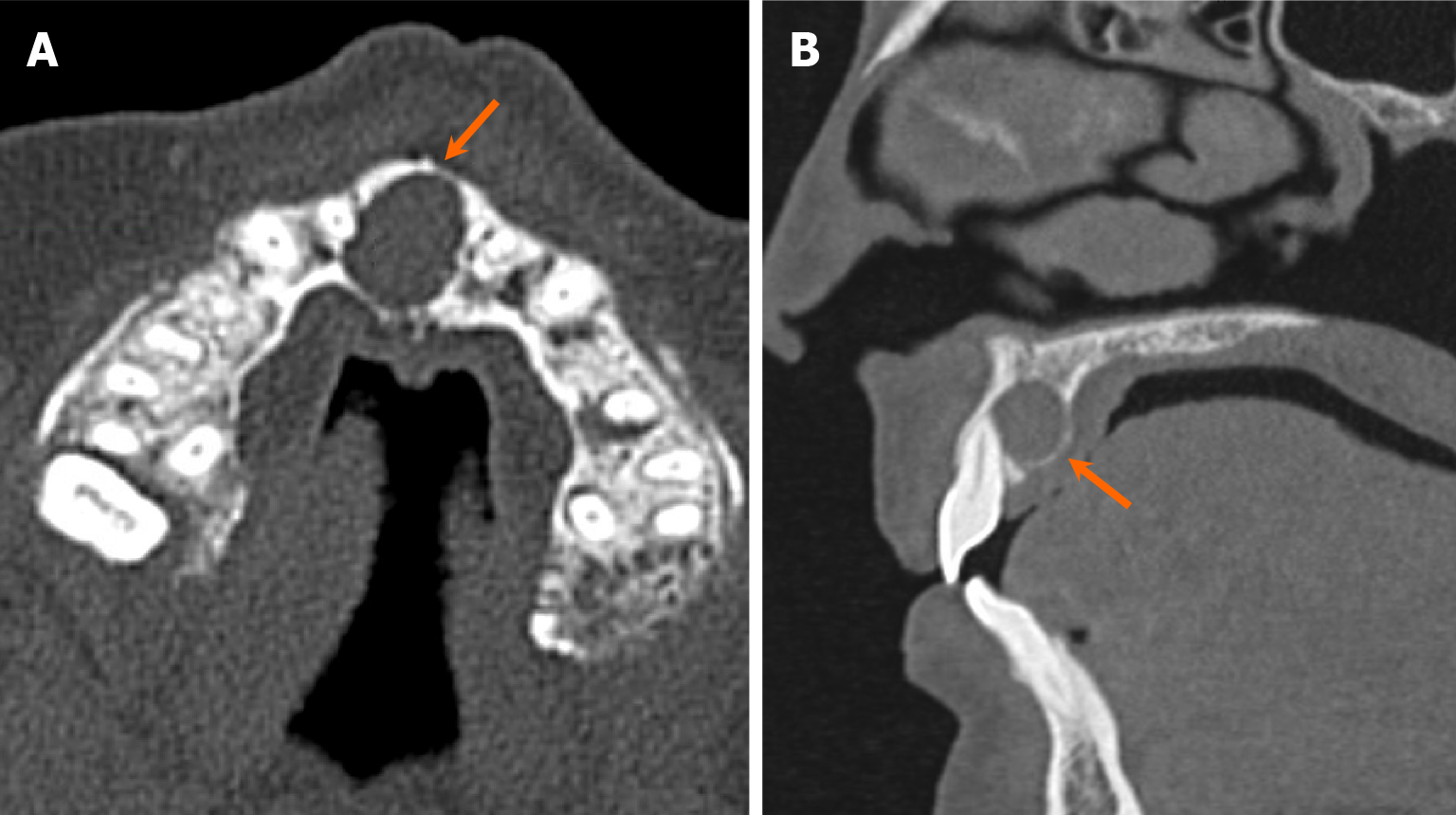
Figure 8 Nasopalatine duct cyst.
A and B: Axial (A) and sagittal (B) computed tomography images demonstrate an expansile, unilocular, well-marginated, cystic lesion located in the region of the incisive foramen (arrows). These findings are highly indicative of a nasopalatine duct cyst, a developmental non-odontogenic cyst resulting from incomplete regression of epithelium in the nasopalatine duct.
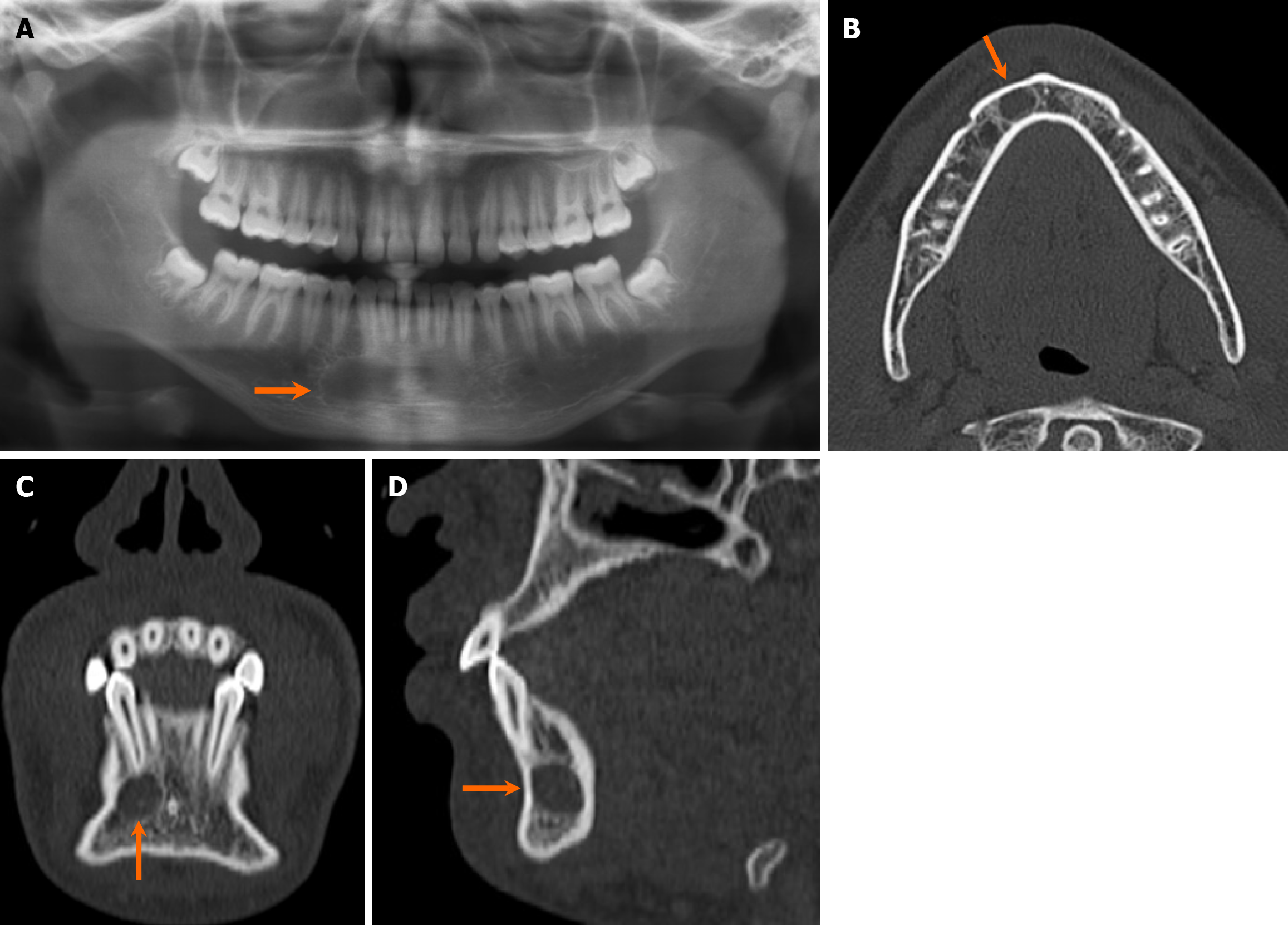
Figure 9 Simple bone cyst (aka traumatic bone cyst).
An 18-year-old man with an incidentally discovered radiolucent lesion in the right mandible. He has reported no associated pain, bony expansion, drainage, or numbness. A-D: Orthopantomogram (A), axial (B), coronal (C), and sagittal (D) computed tomography images reveal a small, well-marginated, unilocular cystic lesion at the right parasymphysis of the mandible, situated inferior to the apex of the lateral incisor (arrows), with no evidence of bone expansion. The tooth appears intact, showing no signs of erosion or associated dental caries. Patient underwent exploration and curettage of the lesion, with pathological confirmation of a simple bone cyst.
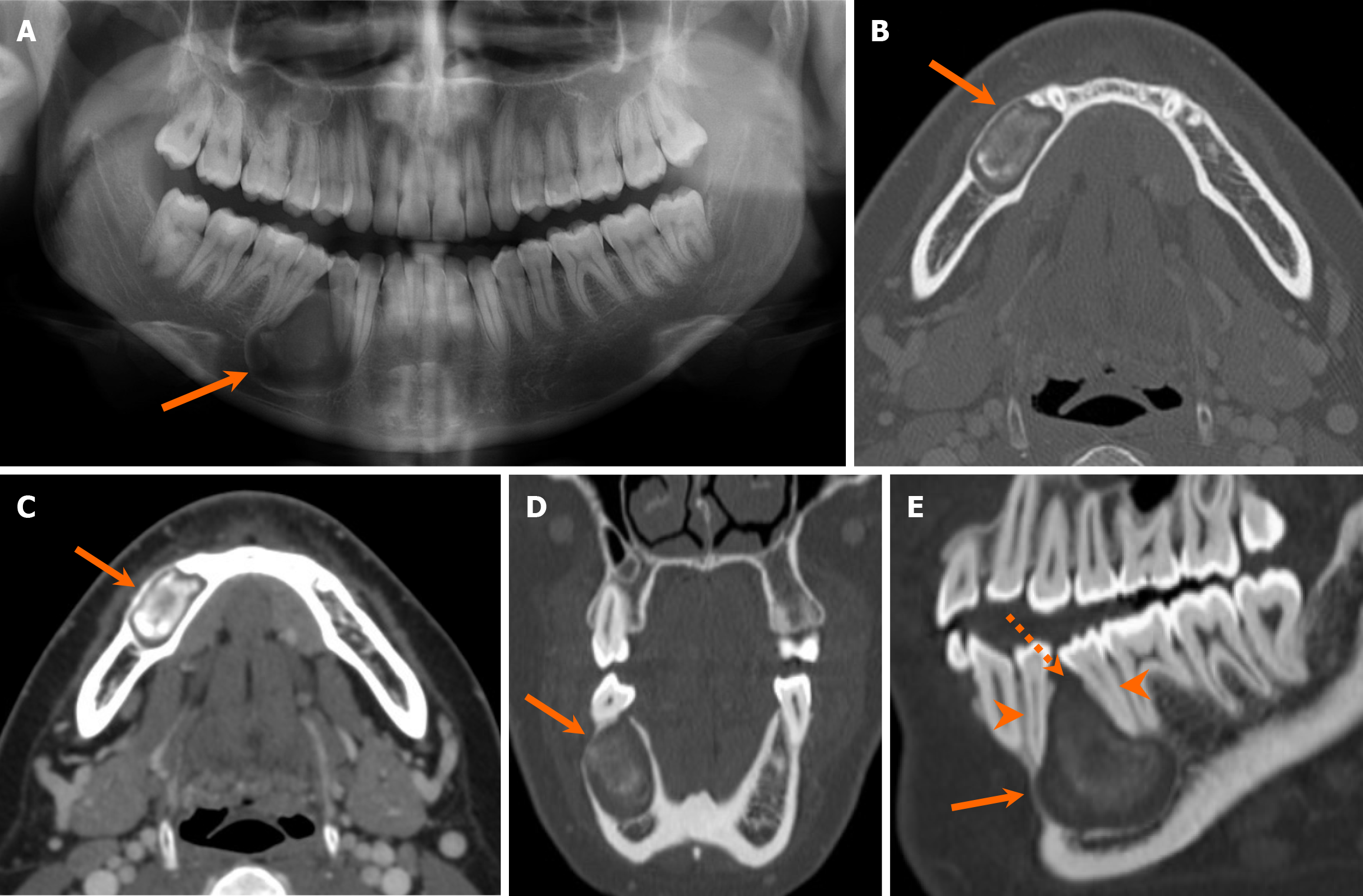
Figure 10 Odontogenic keratocyst.
A 23-year-old woman with an incidental radiolucent mandibular lesion detected on an X-ray. A-E: The orthopantomogram (A), axial (B and C), coronal (D), and sagittal oblique (E) computed tomography images demonstrate an expansile unilocular radiolucent lesion centered in the right mandibular body (arrows), containing mixed-density content. The lesion extends along the longitudinal axis of the mandible and exerts mass effect, causing mild displacement but no erosion of the adjacent teeth (arrowheads). There is focal cortical dehiscence at the superior aspect of the lesion (dashed arrow). Patient underwent surgical resection, and final pathology confirmed an odontogenic keratocyst.
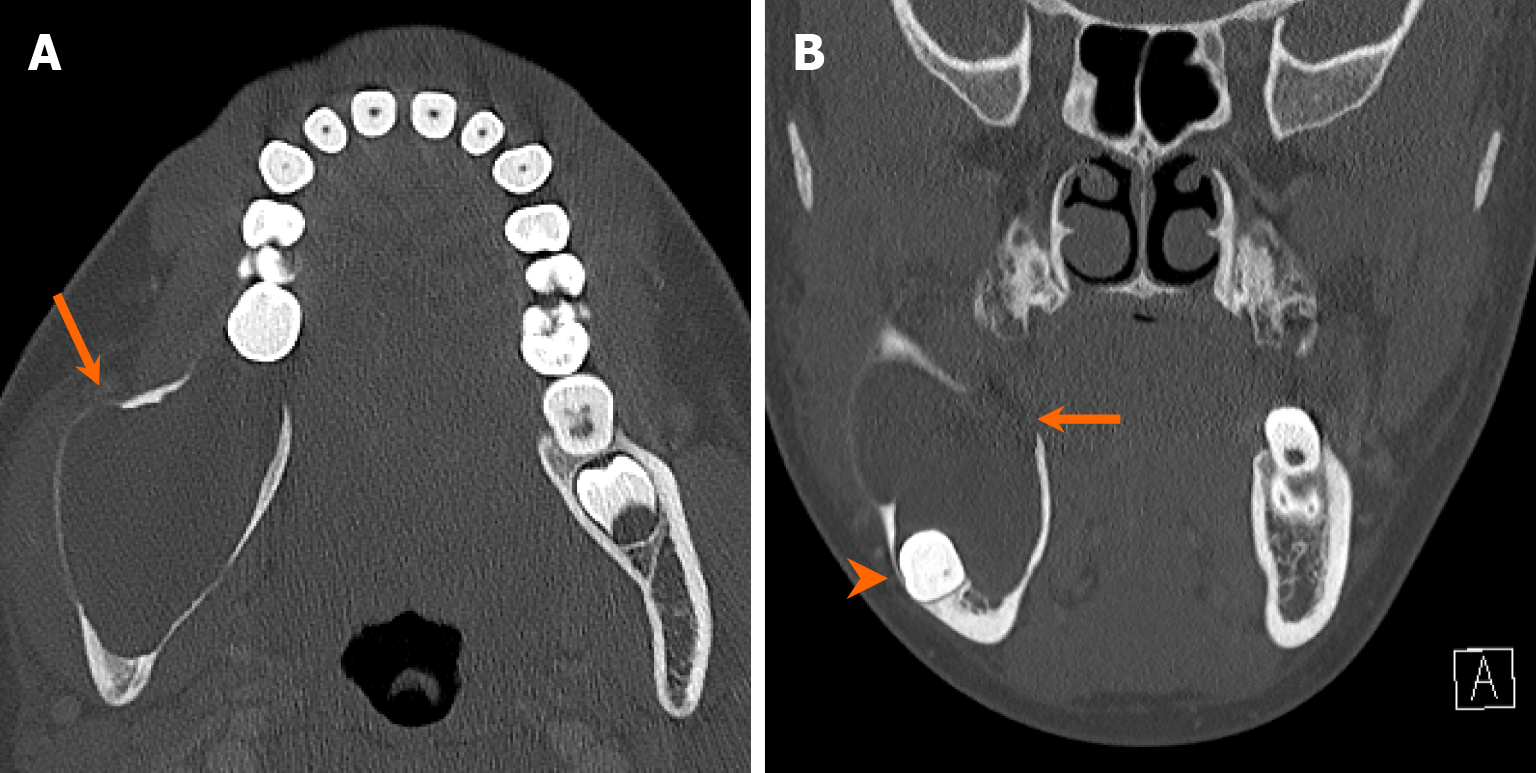
Figure 11 Unicystic ameloblastoma.
An 11-year-old girl with a 2-week history of right lower jaw swelling and facial pain. A and B: Axial (A) and coronal (B) computed tomography images demonstrate a large, expansile, unilocular, cystic lesion centered at the right mandibular angle (arrows). There is associated cortical thinning and multifocal bone dehiscence. Notably, there is inferior displacement of the unerupted third molar due to mass effect (arrowhead). Patient underwent surgical resection, with a pathologically confirmed diagnosis of unicystic ameloblastoma.
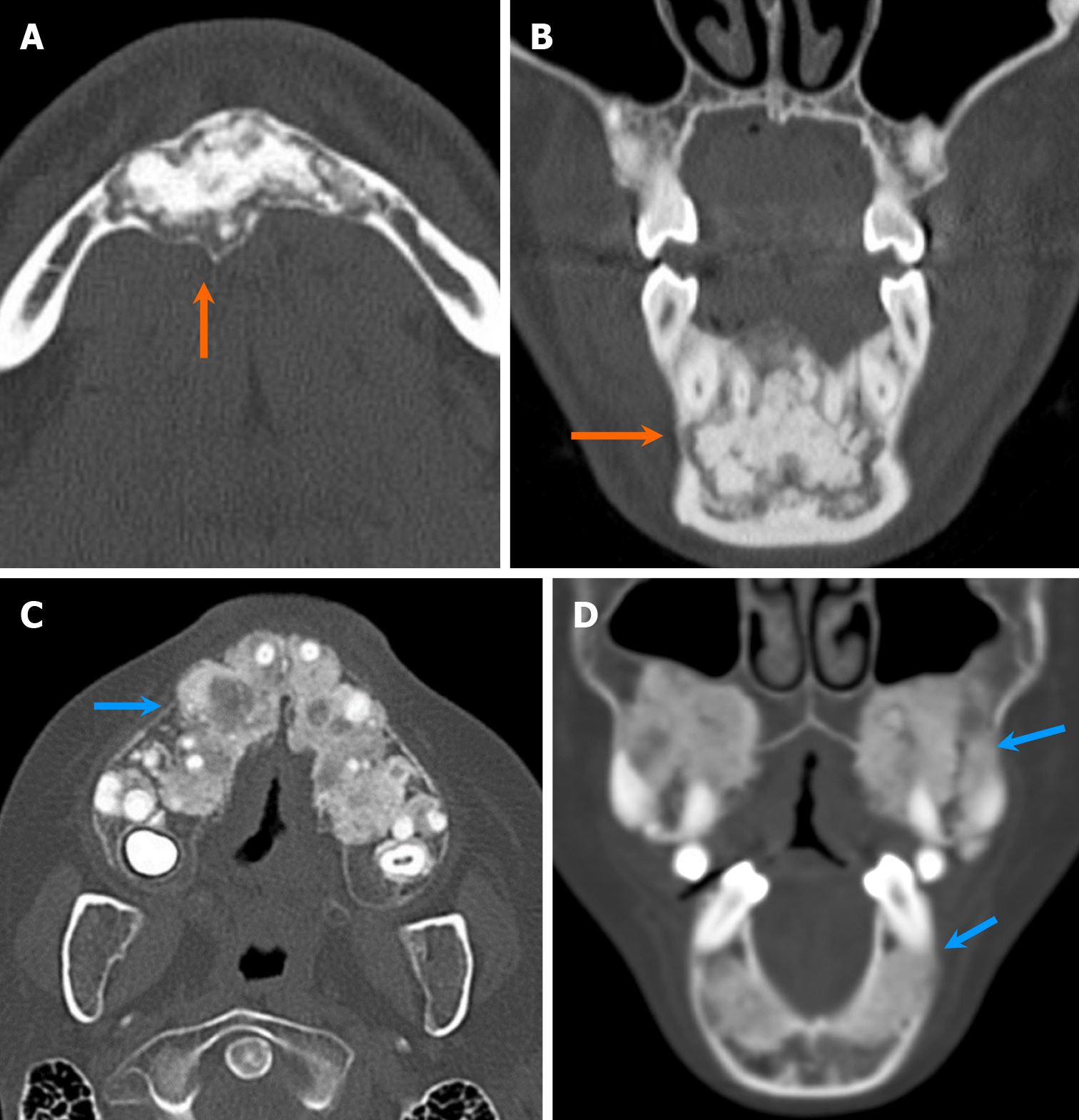
Figure 12 Conventional ameloblastoma of the mandible.
A 17-year-old girl with a several-month history of mandibular swelling and bilateral facial pain. A and B: Axial (A) and coronal (B) computed tomography images reveal an expansile multilocular radiolucent lesion in the left anterior aspect of the mandible (arrows), with a soap-bubble appearance. Note the multifocal cortical dehiscence in the affected bone (arrowhead). Patient underwent surgical resection with free flap reconstruction, and final pathology confirmed ameloblastoma.
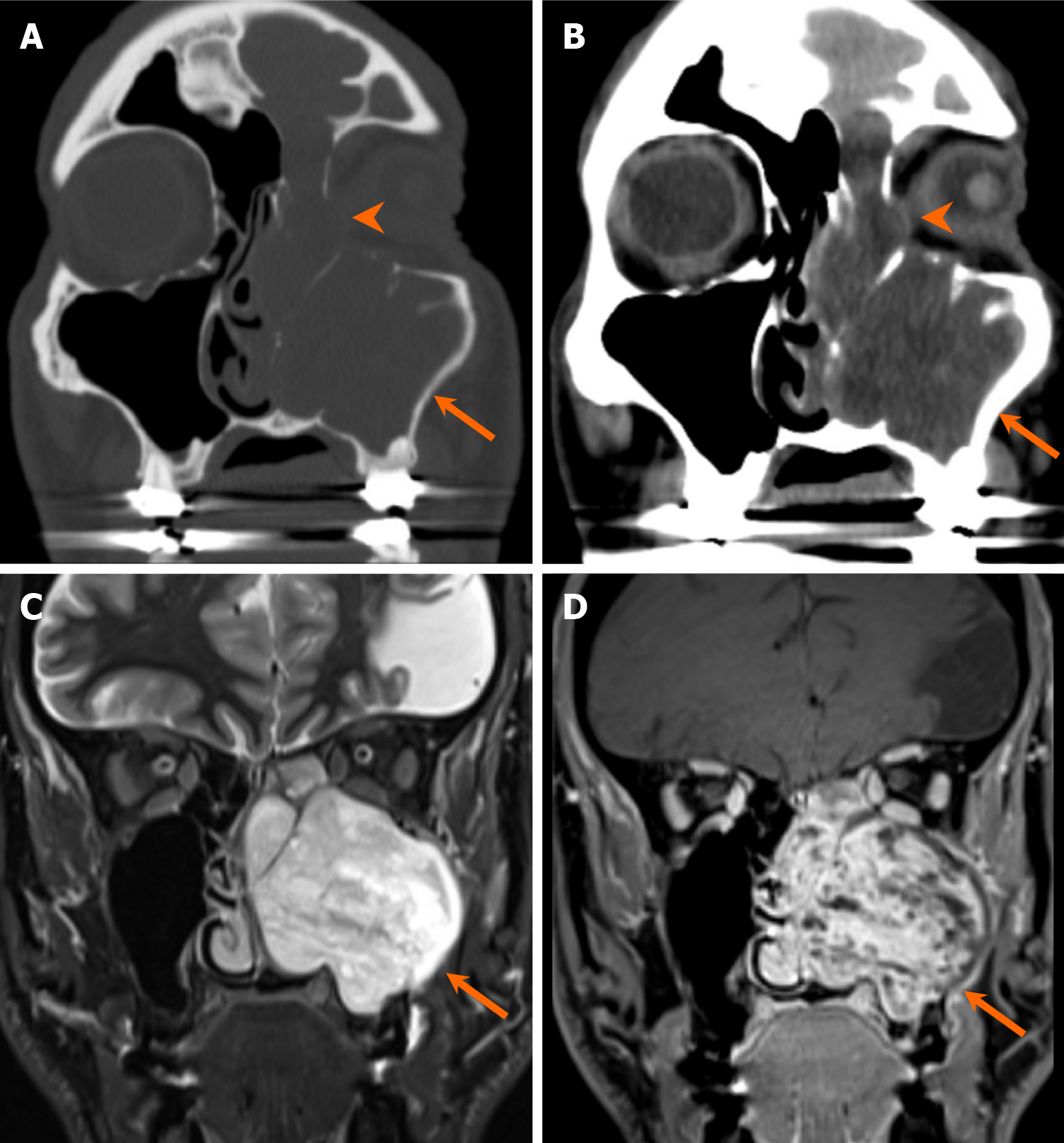
Figure 13 Conventional ameloblastoma of the maxilla.
A 61-year-old man with a several-month history of left-sided nasal congestion and facial pain. A-D: Coronal computed tomography (A and B), T2-weighted (C), and contrast-enhanced, fat-suppressed T1-weighted (D) magnetic resonance images reveal a large soft tissue mass occupying the left maxillary sinus and nasal cavity (arrows). The mass is T2 hyperintense and heterogeneously enhancing. There is focal dehiscence of the left lamina papyracea, with tumor extension into the orbit (arrowheads). Pathology confirmed ameloblastoma following resection.
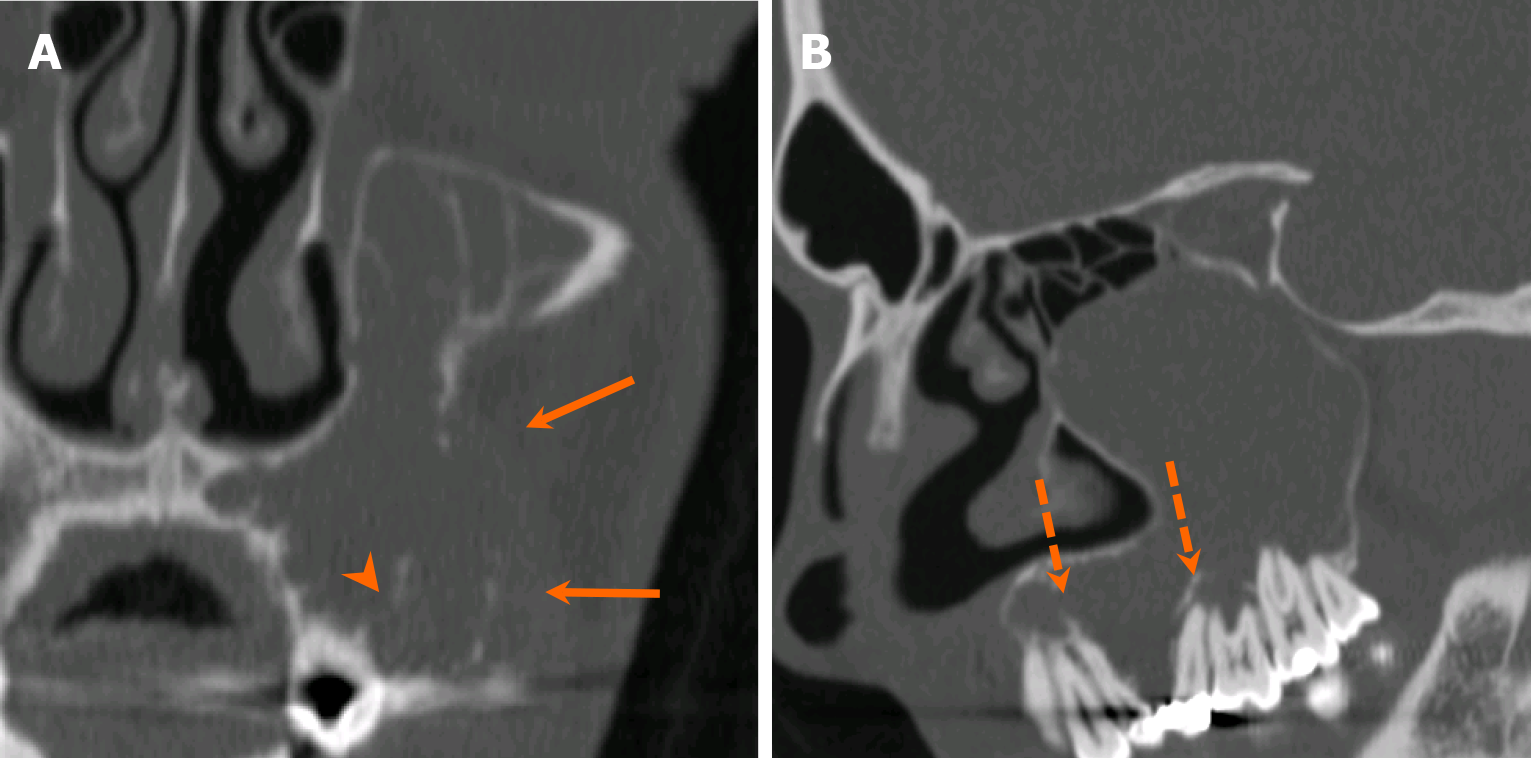
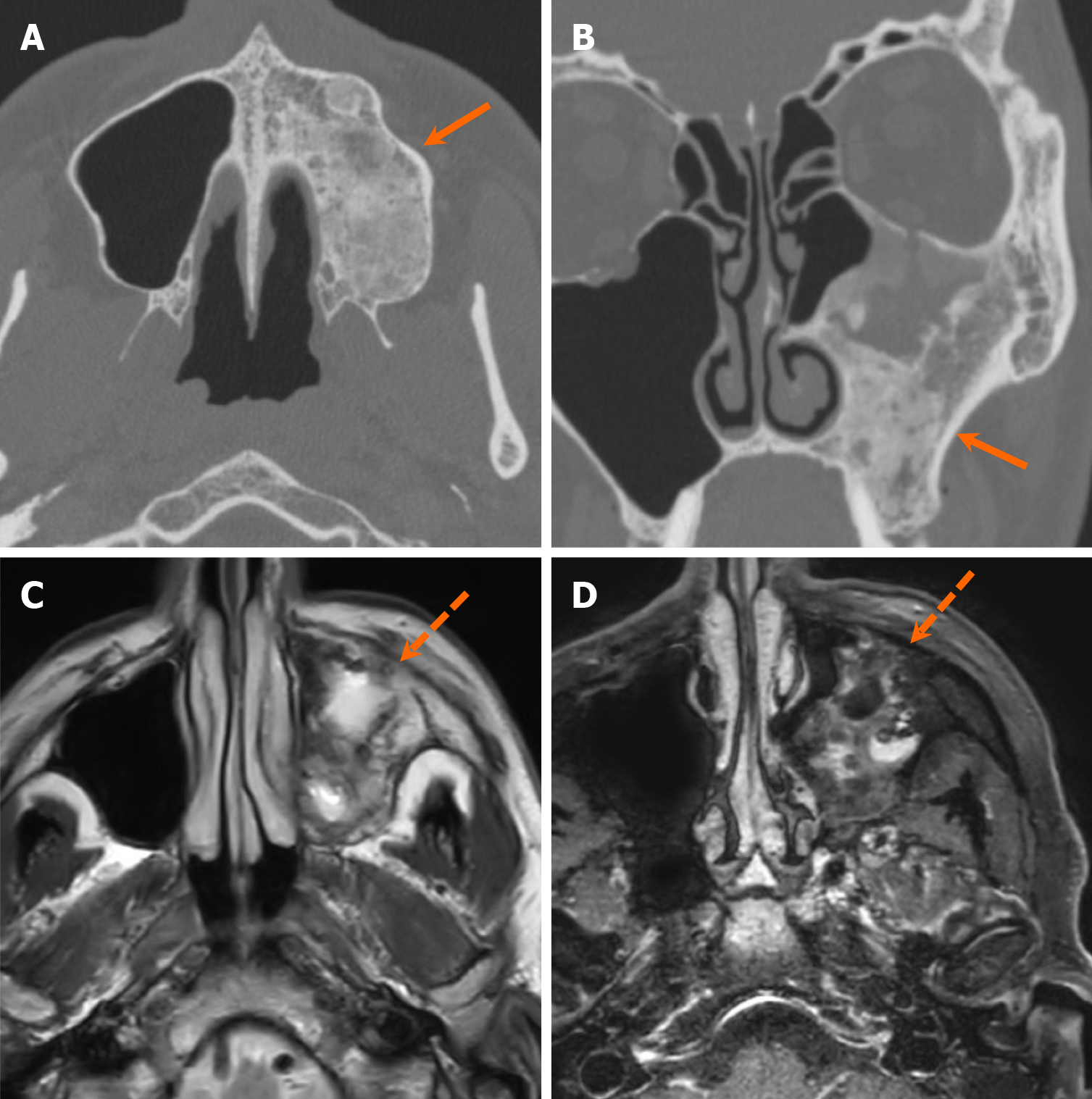
Figure 14 Odontogenic myxoma.
A 27-year-old man with a slowly enlarging, nonpainful left maxillary alveolar mass for several years. A and B: Coronal (A) and sagittal (B) computed tomography images reveal a large, expansile, multilocular radiolucent lesion originating from the maxillary alveolus and extending into the maxillary sinus, causing bone destruction with multifocal dehiscence (arrows). Note the ill-defined margins with internal septations along the alveolar process (arrowhead). The mass exerts a mass effect, causing tilting of the adjacent teeth (dashed arrows). Pathology confirmed odontogenic myxoma following resection.
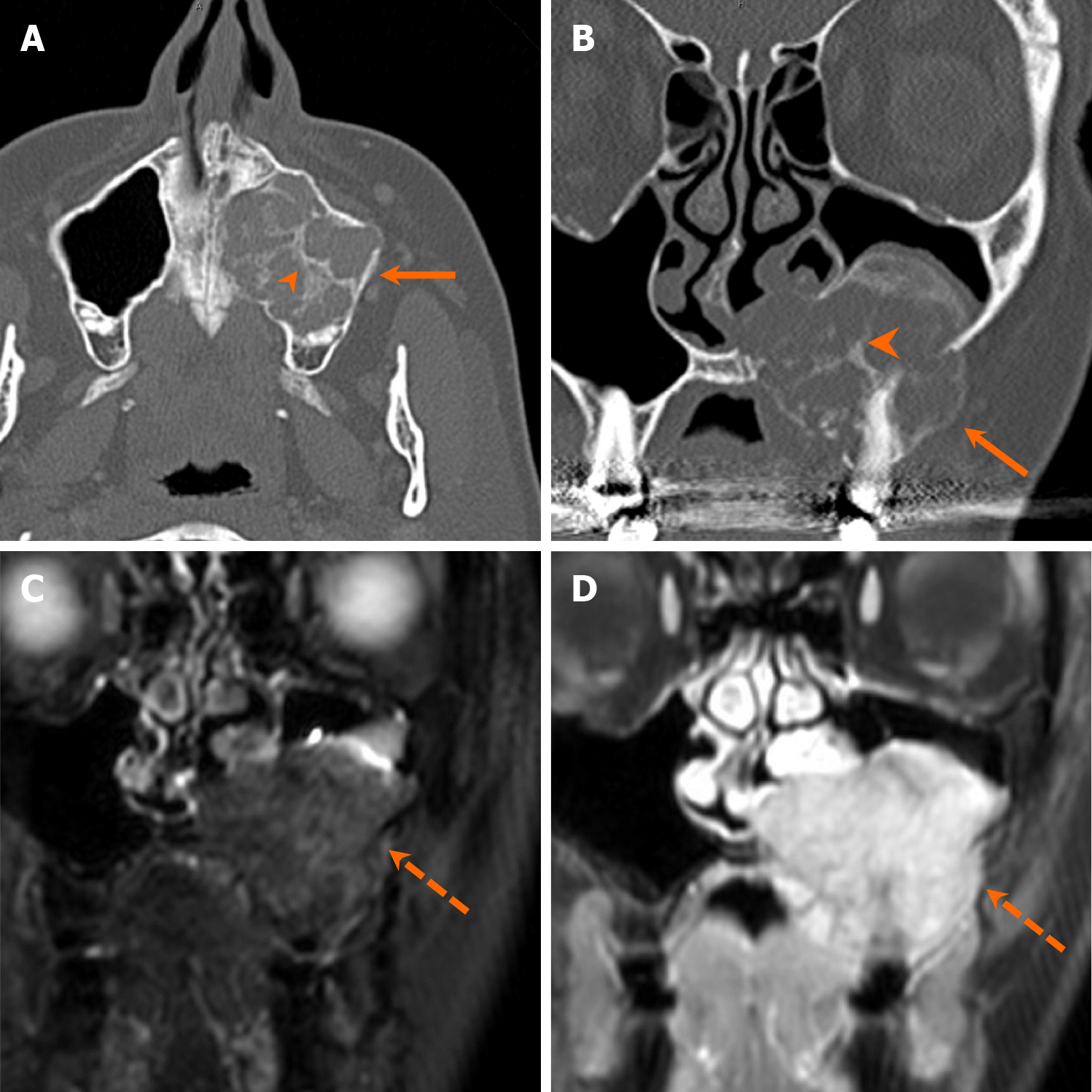
Figure 15 Giant cell granuloma.
A 58-year-old woman with left cheek discomfort. A and B: Axial (A) and coronal (B) computed tomography images show an expansile, multilocular radiolucent lesion involving the maxillary alveolus (arrows), with visible irregular ground-glass septa (arrowheads); C and D: Coronal STIR (C) and contrast-enhanced fat-suppressed T1-weighted (D) magnetic resonance images reveal an avidly enhancing, T2 hyperintense mass (dashed arrows). Pathology confirmed giant cell granuloma following resection.
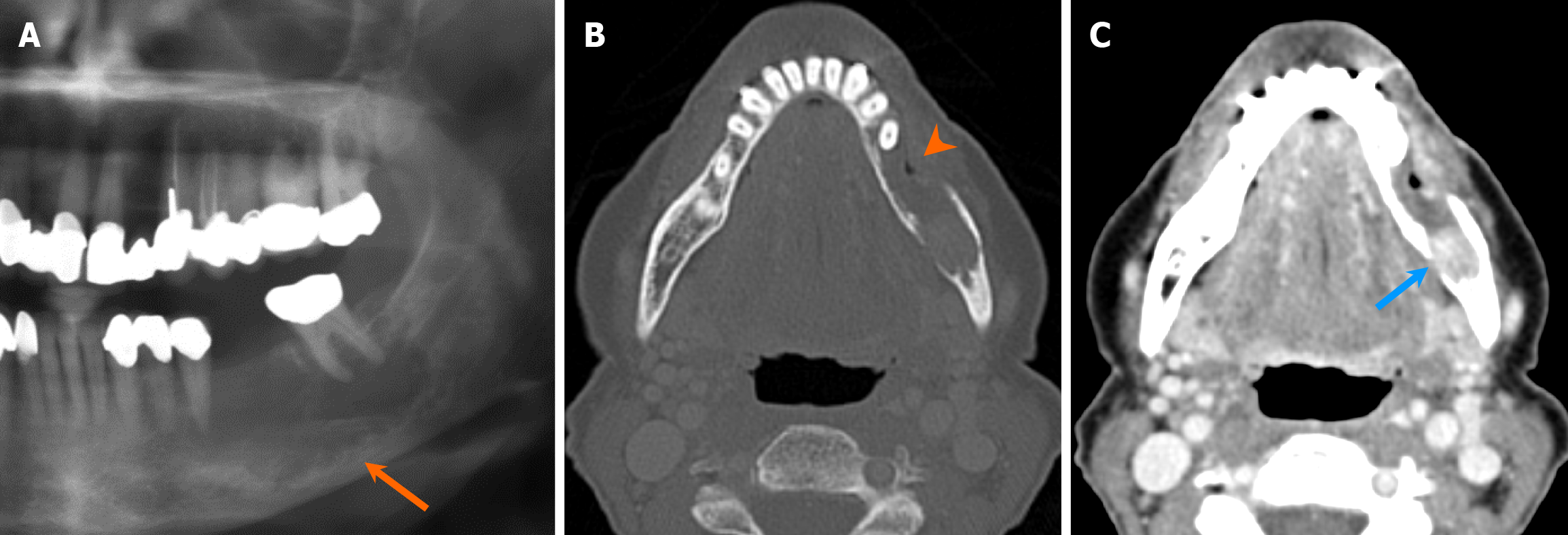
Figure 16 Odontogenic carcinoma.
A 71-year-old woman with persistent dull aching pain of the left mandible and left V3 paresthesia. A-C: Orthopantomogram (A) reveals a radiolucent lesion with ill-defined margins in the mandibular body, involving the inferior alveolar canal (arrow). Axial computed tomography images in bone (B) and soft tissue (C) windows show extensive cortical destruction (arrowhead) and an enhancing soft tissue component within the lesion (blue arrow). Pathology confirmed odontogenic carcinoma following resection.
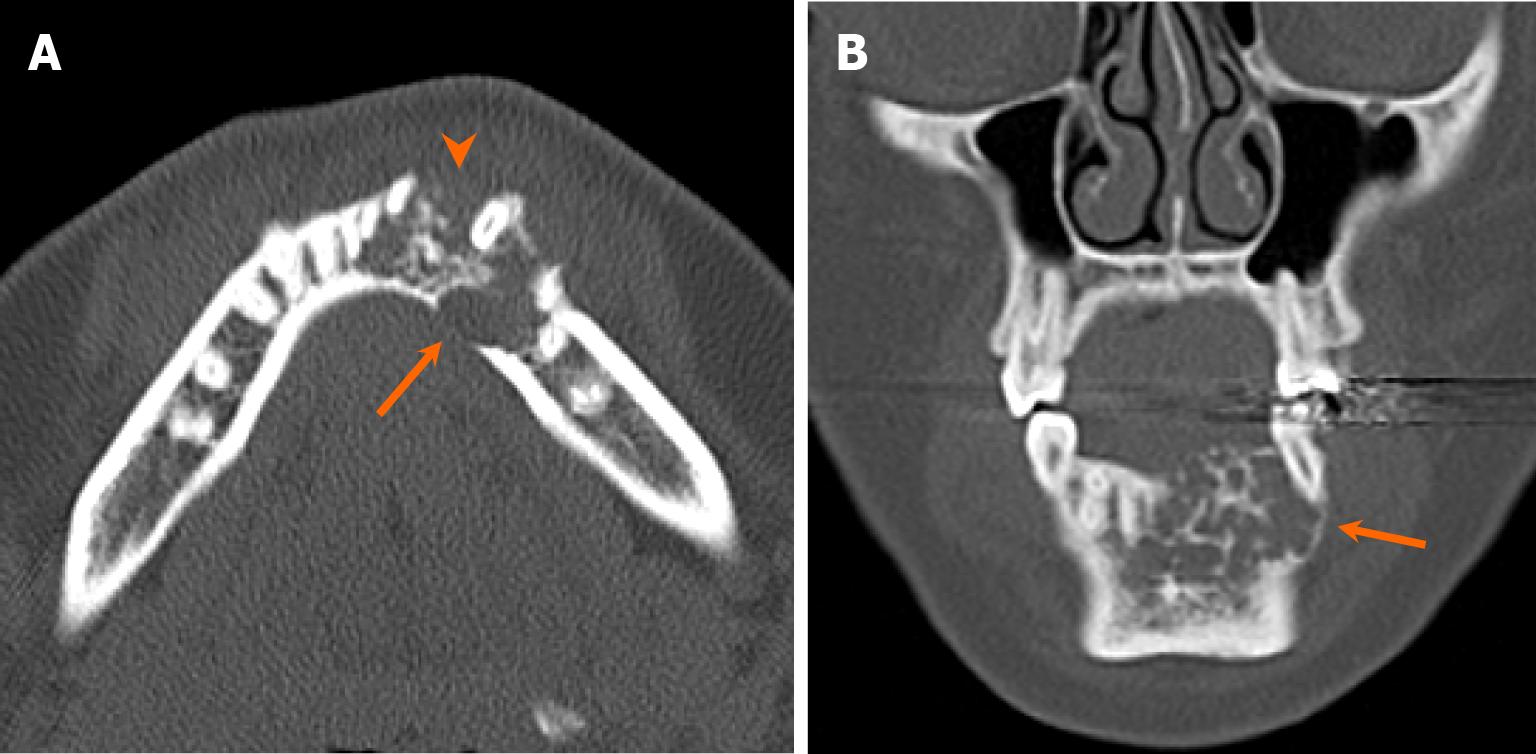
Figure 17 Cementoblastoma.
A-C: Orthopantomogram (A), sagittal (B) and coronal (C) computed tomography images show a densely sclerotic lesion (arrows) in the left mandible attached to the root of a canine, characteristic location of cementoblastoma. Note the lucent halo surrounding the lesion.
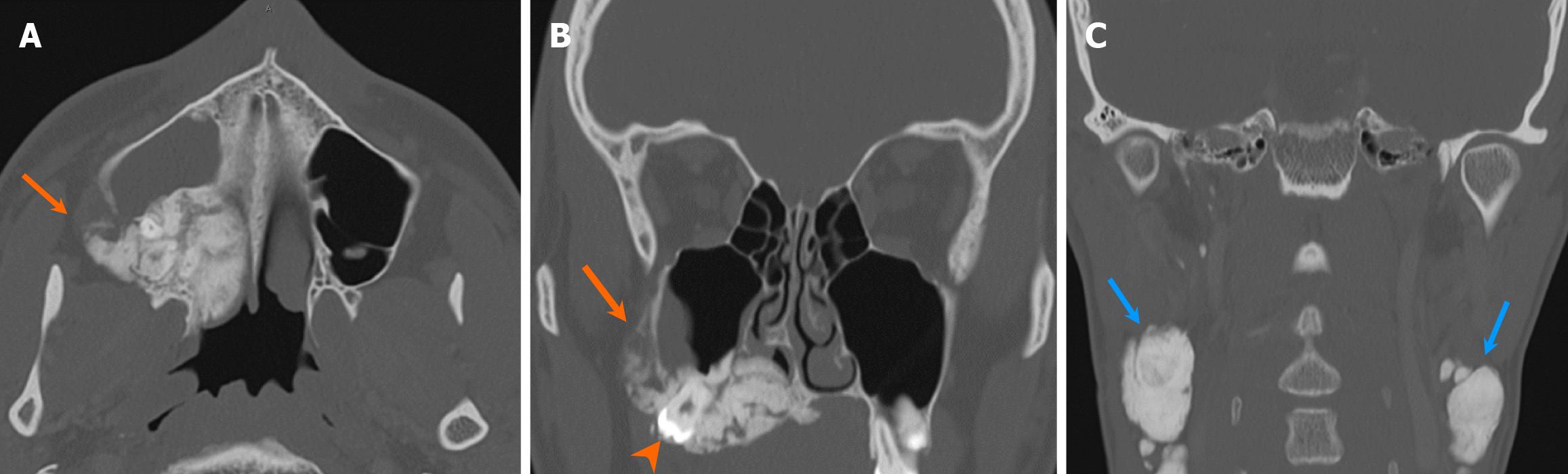
Figure 18 Compound and complex odontomas.
A and B: Coronal (A) and sagittal (B) computed tomography images show a densely sclerotic lesion in the right maxilla (arrows), composed of several small denticles resembling a tooth, consistent with a compound odontoma; C and D: Coronal (C) and sagittal (D) computed tomography images reveal an amorphous, densely sclerotic lesion in the left maxilla with a lucent rim (blue arrows), consistent with a complex odontoma. Note the displaced unerupted tooth just above the lesion (arrowhead).
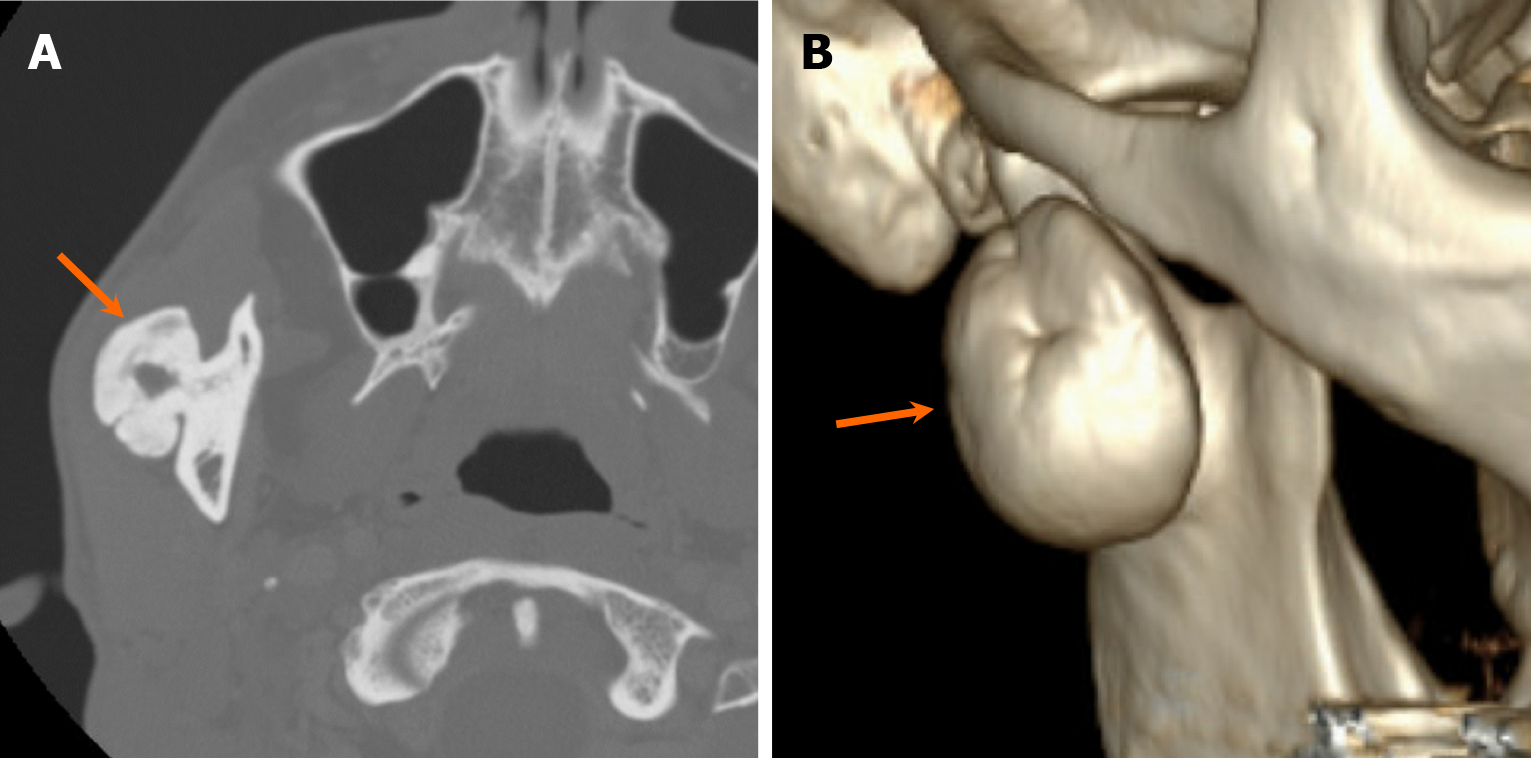
Figure 19 Osteoma.
A 43-year-old man with right mandibular osteoma. A and B: Axial (A) and volume-rendering reformatted (B) computed tomography images demonstrate a densely sclerotic, pedunculated, exophytic lesion arising from the outer cortex of the right posterior mandible (arrows). Pathology confirmed osteoma following resection.
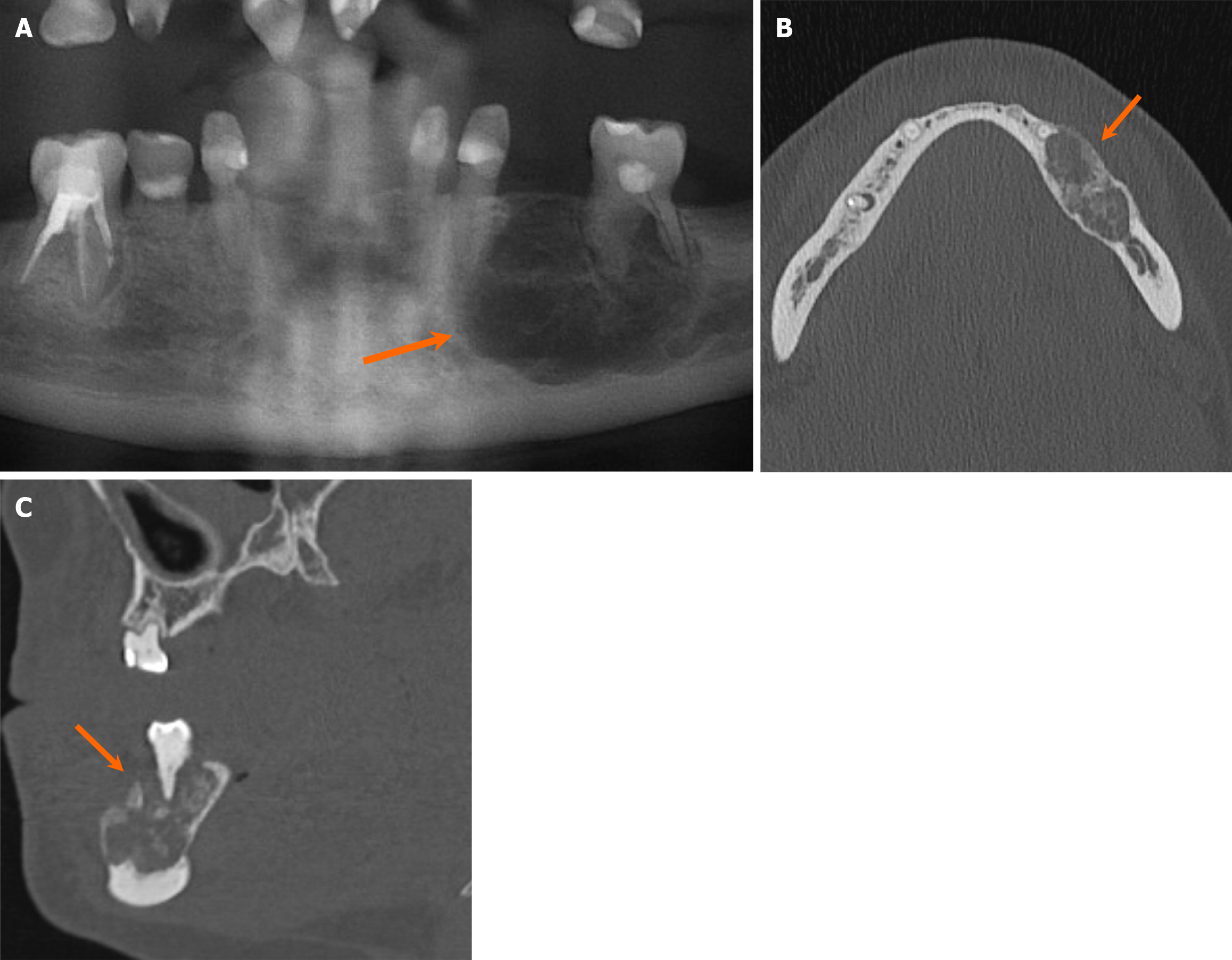
Figure 20 Cemento-ossifying fibroma.
A 34-year-old woman with an incidentally discovered radiolucent mandibular lesion. A-C: Orthopantomogram (A), axial (B) and sagittal (C) computed tomography images demonstrate a mixed lucent and ground-glass, mildly expansile lesion with well-circumscribed borders, involving the left mandibular body (arrows). Pathology confirmed cemento-ossifying fibroma following resection.
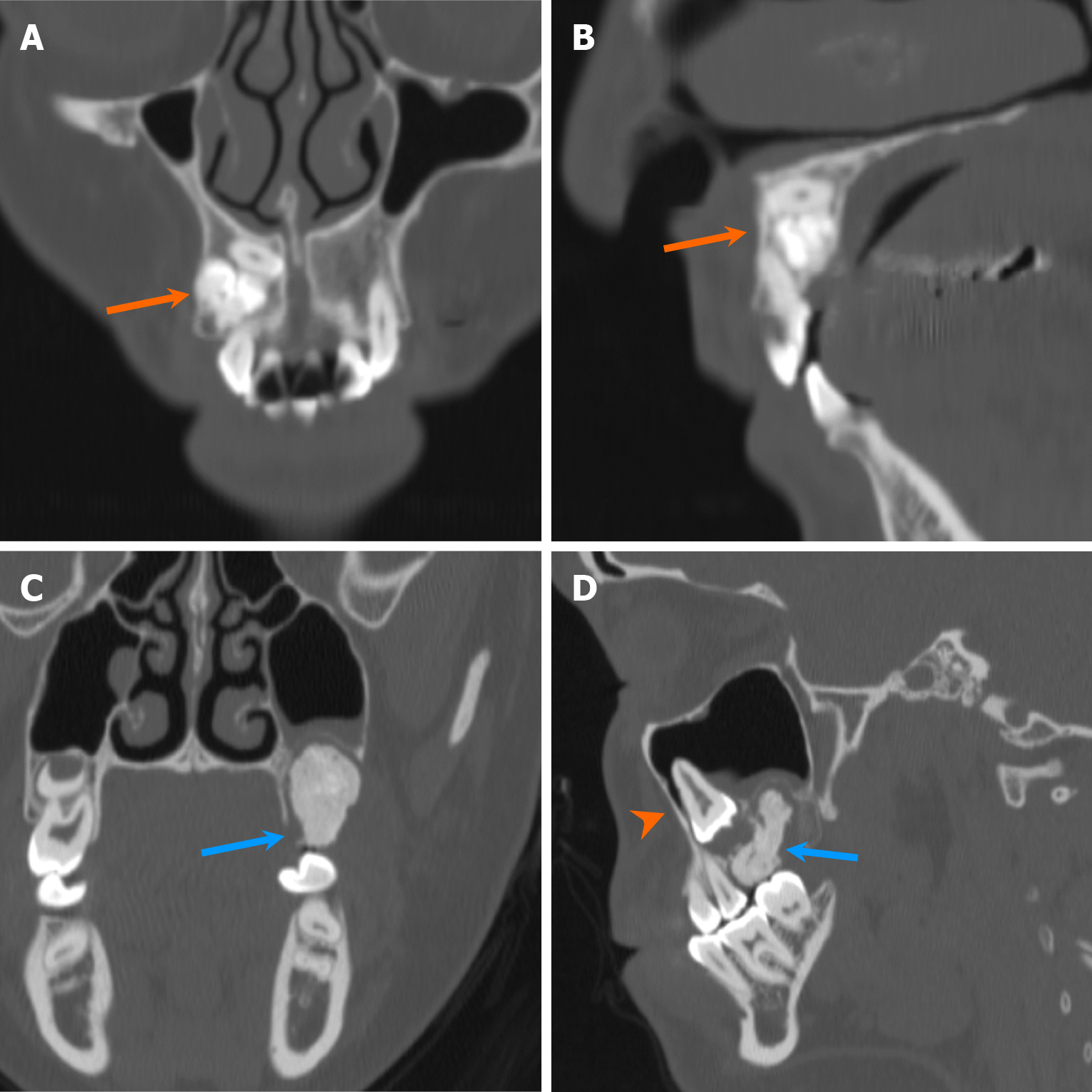
Figure 21 Two cases of cemento-osseous dysplasia.
A and B: Axial (A) and coronal (B) computed tomography images show a solitary, mildly expansile, densely sclerotic lesion in the anterior mandible with a narrow radiolucent rim and well-circumscribed borders (orange arrows). The lesions are attached to the roots of multiple teeth, indicating periapical cemento-osseous dysplasia; C and D: Axial (C) and coronal (D) computed tomography images of a companion case depict multifocal lesions with a ground-glass matrix in both maxilla and mandible (blue arrows), indicative of florid cemento-osseous dysplasia.
Figure 22 Fibrous dysplasia.
A 62-year-old man was found to have an incidental lesion in the left maxillary sinus wall on magnetic resonance imaging conducted to evaluate sensorineural hearing loss. A and B: Axial (A) and coronal (B) computed tomography images demonstrate an expansile, ground-glass density lesion involving the left maxilla (arrows) which is characteristic of fibrous dysplasia; C and D: Axial T2-weighted (C) and contrast-enhanced fat-suppressed T1-weighted (D) magnetic resonance images show mixed T2 signal intensity and heterogeneous enhancement (dashed arrows). The lesion has remained stable over 7 years of follow-up magnetic resonance imaging.
Figure 23 Osteosarcoma.
A 24-year-old man with a 2-year history of progressive soreness and swelling over the right palate. A-C: Axial (A) and coronal (B and C) computed tomography images show an expansile, irregular, densely sclerotic lesion with aggressive periosteal reaction (arrows). The lesion causes displacement of a tooth (arrowhead). There are multiple, large, densely calcified, bilateral cervical lymph nodes, consistent with metastatic lymph nodes (blue arrows). Pathology confirmed osteosarcoma following resection.
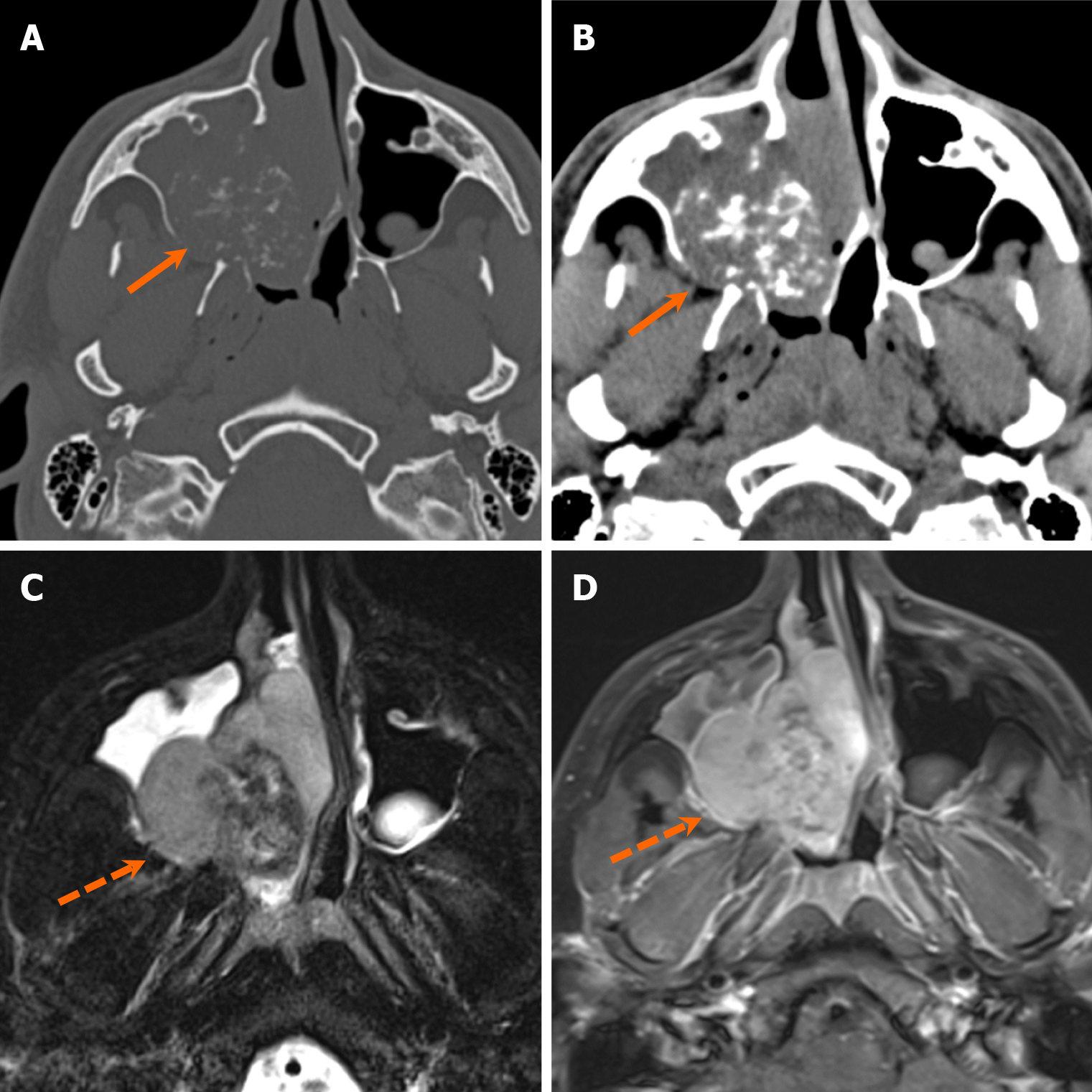
Figure 24 Chondrosarcoma.
A 19-year-old man with right nasal obstruction. A and B: Axial computed tomography images in bone (A) and soft tissue (B) windows depict an expansile right maxillary soft tissue mass with internal “ring-and-arc” calcifications (arrows); C and D: Axial T2-weighted (C) and contrast-enhanced fat-suppressed T1-weighted (D) magnetic resonance images demonstrate an enhancing mass (arrowheads) with heterogenous intermediate to low T2 signal due to internal calcifications. Pathology confirmed mesenchymal chondrosarcoma following resection.
- Citation: Choi WJ, Lee P, Thomas PC, Rath TJ, Mogensen MA, Dalley RW, Wangaryattawanich P. Imaging approach for jaw and maxillofacial bone tumors with updates from the 2022 World Health Organization classification. World J Radiol 2024; 16(8): 294-316
- URL: https://www.wjgnet.com/1949-8470/full/v16/i8/294.htm
- DOI: https://dx.doi.org/10.4329/wjr.v16.i8.294