Copyright
©The Author(s) 2023.
World J Radiol. Jun 28, 2023; 15(6): 157-169
Published online Jun 28, 2023. doi: 10.4329/wjr.v15.i6.157
Published online Jun 28, 2023. doi: 10.4329/wjr.v15.i6.157
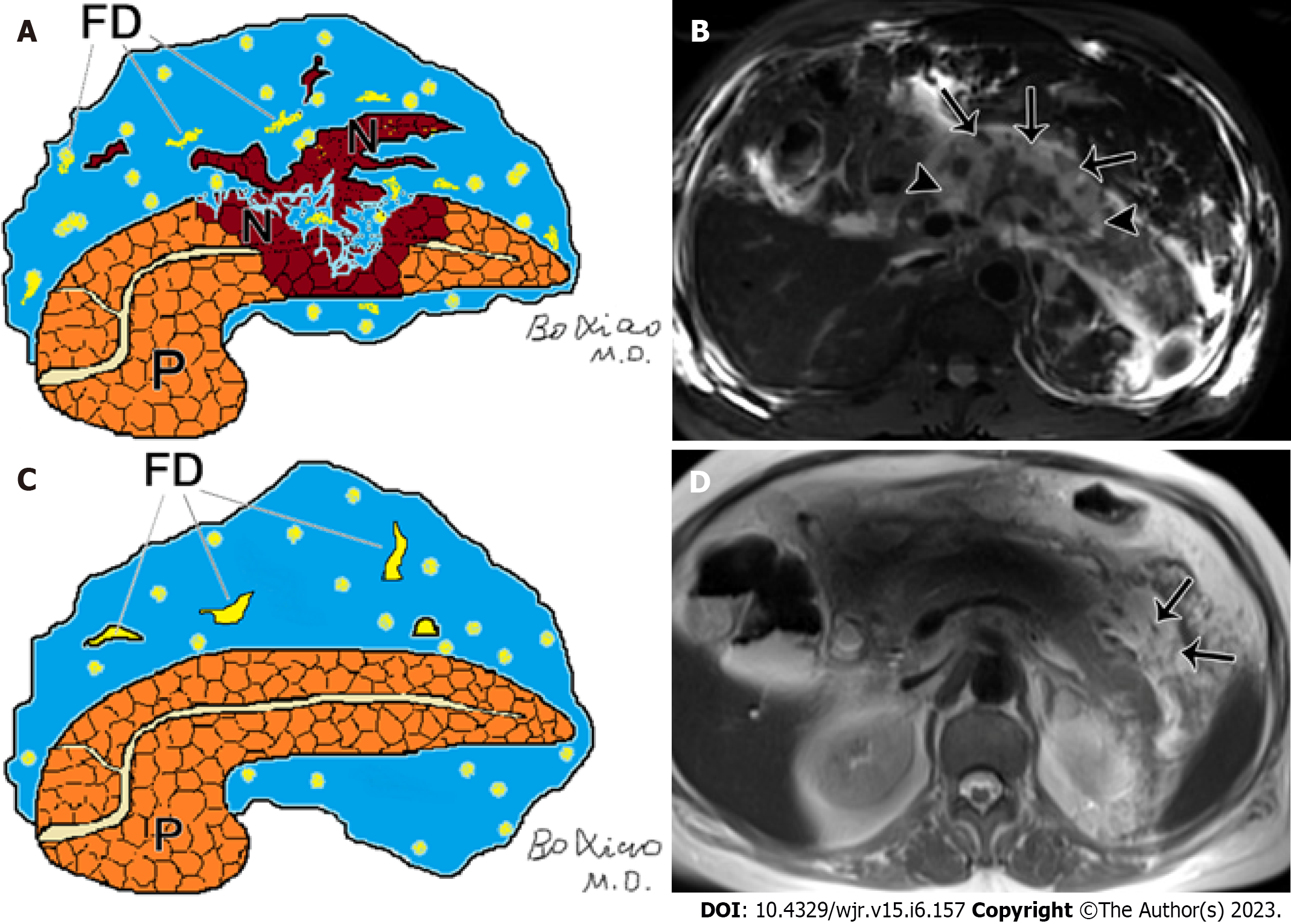
Figure 1 Pancreatic and peripancreatic necrosis.
A: Schematic diagram of pancreatic and peripancreatic necrosis (mixed type): pancreatic body necrosis (N) accompanied by peripancreatic fatty tissue debris (FD); B: A 61-year-old male with acute necrotizing pancreatitis (both pancreatic and peripancreatic necrosis). Fat-suppressed axial T1-weighted imaging shows a wide range of necrosis of the head and body of the pancreas (arrowheads), as well as peripancreatic collections containing large amounts of fat necrotic debris (arrows); C: Schematic diagram of necrotizing pancreatitis (peripancreatic necrosis alone): FD and absence of necrosis of pancreatic parenchyma; D: A 65-year-old woman with acute necrotizing pancreatitis (peripancreatic necrosis alone). Magnetic resonance imaging T2WI shows multiple patchy fatty fragments (hypointensity areas) (arrows) surrounding the pancreas.
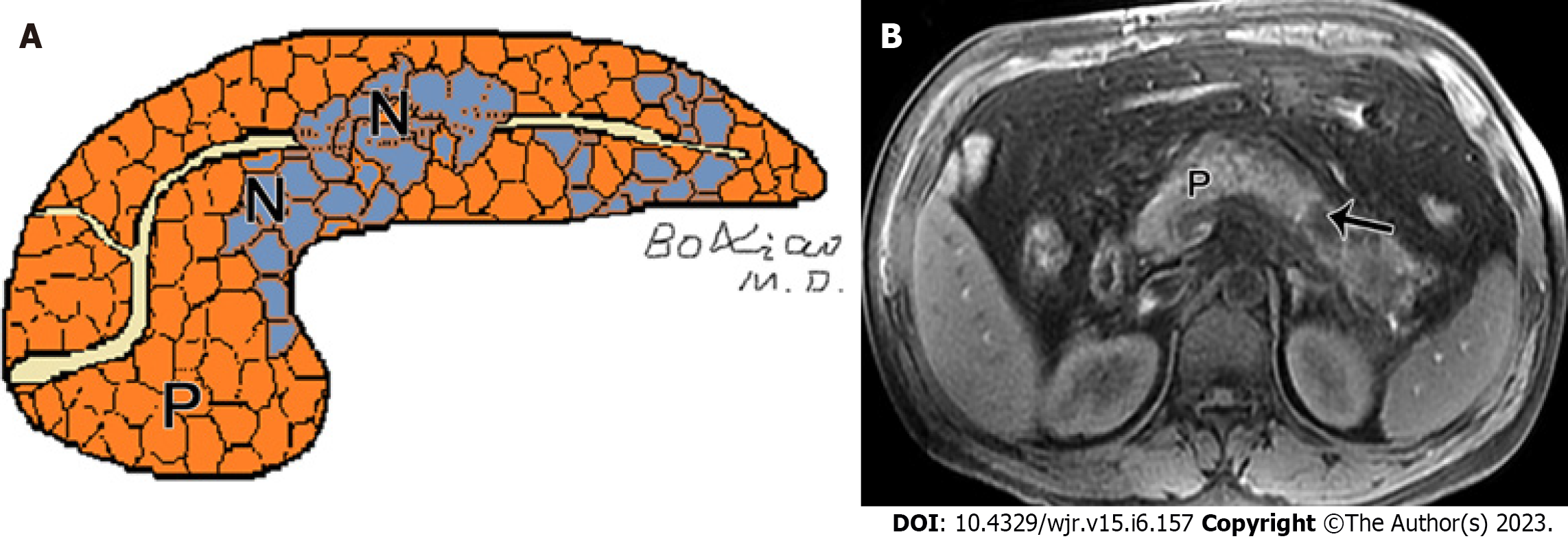
Figure 2 Peripancreatic necrosis only.
A: Schematic diagram of necrotizing pancreatitis (pancreatic necrosis alone): Scattered necrotic lesions (N) within the pancreatic parenchyma; B: A 40-year-old man with necrotizing pancreatitis (pancreatic necrosis alone). Magnetic resonance imaging fat-suppressed T1-weighted imaging shows hypointensity area (arrow) in the pancreatic body, as well as absence of peripancreatic fat involvement.
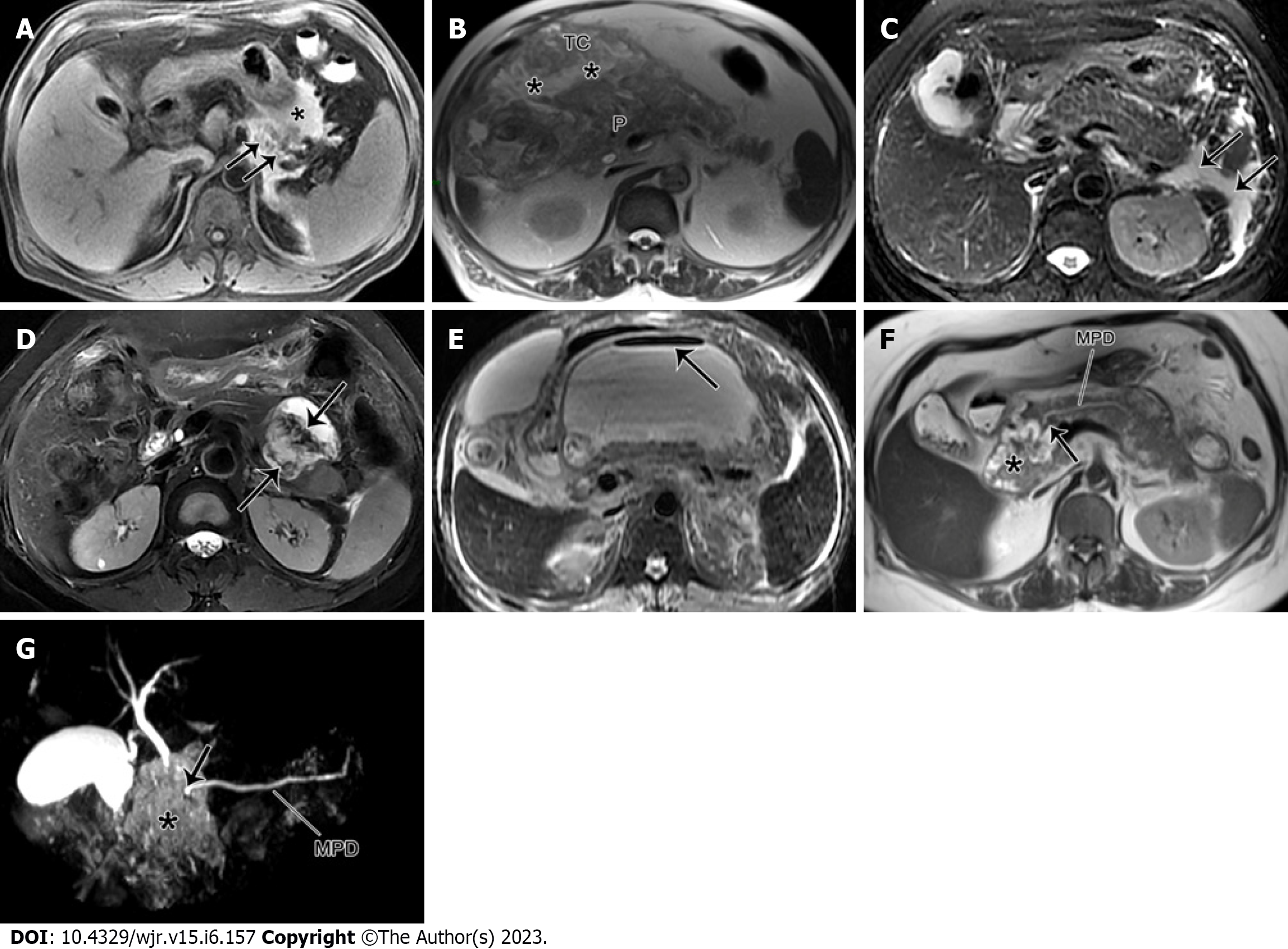
Figure 3 Pancreatic necrosis only.
A: A 47-year-old male with acute necrotizing pancreatitis complicated by hemorrhage. Magnetic resonance imaging (MRI) fat-suppressed T1WI depicts a large area of hyperintensity in the pancreatic body (arrow) and peripancreatic areas (*), indicating the presence of pancreatic and peripancreatic fat necrosis with hemorrhage; B: A 73-year-old man with acute necrotizing pancreatitis complicated with transverse mesenteric effusion. MRI T1-weighted imaging (T1WI) demonstrates peripancreatic inflammation spreading from the root of mesentery to the transverse colon along the involved transverse mesentery (*). P: pancreas; C: A 63-year-old woman with acute interstitial pancreatitis with acute peripancreatic fluid collection. MRI fat-suppressed T2WI reveals the uniformly hyperintense fluid collections (arrows) around the pancreas; D: A 53-year-old woman with walled-off necrosis secondary to acute necrotizing pancreatitis (pancreatic and peripancreatic necrosis type). MRI fat-suppressed T2WI shows an enveloped necrotic collection involving the body and tail of the pancreas, with solid necrotic debris (arrows) accounting for more than 40%; E: A 45-year-old man with acute necrotizing pancreatitis accompanied by walled-off necrosis and secondary infection. MRI fat-suppressed T2WI shows extensive walled-off necrosis in the omental sac, as well as a gas-fluid level sign (arrow). Thereafter, the open surgery and drainage for infectious collections was performed; F: A 55-year-old woman with pancreatic duct disruption syndrome secondary to acute necrotizing pancreatitis with walled-off necrosis. MRI T2WI shows an enveloped necrosis lesion (*) in the pancreatic head, and a cut-off sign (arrow) of the main pancreatic duct (MPD) traveling into this lesion (*). G: MRCP reveals that the MPD of the pancreatic body and tail directly enters into the lesion (*) in a right-angle, concomitant with the interrupted MPD.
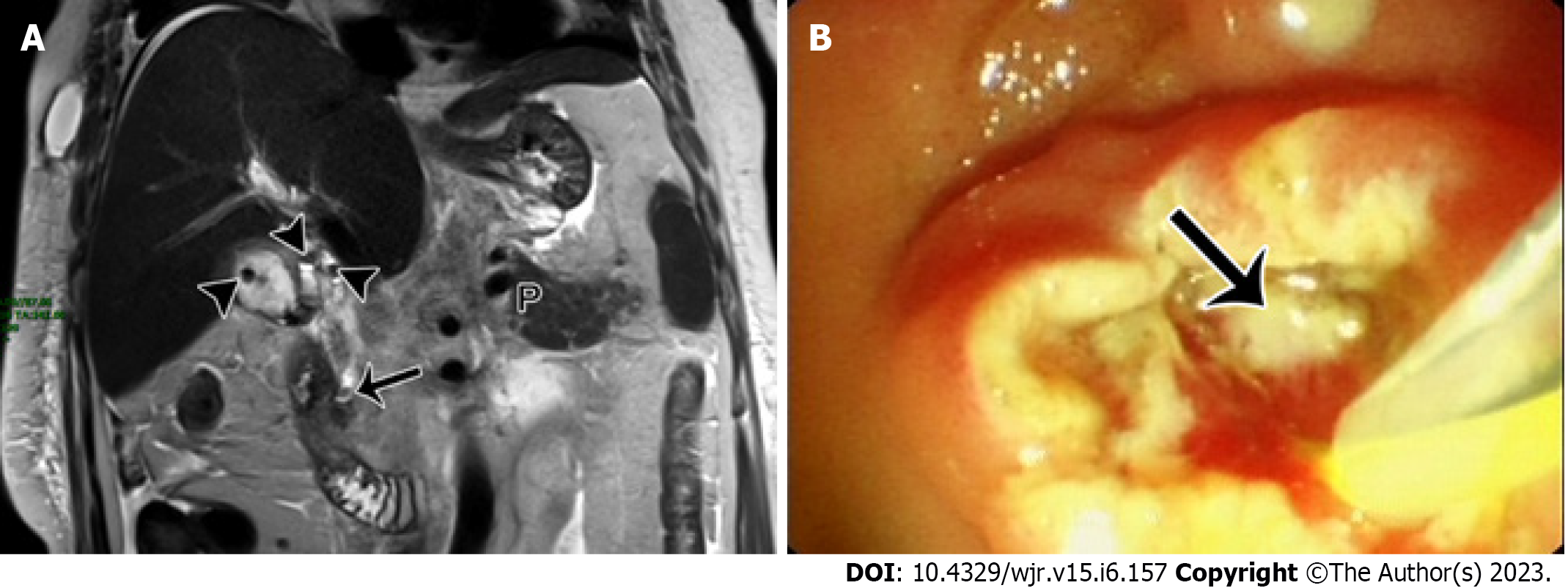
Figure 4 The magnetic resonance imaging report description needs to be focused on gallstone pancreatitis.
A 56-year-old woman with acute gallstone pancreatitis. A: Magnetic resonance imaging T2WI coronal imaging shows multiple hypointensity stones (arrowheads) in the gallbladder and gallbladder duct, and another hypointensity stone (arrow) in the lower level of the common bile duct. The patient was underwent an endoscopic retrograde cholangiopancreatography (ERCP) procedure; B: ERCP shows a stone in the lower part of the common bile duct with suppurative conditions (arrow). P: Pancreas.
Figure 5 Acute pancreatitis can also cause subcutaneous edema and fluid collection changes in the abdominal walls.
A 25-year-old man with acute necrotizing pancreatitis and acute necrotic collection accompanied by conspicuous subcutaneous edema. Magnetic resonance imaging fat-suppressed T1-weighted imaging shows a majority of hyperintense fluid collections (*) in the left pararenal anterior space, and large flaps of hyperintense changes (arrows) in subcutaneous tissues of bilateral flanks and abdominal walls. P: Pancreas.
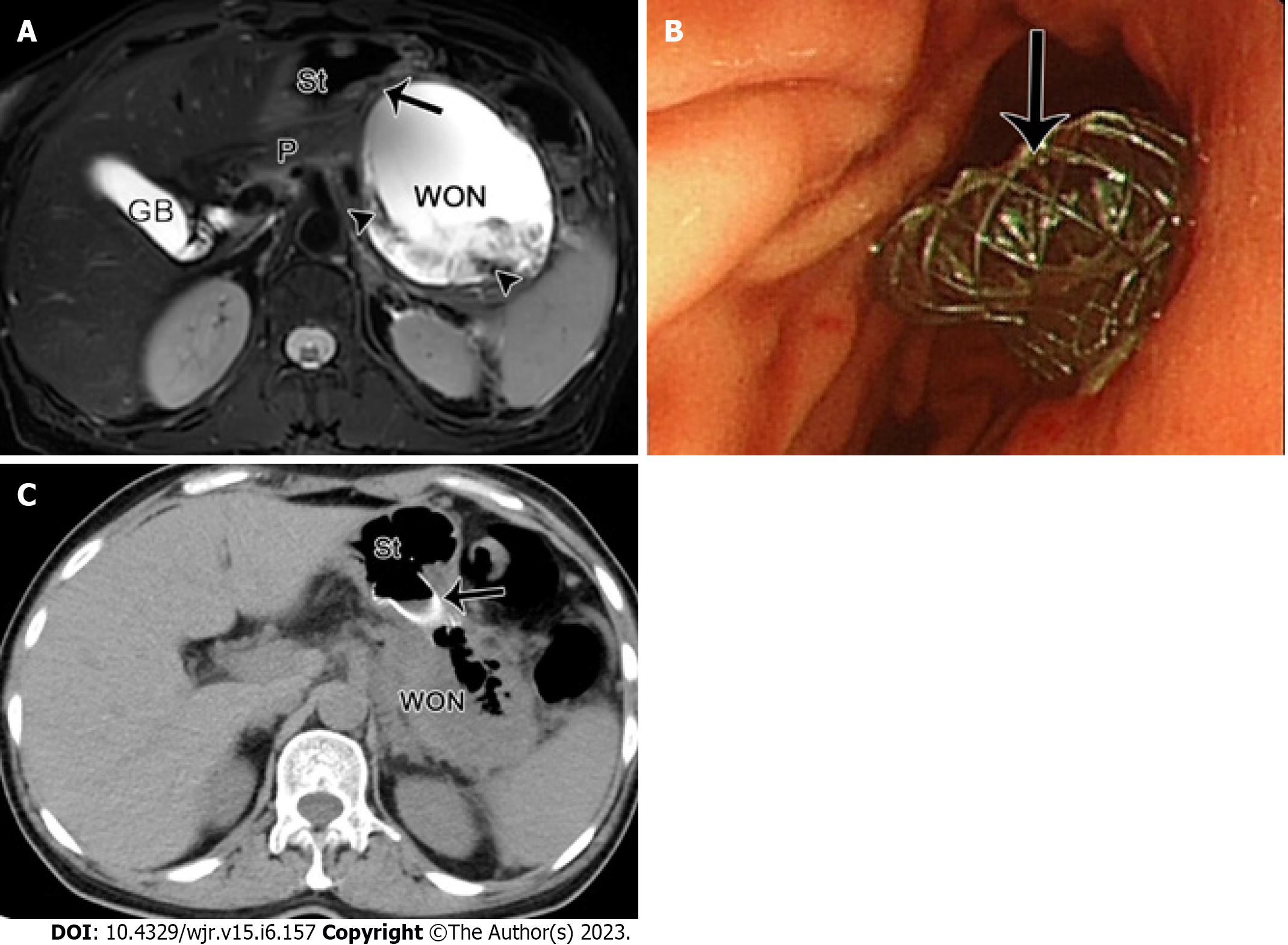
Figure 6 The radiological changes in pancreatic/peripancreatic fluid.
A 49-year-old woman with acute necrotizing pancreatitis and pancreatic walled-off necrosis, performed by endoscopic ultrasound drainage. A: Magnetic resonance imaging fat-suppressed T1-weighted imaging shows a walled-off necrosis (WON) with a diameter of 10 cm × 9 cm in the omental sac and pancreatic body and tail, as well as numerous necrotic fragments (arrowheads) within the WON. The WON is adjacent to the gastric body; B: Thereafter, under the guidance of endoscopic ultrasonography, a fully coated mushroom metal stent (arrow) was placed through the stomach for internal drainage; C: Postoperative computed tomography image shows that the WON was apparently decreased, with a large amount of gas and a high-density stent (arrow) in place. St: Stomach, P: Pancreas, GB: Gallbladder.
- Citation: Song LJ, Xiao B. Acute pancreatitis: Structured report template of magnetic resonance imaging. World J Radiol 2023; 15(6): 157-169
- URL: https://www.wjgnet.com/1949-8470/full/v15/i6/157.htm
- DOI: https://dx.doi.org/10.4329/wjr.v15.i6.157